Pyomyositis
| Classification according to ICD-10 | |
|---|---|
| M60.0 | Infectious myositis, tropical pyomyositis (possibly also B95 – B97 to indicate the infectious agent; B95.6 for Staphylococcus aureus ) |
| ICD-10 online (WHO version 2019) | |
Pyomyositis , also known as pyomyositis tropicans , myositis purulenta , Bungpagga or Lambo Lambo , is an acute bacterial infection of the skeletal muscles , which is usually caused by the pathogen Staphylococcus aureus . The most important symptom of the disease in its advanced stages are pus-filled abscesses in the muscles. It is much more common in tropical areas than in other regions, where it is considered rare and often occurs in immunocompromised patients. The treatment is carried out by surgical therapy of the abscesses and an accompanying administration of antibiotics .
distribution
In the tropics , pyomyositis is considered to be endemic ; the incidence rate in Uganda, for example, is 1: 1000. In these regions, the proportion of affected patients in all hospital admissions is one to four percent and in deaths up to 13 percent. The disease occurs here with a sex ratio (male / female) of 3: 1 to 5: 3, predominantly in male patients. It can affect all age groups, but is mainly found in children and younger people with an age focus of 10 to 40 years.
In non-tropical areas, however, pyomyositis is rare today. In these regions, it is mainly adults and the elderly who are affected; there is no evidence of an increased prevalence in men or women. With up to 75 percent of non-tropical cases it is a sequela of severe immunodeficiency forms such as in AIDS patients in cancer patients with chemotherapy or in patients with immunosuppressive treatment following organ transplantation . An infection with HIV can be detected in around 20 percent of pyomyositis patients in the temperate regions . In addition, the disease occurs in around a quarter of patients from regions with a temperate climate close to a trip to the tropics. Nevertheless, cases from moderate climates without a history of a tropical trip are reported again and again (Broich 1991).
A previous or accompanying injury from accidents or other forms of violence in the affected muscle area can be detected in 25 to 40 percent of patients. The period from July to September is considered the maximum incidence over the course of the year.
Cause and development of the disease
Pyomyositis is caused by a bacterial infection of the skeletal muscles . This is caused by Staphylococcus aureus in around 90 to 95 percent of affected patients in the tropics and in around 70 to 75 percent of cases in non-tropical regions . In up to five percent of the other cases, A streptococci such as Streptococcus pyogenes can be detected, other pathogens described include Staphylococcus epidermidis , Streptococcus pneumoniae , Proteus mirabilis , Yersinia enterocolitica , Escherichia coli and various types of salmonella .
Due to the frequency of injuries immediately before the disease as well as the detection of pyomyositis after injury in connection with an intravenous infection with Staphylococcus aureus in an experimental model (Myake 1904), an injury is considered by some authors to be decisive or a risk factor. In addition to trauma, intense stress, generalized muscle contractions such as in electrical accidents , chronic diseases such as diabetes mellitus and the use of medication such as zidovudine (AZT) or steroids are all possible causes of muscle damage that can lead to pyomyositis in the affected muscles after a corresponding infection . Worm diseases , for example with nematodes or viruses, have also been postulated as causes or risk factors for tropical pyomyositis .
The exact pathogenesis has not yet been clearly clarified, although there is much to be said for a bacterial origin. It is believed that this is a complication of temporary bacteremia (presence of bacteria in the blood) and that an injury to the muscles creates a locus minoris resistentiae , i.e. a place where the normally high resistance of muscle tissue to bacterial infections is decreased. In addition, the release of iron from the myoglobin of damaged muscles may encourage the growth of bacteria.
Clinical manifestations
In principle, all muscles on the body can be affected when the abscesses are distributed. The frequency seems to tend to correspond to the distribution of muscle mass, which is why large muscles appear to be affected more often. Most of the reporters do not find a preferred page location (Broich 1991), so that the theory of preferred right-sidedness cannot be maintained because of the more frequent trauma there (Asken and Cotton 1963).
In the first phase of the disease, which is also known as the invasive phase and lasts around two weeks after infection, the symptoms are usually subacute and unspecific, which means that they usually remain undetected or are neglected. The most common signs during this phase are fever and loss of appetite (anorexia). Local symptoms include swelling and mild pain . Skin reddening (erythema) and overheating of the affected areas do not always occur in this phase , as the infection is still localized in the deeper muscle areas.
In the second phase, also known as the festering phase , in which the diagnosis is often made, there is a high fever, chills and a septic- induced systemic inflammatory response syndrome (SIRS). Local symptoms during this phase include increased muscle tension and pain , inflammation of the skin, and the appearance of pus .
In the third and most serious phase, the so-called late phase , in addition to the symptoms already mentioned, there is an increased formation of pus, the increased formation of abscesses (encapsulated pus collections), arthritis (joint inflammation), kidney failure and sepsis up to septic disease Shock.
Investigation methods
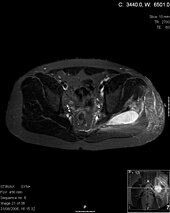
The most important diagnostic methods for suspected pyomyositis are imaging procedures such as sonography , which can confirm disorders of the muscle structure and the presence of accumulations of pus in the muscles. However, the benefits are limited during the first phase of the disease. With a computed tomography , muscle swelling and reduced muscle density can be detected before the appearance of abscesses, with an MRI examination the extent and localization of the disease can be assessed. Gallium scintigraphy is used as the reference method for the detection of multiple abscesses . Imaging procedures are also important for follow-up.
For the microbiological detection of pathogens, the gold standard for the definitive diagnosis of the disease is usually a puncture of abscesses or a biopsy of muscle tissue. Blood cultures are positive 5 to 30 percent of the time. A biopsy also enables the differential diagnosis of other muscle diseases and injuries such as osteomyelitis and polymyositis , hematomas and torn muscle fibers , deep vein thrombosis and trichinosis . The serum levels of the enzymes creatine phosphokinase and aldolase as markers of muscle damage are typically in the normal range; acute phase proteins such as C-reactive protein are usually just as increased as the rate of sedimentation . Leukocytosis and eosinophilia are frequently detectable in connection with pyomyositis .
pathology
Pathologically, in pyomyositis an edematous separation of the muscle fibers can be seen , followed by uneven cell dissolution (cytolysis) up to a complete necrotic decomposition of affected muscle areas, which can be detected in different degrees in each phase of the disease. The muscle fibers, whose transverse stripes can no longer be seen, are initially mainly surrounded by granulocytes and later by lymphocytes , plasma cells and macrophages . Pathogens phagocytosed by macrophages are also often detectable.
treatment
The is usually used to treat a pyomyositis surgical drainage of abscesses, optionally with the use of interventional radiology . An amputation of muscle affected areas is only necessary in rare cases. This treatment is accompanied by an intravenous administration of antibiotics , the selection of which depends on the identification of the pathogen as well as its grief status and the determination of its resistance . When diagnosed in the first phase of the disease, antibiotic therapy alone is usually promising. There are no established recommendations for the duration of the treatment; in most cases it is around three to four weeks and depends on the individual characteristics of the disease.
prevention
There are no established guidelines for prophylaxis for pyomyositis. The removal of symptom-free colonization of the nasal mucous membrane with Staphylococcus aureus , as is found in 25 to 30 percent of all people, by the topical application of mupirocin or the oral administration of rifampicin is recommended occasionally .
Prospect of healing
The prognosis of pyomyositis is very good, provided that the disease is recognized in the first or second phase and effective antibiotics are available against the causative agent. The mortality is 0.5 to two percent with timely diagnosis and appropriate treatment. Even with major muscle damage, the resulting permanent deformations and functional restrictions are usually minor.
A disease that is not recognized or recognized too late, or is untreated or progressing, is considered life-threatening; the mortality in these cases is around ten percent. The most common cause of death are septic complications, and the rupture of accompanying abscesses in internal organs and purulent pericarditis or endocarditis can also lead to death.
history

It was first described in 1852 by Virchow in his habilitation thesis under the name "Spontaneous acute myositis". A clinical picture was described with a high fever, chills, body aches, drowsiness, often even with delirium, which leads to death in a short time. He saw the cause in a "Materia peccans zu Blute" without specifying it. Gobée (1855) (Netherlands), Gay (1858) (England) and Gellé (1858) (France) independently described muscle abscesses. All of these cases were fatal. The disease became generally known after a description by the German surgeon Julius Scriba who worked in Japan and who reported 4 cases from Japan (1885). Around the same time as in Japan, reports about this clinical picture from tropical colonial areas (van Dorssen 1885) from Java (then: Dutch East Indies) appeared in Central Europe with increasing frequency. The current term "pyomyositis" is first used as "pyomyosite" by Commes (1918). The oldest report from North America comes from Mynter (1881) about an abscess of the psoas muscle. De Saliva (1866) reported an abscess of the rectus abdominalis muscle in tropical South America. Both cases could be cured by incision. As the spread of HIV / AIDS increased in the late 1980s, the number of reports of pyomyositis cases also increased in Western countries, although it is still considered a rare disease here.
literature
- HM Broich: "Pyomyositis" -A tropical S. aureus disease-? A review. Inaugural dissertation from the University of Cologne, 1991. (199 sources).
- F. Lanternier, N. Memain, O. Lortholary: Pyomyositis. In: Orphanet Encyclopedia . Published in March 2004, available online at Orphanet: Pyomyositis ( PDF file , approx. 85 KB)
- LN Small, JJ Ross: Tropical and Temperate Pyomyositis. In: Infectious Disease Clinics of North America. 19 (4 )/2005. Elsevier, pp. 981-989, ISSN 0891-5520
- NF Crum-Cianflone: Infectious myositis. In: Best Practice & Research Clinical Rheumatology . 20 (6) / 2006. Elsevier, pp. 1083-1097, ISSN 1521-6942
- S. Chauhan, S. Jain, S. Varma, SS Chauhan: Tropical pyomyositis (myositis tropicans): current perspective. In: Postgraduate Medical Journal. 80/2004. The Fellowship of Postgraduate Medicine, pp. 267-270, ISSN 0032-5473
- S. Schalinski, M. Tsokos: Pyomyositis. In: Forensic Medicine. 16 (3) / 2006. Springer, pp. 151-155, ISSN 0937-9819
- AK Argawal, S. Singla, A. Sirohi: Tropical Pyomyositis. In: AK Argawal: Clinical Medicine. A Practical Manual for Students and Practitioners. Jaypee Brothers Publishers, New Delhi 2007, ISBN 8-18-061928-1 , pp. 368-373
- J. Bickels, L. Ben-Sira, A. Kessler, S. Wientroub: Primary Pyomyositis. In: Journal of Bone and Joint Surgery (American). 84/2002. The Journal of Bone and Joint Surgery, Inc. & Stanford University Libraries' HighWire Press, pp. 2277-2286, ISSN 0021-9355
Web links
- Pyomyositis: MRI images MRI images of pyomyositis infections
- John G. Bartlett: Antibiotic Guide: Pyomyositis Information on the clinic, diagnosis and therapy of pyomyositis (English)