Myasthenia gravis
| Classification according to ICD-10 | |
|---|---|
| G70 | Myasthenia gravis and other neuromuscular diseases |
| G70.0 | Myasthenia gravis |
| ICD-10 online (WHO version 2019) | |
The myasthenia gravis (pseudoparalytica) (. From Greek mys "muscle" -asthenia "weakness", lat. Gravis "heavy" pseudo "wrong" and paralysis "paralysis"; symbol: MG ) belongs to a group of neurological disorders are characterized by a disturbed signal transmission between nerve and muscle and are summarized as disorders of neuromuscular impulse transmission or as myasthenic syndromes . It is an autoimmune disease in which there is a disorder in the motor end plate of the striated muscles (skeletal muscles), the cause of which has not yet been fully researched. The clinical picture of myasthenia gravis is characterized by a load-dependent muscle weakness that often affects the above-mentioned muscles asymmetrically , including single or multiple muscles, regardless of the half of the body. The main symptoms include their changing expression, for example, in addition to the change in affected muscles, they can often increase spontaneously during the day for no apparent reason, and / or the affected muscles can recover just as suddenly at rest.
Myasthenia gravis occurs in both humans and animals, especially domestic dogs .
An outdated term for the disease, which is no longer in use today, is Erb-Goldflam Syndrome .
Myasthenia gravis in humans
frequency
Myasthenia gravis is a relatively rare disease. The disease frequency (prevalence) is around 100 to 200 diseases per 1 million population. The disease can manifest itself at any age , but it has two peaks of manifestation. The first peak lies between the second and third decade of life with a preference for the female sex, the second peak between the sixth and eighth decade of life with a preference for the male sex. Myasthenia gravis is more common in women (ratio 3: 2). In North America and Europe, 10 to 14% of patients are younger than 10 years. The incidence of the disease has increased since the epidemiological surveys on this disease began around 1950; in the 1990s the incidence of the disease was about four times higher. This increase is attributed to the increasing awareness of the disease, better diagnostic procedures, the decrease in mortality and changes in the age structure of the population.
Cause and development of the disease
Myasthenia gravis is an autoimmune disease , which means that the body forms autoantibodies against the body's own structures. In myasthenia gravis, it is antibodies that are directed against structures of the postsynaptic membrane in the area of the neuromuscular endplate . By far the most common, in around 85% of cases, acetylcholine receptor antibodies are detectable, i.e. antibodies that are directed against the nicotinic acetylcholine receptor . Antibodies against muscle-specific tyrosine kinase (MuSK) can be detected in 1 to 10% of those affected and so-called low - affinity acetylcholine receptor antibodies or antibodies against lipoprotein receptor-related protein (LRP4) can be detected in some of those affected . In some of the patients who have a high probability of suffering from myasthenia gravis, no antibodies can be detected ( seronegative myasthenia gravis ).
It is assumed that there could be other myasthenia-relevant antibodies in addition to the antibodies mentioned. Only existing connections to myasthenia-relevant antibodies and the thymus and the causal basis of the disease, the disturbed signal transmission between nerve and muscle, are proven . The trigger for the fluctuating symptoms in environmental influences, infections, inflammations, emotional and psychological stress is also unclear.
Acetylcholine receptor antibodies
The interaction between the transmitter acetylcholine and its receptor is prevented or made more difficult by acetylcholine receptor antibodies. Therefore the electrical impulse (the action potential) can no longer be transferred from the nerve to the muscle, the muscle is not excited. In addition, the number of acetylcholine receptors is reduced, since the binding of the antibodies to the acetylcholine receptors causes them to be broken down by immune activity. The structure of the subsynaptic membrane breaks down into fragments. By endocytosis a car created phagosome . Transport vesicles containing digestive enzymes fuse with the autophagosomes. The acetylcholine receptors are broken down every two to three days by this immune reaction. The structure of the motor end plates is changed. The sub-synaptic folds become shallower and the synaptic gap becomes wider. As a result, the acetylcholine diffuses when it is released from the synaptic gap or it is hydrolyzed by the enzyme cholinesterase before it can occupy an acetylcholine receptor.
Importance of the thymus
In myasthenia gravis, pathological changes in the thymus can very often be detected. The thymus is assigned a crucial role in the development of the autoimmune process. In up to 70% of cases, thymitis (lymphofollicular hyperplasia) with active germinal centers is noticeable. A thymoma is detectable in 10–15% of those affected . Under certain circumstances, surgical removal of the thymus can have a positive effect on the course of the disease. An indication for surgery should be made at any age.
Clinical manifestations
Performance is best in the morning and after breaks, but after a few repetitive movements, various muscles or entire muscle groups are exhausted. Often the symptoms appear more pronounced in the evening. Small muscles in particular are affected by the paralysis or initially only restricted mobility, but in principle all striated (arbitrarily movable) muscles can be affected.
Muscle tissues without motor endplates, such as the heart muscle and smooth muscles , are not affected by the disease. However, the participation of the latter has never been scientifically ruled out. An indication of their involvement could be the effectiveness of the pyridostigmine- based myasthenia drugs on bowel function, since the bowel (except for the voluntary sphincter muscles) is made up of smooth muscles. Another indication could be the bowel-induced constipation , which is one of the symptoms of the also autoimmune-caused suspected Lambert-Eaton-Rooke syndrome (LEMS).
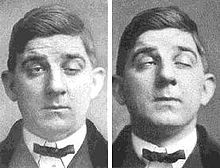
In around 50% of cases, myasthenia gravis first becomes noticeable in the eyes , eyelids and / or the external eye muscles : When the eyelid lifter muscles get tired, the typical "bedroom look" ( ptosis ) occurs because the eyelids can no longer be held up. Patients tilt their heads back so that they can look under the lids. Typical early symptoms are therefore ptosis and diplopia (double vision ) or an inability or impossible to close one or both eyelids. In this context, the “Signe des cils” ( cilia mark) refers to the fact that the eyelashes remain visible when the eyelashes are weakly closed (also observed with peripheral facial paralysis ). Other muscle groups typically affected at an early stage are the facial muscles , the mouth and tongue muscles ("laughing" rigid face, slurred or impossible speech), the neck and neck muscles (weak head posture), the chewing and throat muscles (swallowing disorders up to the inability to Swallowing saliva). As you progress, the arms are more affected than the legs in most cases. Furthermore, the respiratory muscles can be so severely impaired that those affected can only sleep while sitting or have to be ventilated at an advanced stage. The swallowing muscles can also be so severely affected that a supportive or complete supply via a gastric tube is indicated.
Impairment of balance, degenerative memory, or impaired sensation are not signs of MG.
Regarding the characteristics of the symptoms, it can be said that they are variable, not static and rigid; changing both with regard to the time, the triggering strength of the load and the "selection" of currently affected muscles or muscle groups - e.g. B. left hand right eye, once together, once individually or in the morning or in the evening. The symptoms are unpredictable and usually "break in" suddenly. Some muscles or muscle groups are only restricted in their mobility, while others may lack all the strength to move them at all. Since this variability of the course is so varied in an individual affected person or in a comparison from patient to patient, one cannot actually speak of a general clinical picture (manifestation).
A distinction is made between types and progressive forms:
Types of manifestation
- Ocular MG
- Generalized MG
- MG in childhood (EOMG - Early Onset MG)
- Age MG (LOMG - Late Onset MG)
Gradient forms
- “Classic” AChR antibody MG
- MuSK antibody positive MG
- Kv1.4 antibody positive MG, a potassium channel antibody
- MG with the involvement of other antibodies such as B. MGT30 or RyR
- Seronegative MG, i.e. without antibody involvement
- Age MG, with more common titin antibodies
- MG in childhood with more frequent cases of undetectable antibodies
- Neonatal MG in the newborn
Initial symptoms
- Over 50% starting with ocular symptoms (e.g. weak eyelids and / or double vision)
- About 14% starting with swallowing and speaking disorders
- Around 8% starting with weak arms or legs (e.g. unclear foot lifter paresis)
- Very rare onset of the trunk and spinal muscles
Complications
The acute failure of the respiratory muscles is life-threatening in a crisis. This acute worsening of symptoms with breathing problems is called a “myasthenic crisis” or, in the case of an overdose of cholinesterase inhibitors such as pyridostigmine, a “cholinergic crisis”. The emergency aid card, which describes medical measures and contact persons, is very helpful here. (ID cards are issued by the "German Myasthenia Society" or by the relevant pharmaceutical manufacturers). In the case of both crises, rapid admission and competent treatment in an intensive care unit are required, since the mortality rate is still quite high (according to literature 4–13%).
Ingestion (swallowing disorder) can lead to severe pneumonia , an aspiration pneumonia .
Symptom aggravating are:
- Infections, inflammations, fever, heat, vibrations
- Intercurrent diseases (thyroid)
- extreme stress (mental, physical)
- also loads such as anesthesia, especially when choosing myasthenia-contraindicated narcotics
- hormonal fluctuations
- Incorrect treatment or dosing in drug therapy (too much or too little, which also varies symptomatically)
- Various drugs (myasthenia-contraindicated painkillers, antibiotics, psychotropic drugs, hormone products, X-ray contrast media, etc.)
A not inconsiderable complication also arises from the fact that the diagnosis MG is made very late (statistically after 2.7 years). Due to the variability of the symptoms mentioned as well as the initially weak expression of symptoms, these are often overlooked or misinterpreted, so that considerable diagnostic misunderstandings and misdiagnoses can even occur. On the one hand, this means an additional worsening of symptoms for those affected due to the lack of urgent drug treatment and an additional psychological burden due to the frequent odyssey through medical facilities.
Investigation methods
The diagnosis is made primarily on the basis of the clinical picture in connection with the detection of disease-specific autoantibodies, the response to myasthenic symptoms after administration of acetylcholinesterase inhibitors and with the help of electrophysiological examinations. Depending on the severity of the disease, MG is divided into different stages (according to Osserman and Genkins):
| stage | designation | affected body regions |
|---|---|---|
| I. | purely ocular myasthenia gravis | eye muscles only |
| IIa | slight generalization | hole body |
| IIb | moderate generalization | hole body |
| III | severe acute generalization | whole body with respiratory muscles |
| IV | severe chronic generalization |
The Besinger score is used to assess clinical progress.
Individual examination methods are:
- Simpson test (in connection with the Tensilon test , eyelid fatigue when looking up for a longer period of time, which temporarily disappears after administration of Tensilon)
- Detection of eye muscle imbalance disorders with double vision
- Intensive stress tests of various muscle groups that go beyond the “normal level” of standard neurology - a prerequisite for creating a meaningful MG score
- Prostigmintest, Tensilon-Test (temporary disappearance of symptoms after intravenous injection of Tensilon), indicative for a neurotransmitter disease, but not specific for MG
- Ice pack test; Similar to the drug test just mentioned, an ice compress, e.g. B. on a difficult to close or drooping eyelid to alleviate the symptom. If the cold affects the symptom, this is a guideline.
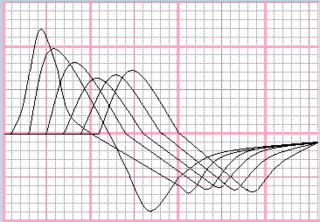
- Repetitive series stimulation of individual nerves (RSN) - electrophysiological test in which a decrement can be detected in those affected under the artificial simulation (imitation) of muscle stress.
- Single fiber EMG - similar to the electrophysiological stimulation, but very complex and no detection possible in the case of seronegative MG
- Electromyography (decrement sign - decrease in the amplitude of the evoked stimulus response potentials in the success muscle)
- Histological evidence of lymphoid cells in muscle biopsies
- Laboratory diagnostics - detection of acetylcholine receptor antibodies and / or anti-MuSK antibodies in the blood
- Exercise tests as part of swallowing diagnostics by speech therapists with experience of myasthenia , using a video endoscopy and / or imaging swallowing study
- Imaging diagnostics (CT with contrast agent) of the lung region around the thymus
- ↑ a b Decrement - Special decreasing shape (saddle shape) of an amplitude from which a removable muscle load capacity can be read. The opposite increment is a special increasing form of amplitude. If this is shown in a series stimulation, a LEMS (Lambert-Eaton Myasthenes Syndrome) should be considered for differential diagnosis in addition to myasthenia gravis. A test for calcium channel antibodies (VGCC-AK) should then be considered. Like MG, LEMS is a muscle-weakening disease.
With regard to laboratory diagnostics, it should be noted that in 50% of the ocular and about 10–15% of the generalized cases no AChR-Ab and in half of these cases no MuSK-Ab or other antibodies can be detected. It is then a seronegative MG . Here, too, diagnosis is more difficult and neurologists with experience of myasthenia must be assessed on the basis of the course.
Regarding the electrophysiological examinations, it should be said that a certain amount of experience is necessary for diagnostics. Sources of error include muscles that have not been examined enough, muscles that are too cold and / or muscles that are under-stressed by the examiner or only actuated by the patient during the examination, as well as a lack of knowledge, e.g. B. regarding the timely discontinuation (if medically justifiable) of influencing drug therapies (e.g. pyridostigmine, the cholinesterase inhibitors). Also, only a marginal decrement (7–9%) at the first moment, after another 2 and 5 minutes post-tetanic measurement, can be assessed as pathological.
Differential diagnostics
In relation to myasthenia gravis, the following are to be excluded in particular:
- Lambert-Eaton-Rooke Syndrome (LEMS)
- Amyotrophic lateral sclerosis (ALS)
- Multiple sclerosis (MS)
- More general muscle weaknesses caused by e.g. B. anorexia , cachexia or other mental, psychiatric or neurological diseases
- Brain diseases, circulatory disorders, metabolic disorders
or special forms to be defined manifest themselves:
- neonatal myasthenia (newborns)
- myasthenic symptoms caused by drugs, boreol or poisons
- congenital myasthenic syndrome
therapy
In the medical treatment of myasthenia gravis, three therapeutic principles can be distinguished. Surgical removal of the thymus can influence the course of the disease.
The therapy with acetylcholinesterase inhibitors serves to improve the neuromuscular impulse transmission. They inhibit the enzyme acetylcholinesterase and thus the breakdown of acetylcholine in the synaptic gap. This increases both the temporal availability and the concentration of acetylcholine in the synaptic gap. Accordingly, the acetylcholine receptors located in the postsynaptic position remain occupied for longer and are activated for longer. The myasthenic symptoms respond variably to therapy with acetylcholinesterase inhibitors. While the weakness of the extremity muscles often improves significantly, eye muscles, for example, often do not respond well to therapy.
The active ingredients pyridostigmine bromide are used for oral administration and ambenium chloride for the rare bromine intolerance . Neostigmine and pyridostigmine are available for intravenous use . The therapy with acetylcholinesterase inhibitors is a purely symptomatic therapy that cannot influence the course of the disease or the prognosis of the disease. Important side effects of therapy with acetylcholinesterase inhibitors are excessive sweating and muscle cramps. With high doses there is a risk of a cholinergic crisis , so that a dose of 600 mg should only be exceeded in exceptional cases.
Immunosuppressive treatment with glucocorticoids or azathioprine can weaken the effect of the antibodies. If the course is severe or critical, plasmapheresis or high-dose immunoglobulin doses are used.
There is also the option of surgically removing the thymus or a thymoma ( thymectomy ). It may be necessary to switch to food that is less hazardous to aspiration, preventive swallowing therapy and, in severe cases, nutrition via PEG ( gastric tube), secretion suction apparatus and / or tracheostomy (→ tracheotomy ). If double images remain constant in ocular myasthenia, an ophthalmologist-measured prismatic lens in glasses or a prismatic film that can be sucked or glued onto the glass of existing glasses by means of a water film will compensate for this.
Course and prospect of recovery
If only the eye muscles are affected, the prognosis is good and manageable with drug therapy. The spread to the whole body (generalization), however, was incurable a few years ago. Thanks to modern drugs, the prognosis in these cases has improved significantly in recent years. But that means lifelong medication. Further measures such as B. mentioned PEG or tracheostoma have a life-prolonging effect, but can mean a considerable loss of quality of life. If the diagnosis is too late or not made at all, the course of the disease is severe and the crisis (see complications), the lifespan can be shortened.
Thymectomy often leads to a decrease in symptoms, especially in young patients. In this case, a few years after the thymus has been removed, it may be possible to discontinue the immunosuppressive medication and thus a clear improvement can be seen, sometimes a remission is achieved.
history
Myasthenia gravis has been known to humans since the 17th century. The first documented case from 1644 was found in the British colonial mail from North America . There it is described how the Indian chief Opechankanough could no longer walk due to a sudden weakness. The first detailed medical description of cases with myasthenic main symptoms in the form of speech disorders , double vision and rapid fatigue followed a few years later in 1672 by the Oxford doctor Thomas Willis in the Latin “De Anima Brutorum” . However, Willis' work went unnoticed in medical science for over 200 years or was not followed by any further verifiable observation of myasthenic symptoms.
It was not until 1877 that the London doctor Samuel Wilks wrote the next case report of a girl with a speech disorder and referred to the disease as bulbar paralysis . The first German-language report was published in 1879 by Wilhelm Erb, who worked at the Heidelberg Friedreich Clinic , with the work “On the casuistry of bulbar paralysis” in three patients. Hermann Oppenheim , a neurologist from the Berlin Charité , presented a case in 1887. In 1893 Samuel Goldflam followed in Warsaw with the most comprehensive publication to date. Hence the (outdated) name Erb-Goldflam-Syndrome . Unfortunately, even then, myasthenic symptoms were often misinterpreted as a sign of a neurotic disease, hysteria , similar to how it is confused with psychosomatic symptoms up to the present day .
Friedrich Jolly carried out demonstrative electrophysiological examinations and in 1895 coined the name " Myasthenia gravis pseudoparalytica ", which is still common today, with his work of the same name . After the first new knowledge about the connection with the thymus at the beginning of the 20th century, Sauerbruch carried out the first thymectomy in 1912 .
The first successful drug attempts to treat myasthenia gravis were made by two doctors. Harriet Edgeworth from the United States, herself affected by myasthenic symptoms , found that ephedrine improved her muscle strength. In 1933, after a first, she published a more comprehensive second report on her long-term experiments. A year later in 1934, the British Mary Broadfoot Walker , who worked at St. Alfege's Hospital in Greenwich , published the article Treatment of Myasthenia gravis with physostigmine . In it she described the observation that the symptoms of myasthenia gravis are similar to poisoning with the poison curare. This can be treated with cholinesterase inhibitors. This is the most effective drug therapy to date. The active ingredient is pyridostigmine . Walker found and thus proved an indication of a disturbed transmission between nerve and muscle. This causal relationship was only proven experimentally after 1960.
As early as 1960, John Alexander Simpson hypothetically pointed to an autoimmune pathogenesis . The AChR antibodies were only detected in 1974. MuSK antibodies were first described in 2001.
Myasthenia gravis in animals
Myasthenia gravis occurs primarily in domestic dogs (also in cats or farm animals ). A distinction is made here between an innate and an acquired form. The pathogenesis is the same as in humans, i.e. an autoimmune disease that is directed against the acetylcholine receptors. Treatment is the same as for humans.
Congenital myasthenia gravis
Congenital myasthenia gravis is relatively rare and occurs more frequently in some dog breeds ( Jack Russell Terrier , Smooth-haired Fox Terrier , Springer Spaniel ). The disease is autosomal - recessive inherited and typically occurs in 6 to 8 weeks of age.
Acquired myasthenia gravis
Acquired myasthenia gravis is more common and presumably multifactorial, although there is also a genetic predisposition. Thymomas are also possible triggers. Age predisposition is two-phase, with a maximum frequency in young dogs (1-4 years of age) and one in old dogs (from 9 years of age).
Clinically, it mostly manifests itself in local muscle disorders. Often (about 80% of cases) the esophagus is primarily affected and a megaesophagus develops . Clinically, regurgitation is frequent . Here there is a particularly high risk of aspiration pneumonia . The throat muscles can also be involved, which manifests itself in voice changes. A third common location is, like in humans, the eye muscles. In this case, the blink reflex is reduced and quickly fatigued. The generalized form manifests itself in quick fatigue, stiff gait up to paraparesis of the hind limbs or tetraparesis . Megaesophagus is also common. A myasthenic crisis with acute para- or tetraparesis and megaesophagus can also occur.
The diagnosis can only be made reliably with the detection of the autoantibodies. In a megaesophagus or thymoma one can x-ray of the chest provide important information. Other polyneuropathies , botulism (rarely in dogs), polymyositis , tick paralysis (rarely) and acetylcholine or organophosphate poisoning must be excluded from the differential diagnosis ( see also VETAMIN D ).
literature
- Diagnosis and therapy of myasthenia gravis and Lambert-Eaton syndrome. In: Guidelines for Diagnostics and Therapy in Neurology. Published by the "Guidelines" commission of the German Society for Neurology . 5th edition. Thieme Verlag , 2012, ISBN 978-3-13-132415-3 .
- S1 guidelines for myasthenia gravis and Lambert-Eaton syndrome, diagnostics and therapy of the German Society for Neurology (DGN). In: AWMF online (as of 2012)
- VC Juel, JM Massey: Myasthenia gravis. In: Orphanet Journal of Rare Diseases. Volume 2, 2007, p. 44, ISSN 1750-1172 . doi: 10.1186 / 1750-1172-2-44 . PMID 17986328 . PMC 2211463 (free full text). (Review).
- BM Conti-Fine, M. Milani, HJ Kaminski: Myasthenia gravis: past, present, and future. In: The Journal of clinical investigation. Volume 116, Number 11, November 2006, pp. 2843-2854, ISSN 0021-9738 . doi: 10.1172 / JCI29894 . PMID 17080188 . PMC 1626141 (free full text). (Review).
- M. Hohenegger: General anesthesia for myasthenia gravis. In: intense. 2006; 14, pp. 72-75.
- Wolfgang Koehler Myasthenia Gravis . Uni-Med Verlag, Bremen 2000-2008, ISBN 978-3-8374-1042-6 .
Individual evidence
- ↑ Wolfgang Köhler, Chapter Introduction and Clinic in: Myasthenia Gravis. Uni-Med Verlag AG. Bremen, 2000–2008, ISBN 978-3-8374-1042-6 , pp. 19 and 26ff.
- ^ LH Phillips: The epidemiology of myasthenia gravis. In: Semin Neurol. 2004 Mar; 24 (1), pp. 17-20. PMID 15229788 In: Shawn J Bird: Clinical manifestations of myasthenia gravis . UpToDate version 17.2 (2009).
- ↑ Claus Werner Wallesch: Neurology: Diagnostics and therapy in clinic and practice. Elsevier, 2005, ISBN 3-437-23390-4 , p. 841.
- ↑ J. Dörr, F. Zipp: Myasthenia gravis: Current aspects of pathogenesis, diagnosis and therapy. In: Neurology. 2007; 26, pp. 587-595 Summary ( Memento of October 17, 2013 in the Internet Archive ).
- ↑ NE Gilhus: myasthenia and the neuromuscular junction. In: Current Opinion in Neurology . Volume 25, Number 5, October 2012, pp. 523-529, ISSN 1473-6551 . doi: 10.1097 / WCO.0b013e3283572588 . PMID 22892950 .
- ↑ Myasthenia gravis and Lambert-Eaton syndrome, diagnosis and therapy . S1 guidelines of the German Society for Neurology (DGN), p. 6, as of September 2014. PDF version
- ↑ Wolfgang Köhler, ibid.
- ^ Myasthenia gravis and myasthenic syndromes (2nd part): Therapy. (PDF; 176 kB) Retrieved October 17, 2013 .
- ^ Andrew G. Engel, Myasthenia Gravis and Myasthenic Disorders. Oxford University Press, New York, 2012, ISBN 978-0-19-973867-0 , pp. 156-173.
- ↑ Christian Bischoff u. a .: The EMG book and peripheral neurology in question and answer. Georg-Thieme-Verlag, 2005, ISBN 3-13-110342-6 , p. 288 ff.
- ↑ David Buchholz et al. a .: Swallowing disorders - diagnostics and rehabilitation. Elsevier, 2006, ISBN 3-437-47160-0 .
- ↑ Martin Stangel, Mathias Mäurer: Autoimmune diseases in neurology. Diagnostics and therapy. Springer Verlag, 2012, ISBN 978-3-642-20476-0 , p. 174.
- ^ Shawn J Bird: Treatment of myasthenia gravis . UpToDate version 21.8, 2013.
- ^ J. Sieb: Myasthenia and Myasthenic Syndromes: What's New? In: Clinical Neurophysiology. 43, 2012, pp. 177-187, doi: 10.1055 / s-0032-1305253 .
- ↑ Helen C. Rountree: Pocahontas, Powhatan, Opechancanough: Three Indian Lives Changed by Jamestown. University of Virginia Press, Charlottesville 2005, ISBN 0-8139-2596-7 .
- ^ The effect of Ephedrine in the treatment of Myasthenia gravis: Second Report. In: Journal of American Medical Association (JAMA). 1933. Volume 100 Number 18, p. 1401.
- ^ Mary Broadfoot Walker: Treatment of Myasthenia Gravis with Physostigmine. In: The Lancet. Medical Journal of Reed Elsevier Properties SA Oxford, 1934. No. 1, pp. 1200-1201.
- ↑ RM Pascuzzi: The history of myasthenia gravis. In: Neurologic clinics. Volume 12, Number 2, May 1994, pp. 231-242, ISSN 0733-8619 . PMID 8041339 .
- ^ T. Hughes: The early history of myasthenia gravis. In: Neuromuscular disorders: NMD. Volume 15, Number 12, December 2005, pp. 878-886, ISSN 0960-8966 . doi: 10.1016 / j.nmd.2005.08.007 . PMID 16289896 . (Review).
- ^ W. Hoch, J. McConville et al. a .: Auto-antibodies to the receptor tyrosine kinase MuSK in patients with myasthenia gravis without acetylcholine receptor antibodies. In: Nature medicine. Volume 7, Number 3, March 2001, pp. 365-368, ISSN 1078-8956 . doi: 10.1038 / 85520 . PMID 11231638 .