Q fever
| Classification according to ICD-10 | |
|---|---|
| A78 | Q fever |
| ICD-10 online (WHO version 2019) | |
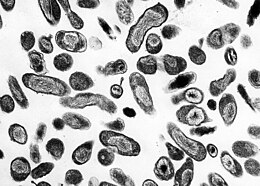
Q fever (from English query ) is a zoonosis ( disease transmitted from animals to humans ) caused by the strictly intracellular, gram-negative bacterium Coxiella burnetii , which usually causes flu-like symptoms. The pathogen can be a so-called permanent form ( spores ) z. B. survive in dust , on hay or on wool for years and remain infectious. In Germany, sheep in particular are carriers of the pathogen (through the droppings of the alluvial forest ticks ). It is usually transmitted by inhalationcontaminated dust. Person-to-person transmission only occurs in exceptional cases. The incubation period is 9 to 40 days. Q fever is a reportable disease in the Federal Republic of Germany according to the Infection Protection Act. Diseases of ruminants from Q fever are subject to reporting in Germany under the Animal Health Act.
Synonyms
Query fever (hence: Q fever), Queensland fever, Balkan flu, Balkan fever, Coxiellosis, Euboea fever, Crete fever, Crimean fever, pneumorickettsiosis, slaughterhouse fever, seven-day fever, desert fever, goat flu.
The disease known in English as "Australian tick typhus" or "Queensland tick typhus" ("Queensland tick bite fever") is - unlike Q fever (English also "queensland fever") - caused by rickettsiae ( Rickettsia australis ).
history
The disease was first observed among the slaughterhouse staff in Brisbane , Queensland , Australia in 1935 and scientifically described by Edward Holbrook Derrick in 1937 as a disease of unknown cause, which led to the name Q fever (from English query for "question" in the sense of "questionable", "Doubtful"). The bacterium was also isolated in 1937 by Frank Macfarlane Burnet and Mavis Freeman from one of Derrick's patients and identified as Rickettsia species ( Rickettsia burneti ). HR Cox and Gordon Davis isolated the pathogen in 1938 from ticks in Montana , USA, and described the route of transmission; the organism was officially recognized as Coxiella burnetii a few years later . Meanwhile, Coxiella burnetii is no longer considered a close relative of the rickettsiae.
Occurrence and occurrence
The pathogen occurs worldwide, except in New Zealand and the Antarctic . It is more common in Europe by triggering liver inflammation and in North America by pneumonia . The bacterium is extremely viable and extremely contagious ( infectious ): a single bacterium can cause an infection . The main carriers of the bacteria in Germany are sheep. It is transmitted to humans in particular through inhalation of the feces that have broken down to dust and are contaminated by parts containing pathogens . In addition, transmission through contact with contaminated products such as wool, milk or meat is possible.
Ticks, particularly the genus dermacentor ( Dermacentor belonging) marsh tick ( Dermacentor reticulatus ) can be the causative agent by biological transmission to other animals. Direct human-to-human transmission appears to be extremely rare and has only been described a few times.
Men are affected somewhat more often than women, which is probably related to the occupational exposure of people who are involved in animal breeding, milk processing and slaughtering.
In 2009, 2,300 people in the Netherlands contracted Q fever, 25 of whom died. To contain the spread, tens of thousands of symptom-free goats were culled around the turn of 2010/2011 .
According to the Robert Koch Institute , a total of 148 cases were registered in Germany in 2019, after 93 cases in 2018, 107 cases in 2017, 275 cases in 2016, 320 cases in 2015 and 262 cases in 2014.
Clinical manifestations
Symptoms in humans

In about half of the cases, the infection goes unnoticed or with only mild symptoms. The mostly flu-like appearance can be accompanied by sudden onset of fever , severe exhaustion, severe headache , myalgia (muscle pain), loss of appetite, dry cough , chest pain, chills, confusion and - less often - gastrointestinal symptoms such as nausea, vomiting and diarrhea . The mostly mild fever lasts about 7 to 14 days.
In the course of the disease, pneumonia ( atypical pneumonia ) can occur, which can result in life-threatening acute respiratory distress syndrome ( ARDS ). Any breathing-related symptoms usually appear early (4–5 days after the onset of the disease).
Q fever is a little less common than inflammation of the liver ( granulomatous hepatitis ) due to general exhaustion, fever , enlarged liver, pain in the right upper abdomen and jaundice ( jaundice ).
A meningitis may occur. In addition, reactivations occur during pregnancy or under immunosuppression.
The somewhat rarer chronic form of Q fever is practically identical to an inflammation of the inner skin of the heart ( endocarditis ) and the pericardium ( pericarditis ) caused by the bacterium , which is usually fatal if left untreated. The mortality (death rate) decreases with treatment at about ten percent.
Symptoms in animals
In cattle and sheep, Q fever usually runs without clear symptoms (subclinical), the most common symptoms are unwillingness to eat and miscarriages in late pregnancy. In addition, the infection can cause infertility and udder infections .
After experimental infection, cats develop fever, fatigue and unwillingness to eat for several days.
diagnosis
If the cause of the fever is unclear, Q fever can be used for differential diagnosis. An x-ray of the lungs can help make the diagnosis.
In a handout from the Robert Koch Institute for Doctors it says:
- “A clinical or clinical- epidemiological suspicion diagnosis can also be confirmed in laboratory diagnostics by means of serodiagnostic procedures by means of detection of antibodies (against Coxielle-Ag phase II as well as against phase I). In acute illness, antibodies are primarily formed against the phase II antigen; Anti-Phase I antibodies in high titers are typical of a chronic course. [...] In special laboratories, pathogens can also be detected using cell culture or nucleic acid detection ( PCR ). The pathogen can be detected in biopsy material by means of immunofluorescence or electron microscopy. C. burnetii is classified as a pathogen in safety level 3. "
therapy
The therapy of the acute form is usually successful and takes place in consultation with infectiologists with antibiotics . Antibiotics with intracellular activity are used, in particular tetracyclines (e.g. doxycycline ), macrolide antibiotics (e.g. clarithromycin ) and quinolone antibiotics (e.g. ciprofloxacin or levofloxacin ). The anti- malarial drug hydrochloroquine and chloramphenicol are also effective.
To treat the chronic form, a combination of two or three of the antibiotics mentioned is administered for a period of one to four years, depending on the author.
As a vaccine exists, particularly exposed persons such as veterinarians, slaughterhouse staff or laboratory workers could be vaccinated as a precaution. However, the Australian vaccine ( Q-Vax ) is not approved in Germany.
Use as a weapon
Due to the route of infection and the development of permanent forms, the spread of Q fever is a biological weapon that causes a forecast 23-77% failures with low mortality in military use and significantly influences the ability of the affected unit to act .
Q fever is easy to produce and has been found in examinations up to two kilometers from the source of infection. For military use - also in view of the estimated infectious dose of 1–10 organisms - distribution as an aerosol is particularly effective. According to one estimate, such a deployment of 50 kilograms of C. burnetii as a two-kilometer-long line in an affected city with 500,000 inhabitants would result in around 150 deaths and 125,000 incapacitated, around 9,000 of them with chronic consequences. In particular, these chronic consequences, as well as the effect on farm animals in the form of miscarriages and malformations and the resulting fear of consuming them, make the pathogen of Q fever a suitable bioterrorist substance due to the psychological effect of the following illness.
Q fever was listed as a possible weapons-grade pathogen in the US weapons program, which began in 1942 at Fort Detrick. In 1954 attempts were made on volunteers as part of Project Whitecoat . By the end of the biological weapons program in 1969/70, Q fever was probably in the active arsenal of the USA. Between 1950 and 1965, 50 virologists, bacteriologists and technicians working at Fort Detrick were infected with Q fever - only five of the infections came from known laboratory accidents. But defensive bioweapons research is still being carried out in the United States on Q fever today. In February 2006, an employee of the Bioweapons Research Laboratory at Texas A&M University was infected .
In Russia, C. burnetii was manufactured as a weapon before World War II, and production continued until at least 1990.
Q fever was initially considered bio-terrorist by Ōmu Shinrikyō . A possible attack took place in 1987 in Oxfordshire against the British Post Office . The origin of the pathogen was not discovered, but the carrier is suspected to be contaminated letters. This distribution route is a particular problem due to the high speed of modern sorting systems and the resulting wide distribution of the agent.
literature
- Robert Koch Institute : 'Q fever. RKI guide for doctors . May 1, 2012.
- Dietrich Falke : The blood count in guinea pigs infected with Queensland fever. Dissertation . Tübingen 1953.
- M. Maurin, D. Raoult: Q Fever. In: Clinical Microbiology Reviews. Volume 12, No. 4, October 1999, pp. 518-583. (Full text online)
- Coxiella burnetii - causative agent of Q (query) fever. In: Federal Health Gazette 2005. July 2005, pp. 814–821.
- Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , p. 224 f.
Web links
- Q fever - information from the Robert Koch Institute
- Information from the Federal Ministry of Education and Research on the Q-Fever research project
- Workshop on Q Fever (English, PDF, 474 KiB)
- The stroller plague on FAZ .NET
Individual evidence
- ↑ Annex to Section 1 of the Ordinance on Notifiable Animal Diseases (TKrMeldpflV) in the version published on February 11, 2011 ( Federal Law Gazette I p. 252 ), last amended by Article 381 of the Ordinance of August 31, 2015 ( Federal Law Gazette I p. 1474 )
- ↑ TJ Marrie: Coxiella burnetii pneumonia. In: European Respiratory Journal. Volume 21, 2003, pp. 713-719.
- ↑ Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 9-223, here: pp. 121 f.
- ↑ Q-coorts . Rijksinstituut voor Volksgezondheid en Milieu (Dutch); last accessed on August 31, 2014.
- ↑ goat flu: Netherlands cull 36,000 goats . On: zeit.de from December 17, 2009, last accessed on August 31, 2014.
- ↑ Goat culling started in Holland. . On: agrarheute.com from December 22, 2009, last accessed on August 31, 2014.
- ^ Robert Koch Institute: Epidemiological Bulletin . No. 3 from January 16, 2020 ( full text as PDF file ).
- ↑ Marianne Abele-Horn (2009), p. 224.
- ^ A b Merck Veterinary Manual: Q Fever . On: merckmanuals.com , March 2012 (last revision); last accessed on July 4, 2014.
- ^ RKI: Q fever: RKI advice for doctors . May 1, 2012, last accessed on August 31, 2014.
- ↑ About The Q Fever Vaccine . On: qfever.com.au Dump of October 5, 2012, last accessed on August 31, 2014.
- ↑ a b c d e M. G. Madariaga, K. Rezai, GM Trenholme, RA Weinstein: Q fever: a biological weapon in your backyard. In: The Lancet. 2003, Volume 3, No. 11, pp. 709-721, doi: 10.1016 / S1473-3099 (03) 00804-1 .
- ^ SR Klee, D. Jacob, H. Nattermann, B. Appel: Bioterroristically relevant bacterial pathogens . In: Federal Health Gazette - Health Research - Health Protection. tape 46 , no. 11 , 2003, p. 935-948 , doi : 10.1007 / s00103-003-0724-0 .
- ↑ Texas: Neglect for months in the biological weapons lab . On: spiegel.de , July 3, 2007, last accessed on August 31, 2014.