Tuberculosis: Difference between revisions
→Transmission: restored fact that is well-supported (in discussion with SandyGeorgia) - I will continue to look for a good source |
ER |
||
| Line 1: | Line 1: | ||
{{Short description|Infectious disease}} |
|||
{{Infobox_Disease | |
|||
{{Good article}} |
|||
Name = Tuberculosis | |
|||
{{Pp-semi-indef}} |
|||
Image = Tuberculosis-x-ray-1.jpg | |
|||
{{Pp-move-indef}} |
|||
Caption = Chest [[X-ray]] of a patient suffering from tuberculosis | |
|||
{{Use dmy dates|date=January 2023}} |
|||
DiseasesDB = 8515 | |
|||
{{cs1 config|name-list-style=vanc|display-authors=6}} |
|||
ICD10 = {{ICD10|A|15||a|15}}-{{ICD10|A|19||a|15}} | |
|||
{{Infobox medical condition (new) |
|||
ICD9 = {{ICD9|010}}-{{ICD9|018}} | |
|||
| name = Tuberculosis |
|||
| image = Tuberculosis-x-ray-1.jpg |
|||
| caption = [[Chest radiograph|Chest X-ray]] of a person with advanced tuberculosis: Infection in both lungs is marked by white arrow-heads, and the formation of a cavity is marked by black arrows. |
|||
MedlinePlus = 000077 | |
|||
| field = [[Infectious disease (medical specialty)|Infectious disease]], [[pulmonology]] |
|||
MedlinePlus_mult = {{MedlinePlus2|000624}} | |
|||
| synonyms = Phthisis, phthisis pulmonalis, consumption, great white plague |
|||
eMedicineSubj = med | |
|||
| symptoms = [[Chronic cough]], [[fever]], [[hemoptysis|cough with bloody mucus]], weight loss<ref name=WHO2015Fact/> |
|||
eMedicineTopic = 2324 | |
|||
| onset = |
|||
eMedicine_mult = {{eMedicine2|emerg|618}} {{eMedicine2|radio|411}} | |
|||
| duration = |
|||
| causes = ''[[Mycobacterium tuberculosis]]''<ref name=WHO2015Fact/> |
|||
MeshNumber = C01.252.410.040.552.846 | |
|||
| risks = Smoking, [[HIV/AIDS]]<ref name=WHO2015Fact/> |
|||
}} |
|||
| diagnosis = [[Chest X-ray|CXR]], [[microbial culture|culture]], [[tuberculin skin test]], [[QuantiFERON]]<ref name=WHO2015Fact/> |
|||
| differential = [[Pneumonia]], [[histoplasmosis]], [[sarcoidosis]], [[coccidioidomycosis]]<ref>{{cite book | vauthors = Ferri FF |title=Ferri's differential diagnosis : a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders|date=2010|publisher=Elsevier/Mosby|location=Philadelphia, PA|isbn=978-0-323-07699-9|page=Chapter T|edition=2nd}}</ref> |
|||
| prevention = Screening those at high risk, treatment of those infected, [[vaccination]] with [[bacillus Calmette-Guérin]] (BCG)<ref name=Haw2014/><ref name=TBCon2008/><ref name=Harr2013/> |
|||
| treatment = [[Antibiotic]]s<ref name=WHO2015Fact/> |
|||
| medication = |
|||
| frequency = 25% of people (latent TB)<ref name=WHO2018Fact/> |
|||
| deaths = 1.3 million (2022)<ref name=WHO2018Fact/> |
|||
}} |
|||
'''Tuberculosis''' ('''TB'''), also known colloquially as the "'''white death'''", or historically as '''consumption''',<ref name=Cha1998>{{cite book|title=The Chambers Dictionary.|year=1998|publisher=Allied Chambers India Ltd.|location=New Delhi|isbn=978-81-86062-25-8|page=352|url=https://books.google.com/books?id=pz2ORay2HWoC&pg=RA1-PA352|url-status=live|archive-url=https://web.archive.org/web/20150906201311/https://books.google.com/books?id=pz2ORay2HWoC&pg=RA1-PA352|archive-date=6 September 2015}}</ref> is an [[infectious disease]] usually caused by ''[[Mycobacterium tuberculosis]]'' (MTB) [[bacteria]].<ref name=WHO2015Fact/> Tuberculosis generally affects the [[lung]]s, but it can also affect other parts of the body.<ref name=WHO2015Fact/> Most infections show no symptoms, in which case it is known as [[latent tuberculosis]].<ref name=WHO2015Fact/> Around 10% of latent infections progress to active disease which, if left untreated, kill about half of those affected.<ref name=WHO2015Fact/> Typical symptoms of active TB are chronic [[cough]] with [[hemoptysis|blood-containing]] [[sputum|mucus]], [[fever]], [[night sweats]], and [[weight loss]].<ref name=WHO2015Fact/> [[Infection]] of other organs can cause a wide range of symptoms.<ref name=ID10>{{cite book | vauthors = Adkinson NF, Bennett JE, Douglas RG, Mandell GL |title=Mandell, Douglas, and Bennett's principles and practice of infectious diseases|year=2010|publisher=Churchill Livingstone/Elsevier|location=Philadelphia, PA|isbn=978-0-443-06839-3|page=Chapter 250|edition=7th}}</ref> |
|||
Tuberculosis is [[Human-to-human transmission|spread from one person to the next]] [[Airborne disease|through the air]] when people who have active TB in their lungs cough, spit, speak, or [[sneeze]].<ref name=WHO2015Fact/><ref name=CDC2012B>{{cite web|title=Basic TB Facts|url=https://www.cdc.gov/tb/topic/basics/default.htm|publisher=[[Centers for Disease Control and Prevention]] (CDC)|access-date=11 February 2016|date=13 March 2012|url-status=live|archive-url=https://web.archive.org/web/20160206032136/http://www.cdc.gov/tb/topic/basics/default.htm|archive-date=6 February 2016}}</ref> People with latent TB do not spread the disease.<ref name=WHO2015Fact/> Active infection occurs more often in people with [[HIV/AIDS]] and in those who [[Tobacco smoking|smoke]].<ref name=WHO2015Fact/> [[Diagnosis]] of active TB is based on [[chest X-ray]]s, as well as [[microscopic]] examination and [[microbiological culture|culture]] of body fluids.<ref name=AP/> Diagnosis of latent TB relies on the [[Mantoux test|tuberculin skin test]] (TST) or blood tests.<ref name=AP>{{cite journal | vauthors = Konstantinos A |year=2010 |title=Testing for tuberculosis |journal=Australian Prescriber |volume=33 |issue=1 |pages=12–18 |doi=10.18773/austprescr.2010.005 |doi-access=free }}</ref> |
|||
'''Tuberculosis''' (abbreviated as '''TB''' for ''tubercle bacillus''<!-- Do not link to the genus [[Bacillus]] -->) is a common and deadly [[infectious disease]] caused by [[mycobacterium|mycobacteria]], mainly ''[[Mycobacterium tuberculosis]]''. Tuberculosis most commonly attacks the lungs (as [[Lung|pulmonary]] TB) but can also affect the [[central nervous system]], the [[lymphatic system]], the [[circulatory system]], the [[genitourinary system]], [[bone]]s, [[joint]]s and even the [[skin]]. Other mycobacteria such as ''[[Mycobacterium bovis]]'', ''[[Mycobacterium africanum]]'', ''[[Mycobacterium canetti]]'', and ''[[Mycobacterium microti]]'' can also cause tuberculosis, but these species do not usually infect healthy adults.<ref name="Harrison">{{cite book | author = Raviglione MC, O'Brien RJ | chapter = Tuberculosis | title = Harrison's Principles of Internal Medicine | editor = Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, Isselbacher KJ, eds. | edition = 16th ed. | publisher = McGraw-Hill Professional | year = 2004 | pages = 953–66 | doi =10.1036/0071402357 | isbn = 0071402357 }}</ref> |
|||
Prevention of TB involves screening those at high risk, early detection and treatment of cases, and [[vaccination]] with the [[bacillus Calmette-Guérin]] (BCG) vaccine.<ref name=Haw2014>{{cite journal | vauthors = Hawn TR, Day TA, Scriba TJ, Hatherill M, Hanekom WA, Evans TG, Churchyard GJ, Kublin JG, Bekker LG, Self SG | title = Tuberculosis vaccines and prevention of infection | journal = Microbiology and Molecular Biology Reviews | volume = 78 | issue = 4 | pages = 650–71 | date = December 2014 | pmid = 25428938 | pmc = 4248657 | doi = 10.1128/MMBR.00021-14 }}</ref><ref name=TBCon2008>{{cite book |title=Implementing the WHO Stop TB Strategy: a handbook for national TB control programmes|date=2008|publisher=[[World Health Organization]] (WHO)|location=Geneva|isbn=978-92-4-154667-6|page=179|url=https://books.google.com/books?id=EUZXFCrlUaEC&pg=PA179|access-date=17 September 2017|archive-date=2 June 2021|archive-url=https://web.archive.org/web/20210602232631/https://books.google.com/books?id=EUZXFCrlUaEC&pg=PA179|url-status=live}}</ref><ref name=Harr2013>{{cite book|vauthors=Harris RE|chapter=Epidemiology of Tuberculosis|title=Epidemiology of chronic disease: global perspectives|date=2013|publisher=Jones & Bartlett Learning|location=Burlington, MA|isbn=978-0-7637-8047-0|page=682|chapter-url=https://books.google.com/books?id=KJLEIvX4wzoC&pg=PA682|access-date=17 September 2017|archive-date=7 February 2024|archive-url=https://web.archive.org/web/20240207093803/https://books.google.com/books?id=KJLEIvX4wzoC&pg=PA682#v=onepage&q&f=false|url-status=live}}</ref> Those at high risk include household, workplace, and social contacts of people with active TB.<ref name=TBCon2008/> Treatment requires the use of multiple [[antibiotic]]s over a long period of time.<ref name=WHO2015Fact/> [[Antibiotic resistance]] is a growing problem, with increasing rates of [[multi-drug-resistant tuberculosis|multiple drug-resistant tuberculosis]] (MDR-TB).<ref name=WHO2015Fact/> |
|||
Over one-third of the world's population now carries the TB bacterium, and new infections occur at a rate of one per second.<ref name="WHO2004data">[[World Health Organization]] (WHO). [http://www.who.int/mediacentre/factsheets/fs104/en/index.html Tuberculosis Fact sheet N°104 - Global and regional incidence.] March 2006, Retrieved on 6 October 2006.</ref> Not everyone infected develops the full-blown disease, so [[asymptomatic]], latent TB infection is most common. However, one in ten latent infections will progress to active TB disease, which, if left untreated, kills more than half of its victims. |
|||
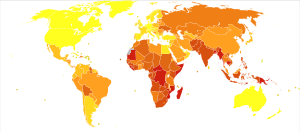
In 2018, one quarter of the world's population was thought to have a latent infection of TB.<ref name=WHO2018Fact>{{cite web |title=Tuberculosis (TB) |url=https://www.who.int/en/news-room/fact-sheets/detail/tuberculosis |publisher=[[World Health Organization]] (WHO) |access-date=15 September 2018 |date=16 February 2018 |archive-date=30 December 2013 |archive-url=https://web.archive.org/web/20131230232509/http://www.who.int/mediacentre/factsheets/fs104/en/index.html |url-status=live }}</ref><!-- Quote = About one-quarter of the world's population has latent TB --> New infections occur in about 1% of the population each year.<ref name=WHO2002>{{cite web|title=Tuberculosis|url=https://www.who.int/mediacentre/factsheets/who104/en/print.html|publisher=World Health Organization (WHO)|year=2002|url-status=dead|archive-url=https://web.archive.org/web/20130617193438/http://www.who.int/mediacentre/factsheets/who104/en/print.html|archive-date=17 June 2013}}</ref> In 2022, an estimated 10.6 million people developed active TB, resulting in 1.3 million deaths, making it the second leading [[List of causes of death by rate|cause of death from an infectious disease]] after [[COVID-19]].<ref name="WHO2020">{{cite web | title=Tuberculosis (TB) | website=WHO | url=https://www.who.int/news-room/fact-sheets/detail/tuberculosis | access-date=16 October 2021 | archive-date=30 July 2020 | archive-url=https://web.archive.org/web/20200730165218/https://www.who.int/news-room/fact-sheets/detail/tuberculosis | url-status=live }}</ref> As of 2018, most TB cases occurred in the regions of South-East Asia (44%), Africa (24%), and the Western Pacific (18%), with more than 50% of cases being diagnosed in seven countries: India (27%), China (9%), Indonesia (8%), the Philippines (6%), Pakistan (6%), Nigeria (4%), and Bangladesh (4%).<ref name=WHO2017Report>{{Cite web|url=https://www.who.int/tb/publications/global_report/en/|title=Global tuberculosis report|publisher=World Health Organization (WHO)|access-date=9 November 2017|archive-date=30 December 2013|archive-url=https://web.archive.org/web/20131230020808/http://www.who.int/tb/publications/global_report/en/index.html|url-status=live}}</ref> By 2021, the number of new cases each year was decreasing by around 2% annually.<ref name="WHO2020"/><ref name=WHO2015Fact>{{Cite web|title=Tuberculosis (TB)|url=https://www.who.int/news-room/fact-sheets/detail/tuberculosis|website=who.int|language=en|access-date=8 May 2020|archive-date=30 July 2020|archive-url=https://web.archive.org/web/20200730165218/https://www.who.int/news-room/fact-sheets/detail/tuberculosis|url-status=live}}</ref> About 80% of people in many Asian and African countries test positive, while 5–10% of people in the United States test positive via the tuberculin test.<ref name=Robbins>{{Cite book|title=Robbins Basic Pathology|date=2007|publisher=Elsevier| vauthors = Kumar V, Robbins SL |isbn=978-1-4160-2973-1|edition=8th|location=Philadelphia|oclc=69672074}}</ref> Tuberculosis has been present in humans since [[Ancient history|ancient times]].<ref name=Lancet11>{{cite journal | vauthors = Lawn SD, Zumla AI | s2cid = 208791546 | title = Tuberculosis | journal = Lancet | volume = 378 | issue = 9785 | pages = 57–72 | date = July 2011 | pmid = 21420161 | doi = 10.1016/S0140-6736(10)62173-3 }}</ref> |
|||
In 2004, mortality and morbidity statistics included 14.6 million chronic active TB cases, 8.9 million new cases, and 1.6 million deaths, mostly in [[Developing nation|developing countries]].<ref name="WHO2004data"/> In addition, a rising number of people in the [[Developed country|developed world]] are contracting tuberculosis because their [[immune system]]s are compromised by [[immunosuppressive drug]]s, [[substance abuse]] or [[HIV]]/[[AIDS]]. |
|||
[[File:En.Wikipedia-VideoWiki-Tuberculosis.webm|thumb|thumbtime=1:00|Video summary ([[Wikipedia:VideoWiki/Tuberculosis|script]])|303x303px]] |
|||
{{TOC limit}} |
|||
== History == |
|||
The rise in HIV infections and the neglect of TB control programs have enabled a resurgence of tuberculosis.<ref>{{cite journal |author=Iademarco MF, Castro KG |title=Epidemiology of tuberculosis |journal=Seminars in respiratory infections |volume=18 |issue=4 |pages=225-40 |year=2003 |pmid=14679472}}</ref> The emergence of [[Antibiotic resistance|drug-resistant]] strains has also contributed to this new epidemic with, from 2000 to 2004, 20% of TB cases being resistant to standard treatments and 2% resistant to [[Tuberculosis treatment#Treatment of MDR-TB|second-line drugs]].<ref name="MMWR2006">{{cite journal |title=Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs—worldwide, 2000–2004 |journal=MMWR Morb Mortal Wkly Rep |volume=55 |issue=11 |pages=301-5 |year=2006 |url=http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5511a2.htm | pmid = 16557213}}</ref> TB incidence varies widely, even in neighboring countries, apparently because of differences in health care systems.<ref name=Sobero_2006>{{cite journal |author=Sobero R, Peabody J |title=Tuberculosis control in Bolivia, Chile, Colombia and Peru: why does incidence vary so much between neighbors? |journal=Int J Tuberc Lung Dis |volume=10 |issue=11 |pages=1292–5 |year=2006 | pmid = 17131791}}</ref> The [[World Health Organization]] declared TB a global health emergency in 1993, and the Stop TB Partnership developed a [[Global Plan to Stop Tuberculosis]] aiming to save 14 million lives between 2006 and 2015.<ref>[[World Health Organization]] (WHO). [http://www.stoptb.org/globalplan/ Stop TB Partnership.] Retrieved on 3 October 2006.</ref> |
|||
{{Main|History of tuberculosis}} |
|||
[[File:Mummy at British Museum.jpg|thumb|[[Egyptian mummy]] in the [[British Museum]] – tubercular decay has been found in the spine.]] |
|||
<!-- Ancient history --> |
|||
Tuberculosis has existed since [[Ancient history|antiquity]].<ref name=Lancet11/> The oldest unambiguously detected ''M. tuberculosis'' gives evidence of the disease in the remains of bison in Wyoming dated to around 17,000 years ago.<ref>{{cite journal | vauthors = Rothschild BM, Martin LD, Lev G, Bercovier H, Bar-Gal GK, Greenblatt C, Donoghue H, Spigelman M, Brittain D | title = Mycobacterium tuberculosis complex DNA from an extinct bison dated 17,000 years before the present | journal = Clinical Infectious Diseases | volume = 33 | issue = 3 | pages = 305–11 | date = August 2001 | pmid = 11438894 | doi = 10.1086/321886 | doi-access = free }}</ref> However, whether tuberculosis originated in bovines, then transferred to humans, or whether both bovine and human tuberculosis diverged from a common ancestor, remains unclear.<ref>{{cite journal | vauthors = Pearce-Duvet JM | title = The origin of human pathogens: evaluating the role of agriculture and domestic animals in the evolution of human disease | journal = Biological Reviews of the Cambridge Philosophical Society | volume = 81 | issue = 3 | pages = 369–82 | date = August 2006 | pmid = 16672105 | doi = 10.1017/S1464793106007020 | s2cid = 6577678 }}</ref> A comparison of the [[gene]]s of [[M. tuberculosis complex]] (MTBC) in humans to MTBC in animals suggests humans did not acquire MTBC from animals during animal domestication, as researchers previously believed. Both strains of the tuberculosis bacteria share a common ancestor, which could have infected humans even before the [[Neolithic Revolution]].<ref>{{cite journal | vauthors = Comas I, Gagneux S | title = The past and future of tuberculosis research | journal = PLOS Pathogens | volume = 5 | issue = 10 | page = e1000600 | date = October 2009 | pmid = 19855821 | pmc = 2745564 | doi = 10.1371/journal.ppat.1000600 | veditors = Manchester M | doi-access = free }}</ref> Skeletal remains show some prehistoric humans (4000 [[Common Era|BC]]) had TB, and researchers have found tubercular decay in the spines of [[Ancient Egypt|Egyptian]] [[mummy|mummies]] dating from 3000 to 2400 BC.<ref>{{cite journal | vauthors = Zink AR, Sola C, Reischl U, Grabner W, Rastogi N, Wolf H, Nerlich AG | title = Characterization of Mycobacterium tuberculosis complex DNAs from Egyptian mummies by spoligotyping | journal = Journal of Clinical Microbiology | volume = 41 | issue = 1 | pages = 359–67 | date = January 2003 | pmid = 12517873 | pmc = 149558 | doi = 10.1128/JCM.41.1.359-367.2003 }}</ref> Genetic studies suggest the presence of TB in [[the Americas]] from about AD 100.<ref>{{cite journal | vauthors = Konomi N, Lebwohl E, Mowbray K, Tattersall I, Zhang D | title = Detection of mycobacterial DNA in Andean mummies | journal = Journal of Clinical Microbiology | volume = 40 | issue = 12 | pages = 4738–40 | date = December 2002 | pmid = 12454182 | pmc = 154635 | doi = 10.1128/JCM.40.12.4738-4740.2002 }}</ref> |
|||
Before the [[Industrial Revolution]], folklore often associated tuberculosis with [[vampire]]s. When one member of a family died from the disease, the other infected members would lose their health slowly. People believed this was caused by the original person with TB draining the life from the other family members.<ref name=sledzik>{{cite journal | vauthors = Sledzik PS, Bellantoni N | title = Brief communication: bioarcheological and biocultural evidence for the New England vampire folk belief | journal = American Journal of Physical Anthropology | volume = 94 | issue = 2 | pages = 269–74 | date = June 1994 | pmid = 8085617 | doi = 10.1002/ajpa.1330940210 | url = http://www.yorku.ca/kdenning/+++2150%202007-8/sledzik%20vampire.pdf | archive-url = https://web.archive.org/web/20170218082115/http://www.yorku.ca/kdenning/+++2150%202007-8/sledzik%20vampire.pdf | url-status=live | archive-date = 18 February 2017 }}</ref> |
|||
==Other names== |
|||
In the past, tuberculosis was called '''consumption''', because it seemed to consume people from within, with a [[hemoptysis|bloody cough]], fever, [[pallor]], and long relentless wasting. Other names included '''phthisis''' (Greek for consumption) and '''phthisis pulmonalis'''; '''[[scrofula]]''' (in adults), affecting the lymphatic system and resulting in swollen neck glands; '''tabes mesenterica''', TB of the abdomen and '''[[lupus vulgaris]]''', TB of the skin; '''wasting disease'''; '''white plague''', because sufferers appear markedly pale; '''king's evil''', because it was believed that a king's touch would heal scrofula; and '''[[Pott's disease]]''', or '''gibbus''' of the spine and joints.<ref name=Britannica1911>[http://www.1911encyclopedia.org/Tuberculosis Tuberculosis] ''Encyclopedia Britannica,'' 11th ed.</ref><ref>[http://www.antiquusmorbus.com/English/English.htm Rudy's List of Archaic Medical Terms] English Glossary of Archaic Medical Terms, Diseases and Causes of Death. Accessed 09 Oct 06</ref> ''[[Miliary tuberculosis]]'' – now commonly known as '''disseminated TB'''– occurs when the infection invades the circulatory system resulting in lesions which have the appearance of [[millet]] seeds on X-ray.<ref name=Britannica1911/><ref>[http://www.nlm.nih.gov/medlineplus/ency/article/000624.htm Disseminated tuberculosis] NIH Medical Encyclopedia. Accessed 09 Oct 06</ref> |
|||
===Identification=== |
|||
==Symptoms== |
|||
Although [[Dr Richard Morton|Richard Morton]] established the pulmonary form associated with [[tubercle (anatomy)|tubercles]] as a pathology in 1689,<ref name="WhoNamedIt-Calmette">{{WhoNamedIt|doctor|2413|Léon Charles Albert Calmette}}</ref><ref name="MedHist1970-Trail">{{cite journal | vauthors = Trail RR | title = Richard Morton (1637-1698) | journal = Medical History | volume = 14 | issue = 2 | pages = 166–74 | date = April 1970 | pmid = 4914685 | pmc = 1034037 | doi = 10.1017/S0025727300015350 }}</ref> due to the variety of its symptoms, TB was not identified as a single disease until the 1820s. [[Benjamin Marten]] conjectured in 1720 that consumptions were caused by microbes which were spread by people living close to each other.<ref>{{cite book |vauthors=Marten B |title=A New Theory of Consumptions—More Especially a Phthisis or Consumption of the Lungs |date=1720 |publisher=T. Knaplock |location=London, England |url=https://babel.hathitrust.org/cgi/pt?id=ucm.5320214800&view=1up&seq=7 |access-date=8 December 2020 |archive-date=26 March 2023 |archive-url=https://web.archive.org/web/20230326205015/https://babel.hathitrust.org/cgi/pt?id=ucm.5320214800&view=1up&seq=7 |url-status=live }} P. 51: "The ''Original'' and ''Essential Cause'' ... may possibly be some certain Species of ''Animalcula'' or wonderfully minute living Creatures, ... " P. 79: "It may be therefore very likely, that by an habitual lying in the same Bed with a Consumptive Patient, constantly Eating and Drinking with him, or by very frequently conversing so nearly, as to draw in part of the Breath he emits from his Lungs, a Consumption may be caught by a sound Person; ... "</ref> In 1819, [[René Laennec]] claimed that tubercles were the cause of pulmonary tuberculosis.<ref>{{cite book |vauthors=Laennec RT |title=De l'auscultation médiate ... |date=1819 |publisher=J.-A. Brosson et J.-S Chaudé |location=Paris, France |volume=1 |page=20 |url=https://books.google.com/books?id=LcZEAAAAcAAJ&pg=PA20 |language=fr |access-date=6 December 2020 |archive-date=2 June 2021 |archive-url=https://web.archive.org/web/20210602212549/https://books.google.com/books?id=LcZEAAAAcAAJ&pg=PA20 |url-status=live }} From p. 20: ''"L'existence des tubercules dans le poumon est la cause et constitue le charactère anatomique propre de la phthisie pulmonaire (a). (a) ... l'effet dont cette maladie tire son nom, c'est-à-dire, la consumption."'' (The existence of tubercles in the lung is the cause and constitutes the unique anatomical characteristic of pulmonary tuberculosis (a). (a) ... the effect from which this malady [pulmonary tuberculosis] takes its name, that is, consumption.)</ref> [[Johann Lukas Schönlein|J. L. Schönlein]] first published the name "tuberculosis" (German: ''Tuberkulose'') in 1832.<ref>{{cite book |vauthors=Schönlein JL |title=Allgemeine und specielle Pathologie und Therapie |trans-title=General and Special Pathology and Therapy |date=1832 |publisher=C. Etlinger |location=Würzburg, (Germany) |volume=3 |page=103 |url=https://books.google.com/books?id=zAtbAAAAcAAJ&pg=PA103 |language=de |access-date=6 December 2020 |archive-date=2 June 2021 |archive-url=https://web.archive.org/web/20210602233224/https://books.google.com/books?id=zAtbAAAAcAAJ&pg=PA103 |url-status=live }}</ref><ref>The word "tuberculosis" first appeared in Schönlein's clinical notes in 1829. See: {{cite journal | vauthors = Jay SJ, Kırbıyık U, Woods JR, Steele GA, Hoyt GR, Schwengber RB, Gupta P | title = Modern theory of tuberculosis: culturomic analysis of its historical origin in Europe and North America | journal = The International Journal of Tuberculosis and Lung Disease | volume = 22 | issue = 11 | pages = 1249–1257 | date = November 2018 | pmid = 30355403 | doi = 10.5588/ijtld.18.0239 | s2cid = 53027676 }} See especially Appendix, p. iii.</ref> Between 1838 and 1845, John Croghan, the owner of [[Mammoth Cave]] in Kentucky from 1839 onwards, brought a number of people with tuberculosis into the cave in the hope of curing the disease with the constant temperature and purity of the cave air; each died within a year.<ref>{{cite web | url = http://edition.cnn.com/2004/TRAVEL/DESTINATIONS/02/26/mammoth.cave.ap/index.html | title = Kentucky: Mammoth Cave long on history. | archive-url = https://web.archive.org/web/20060813140746/http://edition.cnn.com/2004/TRAVEL/DESTINATIONS/02/26/mammoth.cave.ap/index.html | archive-date= 13 August 2006| work = [[CNN]] | date = 27 February 2004 | access-date = 8 October 2006 }}</ref> Hermann Brehmer opened the first TB [[sanatorium]] in 1859 in Görbersdorf (now [[Sokołowsko]]) in [[Silesia]].<ref name =sanatoria>{{cite journal | vauthors = McCarthy OR | title = The key to the sanatoria | journal = Journal of the Royal Society of Medicine | volume = 94 | issue = 8 | pages = 413–17 | date = August 2001 | pmid = 11461990 | pmc = 1281640 | url = http://www.jrsm.org/cgi/pmidlookup?view=long&pmid=11461990 | doi = 10.1177/014107680109400813 | access-date = 28 September 2011 | archive-date = 3 August 2012 | archive-url = https://archive.today/20120803180504/http://www.jrsm.org/cgi/pmidlookup?view=long&pmid=11461990 | url-status = live }}</ref> In 1865, [[Jean Antoine Villemin]] demonstrated that tuberculosis could be transmitted, via inoculation, from humans to animals and among animals.<ref>{{cite journal |vauthors=Villemin JA |title=Cause et nature de la tuberculose |journal=Bulletin de l'Académie Impériale de Médecine |date=1865 |volume=31 |pages=211–216 |url=https://babel.hathitrust.org/cgi/pt?id=hvd.32044103060562&view=1up&seq=215 |trans-title=Cause and nature of tuberculosis |language=fr |access-date=6 December 2020 |archive-date=9 December 2021 |archive-url=https://web.archive.org/web/20211209200251/https://babel.hathitrust.org/cgi/pt?id=hvd.32044103060562&view=1up&seq=215 |url-status=live }} |
|||
{{Further|[[Tuberculosis classification]]}} |
|||
When the disease becomes active, 75% of the cases are pulmonary TB. Symptoms include chest pain, [[hemoptysis|coughing up blood]], and a productive, prolonged cough for more than three weeks. Systemic symptoms include fever, chills, [[night sweats]], [[appetite loss]], weight loss, pallor, and often a tendency to fatigue very easily.<ref name="WHO2004data"/> |
|||
* See also: {{cite book |vauthors=Villemin JA |title=Etudes sur la tuberculose: preuves rationnelles et expérimentales de sa spécificité et de son inoculabilité |trans-title=Studies of tuberculosis: rational and experimental evidence of its specificity and inoculability |date=1868 |publisher=J.-B. Baillière et fils |location=Paris, France |url=https://books.google.com/books?id=JFg7AAAAcAAJ&pg=PP7 |language=fr |access-date=6 December 2020 |archive-date=7 February 2024 |archive-url=https://web.archive.org/web/20240207093804/https://books.google.com/books?id=JFg7AAAAcAAJ&pg=PP7#v=onepage&q&f=false |url-status=live }}</ref> (Villemin's findings were confirmed in 1867 and 1868 by [[John Burdon-Sanderson]].<ref>Burdon-Sanderson, John Scott. (1870) "Introductory Report on the Intimate Pathology of Contagion." Appendix to: Twelfth Report to the Lords of Her Majesty's Most Honourable Privy Council of the Medical Officer of the Privy Council [for the year 1869], Parliamentary Papers (1870), vol. 38, 229–256.</ref>) |
|||
In the other 25% of active cases, the infection moves from the lungs, causing other kinds of TB more common in [[immunosuppressed]] persons and young children. Extrapulmonary infection sites include the [[pleura]], the [[central nervous system]] in [[meningitis]], the [[lymphatic system]] in [[scrofula]] of the neck, the [[genitourinary system]] in urogenital tuberculosis, and bones and joints in [[Pott's disease]] of the spine. An especially serious form is disseminated TB, more commonly known as [[miliary tuberculosis]]. Although extrapulmonary TB is not contagious, it may co-exist with pulmonary TB, which ''is'' contagious.<ref name=CDCcourse>[[Centers for Disease Control and Prevention]] (CDC), Division of Tuberculosis Elimination. [http://www.cdc.gov/nchstp/tb/pubs/corecurr/default.htm Core Curriculum on Tuberculosis: What the Clinician Should Know.] 4th edition (2000). Updated Aug 2003.</ref> |
|||
[[File:RobertKoch.jpg|upright|thumb|Robert Koch discovered the tuberculosis bacillus.]] |
|||
==Bacterial species== |
|||
[[Robert Koch]] identified and described the bacillus causing tuberculosis, ''M. tuberculosis'', on 24 March 1882.<ref>{{cite book | vauthors = Koch R | title = Robert Koch: Zentrale Texte | chapter = Die Ätiologie der Tuberkulose (1882) |series=Klassische Texte der Wissenschaft |date=24 March 1882|trans-title=The Etiology of Tuberculosis| chapter-url = http://edoc.rki.de/docviews/abstract.php?id=610|volume=19|pages=221–30|doi=10.1007/978-3-662-56454-7_4|isbn=978-3-662-56454-7|access-date=15 June 2021|archive-date=6 November 2018|archive-url= https://web.archive.org/web/20181106191545/https://babel.hathitrust.org/cgi/pt?id=mdp.39015020075001;view=1up;seq=235|url-status=live|publisher=Springer Spektrum|location=Berlin, Heidelberg}}</ref><ref name="discoverydate">{{cite web|url=https://www.cdc.gov/tb/worldtbday/history.htm|title=History: World TB Day|publisher=[[Centers for Disease Control and Prevention]] (CDC)|url-status=live|access-date=23 March 2019|date=12 December 2016|archive-date=7 December 2018|archive-url=https://web.archive.org/web/20181207112253/https://www.cdc.gov/tb/worldtbday/history.htm}}</ref> In 1905, he was awarded the [[Nobel Prize in Physiology or Medicine]] for this discovery.<ref>{{Cite web|title=The Nobel Prize in Physiology or Medicine 1905|url=https://www.nobelprize.org/prizes/medicine/1905/summary/|access-date=7 October 2006|archive-url=https://web.archive.org/web/20061210184150/http://nobelprize.org/nobel_prizes/medicine/laureates/1905/|archive-date=10 December 2006|url-status=live|website=www.nobelprize.org|language=en-US}}</ref> |
|||
{{main|Mycobacterium tuberculosis}} |
|||
===Development of treatments=== |
|||
[[Image:Mycobacterium tuberculosis.jpg|300px|right|thumb|Scanning electron micrograph of ''[[Mycobacterium tuberculosis]]'']] |
|||
In Europe, rates of tuberculosis began to rise in the early 1600s to a peak level in the 1800s, when it caused nearly 25% of all deaths.<ref>{{cite book| vauthors = Bloom BR |title= Tuberculosis: pathogenesis, protection, and control|year= 1994|publisher= ASM Press|location= Washington, DC|isbn= 978-1-55581-072-6|url-access= registration|url= https://archive.org/details/tuberculosispath0000unse}}</ref> In the 18th and 19th century, [[History of tuberculosis#Epidemic tuberculosis|tuberculosis had become epidemic in Europe]], showing a seasonal pattern.<ref name=":02">{{Cite web| vauthors = Frith J |title=History of Tuberculosis. Part 1 – Phthisis, consumption and the White Plague|url=https://jmvh.org/article/history-of-tuberculosis-part-1-phthisis-consumption-and-the-white-plague/|url-status=live|access-date=26 February 2021|website=Journal of Military and Veterans' Health|archive-date=8 April 2021|archive-url=https://web.archive.org/web/20210408050305/https://jmvh.org/article/history-of-tuberculosis-part-1-phthisis-consumption-and-the-white-plague/}}</ref><ref name=":5">{{cite journal | vauthors = Zürcher K, Zwahlen M, Ballif M, Rieder HL, Egger M, Fenner L | title = Influenza Pandemics and Tuberculosis Mortality in 1889 and 1918: Analysis of Historical Data from Switzerland | journal = PLOS ONE | volume = 11 | issue = 10 | pages = e0162575 | date = 5 October 2016 | pmid = 27706149 | pmc = 5051959 | doi = 10.1371/journal.pone.0162575 | doi-access = free | bibcode = 2016PLoSO..1162575Z }}</ref> Tuberculosis caused widespread public concern in the 19th and early 20th centuries as the disease became common among the urban poor. In 1815, one in four deaths in England was due to "consumption". By 1918, TB still caused one in six deaths in France.{{Citation needed|date=August 2020}} After TB was determined to be contagious, in the 1880s, it was put on a [[List of notifiable diseases|notifiable-disease]] list in Britain; campaigns started to stop people from spitting in public places, and the infected poor were "encouraged" to enter [[sanatorium|sanatoria]] that resembled prisons (the sanatoria for the middle and upper classes offered excellent care and constant medical attention).<ref name =sanatoria/> Whatever the benefits of the "fresh air" and labor in the sanatoria, even under the best conditions, 50% of those who entered died within five years ({{circa}} 1916).<ref name =sanatoria/> |
|||
Robert Koch did not believe the cattle and human tuberculosis diseases were similar, which delayed the recognition of infected milk as a source of infection. During the first half of the 1900s, the risk of transmission from this source was dramatically reduced after the application of the [[pasteurization]] process. Koch announced a [[glycerine]] extract of the tubercle bacilli as a "remedy" for tuberculosis in 1890, calling it "tuberculin". Although it was not effective, it was later successfully adapted as a screening test for the presence of pre-symptomatic tuberculosis.<ref>{{cite journal | vauthors = Waddington K | title = To stamp out 'so terrible a malady': bovine tuberculosis and tuberculin testing in Britain, 1890–1939 | journal = Medical History | volume = 48 | issue = 1 | pages = 29–48 | date = January 2004 | pmid = 14968644 | pmc = 546294 | doi = 10.1017/S0025727300007043 }}</ref> [[World Tuberculosis Day]] is marked on 24 March each year, the anniversary of Koch's original scientific announcement. When the [[Medical Research Council (UK)|Medical Research Council]] formed in Britain in 1913, it initially focused on tuberculosis research.<ref>{{cite book | vauthors = Hannaway C |title= Biomedicine in the twentieth century: practices, policies, and politics|year= 2008|publisher= IOS Press|location= Amsterdam|isbn=978-1-58603-832-8|page= 233|url= https://books.google.com/books?id=o5HBxyg5APIC&pg=PA233|url-status=live|archive-url= https://web.archive.org/web/20150907185226/https://books.google.com/books?id=o5HBxyg5APIC&pg=PA233|archive-date= 7 September 2015}}</ref> |
|||
The primary cause of TB , ''[[Mycobacterium tuberculosis]]'' (MTB), is an [[aerobic organism|aerobic]] [[bacterium]] that [[cell division|divides]] every 16 to 20 hours, an extremely slow rate compared with other bacteria, which usually divide in less than an hour.<ref name=Cox_2004>{{cite journal |author=Cox R |title=Quantitative relationships for specific growth rates and macromolecular compositions of ''Mycobacterium tuberculosis'', ''Streptomyces coelicolor'' A3(2) and ''Escherichia coli'' B/r: an integrative theoretical approach |journal=Microbiology |volume=150 |issue=Pt 5 |pages=1413–26 |year=2004 |url=http://mic.sgmjournals.org/cgi/content/full/150/5/1413?view=long&pmid=15133103#R35 | pmid = 15133103}}</ref> (For example, one of the fastest-growing bacteria is a strain of ''[[E. coli]]'' that can divide roughly every 20 minutes.) Since MTB has a cell wall but lacks a [[phospholipid]] [[Bacterial cell structure|outer membrane]], it is [[Tuberculosis classification|classified]] as a [[Gram-positive]] bacterium. However, if a [[Gram stain]] is performed, MTB either stains very weakly Gram-positive or does not retain dye due to the high lipid & mycolic acid content of its cell wall.<ref name=Madison_2001>{{cite journal |author=Madison B |title=Application of stains in clinical microbiology. |journal=Biotech Histochem |volume=76 |issue=3 |pages=119-25 |year=2001 |pmid=11475314}}</ref> MTB is a small rod-like [[bacillus]] that can withstand weak [[disinfectant]]s and survive in a [[Endospore|dry state]] for weeks. In nature, the bacterium can grow only within the cells of a [[host (biology)|host]] organism, but ''M. tuberculosis'' can be cultured ''[[in vitro]]''.<ref name=Parish_1999>{{cite journal |author=Parish T, Stoker N |title=Mycobacteria: bugs and bugbears (two steps forward and one step back) |journal=Mol Biotechnol |volume=13 |issue=3 |pages=191–200 |year=1999 | pmid = 10934532}}</ref> |
|||
[[Albert Calmette]] and [[Camille Guérin]] achieved the first genuine success in immunization against tuberculosis in 1906, using attenuated bovine-strain tuberculosis. It was called [[BCG vaccine|bacille Calmette–Guérin]] (BCG). The BCG vaccine was first used on humans in 1921 in France,<ref name=Bonah>{{cite journal | vauthors = Bonah C | title = The 'experimental stable' of the BCG vaccine: safety, efficacy, proof, and standards, 1921–1933 | journal = Studies in History and Philosophy of Biological and Biomedical Sciences | volume = 36 | issue = 4 | pages = 696–721 | date = December 2005 | pmid = 16337557 | doi = 10.1016/j.shpsc.2005.09.003 }}</ref> but achieved widespread acceptance in the US, Great Britain, and Germany only after World War II.<ref name=Comstock>{{cite journal | vauthors = Comstock GW | title = The International Tuberculosis Campaign: a pioneering venture in mass vaccination and research | journal = Clinical Infectious Diseases | volume = 19 | issue = 3 | pages = 528–40 | date = September 1994 | pmid = 7811874 | doi = 10.1093/clinids/19.3.528 }}</ref> |
|||
Using certain [[histology|histological]] techniques on expectorate samples from [[phlegm]] (also called sputum), scientists can identify MTB under a regular microscope. Since MTB retains certain stains after being treated with acidic solution, it is classified as an [[acid-fast bacillus]] (AFB).<ref name=Madison_2001>{{cite journal |author=Madison B |title=Application of stains in clinical microbiology |journal=Biotech Histochem |volume=76 |issue=3 |pages=119-25 |year=2001 | pmid = 11475314}}</ref> The most common staining technique, the [[Ziehl-Neelsen stain]], dyes AFBs a bright red that stands out clearly against a blue background. Other ways to visualize AFBs include an [[auramine-rhodamine stain]] and [[Fluorescence microscope|fluorescent microscopy]]. |
|||
<!-- Effective management --> |
|||
The ''M. tuberculosis'' complex includes 3 other TB-causing [[mycobacterium|mycobacteria]]: ''[[Mycobacterium bovis|M. bovis]]'', ''[[Mycobacterium africanum|M. africanum]]'' and ''[[Mycobacterium microti|M. microti]]''. The first two only very rarely cause disease in [[immunocompetent]] people. On the other hand, although ''M. microti'' is not usually [[pathogen|pathogenic]], it is possible that the [[prevalence]] of ''M. microti'' infections has been underestimated.<ref name=Niemann_2000>{{cite journal |author=Niemann S, Richter E, Dalügge-Tamm H, Schlesinger H, Graupner D, Königstein B, Gurath G, Greinert U, Rüsch-Gerdes S |title=Two cases of ''Mycobacterium microti'' derived tuberculosis in HIV-negative immunocompetent patients |journal=Emerg Infect Dis |volume=6 |issue=5 |pages=539-42 |year=2000 |pmid = 10998387}}</ref> |
|||
By the 1950s mortality in Europe had decreased about 90%.<ref name=Per2010>{{cite book| vauthors = Persson S |title= Smallpox, Syphilis and Salvation: Medical Breakthroughs That Changed the World|year= 2010|publisher= ReadHowYouWant.com|isbn= 978-1-4587-6712-7|page= 141|url= https://books.google.com/books?id=-W7ch1d6JOoC&pg=PA141|url-status=live|archive-url= https://web.archive.org/web/20150906192102/https://books.google.com/books?id=-W7ch1d6JOoC&pg=PA141|archive-date= 6 September 2015}}</ref> Improvements in sanitation, vaccination, and other public-health measures began significantly reducing rates of tuberculosis even before the arrival of [[streptomycin]] and other antibiotics, although the disease remained a significant threat.<ref name=Per2010/> In 1946, the development of the antibiotic streptomycin made effective treatment and cure of TB a reality. Prior to the introduction of this medication, the only treatment was surgical intervention, including the "[[pneumothorax]] technique", which involved collapsing an infected lung to "rest" it and to allow tuberculous lesions to heal.<ref>{{cite book| vauthors = Shields T |title= General thoracic surgery|year= 2009|publisher= Wolters Kluwer Health/Lippincott Williams & Wilkins|location= Philadelphia|isbn= 978-0-7817-7982-1|page= 792|url= https://books.google.com/books?id=bVEEHmpU-1wC&pg=PA792|edition= 7th|url-status=live|archive-url= https://web.archive.org/web/20150906212146/https://books.google.com/books?id=bVEEHmpU-1wC&pg=PA792|archive-date= 6 September 2015}}</ref> |
|||
===Current reemergence=== |
|||
Other known pathogenic [[Mycobacterium|mycobacteria]] include ''[[Mycobacterium leprae]]'', [[Mycobacterium avium complex|''Mycobacterium avium'']] and ''M. kansasii''. The last two are part of the [[nontuberculous mycobacteria]] (NTM) group. Nontuberculous mycobacteria cause neither TB nor [[leprosy]], but they ''do'' cause pulmonary diseases resembling TB.<ref name=ALA_1997>{{cite journal |author= |title=Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Medical Section of the American Lung Association |journal=Am J Respir Crit Care Med |volume=156 |issue=2 Pt 2 |pages=S1–25 |year=1997 |pmid = 9279284}}</ref> |
|||
Because of the emergence of [[multidrug-resistant tuberculosis]] (MDR-TB), surgery has been re-introduced for certain cases of TB infections. It involves the removal of infected chest cavities ("bullae") in the lungs to reduce the number of bacteria and to increase exposure of the remaining bacteria to antibiotics in the bloodstream.<ref>{{cite journal | vauthors = Lalloo UG, Naidoo R, Ambaram A | s2cid = 24221563 | title = Recent advances in the medical and surgical treatment of multi-drug resistant tuberculosis | journal = Current Opinion in Pulmonary Medicine | volume = 12 | issue = 3 | pages = 179–85 | date = May 2006 | pmid = 16582672 | doi = 10.1097/01.mcp.0000219266.27439.52 }}</ref> Hopes of eliminating TB ended with the rise of [[Antibiotic resistant|drug-resistant]] strains in the 1980s. The subsequent resurgence of tuberculosis resulted in the declaration of a global health emergency by the World Health Organization (WHO) in 1993.<ref>{{cite web |title= Frequently asked questions about TB and HIV |url=https://www.who.int/tb/hiv/faq/en/index.html |publisher=World Health Organization (WHO) |access-date= 15 April 2012 |archive-url= https://web.archive.org/web/20110808115404/http://www.who.int/tb/hiv/faq/en/ |archive-date= 8 August 2011 |url-status=dead }}</ref> |
|||
== Signs and symptoms == |
|||
===Evolution=== |
|||
During its [[evolution]], ''M. tuberculosis'' has lost numerous coding and non-coding regions in its [[genome]], losses that can be used to distinguish between strains of the bacterium. The implication is that ''M. tuberculosis'' strains differ geographically, so their genetic differences can be used to track the origins and movement of each strain.<ref name=Rao_2005>{{cite journal |author=Rao K, Kauser F, Srinivas S, Zanetti S, Sechi L, Ahmed N, Hasnain S |title=Analysis of genomic downsizing on the basis of region-of-difference polymorphism profiling of Mycobacterium tuberculosis patient isolates reveals geographic partitioning |journal=J Clin Microbiol |volume=43 |issue=12 |pages=5978–82 |year=2005 | pmid = 16333085}}</ref> |
|||
[[File:Tuberculosis symptoms.svg|thumb|upright=1.5|The main symptoms of variants and stages of tuberculosis are given,<ref>{{cite web|url=http://www.emedicinehealth.com/tuberculosis/page3_em.htm|title=Tuberculosis Symptoms|publisher=eMedicine Health| vauthors = Schiffman G |date=15 January 2009|url-status=live|archive-url=https://web.archive.org/web/20090516075020/http://www.emedicinehealth.com/tuberculosis/page3_em.htm|archive-date=16 May 2009}}</ref> with many symptoms overlapping with other variants, while others are more (but not entirely) specific for certain variants. Multiple variants may be present simultaneously.]] |
|||
==Transmission== |
|||
Tuberculosis may infect any part of the body, but most commonly occurs in the lungs (known as pulmonary tuberculosis).<ref name=ID10/> Extrapulmonary TB occurs when tuberculosis develops outside of the lungs, although extrapulmonary TB may coexist with pulmonary TB.<ref name=ID10/> |
|||
When people suffering from active pulmonary TB cough, sneeze, speak, kiss, or spit, they expel infectious [[particulate|aerosol]] droplets 0.5 to 5 [[µm]] in diameter. A single sneeze, for instance, can release about 40,000.<ref name=Cole_1998>{{cite journal |author=Cole E, Cook C |title=Characterization of infectious aerosols in health care facilities: an aid to effective engineering controls and preventive strategies |journal=Am J Infect Control |volume=26 |issue=4 |pages=453-64 |year=1998 | pmid = 9721404}}</ref> People with prolonged, frequent, or intense contact are at highest risk of becoming infected, with an estimated 22% infection rate. A person with active but untreated tuberculosis can infect 10–15 other people per year.<ref name="WHO2004data"/> Others at risk include people in areas where TB is common, people who inject illicit drugs (especially when sharing needles), residents and employees of high-risk congregate settings, medically under-served and low-income populations, high-risk racial or ethnic minority populations, children exposed to adults in high-risk categories, patients [[immunocompromised]] by conditions such as [[HIV]]/[[AIDS]], people who take immunosuppressant drugs, and health care workers serving these high-risk clients.<ref name=Griffith_1996>{{cite journal |author=Griffith D, Kerr C |title=Tuberculosis: disease of the past, disease of the present |journal=J Perianesth Nurs |volume=11 |issue=4 |pages=240-5 |year=1996 | pmid = 8964016}}</ref> |
|||
General signs and symptoms include fever, [[chills]], night sweats, [[Anorexia (symptom)|loss of appetite]], weight loss, and [[fatigue (medical)|fatigue]].<ref name=ID10/> Significant [[nail clubbing]] may also occur.<ref name="Pet2005">{{cite book|url=http://www.wiley.com/WileyCDA/WileyTitle/productCd-072791605X.html|title=Evidence-Based Respiratory Medicine|date=2005|publisher=BMJ Books|isbn=978-0-7279-1605-1|veditors=Gibson PG, Abramson M, Wood-Baker R, Volmink J, Hensley M, Costabel U|edition=1st|page=321|archive-url=https://web.archive.org/web/20151208072842/http://www.wiley.com/WileyCDA/WileyTitle/productCd-072791605X.html|archive-date=8 December 2015|url-status=live}}</ref> |
|||
Transmission can only occur from people with active—not latent—TB. The probability of transmission from one person to another depends upon the number of infectious droplets expelled by a carrier, the effectiveness of ventilation, the duration of exposure, and the [[virulence]] of the ''M. tuberculosis'' [[strain (biology)|strain]].<ref name=CDCcourse/> The chain of transmission can therefore be broken by isolating patients with active disease and starting effective anti-tuberculous therapy. After two weeks of such treatment, people with [[Antibiotic resistance|non-resistant]] active TB generally cease to be contagious.{{cn}} |
|||
== |
=== Pulmonary === |
||
[[Image:TB in sputum.png|thumb|300px|''[[Mycobacterium tuberculosis]]'' (stained red) in sputum]] |
|||
If a tuberculosis infection does become active, it most commonly involves the lungs (in about 90% of cases).<ref name=Lancet11/><ref>{{cite book| vauthors = Behera D |title=Textbook of Pulmonary Medicine|year=2010|publisher=Jaypee Brothers Medical Publishers|location=New Delhi|isbn=978-81-8448-749-7|page=457|url=https://books.google.com/books?id=0TbJjd9eTp0C&pg=PA457|edition=2nd|url-status=live|archive-url=https://web.archive.org/web/20150906185549/https://books.google.com/books?id=0TbJjd9eTp0C&pg=PA457|archive-date=6 September 2015}}</ref> Symptoms may include [[chest pain]] and a prolonged cough producing sputum.<!-- <ref name=Lancet11/> --> About 25% of people may not have any symptoms (i.e., they remain asymptomatic).<ref name=Lancet11/> Occasionally, people may [[hemoptysis|cough up blood]] in small amounts, and in very rare cases, the infection may erode into the [[pulmonary artery]] or a [[Rasmussen's aneurysm]], resulting in massive bleeding.<ref name=ID10/><ref>{{cite journal | vauthors = Halezeroğlu S, Okur E | title = Thoracic surgery for haemoptysis in the context of tuberculosis: what is the best management approach? | journal = Journal of Thoracic Disease | volume = 6 | issue = 3 | pages = 182–85 | date = March 2014 | pmid = 24624281 | pmc = 3949181 | doi = 10.3978/j.issn.2072-1439.2013.12.25 }}</ref> Tuberculosis may become a chronic illness and cause extensive scarring in the upper lobes of the lungs.<!-- <ref name=ID10/> --> The upper lung lobes are more frequently affected by tuberculosis than the lower ones.<ref name=ID10/> The reason for this difference is not clear.<ref name="Robbins" /> It may be due to either better air flow,<ref name="Robbins" /> or poor [[lymph]] drainage within the upper lungs.<ref name=ID10/> |
|||
About 90% of those infected with ''Mycobacterium tuberculosis'' have [[asymptomatic]], latent TB infection (sometimes called LTBI), with only a 10% lifetime chance that a latent infection will progress to TB disease. However, if untreated, the death rate for these active TB cases is more than 50%.<ref name =TDRreport>Onyebujoh, Phillip and Rook, Graham A. W. [http://www.who.int/tdr/dw/tb2004.htm World Health Organization Disease Watch: Focus: Tuberculosis.] December 2004. Accessed 07 October 2006.</ref> |
|||
=== Extrapulmonary === |
|||
TB infection begins when the mycobacteria reach the [[Pulmonary alveolus|pulmonary alveoli]], where they invade and replicate within alveolar [[macrophages]].<ref name=Houben>{{cite journal |author=Houben E, Nguyen L, Pieters J |title=Interaction of pathogenic mycobacteria with the host immune system |journal=Curr Opin Microbiol |volume=9 |issue=1 |pages=76–85 |year=2006 | pmid = 16406837}}</ref> The primary site of infection in the lungs is called the [[Ghon focus]]. Bacteria are picked up by [[dendritic cell]]s, which do not allow replication, although these cells can transport the bacilli to local ([[mediastinal]]) [[lymph node]]s. Further spread is through the bloodstream to the more distant tissues and organs where secondary TB lesions can develop in lung apices, peripheral lymph nodes, kidneys, brain, and bone.<ref name=Herrmann_2005>{{cite journal |author=Herrmann J, Lagrange P |title=Dendritic cells and Mycobacterium tuberculosis: which is the Trojan horse? |journal=Pathol Biol (Paris) |volume=53 |issue=1 |pages=35–40 |year=2005 | pmid = 15620608}}</ref> All parts of the body can be affected by the disease, though it rarely affects the [[heart]], [[skeletal muscle]]s, [[pancreas]] and [[thyroid]].<ref>{{cite journal |author=Agarwal R, Malhotra P, Awasthi A, Kakkar N, Gupta D |url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=15857515 |title=Tuberculous dilated cardiomyopathy: an under-recognized entity? |journal=BMC Infect Dis |volume=5 |issue=1 |pages=29 |year=2005 |pmid=15857515}}</ref> |
|||
{{Main|Extrapulmonary tuberculosis}} |
|||
In 15–20% of active cases, the infection spreads outside the lungs, causing other kinds of TB.<ref>{{cite book| veditors = Jindal SK |title=Textbook of Pulmonary and Critical Care Medicine|publisher=Jaypee Brothers Medical Publishers|location=New Delhi|isbn=978-93-5025-073-0|page=549|url=https://books.google.com/books?id=EvGTw3wn-zEC&pg=PA549|year=2011|url-status=live|archive-url=https://web.archive.org/web/20150907185434/https://books.google.com/books?id=EvGTw3wn-zEC&pg=PA549|archive-date=7 September 2015}}</ref> These are collectively denoted as extrapulmonary tuberculosis.<ref name=Extra2005>{{cite journal | vauthors = Golden MP, Vikram HR | title = Extrapulmonary tuberculosis: an overview | journal = American Family Physician | volume = 72 | issue = 9 | pages = 1761–68 | date = November 2005 | pmid = 16300038 }}</ref> Extrapulmonary TB occurs more commonly in people with a [[Immunosuppression|weakened immune system]] and young children. In those with HIV, this occurs in more than 50% of cases.<ref name=Extra2005/> Notable extrapulmonary infection sites include the [[Pleural cavity|pleura]] (in tuberculous pleurisy), the [[central nervous system]] (in [[tuberculous meningitis]]), the [[lymphatic system]] (in [[Tuberculous cervical lymphadenitis|scrofula]] of the neck), the [[genitourinary system]] (in [[urogenital tuberculosis]]), and the [[bone]]s and joints (in [[Pott disease]] of the spine), among others. A potentially more serious, widespread form of TB is called "disseminated tuberculosis"; it is also known as [[miliary tuberculosis]].<ref name=ID10/> Miliary TB currently makes up about 10% of extrapulmonary cases.<ref name=Gho2008/> |
|||
== Causes == |
|||
Tuberculosis is classified as one of the [[granuloma]]tous inflammatory conditions. [[Macrophage]]s, [[T cell|T lymphocytes]], [[B cell|B lymphocytes]] and [[fibroblast]]s are among the cells that aggregate to form a [[granuloma]], with [[lymphocytes]] surrounding the infected macrophages. The granuloma functions not only to prevent dissemination of the mycobacteria, but also provides a local environment for communication of cells of the immune system. Within the granuloma, T lymphocytes (CD4+) secrete [[cytokines]] such as [[interferon gamma]], which activates macrophages to destroy the bacteria with which they are infected.<ref name=Kaufmann_2002>{{cite journal |author=Kaufmann S |title=Protection against tuberculosis: cytokines, T cells, and macrophages |journal=Ann Rheum Dis |volume=61 Suppl 2 |issue= |pages=ii54-8 |year=2002 | pmid = 12379623}}</ref> T lymphocytes (CD8+) can also directly kill infected cells.<ref name=Houben/> |
|||
=== Mycobacteria === |
|||
Importantly, bacteria are not always eliminated within the granuloma, but can become dormant, resulting in a latent infection. Another feature of the granulomas of human tuberculosis is the development of cell death, also called [[necrosis]], in the center of [[Tubercle (anatomy)|tubercles]]. To the naked eye this has the texture of soft white cheese and was termed [[caseous]] [[necrosis]].<ref name=Grosset>{{cite journal |author=Grosset J |title=Mycobacterium tuberculosis in the extracellular compartment: an underestimated adversary |journal=Antimicrob Agents Chemother |volume=47 |issue=3 |pages=833-6 |year=2003 | pmid = 12604509}}</ref> |
|||
{{Main| Mycobacterium tuberculosis}} |
|||
[[File:Mycobacterium tuberculosis.jpg|thumb|[[Scanning electron micrograph]] of ''M. tuberculosis'']] |
|||
The main cause of TB is ''[[Mycobacterium tuberculosis]]'' (MTB), a small, [[aerobic organism|aerobic]], nonmotile [[bacillus]].<ref name=ID10/> The high [[lipid]] content of this [[pathogen]] accounts for many of its unique clinical characteristics.<ref>{{cite book | vauthors = Southwick F |title=Infectious Diseases: A Clinical Short Course, 2nd ed. |publisher=McGraw-Hill Medical Publishing Division |year=2007 |pages=104, 313–14 |chapter=Chapter 4: Pulmonary Infections |isbn=978-0-07-147722-2}}</ref> It [[cell division|divides]] every 16 to 20 hours, which is an extremely slow rate compared with other bacteria, which usually divide in less than an hour.<ref>{{cite book| vauthors = Jindal SK |title=Textbook of Pulmonary and Critical Care Medicine|publisher=Jaypee Brothers Medical Publishers|location=New Delhi|isbn=978-93-5025-073-0|page=525|url=https://books.google.com/books?id=rAT1bdnDakAC&pg=PA525|year=2011|url-status=live|archive-url=https://web.archive.org/web/20150906211342/https://books.google.com/books?id=rAT1bdnDakAC&pg=PA525|archive-date=6 September 2015}}</ref> Mycobacteria have an [[Bacterial cell structure|outer membrane]] lipid bilayer.<ref name=Niederweis2010>{{cite journal | vauthors = Niederweis M, Danilchanka O, Huff J, Hoffmann C, Engelhardt H | title = Mycobacterial outer membranes: in search of proteins | journal = Trends in Microbiology | volume = 18 | issue = 3 | pages = 109–16 | date = March 2010 | pmid = 20060722 | pmc = 2931330 | doi = 10.1016/j.tim.2009.12.005 }}</ref> If a [[Gram stain]] is performed, MTB either stains very weakly "Gram-positive" or does not retain dye as a result of the high lipid and [[mycolic acid]] content of its cell wall.<ref name=Madison_2001>{{cite journal | vauthors = Madison BM | title = Application of stains in clinical microbiology | journal = Biotechnic & Histochemistry | volume = 76 | issue = 3 | pages = 119–25 | date = May 2001 | pmid = 11475314 | doi = 10.1080/714028138 }}</ref> MTB can withstand weak [[disinfectant]]s and survive in a [[Endospore|dry state]] for weeks. In nature, the bacterium can grow only within the cells of a [[host (biology)|host]] organism, but ''M. tuberculosis'' can be cultured [[in vitro|in the laboratory]].<ref name=Parish_1999>{{cite journal | vauthors = Parish T, Stoker NG | s2cid = 28960959 | title = Mycobacteria: bugs and bugbears (two steps forward and one step back) | journal = Molecular Biotechnology | volume = 13 | issue = 3 | pages = 191–200 | date = December 1999 | pmid = 10934532 | doi = 10.1385/MB:13:3:191 | doi-access = free }}</ref> |
|||
Using [[histology|histological]] stains on [[expectorate]]d samples from [[phlegm]] (also called sputum), scientists can identify MTB under a microscope. Since MTB retains certain stains even after being treated with acidic solution, it is classified as an [[acid-fast bacillus]].<ref name=Robbins/><ref name="Madison_2001"/> The most common acid-fast staining techniques are the [[Ziehl–Neelsen stain]]<ref name=Stain2000>{{cite book |title=Medical Laboratory Science: Theory and Practice |publisher=Tata McGraw-Hill |location=New Delhi |year=2000 |page=473 |isbn=978-0-07-463223-9 |url=https://books.google.com/books?id=lciNs3VQPLoC&pg=PA473 |url-status=live |archive-url=https://web.archive.org/web/20150906213737/https://books.google.com/books?id=lciNs3VQPLoC&pg=PA473 |archive-date=6 September 2015 }}</ref> and the [[Kinyoun stain]], which dye acid-fast bacilli a bright red that stands out against a blue background.<ref>{{cite web |title=Acid-Fast Stain Protocols |url=http://www.microbelibrary.org/component/resource/laboratory-test/2870-acid-fast-stain-protocols |access-date=26 March 2016 |date=21 August 2013 |url-status=dead |archive-url=https://web.archive.org/web/20111001132818/http://www.microbelibrary.org/component/resource/laboratory-test/2870-acid-fast-stain-protocols |archive-date=1 October 2011 }}</ref> [[Auramine-rhodamine stain]]ing<ref name=Kommareddi_1984>{{cite journal | vauthors = Kommareddi S, Abramowsky CR, Swinehart GL, Hrabak L | title = Nontuberculous mycobacterial infections: comparison of the fluorescent auramine-O and Ziehl-Neelsen techniques in tissue diagnosis | journal = Human Pathology | volume = 15 | issue = 11 | pages = 1085–9 | date = November 1984 | pmid = 6208117 | doi = 10.1016/S0046-8177(84)80253-1 }}</ref> and [[Fluorescence microscope|fluorescence microscopy]]<ref>{{cite book | vauthors = van Lettow M, Whalen C |title=Nutrition and health in developing countries|year=2008|publisher=Humana Press|location=Totowa, N.J. | veditors = Semba RD, Bloem MW |isbn=978-1-934115-24-4 |page=291 |url=https://books.google.com/books?id=RhH6uSQy7a4C&pg=PA291 |edition=2nd|url-status=live|archive-url=https://web.archive.org/web/20150906215906/https://books.google.com/books?id=RhH6uSQy7a4C&pg=PA291|archive-date=6 September 2015}}</ref> are also used. |
|||
If TB bacteria gain entry to the bloodstream from an area of damaged tissue they spread through the body and set up many foci of infection, all appearing as tiny white tubercles in the tissues. This severe form of TB disease is most common in infants and the elderly and is called [[miliary tuberculosis]]. Patients with this [[disseminated]] TB have a fatality rate of approximately 20%, even with intensive treatment.<ref name=Kim_2003>{{cite journal |author=Kim J, Park Y, Kim Y, Kang S, Shin J, Park I, Choi B |title=Miliary tuberculosis and acute respiratory distress syndrome |journal=Int J Tuberc Lung Dis |volume=7 |issue=4 |pages=359-64 |year=2003 | pmid = 12733492}}</ref> |
|||
The [[Mycobacterium tuberculosis complex|''M. tuberculosis'' complex]] (MTBC) includes four other TB-causing [[mycobacterium|mycobacteria]]: ''[[Mycobacterium bovis|M. bovis]]'', ''[[Mycobacterium africanum|M. africanum]]'', ''[[Mycobacterium canettii|M. canettii]]'', and ''[[Mycobacterium microti|M. microti]]''.<ref>{{cite journal | vauthors = van Soolingen D, Hoogenboezem T, de Haas PE, Hermans PW, Koedam MA, Teppema KS, Brennan PJ, Besra GS, Portaels F, Top J, Schouls LM, van Embden JD | title = A novel pathogenic taxon of the Mycobacterium tuberculosis complex, Canetti: characterization of an exceptional isolate from Africa | journal = International Journal of Systematic Bacteriology | volume = 47 | issue = 4 | pages = 1236–45 | date = October 1997 | pmid = 9336935 | doi = 10.1099/00207713-47-4-1236 | doi-access = free }}</ref> ''M. africanum'' is not widespread, but it is a significant cause of tuberculosis in parts of Africa.<ref>{{cite journal | vauthors = Niemann S, Rüsch-Gerdes S, Joloba ML, Whalen CC, Guwatudde D, Ellner JJ, Eisenach K, Fumokong N, Johnson JL, Aisu T, Mugerwa RD, Okwera A, Schwander SK | title = Mycobacterium africanum subtype II is associated with two distinct genotypes and is a major cause of human tuberculosis in Kampala, Uganda | journal = Journal of Clinical Microbiology | volume = 40 | issue = 9 | pages = 3398–405 | date = September 2002 | pmid = 12202584 | pmc = 130701 | doi = 10.1128/JCM.40.9.3398-3405.2002 }}</ref><ref>{{cite journal | vauthors = Niobe-Eyangoh SN, Kuaban C, Sorlin P, Cunin P, Thonnon J, Sola C, Rastogi N, Vincent V, Gutierrez MC | title = Genetic biodiversity of Mycobacterium tuberculosis complex strains from patients with pulmonary tuberculosis in Cameroon | journal = Journal of Clinical Microbiology | volume = 41 | issue = 6 | pages = 2547–53 | date = June 2003 | pmid = 12791879 | pmc = 156567 | doi = 10.1128/JCM.41.6.2547-2553.2003 }}</ref> ''M. bovis'' was once a common cause of tuberculosis, but the introduction of [[pasteurisation|pasteurized milk]] has almost eliminated this as a public health problem in developed countries.<ref name=Robbins/><ref>{{cite journal | vauthors = Thoen C, Lobue P, de Kantor I | title = The importance of Mycobacterium bovis as a zoonosis | journal = Veterinary Microbiology | volume = 112 | issue = 2–4 | pages = 339–45 | date = February 2006 | pmid = 16387455 | doi = 10.1016/j.vetmic.2005.11.047 }}</ref> ''M. canettii'' is rare and seems to be limited to the [[Horn of Africa]], although a few cases have been seen in African emigrants.<ref>{{cite book| vauthors = Acton QA |title=Mycobacterium Infections: New Insights for the Healthcare Professional|year=2011|publisher=ScholarlyEditions|isbn=978-1-4649-0122-5|page=1968|url=https://books.google.com/books?id=g2iFfV6uEuAC&pg=PA1968|url-status=live|archive-url=https://web.archive.org/web/20150906201531/https://books.google.com/books?id=g2iFfV6uEuAC&pg=PA1968|archive-date=6 September 2015}}</ref><ref>{{cite journal | vauthors = Pfyffer GE, Auckenthaler R, van Embden JD, van Soolingen D | title = Mycobacterium canettii, the smooth variant of M. tuberculosis, isolated from a Swiss patient exposed in Africa | journal = Emerging Infectious Diseases | volume = 4 | issue = 4 | pages = 631–4 | date = 1998 | pmid = 9866740 | pmc = 2640258 | doi = 10.3201/eid0404.980414 }}</ref> ''M. microti'' is also rare and is seen almost only in immunodeficient people, although its [[prevalence]] may be significantly underestimated.<ref>{{cite journal | vauthors = Panteix G, Gutierrez MC, Boschiroli ML, Rouviere M, Plaidy A, Pressac D, Porcheret H, Chyderiotis G, Ponsada M, Van Oortegem K, Salloum S, Cabuzel S, Bañuls AL, Van de Perre P, Godreuil S | title = Pulmonary tuberculosis due to Mycobacterium microti: a study of six recent cases in France | journal = Journal of Medical Microbiology | volume = 59 | issue = Pt 8 | pages = 984–989 | date = August 2010 | pmid = 20488936 | doi = 10.1099/jmm.0.019372-0 | doi-access = free }}</ref> |
|||
In many patients the infection waxes and wanes. Tissue destruction and necrosis are balanced by healing and [[fibrosis]].<ref name=Grosset/> Affected tissue is replaced by scarring and cavities filled with cheese-like white necrotic material. During active disease, some of these cavities are joined to the air passages [[bronchi]] and this material can be coughed up. It contains living bacteria and can therefore pass on infection. Treatment with appropriate [[antibiotic]]s kills bacteria and allows healing to take place. Upon cure, affected areas are eventually replaced by scar tissue.<ref name=Grosset/> |
|||
Other known pathogenic mycobacteria include ''[[Mycobacterium leprae|M. leprae]]'', ''[[Mycobacterium avium complex|M. avium]]'', and ''[[Mycobacterium kansasii|M. kansasii]]''. The latter two species are classified as "[[nontuberculous mycobacteria]]" (NTM) or atypical mycobacteria. NTM cause neither TB nor [[leprosy]], but they do cause lung diseases that resemble TB.<ref name=ALA_1997>{{cite journal | author = American Thoracic Society | title = Diagnosis and treatment of disease caused by nontuberculous mycobacteria | journal = American Journal of Respiratory and Critical Care Medicine | volume = 156 | issue = 2 Pt 2 | pages = S1–25 | date = August 1997 | pmid = 9279284 | doi = 10.1164/ajrccm.156.2.atsstatement }}</ref>[[File:TB poster.jpg|thumb|Public health campaigns in the 1920s tried to halt the spread of TB.]] |
|||
==Diagnosis== |
|||
{{details|Tuberculosis diagnosis}} |
|||
[[Image:Mantoux tuberculin skin test.jpg|thumb|right|350px|[[Mantoux test|Mantoux tuberculin skin test]]]] |
|||
=== Transmission === |
|||
Tuberculosis can be a difficult disease to diagnose, due mainly to the difficulty in culturing this slow-growing organism in the laboratory. A complete medical evaluation for TB must include a medical history, a chest X-ray, and a physical examination. [[Tuberculosis radiology]] is used in the diagnosis of TB. It may also include a [[Mantoux test|tuberculin skin test,]] a [[serological]] test, microbiological smears and cultures. The interpretation of the tuberculin skin test depends upon the person's risk factors for infection and progression to TB disease, such as exposure to other cases of TB or immunosuppression.<ref name=CDCcourse/> |
|||
When people with active pulmonary TB cough, sneeze, speak, sing, or spit, they expel infectious [[aerosol]] droplets 0.5 to 5.0 [[μm]] in diameter. A single sneeze can release up to 40,000 droplets.<ref name=Cole_1998>{{cite journal | vauthors = Cole EC, Cook CE | title = Characterization of infectious aerosols in health care facilities: an aid to effective engineering controls and preventive strategies | journal = American Journal of Infection Control | volume = 26 | issue = 4 | pages = 453–64 | date = August 1998 | pmid = 9721404 | doi = 10.1016/S0196-6553(98)70046-X | pmc = 7132666 }}</ref> Each one of these droplets may transmit the disease, since the infectious dose of tuberculosis is very small (the inhalation of fewer than 10 bacteria may cause an infection).<ref>{{cite journal | vauthors = Nicas M, Nazaroff WW, Hubbard A | title = Toward understanding the risk of secondary airborne infection: emission of respirable pathogens | journal = Journal of Occupational and Environmental Hygiene | volume = 2 | issue = 3 | pages = 143–54 | date = March 2005 | pmid = 15764538 | doi = 10.1080/15459620590918466 | pmc = 7196697 }}</ref> |
|||
Currently, latent infection is diagnosed in a non-immunized person by a tuberculin skin test, which yields a delayed hypersensitivity type response to [[Mantoux test|purified protein derivative]]s of ''M. tuberculosis''. Those immunized for TB or with past-cleared infection will respond with delayed hypersensitivity parallel to those currently in a state of infection and thus the test must be used with caution, particularly with regard to persons from countries where TB immunization is common.<ref name=Rothel_2005>{{cite journal |author=Rothel J, Andersen P |title=Diagnosis of latent Mycobacterium tuberculosis infection: is the demise of the Mantoux test imminent? |journal=Expert Rev Anti Infect Ther |volume=3 |issue=6 |pages=981-93 |year=2005 | pmid = 16307510}}</ref> New TB tests are being developed that offer the hope of cheap, fast and more accurate TB testing. These use [[polymerase chain reaction]] detection of bacterial DNA and antibody assays to detect the release of [[interferon gamma]] in response to mycobacteria.<ref nameNahid_2006>{{cite journal |author=Nahid P, Pai M, Hopewell P |title=Advances in the diagnosis and treatment of tuberculosis |journal=Proc Am Thorac Soc |volume=3 |issue=1 |pages=103-10 |year=2006 | pmid = 16493157}}</ref> Rapid and inexpensive diagnosis will be particularly valuable in the developing world. |
|||
==== Risk of transmission ==== |
|||
==Progression== |
|||
Progression from TB infection to TB disease occurs when the TB bacilli overcome the immune system defenses and begin to multiply. In primary TB disease—1 to 5% of cases—this occurs soon after infection. However, in the majority of cases, a latent infection occurs that has no obvious symptoms. These dormant bacilli can produce tuberculosis in 2 to 23% of these latent cases, often many years after infection.<ref name=Parrish_1998>{{cite journal |author=Parrish N, Dick J, Bishai W |title=Mechanisms of latency in Mycobacterium tuberculosis |journal=Trends Microbiol |volume=6 |issue=3 |pages=107-12 |year=1998 | pmid = 9582936}}</ref> The risk of reactivation increases with immunosuppression, such as that caused by infection with HIV. In patients co-infected with ''M. tuberculosis'' and HIV, the risk of reactivation increases to 10% per year.<ref name =TDRreport/> |
|||
People with prolonged, frequent, or close contact with people with TB are at particularly high risk of becoming infected, with an estimated 22% infection rate.<ref name="Ahmed_2011">{{cite journal | vauthors = Ahmed N, Hasnain SE | title = Molecular epidemiology of tuberculosis in India: moving forward with a systems biology approach | journal = Tuberculosis | volume = 91 | issue = 5 | pages = 407–13 | date = September 2011 | pmid = 21514230 | doi = 10.1016/j.tube.2011.03.006 }}</ref> A person with active but untreated tuberculosis may infect 10–15 (or more) other people per year.<ref name="WHO2012data" /> Transmission should occur from only people with active TB – those with latent infection are not thought to be contagious.<ref name="Robbins" /> The probability of transmission from one person to another depends upon several factors, including the number of infectious droplets expelled by the carrier, the effectiveness of ventilation, the duration of exposure, the [[virulence]] of the ''M. tuberculosis'' [[strain (biology)|strain]], the level of immunity in the uninfected person, and others.<ref name="CDCcourse">{{cite web|publisher=[[Centers for Disease Control and Prevention]] (CDC), Division of Tuberculosis Elimination|url=https://www.cdc.gov/tb/education/corecurr/pdf/corecurr_all.pdf|title=Core Curriculum on Tuberculosis: What the Clinician Should Know|page=24|edition=5th|year=2011|url-status=live|archive-url=https://web.archive.org/web/20120519141115/http://www.cdc.gov/tb/education/corecurr/pdf/corecurr_all.pdf|archive-date=19 May 2012}}</ref> The cascade of person-to-person spread can be circumvented by segregating those with active ("overt") TB and putting them on anti-TB drug regimens. After about two weeks of effective treatment, subjects with [[Antibiotic resistance|nonresistant]] active infections generally do not remain contagious to others.<ref name="Ahmed_2011" /> If someone does become infected, it typically takes three to four weeks before the newly infected person becomes infectious enough to transmit the disease to others.<ref>{{cite web|url=http://www.mayoclinic.com/health/tuberculosis/DS00372/DSECTION=3|title=Causes of Tuberculosis|access-date=19 October 2007|date=21 December 2006|publisher=[[Mayo Clinic]]|url-status=live|archive-url=https://web.archive.org/web/20071018051807/http://www.mayoclinic.com/health/tuberculosis/DS00372/DSECTION%3D3|archive-date=18 October 2007}}</ref> |
|||
Other conditions that increase risk include drug injection, mainly due to the lifestyle of [[IV drug users]]; recent TB infection or a history of inadequately treated TB; chest X-ray suggestive of previous TB, showing fibrotic lesions and nodules; [[diabetes mellitus]]; [[silicosis]]; prolonged [[corticosteroid]] therapy and other immunosuppressive therapy; head and neck cancers; [[hematology|hematologic]] and [[Reticuloendothelial system|reticuloendothelial]] diseases, such as [[leukemia]] and [[Hodgkin's lymphoma|Hodgkin's disease;]] end-stage kidney disease; intestinal bypass or [[gastrectomy]]; chronic [[malabsorption]] syndromes; or low body weight.<ref name=CDCcourse/> |
|||
=== Risk factors === |
|||
[[Twin study|Twin studies]] in the 1950's showed that the course of TB infection was highly dependent on the genetics of the patient. At that time, it was rare that one identical twin would die and the other live.<ref>New Scientist, 16 June 2007 [http://www.newscientist.com/article/mg19426086.100-this-week-50-years-ago.html]</ref> |
|||
{{Main|Risk factors for tuberculosis}} |
|||
A number of factors make individuals more susceptible to TB infection and/or disease.<ref name=":0">{{cite journal | vauthors = Narasimhan P, Wood J, Macintyre CR, Mathai D | title = Risk factors for tuberculosis | journal = Pulmonary Medicine | volume = 2013 | pages = 828939 | date = 2013 | pmid = 23476764 | pmc = 3583136 | doi = 10.1155/2013/828939 | doi-access = free }}</ref> |
|||
==== Active disease risk ==== |
|||
Some drugs, including [[rheumatoid arthritis]] drugs that work by blocking [[tumor necrosis factor-alpha]] (an inflammation-causing [[cytokine]]), raise the risk of activating a latent infection due to the importance of this cytokine in the immune defense against TB.<ref name=Mutlu_2006>{{cite journal |author=Mutlu G, Mutlu E, Bellmeyer A, Rubinstein I |title=Pulmonary adverse events of anti-tumor necrosis factor-alpha antibody therapy |journal=Am J Med |volume=119 |issue=8 |pages=639-46 |year=2006 | pmid = 16887405}}</ref> |
|||
The most important risk factor globally for developing active TB is concurrent HIV infection; 13% of those with TB are also infected with HIV.<ref name="WHO2011">{{cite web|year=2011|title=The sixteenth global report on tuberculosis|url=https://www.who.int/tb/publications/global_report/2011/gtbr11_executive_summary.pdf|url-status=dead|archive-url=https://web.archive.org/web/20120906223650/http://www.who.int/tb/publications/global_report/2011/gtbr11_executive_summary.pdf|archive-date=6 September 2012|publisher=World Health Organization (WHO)}}</ref> This is a particular problem in [[sub-Saharan Africa]], where HIV infection rates are high.<ref>{{cite web |title = Global tuberculosis control–surveillance, planning, financing WHO Report 2006 |url= https://www.who.int/tb/publications/global_report/en/index.html |url-status=live |archive-url= https://web.archive.org/web/20061212123736/http://www.who.int/tb/publications/global_report/en/index.html|archive-date=12 December 2006|access-date=13 October 2006|publisher=World Health Organization (WHO) }}</ref><ref>{{cite journal|vauthors=Chaisson RE, Martinson NA|date=March 2008|title=Tuberculosis in Africa – combating an HIV-driven crisis|journal=The New England Journal of Medicine|volume=358|issue=11|pages=1089–92|doi=10.1056/NEJMp0800809|pmid=18337598|doi-access=free}}</ref> Of those without HIV infection who are infected with tuberculosis, about 5–10% develop active disease during their lifetimes;<ref name="Pet2005" /> in contrast, 30% of those co-infected with HIV develop the active disease.<ref name="Pet2005" /> |
|||
==Treatment== |
|||
{{details|Tuberculosis treatment}} |
|||
Treatment for TB uses [[antibiotics]] to kill the bacteria. The two antibiotics most commonly used are [[rifampicin]] and [[isoniazid]]. However, instead of the short course of antibiotics typically used to cure other bacterial infections, TB requires much longer periods of treatment (around 6 to 12 months) to entirely eliminate mycobacteria from the body.<ref name=CDCcourse/> Latent TB treatment usually uses a single antibiotic, while active TB disease is best treated with combinations of several antibiotics, to reduce the risk of the bacteria developing [[antibiotic resistance]].<ref name=OBrien>{{cite journal |author=O'Brien R |title=Drug-resistant tuberculosis: etiology, management and prevention |journal=Semin Respir Infect |volume=9 |issue=2 |pages=104-12 |year=1994 | pmid = 7973169}}</ref> People with these latent infections are treated to prevent them from progressing to active TB disease later in life. However, treatment using Rifampin and Pyrazinamide is not risk-free. The Centers for Disease Control and Prevention (CDC) notified healthcare professionals of revised recommendations against the use of rifampin plus pyrazinamide for treatment of latent tuberculosis infection, due to high rates of hospitalization and death from liver injury associated with the combined use of these drugs.<ref name=MMWR_2003>{{cite journal |author= |title=Update: adverse event data and revised American Thoracic Society/CDC recommendations against the use of rifampin and pyrazinamide for treatment of latent tuberculosis infection—United States, 2003 |journal=MMWR Morb Mortal Wkly Rep |volume=52 |issue=31 |pages=735-9 |year=2003 |url=http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5231a4.htm | pmid = 12904741}}</ref> |
|||
Use of certain medications, such as [[corticosteroids]] and [[infliximab]] (an anti-αTNF monoclonal antibody), is another important risk factor, especially in the [[developed world]].<ref name="Lancet11" /> |
|||
Drug resistant tuberculosis is transmitted in the same way as regular TB. Primary resistance occurs in persons who are infected with a resistant strain of TB. A patient with fully-susceptible TB develops secondary resistance (acquired resistance) during TB therapy because of inadequate treatment, not taking the prescribed regimen appropriately, or using low quality medication.<ref name=OBrien/> Drug-resistant TB is a public health issue in many developing countries, as treatment is longer and requires more expensive drugs. [[Multi-drug resistant TB]] ('''MDR-TB''') is defined as resistance to the two most effective first line TB drugs: [[rifampicin]] and [[isoniazid]]. [[Extensively drug-resistant tuberculosis|Extensively drug-resistant TB]] ('''XDR-TB''') is also resistant to three or more of the six classes of second-line drugs.<ref name="MMWR2006"/> |
|||
Other risk factors include: [[alcoholism]],<ref name="Lancet11" /> [[diabetes mellitus]] (3-fold increased risk),<ref>{{cite journal | vauthors = Restrepo BI | title = Convergence of the tuberculosis and diabetes epidemics: renewal of old acquaintances | journal = Clinical Infectious Diseases | volume = 45 | issue = 4 | pages = 436–438 | date = August 2007 | pmid = 17638190 | pmc = 2900315 | doi = 10.1086/519939 }}</ref> [[silicosis]] (30-fold increased risk),<ref name="table3">{{cite journal | vauthors = | title = Targeted tuberculin testing and treatment of latent tuberculosis infection. American Thoracic Society | journal = MMWR. Recommendations and Reports | volume = 49 | issue = RR-6 | pages = 1–51 | date = June 2000 | pmid = 10881762 | url = https://www.cdc.gov/mmwr/preview/mmwrhtml/rr4906a1.htm#tab3 | url-status = live | archive-url = https://web.archive.org/web/20041217172736/http://www.cdc.gov/MMWR/preview/mmwrhtml/rr4906a1.htm#tab3 | archive-date = 17 December 2004 }}</ref> [[cigarette|tobacco smoking]] (2-fold increased risk),<ref>{{cite journal | vauthors = van Zyl Smit RN, Pai M, Yew WW, Leung CC, Zumla A, Bateman ED, Dheda K | title = Global lung health: the colliding epidemics of tuberculosis, tobacco smoking, HIV and COPD | journal = The European Respiratory Journal | volume = 35 | issue = 1 | pages = 27–33 | date = January 2010 | pmid = 20044459 | pmc = 5454527 | doi = 10.1183/09031936.00072909 | quote = These analyses indicate that smokers are almost twice as likely to be infected with TB and to progress to active disease (RR of about 1.5 for latent TB infection (LTBI) and RR of ~2.0 for TB disease). Smokers are also twice as likely to die from TB (RR of about 2.0 for TB mortality), but data are difficult to interpret because of heterogeneity in the results across studies. | doi-access = free }}</ref> [[indoor air quality|indoor air pollution]], malnutrition, young age,<ref name=":0" /> recently acquired TB infection, recreational drug use, severe kidney disease, low body weight, organ transplant, head and neck cancer,<ref>{{Cite web|date=March 18, 2016 |title=TB Risk Factors |url=https://www.cdc.gov/tb/topic/basics/risk.htm|access-date=25 August 2020|website=CDC |language=en-us|archive-date=30 August 2020|archive-url=https://web.archive.org/web/20200830234002/https://www.cdc.gov/tb/topic/basics/risk.htm|url-status=live}}</ref> and [[genetic susceptibility]]<ref>{{cite journal | vauthors = Möller M, Hoal EG | title = Current findings, challenges and novel approaches in human genetic susceptibility to tuberculosis | journal = Tuberculosis | volume = 90 | issue = 2 | pages = 71–83 | date = March 2010 | pmid = 20206579 | doi = 10.1016/j.tube.2010.02.002 }}</ref> (the overall importance of genetic risk factors remains undefined<ref name="Lancet11" />). |
|||
==Prevention== |
|||
TB prevention and control takes two parallel approaches. In the first, people with TB and their contacts are identified and then treated. Identification of infections often involves testing high-risk groups for TB. In the second approach, children are [[vaccination|vaccinated]] to protect them from TB. Unfortunately, no [[vaccine]] is available that provides reliable protection for adults. However, in tropical areas where the incidence of atypical mycobacteria is high, exposure to [[nontuberculous mycobacteria]] gives some protection against TB.<ref name=Fine_2001>{{cite journal |author=Fine P, Floyd S, Stanford J, Nkhosa P, Kasunga A, Chaguluka S, Warndorff D, Jenkins P, Yates M, Ponnighaus J |title=Environmental mycobacteria in northern Malawi: implications for the epidemiology of tuberculosis and leprosy |journal=Epidemiol Infect |volume=126 |issue=3 |pages=379-87 |year=2001 | pmid = 11467795}}</ref> |
|||
==== Infection susceptibility ==== |
|||
===Vaccines=== |
|||
Many countries use [[Bacillus Calmette-Guérin|BCG]] vaccine as part of their TB control programs, especially for infants. This was the first vaccine for TB and developed at the [[Pasteur Institute]] in [[France]] between 1905 and 1921.<ref name=Bonah>{{cite journal |author=Bonah C |title=The 'experimental stable' of the BCG vaccine: safety, efficacy, proof, and standards, 1921–1933 |journal=Stud Hist Philos Biol Biomed Sci |volume=36 |issue=4 |pages=696–721 |year=2005 | pmid = 16337557}}</ref> However, mass vaccination with BCG did not start until after [[World War II]].<ref name=Comstock>{{cite journal |author=Comstock G |title=The International Tuberculosis Campaign: a pioneering venture in mass vaccination and research |journal=Clin Infect Dis |volume=19 |issue=3 |pages=528-40 |year=1994 | pmid = 7811874}}</ref> The protective efficacy of BCG for preventing serious forms of TB (e.g. [[meningitis]]) in children is greater than 80%; its protective efficacy for preventing pulmonary TB in adolescents and adults is variable, ranging from 0 to 80%.<ref name=Bannon_1999>{{cite journal |author=Bannon M |title=BCG and tuberculosis |journal=Arch Dis Child |volume=80 |issue=1 |pages=80-3 |year=1999 | pmid = 10325767}}</ref> |
|||
Tobacco smoking increases the risk of infections (in addition to increasing the risk of active disease and death). Additional factors increasing infection susceptibility include young age.<ref name=":0" /> |
|||
In [[South Africa]], the country with the highest prevalence of TB, BCG is given to all children under the age of three.<ref>[http://www.who.int/immunization_monitoring/data/south_africa.pdf#search=%22BCG%20africa%22 WHO/UNICEF Review of National Immunization Coverage 1980–2005: South Africa] (PDF). World Health Organization (August 2006). Retrieved on [[2007-06-08]].</ref> However, the effectiveness of BCG is lower in areas where mycobacteria are less [[prevalence|prevalent]], therefore BCG is not given to the entire population in these countries. In the USA, for example, BCG vaccine is not recommended except for people who meet specific criteria:<ref name=CDCcourse/> |
|||
*Infants or children with negative skin-test result who are continually exposed to untreated or ineffectively treated patients or will be continually exposed to [[Multidrug resistance|multidrug-resistant]] TB. |
|||
*Healthcare workers considered on an individual basis in settings in which high percentage of MDR-TB patients has been found, transmission of MDR-TB is likely, and TB control precautions have been implemented and not successful. |
|||
== Pathogenesis == |
|||
Several new vaccines to prevent TB infection are being developed. The first [[recombinant]] tuberculosis [[vaccine]] entered [[clinical trial]]s in the United States in 2004, sponsored by the [[National Institute of Allergy and Infectious Diseases]] (NIAID).<ref>[[National Institute of Allergy and Infectious Diseases]] (NIAID).[http://www2.niaid.nih.gov/newsroom/releases/corixatbvac.htm First U.S. Tuberculosis Vaccine Trial in 60 Years Begins.] ''National Institutes of Health News'' 26 January 2004. Retrieved on 8 May 2006.</ref> A 2005 study showed that a [[DNA vaccine|DNA TB vaccine]] given with conventional [[chemotherapy]] can accelerate the disappearance of bacteria as well as protect against re-infection in mice; it may take four to five years to be available in humans.<ref name=Ha_2005>{{cite journal |author=Ha S, Jeon B, Youn J, Kim S, Cho S, Sung Y |title=Protective effect of DNA vaccine during chemotherapy on reactivation and reinfection of Mycobacterium tuberculosis |journal=Gene Ther |volume=12 |issue=7 |pages=634-8 |year=2005 | pmid = 15690060}}</ref> A very promising TB vaccine, [[MVA85A]], is currently in [[clinical trial|phase II trials]] in South Africa by a group led by [[Oxford University]],<ref name=Ibanga_2006>{{cite journal |author=Ibanga H, Brookes R, Hill P, Owiafe P, Fletcher H, Lienhardt C, Hill A, Adegbola R, McShane H |title=Early clinical trials with a new tuberculosis vaccine, MVA85A, in tuberculosis-endemic countries: issues in study design |journal=Lancet Infect Dis |volume=6 |issue=8 |pages=522-8 |year=2006 |url=http://linkinghub.elsevier.com/retrieve/pii/S1473309906705527| pmid = 16870530}}</ref> and is based on a genetically modified [[vaccinia]] virus. Because of the limitations of current vaccines, researchers and policymakers are promoting new economic models of vaccine development including prizes, tax incentives and [[advance market commitments]].<ref>Webber, David and Kremer, Michael. [http://www.who.int/bulletin/archives/79(8)735.pdf Stimulating Industrial R&D for Neglected Infectious Diseases: Economic Perspectives (PDF).] ''Bulletin of the World Health Organization'' 79(8), 2001, pp. 693–801.</ref><ref>Barder, Owen; Kremer, Michael; Williams, Heidi. [http://www.bepress.com/ev/vol3/iss3/art1 "Advance Market Commitments: A Policy to Stimulate Investment in Vaccines for Neglected Diseases,"] ''The Economists' Voice'', Vol. 3 (2006) Issue 3.</ref> |
|||
[[File:Carswell-Tubercle.jpg|thumb|upright|[[Robert Carswell (pathologist)|Robert Carswell]]'s illustration of tubercle<ref name="GoodCooper1835">{{cite book| vauthors = Good JM, Cooper S, Doane AS |title=The Study of Medicine|url=https://books.google.com/books?id=K906AQAAMAAJ&pg=PA32|year=1835|publisher=Harper|page=32|url-status=live|archive-url=https://web.archive.org/web/20160810194616/https://books.google.com/books?id=K906AQAAMAAJ&pg=PA32|archive-date=10 August 2016}}</ref>]] |
|||
==Epidemiology== |
|||
[[Image:TB incidence.png|thumb|350px|Annual number of new reported TB cases. Data from WHO.<ref name=WHOreport>[[World Health Organization]] (WHO). [http://www.who.int/tb/publications/global_report/en/index.html Global tuberculosis control - surveillance, planning, financing WHO Report 2006.] Retrieved on 13 October 2006.</ref>]][[Image:World tb2005.png|thumb|350px|World TB incidence. Cases per 100,000; Red = >300, orange = 200–300; yellow = 100–200; green 50–100 and grey <50. Data from WHO, 2006.<ref name=WHOreport>[[World Health Organization]] (WHO). [http://www.who.int/tb/publications/global_report/en/index.html Global tuberculosis control - surveillance, planning, financing WHO Report 2006.] Retrieved on 13 October 2006.</ref>]]According to the World Health Organization (WHO), nearly 2 billion people—one–third of the world's population—have tuberculosis.<ref>[[National Institute of Allergy and Infectious Diseases]] (NIAID). [http://www.niaid.nih.gov/publications/microbes.htm Microbes in Sickness and in Health.] 26 October 2005. Retrieved on 3 October 2006. "According to the World Health Organization (WHO), nearly 2 billion people, one-third of the world's population, have TB."</ref> Annually, 8 million people become ill with tuberculosis, and 2 million people die from the disease worldwide.<ref name=CDC>[[Centers for Disease Control]]. [http://www.cdc.gov/od/oc/Media/pressrel/fs050317.htm Fact Sheet: Tuberculosis in the United States.] 17 March 2005, Retrieved on 6 October 2006.</ref> In 2004, around 14.6 million people had active TB disease with 9 million new cases. The annual [[Incidence (epidemiology)|incidence]] rate varies from 356 per 100,000 in [[Africa]] to 41 per 100,000 in the [[Americas]].<ref name="WHO2004data"/> Tuberculosis is the world's greatest infectious killer of women of reproductive age and the leading cause of death among people with [[HIV]]/[[AIDS]].<ref>Stop TB Partnership. [http://www.prnewswire.co.uk/cgi/news/release?id=95088 London tuberculosis rates now at Third World proportions.] ''PR Newswire Europe Ltd.'' 4 December 2002. Retrieved on 3 October 2006.</ref> |
|||
About 90% of those infected with ''M. tuberculosis'' have [[asymptomatic]], latent TB infections (sometimes called LTBI),<ref name=Book90>{{cite book| vauthors = Skolnik R |title=Global health 101|year=2011|publisher=Jones & Bartlett Learning|location=Burlington, MA|isbn=978-0-7637-9751-5|page=[https://archive.org/details/globalhealth1010000skol/page/253 253]|url=https://archive.org/details/globalhealth1010000skol|url-access=registration|edition=2nd}}</ref> with only a 10% lifetime chance that the latent infection will progress to overt, active tuberculous disease.<ref name=Arch2009>{{cite book | vauthors = Mainous III AR, Pomeroy C |title=Management of antimicrobials in infectious diseases: impact of antibiotic resistance|year=2009|publisher=Humana Press|location=Totowa, NJ|isbn=978-1-60327-238-4|page=74|url=https://books.google.com/books?id=hwVFAPLYznsC&pg=PA74|edition=2nd rev.|url-status=live|archive-url=https://web.archive.org/web/20150906224212/https://books.google.com/books?id=hwVFAPLYznsC&pg=PA74|archive-date=6 September 2015}}</ref> In those with HIV, the risk of developing active TB increases to nearly 10% a year.<ref name=Arch2009/> If effective treatment is not given, the death rate for active TB cases is up to 66%.<ref name=WHO2012data>{{cite web|url=https://www.who.int/mediacentre/factsheets/fs104/en/index.html|title=Tuberculosis Fact sheet N°104|publisher=[[World Health Organization]] (WHO)|date=November 2010|access-date=26 July 2011|url-status=live|archive-url=https://web.archive.org/web/20061004013508/http://www.who.int/mediacentre/factsheets/fs104/en/index.html|archive-date=4 October 2006}}</ref> |
|||
In 2004, the country with the highest incidence of TB was [[South Africa]], with 718 cases per 100,000 people. [[India]] has the largest number of infections, with over 1.8 million cases.<ref name=WHOreport/> In developed countries, tuberculosis is less common and is mainly an urban disease. In the United Kingdom, TB incidences range from 40 per 100,000 in [[London]] to less than 5 per 100,000 in the rural South West of England;<ref>[http://www.statistics.gov.uk/StatBase/ssdataset.asp?vlnk=5963&Pos=1&ColRank=1&Rank=224 Notification rates of tuberculosis: by NHS Regional Office area, 1990-2001: Regional Trends 37] Office for National Statistics Retrieved on 13 October 2006.</ref> the national average is 13 per 100,000. The highest rates in [[Western Europe]] are in [[Portugal]] (42 per 100,000) and [[Spain]] (20 per 100,000). These rates compare with 113 per 100,000 in [[People's Republic of China|China]] and 64 per 100,000 in [[Brazil]]. In the United States, the overall tuberculosis case rate was 4.9 per 100,000 persons in 2004.<ref name=CDC/> |
|||
[[File:Tuberculous epididymitis Low Power.jpg|thumb|Microscopy of tuberculous epididymitis. [[H&E]] stain]] |
|||
The incidence of TB varies with age. In Africa, TB primarily affects adolescents and young adults.<ref>[[World Health Organization]] (WHO). [http://www.who.int/tb/publications/global_report/2006/pdf/full_report_correctedversion.pdf Global Tuberculosis Control Report, 2006] - Annex 1 Profiles of high-burden countries. (PDF) Retrieved on 13 October 2006.</ref> However, in countries where TB has gone from high to low incidence, such as America, TB is mainly a disease of older people.<ref>[[Centers for Disease Control and Prevention]] (CDC). [http://www.cdc.gov/nchstp/tb/pubs/slidesets/surv/surv2005/default.htm 2005 Surveillance Slide Set.] (September 12, 2006) Retrieved on 13 October 2006.</ref> |
|||
TB infection begins when the mycobacteria reach the [[Pulmonary alveolus|alveolar air sacs]] of the lungs, where they invade and replicate within [[endosomes]] of alveolar [[macrophages]].<ref name=Robbins/><ref name=Houben>{{cite journal | vauthors = Houben EN, Nguyen L, Pieters J | title = Interaction of pathogenic mycobacteria with the host immune system | journal = Current Opinion in Microbiology | volume = 9 | issue = 1 | pages = 76–85 | date = February 2006 | pmid = 16406837 | doi = 10.1016/j.mib.2005.12.014 }}</ref><ref>{{cite journal | vauthors = Queval CJ, Brosch R, Simeone R | title = Mycobacterium tuberculosis | journal = Frontiers in Microbiology | volume = 8 | page= 2284 | year = 2017 | pmid = 29218036 | pmc = 5703847 | doi = 10.3389/fmicb.2017.02284 | doi-access = free }}</ref> Macrophages identify the bacterium as foreign and attempt to eliminate it by [[phagocytosis]]. During this process, the bacterium is enveloped by the macrophage and stored temporarily in a membrane-bound vesicle called a phagosome. The phagosome then combines with a lysosome to create a phagolysosome. In the phagolysosome, the cell attempts to use [[reactive oxygen species]] and acid to kill the bacterium. However, ''M. tuberculosis'' has a thick, waxy [[mycolic acid]] capsule that protects it from these toxic substances. ''M. tuberculosis'' is able to reproduce inside the macrophage and will eventually kill the immune cell. |
|||
There are a number of known factors that make people more susceptible to TB infection: worldwide the most important of these is [[HIV]]. Co-infection with HIV is a particular problem in [[Sub-Saharan Africa]], due to the high incidence of HIV in these countries.<ref name=WHOreport/> Smoking more than 20 [[cigarette]]s a day also increases the risk of TB by two- to four-times.<ref>{{cite journal |
|||
|title=Smoking and tuberculosis: the epidemiological association and pathogenesis |
|||
|author=Davies PDO, Yew WW, Ganguly D, ''et al.'' |
|||
|year=2006 |
|||
|volume=100 |
|||
|pages=291–8 |
|||
|journal=Trans R Soc Trop Med Hyg |
|||
|pmid=16325875}}</ref> Diabetes mellitus is also an important risk factor that is growing in importance in developing countries.<ref>{{cite journal |
|||
|author=Restrepo BI |
|||
|title=Convergence of the tuberculosis and diabetes epidemics: renewal of old acquaintances |
|||
|journal=Clin Infect Dis |
|||
|year=2007 |
|||
|volume=45 |
|||
|pages=436–8 |
|||
|url=http://www.journals.uchicago.edu/CID/journal/issues/v45n4/51190/51190.html}}</ref> |
|||
The primary site of infection in the lungs, known as the [[Ghon focus]], is generally located in either the upper part of the lower lobe, or the lower part of the [[lung|upper lobe]].<ref name=Robbins/> Tuberculosis of the lungs may also occur via infection from the blood stream. This is known as a [[Simon focus]] and is typically found in the top of the lung.<ref>{{cite book| vauthors = Khan MR |title=Essence of Paediatrics|year=2011|publisher=Elsevier India|isbn=978-81-312-2804-3|page=401|url=https://books.google.com/books?id=gERCc6KTxwoC&pg=PA401|url-status=live|archive-url=https://web.archive.org/web/20150906193259/https://books.google.com/books?id=gERCc6KTxwoC&pg=PA401|archive-date=6 September 2015}}</ref> This hematogenous transmission can also spread infection to more distant sites, such as peripheral lymph nodes, the kidneys, the brain, and the bones.<ref name=Robbins/><ref name=Herrmann_2005>{{cite journal | vauthors = Herrmann JL, Lagrange PH | title = Dendritic cells and Mycobacterium tuberculosis: which is the Trojan horse? | journal = Pathologie-Biologie | volume = 53 | issue = 1 | pages = 35–40 | date = February 2005 | pmid = 15620608 | doi = 10.1016/j.patbio.2004.01.004 }}</ref> All parts of the body can be affected by the disease, though for unknown reasons it rarely affects the [[heart]], [[skeletal muscle]]s, [[pancreas]], or [[thyroid]].<ref>{{cite journal | vauthors = Agarwal R, Malhotra P, Awasthi A, Kakkar N, Gupta D | title = Tuberculous dilated cardiomyopathy: an under-recognized entity? | journal = BMC Infectious Diseases | volume = 5 | issue = 1 | pages = 29 | date = April 2005 | pmid = 15857515 | pmc = 1090580 | doi = 10.1186/1471-2334-5-29 | doi-access = free }}</ref> |
|||
==History== |
|||
[[Image:Mummy at British Museum.jpg|left|thumb|300px|Tubercular decay has been found in the spines of [[Egypt]]ian [[mummy|mummies]]. Pictured: Egyptian mummy in the British Museum]] |
|||
Tuberculosis is classified as one of the [[granuloma]]tous inflammatory diseases. [[Macrophage]]s, [[epithelioid cell]]s, [[T cell|T lymphocytes]], [[B cell|B lymphocytes]], and [[fibroblast]]s <!-- are among the cells that --> aggregate to form granulomas, with [[lymphocytes]] surrounding the infected macrophages. When other macrophages attack the infected macrophage, they fuse together to form a giant multinucleated cell in the alveolar lumen. The granuloma may prevent dissemination of the mycobacteria and provide a local environment for interaction of cells of the immune system.<ref name=Grosset /> However, more recent evidence suggests that the bacteria use the granulomas to avoid destruction by the host's immune system. Macrophages and [[dendritic cell]]s in the granulomas are unable to present antigen to lymphocytes; thus the immune response is suppressed.<ref>{{cite journal | vauthors = Bozzano F, Marras F, De Maria A | title = Immunology of tuberculosis | journal = Mediterranean Journal of Hematology and Infectious Diseases | volume = 6 | issue = 1 | page= e2014027 | year = 2014 | pmid = 24804000 | pmc = 4010607 | doi = 10.4084/MJHID.2014.027 }}</ref> Bacteria inside the granuloma can become dormant, resulting in latent infection. Another feature of the granulomas is the development of abnormal cell death ([[necrosis]]) in the center of [[Tubercle (anatomy)|tubercles]]. To the naked eye, this has the texture of soft, white cheese and is termed [[caseous necrosis]].<ref name=Grosset>{{cite journal | vauthors = Grosset J | title = Mycobacterium tuberculosis in the extracellular compartment: an underestimated adversary | journal = Antimicrobial Agents and Chemotherapy | volume = 47 | issue = 3 | pages = 833–36 | date = March 2003 | pmid = 12604509 | pmc = 149338 | doi = 10.1128/AAC.47.3.833-836.2003 }}</ref> |
|||
Tuberculosis has been present in humans since [[Ancient history|antiquity]]. The earliest unambiguous detection of ''Mycobacterium tuberculosis'' is in the remains of bison dated 17,000 years before the present.<ref name=Rothschild_2001>{{cite journal |author=Rothschild B, Martin L, Lev G, Bercovier H, Bar-Gal G, Greenblatt C, Donoghue H, Spigelman M, Brittain D |title=Mycobacterium tuberculosis complex DNA from an extinct bison dated 17,000 years before the present |journal=Clin Infect Dis |volume=33 |issue=3 |pages=305-11 |year=2001 | pmid = 11438894}}</ref> However, whether tuberculosis originated in cattle and then transferred to humans, or diverged from a common ancestor, is currently unclear.<ref name=Pearce-Duvet_2006>{{cite journal |author=Pearce-Duvet J |title=The origin of human pathogens: evaluating the role of agriculture and domestic animals in the evolution of human disease |journal=Biol Rev Camb Philos Soc |volume=81 |issue=3 |pages=369-82 |year=2006 | pmid = 16672105}}</ref> Skeletal remains show prehistoric humans (4000 [[Before Christ|BC]]) had TB, and tubercular decay has been found in the spines of [[mummy|mummies]] from 3000-2400 BC.<ref name=Zink_2003>{{cite journal |author=Zink A, Sola C, Reischl U, Grabner W, Rastogi N, Wolf H, Nerlich A |title=Characterization of Mycobacterium tuberculosis complex DNAs from Egyptian mummies by spoligotyping |journal=J Clin Microbiol |volume=41 |issue=1 |pages=359-67 |year=2003 | pmid = 12517873}}</ref> Phthisis is a Greek term for tuberculosis; around 460 BC, [[Hippocrates]] identified phthisis as the most widespread disease of the times involving coughing up blood and fever, which was almost always fatal.<ref>Hippocrates. [http://web.archive.org/web/20050211173218/http://classics.mit.edu/Hippocrates/aphorisms.mb.txt Aphorisms.] Accessed 07 October 2006.</ref> Genetic studies suggest that TB was present in [[South America]] for about 2,000 years.<ref name=Konomi_2002>{{cite journal |author=Konomi N, Lebwohl E, Mowbray K, Tattersall I, Zhang D |title=Detection of mycobacterial DNA in Andean mummies |journal=J Clin Microbiol |volume=40 |issue=12 |pages=4738–40 |year=2002 | pmid = 12454182}}</ref> In South America, the earliest evidence of tuberculosis is associated with the [[Paracas]]-Caverna culture.<ref>[http://memorias.ioc.fiocruz.br/98sup/6psa.html "South America: Prehistoric Findings"]. ''Memorias do Instituto Oswaldo Cruz'', Vol. 98 (Suppl.I) January 2003. Retrieved on [[2007-02-08]].</ref> |
|||
If TB bacteria gain entry to the blood stream from an area of damaged tissue, they can spread throughout the body and set up many foci of infection, all appearing as tiny, white tubercles in the tissues.<ref>{{cite book| vauthors = Crowley LV |title=An introduction to human disease: pathology and pathophysiology correlations|year=2010|publisher=Jones and Bartlett|location=Sudbury, MA|isbn=978-0-7637-6591-0|page=374|url=https://books.google.com/books?id=TEiuWP4z_QIC&pg=PA374|edition=8th|url-status=live|archive-url=https://web.archive.org/web/20150906193726/https://books.google.com/books?id=TEiuWP4z_QIC&pg=PA374|archive-date=6 September 2015}}</ref> This severe form of TB disease, most common in young children and those with HIV, is called miliary tuberculosis.<ref>{{cite book| vauthors = Harries AD, Maher D, Graham S |title=TB/HIV a Clinical Manual|year=2005|publisher=World Health Organization (WHO)|location=Geneva|isbn=978-92-4-154634-8|page=75|url=https://books.google.com/books?id=8dfhwKaCSxkC&pg=PA75|edition=2nd|url-status=live|archive-url=https://web.archive.org/web/20150906195514/https://books.google.com/books?id=8dfhwKaCSxkC&pg=PA75|archive-date=6 September 2015}}</ref> People with this disseminated TB have a high fatality rate even with treatment (about 30%).<ref name=Gho2008>{{cite book| vauthors = Habermann TM, Ghosh A |title=Mayo Clinic internal medicine: concise textbook|year=2008|publisher=Mayo Clinic Scientific Press|location=Rochester, MN|isbn=978-1-4200-6749-1|page=789|url=https://books.google.com/books?id=YJtodBwNxokC&pg=PA789|url-status=live|archive-url=https://web.archive.org/web/20150906190055/https://books.google.com/books?id=YJtodBwNxokC&pg=PA789|archive-date=6 September 2015}}</ref><ref>{{cite journal | vauthors = Jacob JT, Mehta AK, Leonard MK | title = Acute forms of tuberculosis in adults | journal = The American Journal of Medicine | volume = 122 | issue = 1 | pages = 12–17 | date = January 2009 | pmid = 19114163 | doi = 10.1016/j.amjmed.2008.09.018 }}</ref> |
|||
===Folklore=== |
|||
Before the [[Industrial Revolution]], tuberculosis may sometimes have been regarded as [[vampirism]]. When one member of a family died from it, the other members that were infected would lose their health slowly. People believed that this was caused by the original victim draining the life from the other family members. Furthermore, people who had TB exhibited symptoms similar to what people considered to be vampire traits. People with TB often have symptoms such as red, swollen eyes (which also creates a sensitivity to bright light), pale skin and coughing blood, suggesting the idea that the only way for the afflicted to replenish this loss of blood was by sucking blood.<ref name=Sledzik_1994>{{cite journal |author=Sledzik P, Bellantoni N |title=Brief communication: bioarcheological and biocultural evidence for the New England vampire folk belief |journal=Am J Phys Anthropol |volume=94 |issue=2 |pages=269-74 |year=1994 |url=http://users.net1plus.com/vyrdolak/tableone.htm | pmid = 8085617}}</ref> Another folk belief attributed it to being forced, nightly, to attend [[fairy]] revels, so that the victim wasted away owing to lack of rest; this belief was most common when a strong connection was seen between the fairies and the dead.<ref name=Briggs>[[Katharine Mary Briggs|Katharine Briggs]], ''An Encyclopedia of Fairies'' "Consumption" ([[Pantheon Books]], 1976) p. 80. ISBN 0-394-73467-X</ref> Similarly, but less commonly, it was attributed to the victims being "hagridden"—being transformed into horses by witches (hags) to travel to their nightly meetings, again resulting in a lack of rest.<ref name=Briggs/> |
|||
In many people, the infection waxes and wanes. Tissue destruction and necrosis are often balanced by healing and [[fibrosis]].<ref name=Grosset/> Affected tissue is replaced by scarring and cavities filled with caseous necrotic material. During active disease, some of these cavities are joined to the air passages ([[bronchi]]) and this material can be coughed up. It contains living bacteria and thus can spread the infection. Treatment with appropriate [[antibiotic]]s kills bacteria and allows healing to take place. Upon cure, affected areas are eventually replaced by scar tissue.<ref name=Grosset/> |
|||
TB was romanticized in the nineteenth century. Many at the time believed TB produced feelings of euphoria referred to as "Spes phthisica" or "hope of the consumptive". It was believed that TB sufferers who were artists had bursts of creativity as the disease progressed. It was also believed that TB sufferers acquired a final burst of energy just before they died which made women more beautiful and men more creative.<ref name="StudiesLiteraryImagination-Clark">Lawlor, Clark. "Transatlantic Consumptions: Disease, Fame and Literary Nationalism in the Davidson Sisters, Southey, and Poe". ''Studies in the Literary Imagination'', Fall 2003. Available at [http://findarticles.com/p/articles/mi_qa3822/is_200310/ai_n9310101 findarticles.com.] Retrieved on [[2007-06-08]].</ref> |
|||
{{Clear}} |
|||
== Diagnosis == |
|||
===Study and treatment=== |
|||
{{Main|Tuberculosis diagnosis}} |
|||
Although it was established that the pulmonary form was associated with 'tubercles' by [[Dr Richard Morton]] in 1689,<ref name="WhoNamedIt-Calmette">Who Named It? [http://www.whonamedit.com/doctor.cfm/2413.html Léon Charles Albert Calmette.] Retrieved on 6 October 2006.</ref><ref name="MedHist1970-Trail">{{cite journal |author=Trail R |title=Richard Morton (1637–1698) |journal=Med Hist |volume=14 |issue=2 |pages=166-74 |year=1970 | pmid = 4914685}}</ref> due to the variety of its symptoms, TB was not identified as a single disease until the 1820s and was not named 'tuberculosis' until 1839 by [[Johann Lukas Schönlein|J. L. Schönlein]].<ref>Zur Pathogenie der Impetigines. Auszug aus einer brieflichen Mitteilung an den Herausgeber. [Müller’s] ''Archiv für Anatomie, Physiologie und wissenschaftliche Medicin''. 1839, page 82.</ref> During the years 1838–1845, Dr. John Croghan, the owner of [[Mammoth Cave]], brought a number of tuberculosis sufferers into the cave in the hope of curing the disease with the constant temperature and purity of the cave air: they died within a year.<ref>[http://edition.cnn.com/2004/TRAVEL/DESTINATIONS/02/26/mammoth.cave.ap/index.html Kentucky: Mammoth Cave long on history.] ''[[CNN]]''. 27 February 2004. Accessed 08 October 2006.</ref> The first TB [[sanatorium]] opened in 1859 in [[Görbersdorf|Görbersdorf, Germany]] (today [[Sokołowsko|Sokołowsko, Poland]]) by Hermann Brehmer.<ref name =sanatoria>{{cite journal |author=McCarthy OR |title=The key to the sanatoria |journal=J R Soc Med |volume=94 |issue=8 |pages=413-7 |year=2001 | pmid = 11461990}}</ref> |
|||
[[File:TB in sputum.png|thumb|''M. tuberculosis'' ([[Ziehl-Neelsen stain|stained red]]) in [[sputum]]]] |
|||
=== Active tuberculosis === |
|||
In regard to this claim, ''The Times'' for January 15, 1859, page 5, column 5, carries an advertisement seeking funds for the Bournemouth Sanatorium for Consumption, referring to the balance sheet for the past year, and offering an annual report to prospective donors, implying that this sanatorium was in existence at least in 1858. |
|||
[[Image:RobertKoch.jpg|right|thumb|200px|Dr. Robert Koch discovered the tuberculosis bacilli.]] |
|||
The bacillus causing tuberculosis, ''Mycobacterium tuberculosis'', was identified and described on [[March 24]], [[1882]] by [[Robert Koch]]. He received the [[Nobel Prize in physiology or medicine]] in 1905 for this discovery.<ref>[[Nobel Foundation]]. [http://nobelprize.org/nobel_prizes/medicine/laureates/1905/ The Nobel Prize in Physiology or Medicine 1905.] Accessed 07 October 2006.</ref> Koch did not believe that bovine (cattle) and human tuberculosis were similar, which delayed the recognition of infected milk as a source of infection. Later, this source was eliminated by the [[pasteurization]] process. Koch announced a [[glycerine]] extract of the tubercle bacilli as a "remedy" for tuberculosis in 1890, calling it 'tuberculin'. It was not effective, but was later adapted as a test for pre-symptomatic tuberculosis.<ref name=Waddington_2004>{{cite journal |author=Waddington K |title=To stamp out "so terrible a malady": bovine tuberculosis and tuberculin testing in Britain, 1890–1939 |journal=Med Hist |volume=48 |issue=1 |pages=29–48 |year=2004 | pmid = 14968644}}</ref> |
|||
Diagnosing active tuberculosis based only on signs and symptoms is difficult,<ref name=DiagP2011>{{cite journal | vauthors = Bento J, Silva AS, Rodrigues F, Duarte R | title = [Diagnostic tools in tuberculosis] | journal = Acta Médica Portuguesa | volume = 24 | issue = 1 | pages = 145–54 | date = 2011 | doi = 10.20344/amp.333 | pmid = 21672452 | s2cid = 76156550 | doi-access = free }}</ref> as is diagnosing the disease in those who have a weakened immune system.<ref name=Clinic2009>{{cite journal | vauthors = Escalante P | s2cid = 639982 | title = In the clinic. Tuberculosis | journal = Annals of Internal Medicine | volume = 150 | issue = 11 | pages = ITC61-614; quiz ITV616 | date = June 2009 | pmid = 19487708 | doi = 10.7326/0003-4819-150-11-200906020-01006 }}</ref> A diagnosis of TB should, however, be considered in those with signs of lung disease or [[constitutional symptoms]] lasting longer than two weeks.<ref name=Clinic2009/> A [[chest X-ray]] and multiple [[sputum culture]]s for [[acid-fast bacilli]] are typically part of the initial evaluation.<ref name=Clinic2009/> [[Interferon gamma release assay|Interferon-γ release assays]] (IGRA) and tuberculin skin tests are of little use in most of the developing world.<ref>{{cite journal | vauthors = Metcalfe JZ, Everett CK, Steingart KR, Cattamanchi A, Huang L, Hopewell PC, Pai M | title = Interferon-γ release assays for active pulmonary tuberculosis diagnosis in adults in low- and middle-income countries: systematic review and meta-analysis | journal = The Journal of Infectious Diseases | volume = 204 | issue = suppl_4 | pages = S1120-9 | date = November 2011 | pmid = 21996694 | pmc = 3192542 | doi = 10.1093/infdis/jir410 }}</ref><ref name="Sester 100–11">{{cite journal | vauthors = Sester M, Sotgiu G, Lange C, Giehl C, Girardi E, Migliori GB, Bossink A, Dheda K, Diel R, Dominguez J, Lipman M, Nemeth J, Ravn P, Winkler S, Huitric E, Sandgren A, Manissero D | title = Interferon-γ release assays for the diagnosis of active tuberculosis: a systematic review and meta-analysis | journal = The European Respiratory Journal | volume = 37 | issue = 1 | pages = 100–11 | date = January 2011 | pmid = 20847080 | doi = 10.1183/09031936.00114810 | doi-access = free }}</ref> IGRA have similar limitations in those with HIV.<ref name="Sester 100–11"/><ref>{{cite journal | vauthors = Chen J, Zhang R, Wang J, Liu L, Zheng Y, Shen Y, Qi T, Lu H | title = Interferon-gamma release assays for the diagnosis of active tuberculosis in HIV-infected patients: a systematic review and meta-analysis | journal = PLOS ONE| volume = 6 | issue = 11 | pages = e26827 | year = 2011 | pmid = 22069472 | pmc = 3206065 | doi = 10.1371/journal.pone.0026827 | veditors = Vermund SH |editor1-link=Sten H. Vermund | bibcode = 2011PLoSO...626827C | doi-access = free }}</ref> |
|||
The first genuine success in immunizing against tuberculosis was developed from attenuated bovine-strain tuberculosis by [[Albert Calmette]] and [[Camille Guerin]] in 1906. It was called 'BCG' ([[Bacillus Calmette-Guérin|Bacillus of Calmette and Guerin]]). The BCG vaccine was first used on humans in [[1921]] in [[France]],<ref name=Bonah/> but it wasn't until after [[World War II]] that BCG received widespread acceptance in the [[United States|USA]], [[Great Britain]], and [[Germany]].<ref name=Comstock/> |
|||
A definitive diagnosis of TB is made by identifying ''M. tuberculosis'' in a clinical sample (e.g., sputum, [[pus]], or a [[Tissue (biology)|tissue]] [[biopsy]]). However, the difficult culture process for this slow-growing organism can take two to six weeks for blood or sputum culture.<ref>{{cite book | author = Special Programme for Research & Training in Tropical Diseases |title=Diagnostics for tuberculosis: global demand and market potential|year=2006|publisher=World Health Organization (WHO)|location=Geneva|isbn=978-92-4-156330-7|page=36|url=https://books.google.com/books?id=CFPpcCef4yQC&pg=PA36|url-status=live|archive-url=https://web.archive.org/web/20150906202315/https://books.google.com/books?id=CFPpcCef4yQC&pg=PA36|archive-date=6 September 2015}}</ref> Thus, treatment is often begun before cultures are confirmed.<ref name=NICE2011/> |
|||
Tuberculosis, or 'consumption' as it was commonly known, caused the most widespread public concern in the 19th and early 20th centuries as an [[endemic (epidemiology)|endemic]] disease of the urban poor. In 1815, one in four deaths in England was of consumption; by 1918 one in six deaths in France were still caused by TB. After the establishment in the 1880s that the disease was contagious, TB was made a [[List of notifiable diseases|notifiable disease]] in Britain; there were campaigns to stop spitting in public places, and the infected poor were "encouraged" to enter [[sanatorium|sanatoria]] that resembled prisons; the sanatoria for the middle and upper classes offered excellent care and constant medical attention.<ref name =sanatoria/> Whatever the purported benefits of the fresh air and labor in the sanatoria, even under the best conditions, 50% of those who entered were dead within five years (1916).<ref name =sanatoria/> |
|||
[[Image:TB poster.jpg|left|thumb|200px|Public health campaigns tried to halt the spread of TB]] |
|||
[[Nucleic acid amplification test]]s and [[adenosine deaminase]] testing may allow rapid diagnosis of TB.<ref name=DiagP2011/> Blood tests to detect antibodies are not [[sensitivity and specificity|specific or sensitive]], so they are not recommended.<ref>{{cite journal | vauthors = Steingart KR, Flores LL, Dendukuri N, Schiller I, Laal S, Ramsay A, Hopewell PC, Pai M | title = Commercial serological tests for the diagnosis of active pulmonary and extrapulmonary tuberculosis: an updated systematic review and meta-analysis | journal = PLOS Medicine | volume = 8 | issue = 8 | page= e1001062 | date = August 2011 | pmid = 21857806 | pmc = 3153457 | doi = 10.1371/journal.pmed.1001062 | doi-access = free | veditors = Evans C }}</ref> |
|||
The promotion of [[Christmas Seals]] began in Denmark during 1904 as a way to raise money for tuberculosis programs. It expanded to the United States and Canada in 1907–08 to help the National Tuberculosis Association (later called the [[American Lung Association]]). |
|||
=== Latent tuberculosis === |
|||
In the United States, concern about the spread of tuberculosis played a role in the movement to prohibit public spitting except into [[spittoon]]s. |
|||
{{Main|Latent tuberculosis}} |
|||
[[File:Mantoux tuberculin skin test.jpg|thumb|left|Mantoux tuberculin skin test]] |
|||
The [[Mantoux test|Mantoux tuberculin skin test]] is often used to screen people at high risk for TB.<ref name=Clinic2009/> Those who have been previously immunized with the Bacille Calmette-Guerin vaccine may have a false-positive test result.<ref name=Rothel_2005>{{cite journal | vauthors = Rothel JS, Andersen P | s2cid = 25423684 | title = Diagnosis of latent Mycobacterium tuberculosis infection: is the demise of the Mantoux test imminent? | journal = Expert Review of Anti-Infective Therapy | volume = 3 | issue = 6 | pages = 981–93 | date = December 2005 | pmid = 16307510 | doi = 10.1586/14787210.3.6.981 }}</ref> The test may be falsely negative in those with [[sarcoidosis]], [[Hodgkin's lymphoma]], [[malnutrition]], and most notably, active tuberculosis.<ref name=Robbins/> [[Interferon gamma release assay]]s, on a blood sample, are recommended in those who are positive to the Mantoux test.<ref name=NICE2011>{{NICE|117|Tuberculosis|2011}}</ref> These are not affected by immunization or most [[environmental mycobacteria]], so they generate fewer [[false-positive]] results.<ref>{{cite journal | vauthors = Pai M, Zwerling A, Menzies D | title = Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update | journal = Annals of Internal Medicine | volume = 149 | issue = 3 | pages = 177–84 | date = August 2008 | pmid = 18593687 | pmc = 2951987 | doi = 10.7326/0003-4819-149-3-200808050-00241 }}</ref> However, they are affected by ''M. szulgai'', ''M. marinum'', and ''M. kansasii''.<ref>{{cite book| veditors = Jindal SK |title=Textbook of Pulmonary and Critical Care Medicine|publisher=Jaypee Brothers Medical Publishers|location=New Delhi|isbn=978-93-5025-073-0|page=544|url=https://books.google.com/books?id=rAT1bdnDakAC&pg=PA544|year=2011|url-status=live|archive-url=https://web.archive.org/web/20150906185238/https://books.google.com/books?id=rAT1bdnDakAC&pg=PA544|archive-date=6 September 2015}}</ref> IGRAs may increase sensitivity when used in addition to the skin test, but may be less sensitive than the skin test when used alone.<ref>{{cite journal | vauthors = Amicosante M, Ciccozzi M, Markova R | title = Rational use of immunodiagnostic tools for tuberculosis infection: guidelines and cost effectiveness studies | journal = The New Microbiologica | volume = 33 | issue = 2 | pages = 93–107 | date = April 2010 | pmid = 20518271 }}</ref> |
|||
The [[US Preventive Services Task Force]] (USPSTF) has recommended screening people who are at high risk for latent tuberculosis with either tuberculin skin tests or [[interferon-gamma release assay]]s.<ref>{{cite journal | vauthors = Bibbins-Domingo K, Grossman DC, Curry SJ, Bauman L, Davidson KW, Epling JW, García FA, Herzstein J, Kemper AR, Krist AH, Kurth AE, Landefeld CS, Mangione CM, Phillips WR, Phipps MG, Pignone MP | title = Screening for Latent Tuberculosis Infection in Adults: US Preventive Services Task Force Recommendation Statement | journal = JAMA | volume = 316 | issue = 9 | pages = 962–9 | date = September 2016 | pmid = 27599331 | doi = 10.1001/jama.2016.11046 | doi-access = free }}</ref> While some have recommend testing health care workers, evidence of benefit for this is poor {{as of|2019|lc=yes}}.<ref>{{cite journal | vauthors = Gill J, Prasad V | title = Testing Healthcare Workers for Latent Tuberculosis: Is It Evidence Based, Bio-Plausible, Both, Or Neither? | journal = The American Journal of Medicine | volume = 132 | issue = 11 | pages = 1260–1261 | date = November 2019 | pmid = 30946831 | doi = 10.1016/j.amjmed.2019.03.017 | doi-access = free }}</ref> The [[Centers for Disease Control and Prevention]] (CDC) stopped recommending yearly testing of health care workers without known exposure in 2019.<ref>{{cite journal | vauthors = Sosa LE, Njie GJ, Lobato MN, Bamrah Morris S, Buchta W, Casey ML, Goswami ND, Gruden M, Hurst BJ, Khan AR, Kuhar DT, Lewinsohn DM, Mathew TA, Mazurek GH, Reves R, Paulos L, Thanassi W, Will L, Belknap R | title = Tuberculosis Screening, Testing, and Treatment of U.S. Health Care Personnel: Recommendations from the National Tuberculosis Controllers Association and CDC, 2019 | journal = MMWR. Morbidity and Mortality Weekly Report | volume = 68 | issue = 19 | pages = 439–443 | date = May 2019 | pmid = 31099768 | pmc = 6522077 | doi = 10.15585/mmwr.mm6819a3 }}</ref> |
|||
In Europe, deaths from TB fell from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. Improvements in public health were reducing tuberculosis even before the arrival of antibiotics, although the disease remained a significant threat to public health, such that when the [[Medical Research Council (UK)|Medical Research Council]] was formed in Britain in 1913 its initial focus was tuberculosis research.<ref>[[Medical Research Council (UK)|]]. [http://www.mrc.ac.uk/YourHealth/StoriesDiscovery/Tuberculosis/index.htm MRC's contribution to Tuberculosis research.] Accessed 02 July 2007.</ref> |
|||
== Prevention == |
|||
It was not until 1946 with the development of the antibiotic [[streptomycin]] that effective treatment and cure became possible. Prior to the introduction of this drug, the only treatment besides sanatoria were surgical interventions, including the [[pneumothorax]] technique—collapsing an infected lung to "rest" it and allow lesions to heal—a technique that was of little benefit and was largely discontinued by the 1950s.<ref name=Wolfart_1990>{{cite journal |author=Wolfart W |title=[Surgical treatment of tuberculosis and its modifications—collapse therapy and resection treatment and their present-day sequelae] |journal=Offentl Gesundheitswes |volume=52 |issue=8–9 |pages=506-11 |year=1990 | pmid = 2146567}}</ref> The emergence of multidrug-resistant TB has again introduced surgery as part of the treatment for these infections. Here, surgical removal of chest cavities will reduce the number of bacteria in the lungs, as well as increasing the exposure of the remaining bacteria to drugs in the bloodstream, and is therefore thought to increase the effectiveness of the chemotherapy.<ref name=Lalloo_2006>{{cite journal |author=Lalloo U, Naidoo R, Ambaram A |title=Recent advances in the medical and surgical treatment of multi-drug resistant tuberculosis |journal=Curr Opin Pulm Med |volume=12 |issue=3 |pages=179-85 |year=2006 | pmid = 16582672}}</ref> |
|||
[[File:Notice Do not spit - National Association for the Prevention of Tuberculosis Dublin Branch.jpg|thumb|Tuberculosis public health campaign in Ireland, c. 1905]] |
|||
Hope that the disease could be completely eliminated have been dashed since the rise of [[Antibiotic resistant|drug-resistant]] strains in the 1980s. For example, tuberculosis cases in Britain, numbering around 117,000 in 1913, had fallen to around 5,000 in 1987, but cases rose again, reaching 6,300 in 2000 and 7,600 cases in 2005.<ref>{{cite web | url =http://www.hpa.org.uk/infections/topics_AZ/tb/epidemiology/table1.htm | title = Tuberculosis – Respiratory and Non-respiratory Notifications, England and Wales, 1913-2005 | publisher = Health Protection Agency Centre for Infections | date = 21 March 2007 | accessdate = 2007-08-01}}</ref> Due to the elimination of public health facilities in New York and the emergence of HIV, there was a resurgence in the late 1980s.<ref name=Paolo_2004>{{cite journal |author=Paolo W, Nosanchuk J |title=Tuberculosis in New York city: recent lessons and a look ahead |journal=Lancet Infect Dis |volume=4 |issue=5 |pages=287-93 |year=2004 | pmid = 15120345}}</ref> The number of those failing to complete their course of drugs is high. NY had to cope with more than 20,000 "unnecessary" TB-patients with [[Multidrug resistance|multidrug-resistant]] strains (resistant to, at least, both Rifampin and Isoniazid). The resurgence of tuberculosis resulted in the declaration of a global health emergency by the World Health Organization in 1993.<ref>[[World Health Organization]] (WHO). [http://www.who.int/tb/hiv/faq/en/index.html Frequently asked questions about TB and HIV.] Retrieved 6 October 2006.</ref> |
|||
Tuberculosis prevention and control efforts rely primarily on the vaccination of infants and the detection and appropriate treatment of active cases.<ref name=Lancet11/> The [[World Health Organization]] (WHO) has achieved some success with improved treatment regimens, and a small decrease in case numbers.<ref name=Lancet11/> Some countries have legislation to involuntarily detain or examine those suspected to have tuberculosis, or [[Involuntary treatment|involuntarily treat]] them if infected.<ref>{{cite journal | vauthors = Coker R, Thomas M, Lock K, Martin R | title = Detention and the evolving threat of tuberculosis: evidence, ethics, and law | journal = The Journal of Law, Medicine & Ethics | volume = 35 | issue = 4 | pages = 609–15, 512 | date = 2007 | pmid = 18076512 | doi = 10.1111/j.1748-720X.2007.00184.x | s2cid = 19924571 }}</ref> |
|||
=== Vaccines === |
|||
==Infection of other animals== |
|||
{{Main|Tuberculosis vaccines|BCG vaccine}} |
|||
{{main|Mycobacterium bovis}} |
|||
The only available [[vaccine]] {{as of|2021|lc=yes}} is [[bacillus Calmette-Guérin]] (BCG).<ref name=McS2011>{{cite journal | vauthors = McShane H | title = Tuberculosis vaccines: beyond bacille Calmette-Guerin | journal = Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences | volume = 366 | issue = 1579 | pages = 2782–89 | date = October 2011 | pmid = 21893541 | pmc = 3146779 |doi-access=free | doi = 10.1098/rstb.2011.0097 }}</ref><ref>{{cite web |title=Vaccines {{!}} Basic TB Facts |url=https://www.cdc.gov/tb/topic/basics/vaccines.htm |date=16 June 2021 |publisher=CDC |access-date=30 December 2021 |archive-date=30 December 2021 |archive-url=https://web.archive.org/web/20211230115301/https://www.cdc.gov/tb/topic/basics/vaccines.htm |url-status=live }}</ref> In children it decreases the risk of getting the infection by 20% and the risk of infection turning into active disease by nearly 60%.<ref>{{cite journal | vauthors = Roy A, Eisenhut M, Harris RJ, Rodrigues LC, Sridhar S, Habermann S, Snell L, Mangtani P, Adetifa I, Lalvani A, Abubakar I | title = Effect of BCG vaccination against Mycobacterium tuberculosis infection in children: systematic review and meta-analysis |doi-access=free | journal = BMJ | volume = 349 | page= g4643 | date = August 2014 | pmid = 25097193 | pmc = 4122754 | doi = 10.1136/bmj.g4643 }}</ref> |
|||
Tuberculosis can be carried by [[mammal]]s; domesticated species, such as cats and dogs, are generally free of tuberculosis, but wild animals may be carriers. In some places, regulations aiming to prevent the spread of TB restrict the ownership of [[novelty pet]]s; for example, the [[United States of America|U.S.]] state of [[California]] forbids the ownership of pet [[gerbil]]s.<ref>14 CA ADC § 671 Barclays official California code of regulations; Title 14. Natural resources; Division 1. Fish and game commission – Department of fish and game; Subdivision 3. General regulations; Chapter 3. Miscellaneous.</ref> |
|||
It is the most widely used vaccine worldwide, with more than 90% of all children being vaccinated.<ref name=Lancet11/> The immunity it induces decreases after about ten years.<ref name=Lancet11/> As tuberculosis is uncommon in most of Canada, Western Europe, and the United States, BCG is administered to only those people at high risk.<ref>{{cite web|url=https://www.cdc.gov/tb/topic/vaccines/|title=Vaccine and Immunizations: TB Vaccine (BCG)|publisher=Centers for Disease Control and Prevention|year=2011|access-date=26 July 2011|url-status=dead|archive-url=https://web.archive.org/web/20111117140855/http://www.cdc.gov/tb/topic/vaccines/|archive-date=17 November 2011}}</ref><ref>{{cite web|title=BCG Vaccine Usage in Canada – Current and Historical|url=http://www.phac-aspc.gc.ca/tbpc-latb/bcgvac_1206-eng.php|work=Public Health Agency of Canada|access-date=30 December 2011|date=September 2010|url-status=dead|archive-url=https://web.archive.org/web/20120330042719/http://www.phac-aspc.gc.ca/tbpc-latb/bcgvac_1206-eng.php|archive-date=30 March 2012}}</ref><ref name=UK06>{{cite journal | vauthors = Teo SS, Shingadia DV | title = Does BCG have a role in tuberculosis control and prevention in the United Kingdom? | journal = Archives of Disease in Childhood | volume = 91 | issue = 6 | pages = 529–31 | date = June 2006 | pmid = 16714729 | pmc = 2082765 | doi = 10.1136/adc.2005.085043 }}</ref> Part of the reasoning against the use of the vaccine is that it makes the tuberculin skin test falsely positive, reducing the test's usefulness as a screening tool.<ref name=UK06/> Several vaccines are being developed.<ref name=Lancet11/> |
|||
[[Mycobacterium bovis]] causes TB in cattle. An effort to eradicate bovine tuberculosis from the cattle and deer herds of [[New Zealand]] is underway. It has been found that herd infection is more likely in areas where infected [[vector species]] such as Australian [[Possums|brush-tailed possums]] come into contact with [[Livestock|domestic livestock]] at farm/bush borders.<ref name=Tweddle_1994>{{cite journal |author=Tweddle N, Livingstone P |title=Bovine tuberculosis control and eradication programs in Australia and New Zealand |journal=Vet Microbiol |volume=40 |issue=1–2 |pages=23–39 |year=1994 | pmid = 8073626}}</ref> Controlling the vectors through possum eradication and monitoring the level of disease in livestock herds through regular surveillance are seen as a "two-pronged" approach to ridding New Zealand of the disease. |
|||
Intradermal MVA85A vaccine in addition to BCG injection is not effective in preventing tuberculosis.<ref>{{cite journal | vauthors = Kashangura R, Jullien S, Garner P, Johnson S | title = MVA85A vaccine to enhance BCG for preventing tuberculosis | journal = The Cochrane Database of Systematic Reviews | volume = 2019 | pages = CD012915 | date = April 2019 | issue = 4 | pmid = 31038197 | pmc = 6488980 | doi = 10.1002/14651858.CD012915.pub2 | collaboration = Cochrane Infectious Diseases Group }}</ref> |
|||
In the [[Republic of Ireland]] and the [[United Kingdom]], [[Eurasian Badger|badger]]s have been identified as one vector species for the transmission of bovine tuberculosis. As a result, governments have come under pressure from some quarters, primarily dairy farmers, to mount an active campaign of eradication of badgers in certain areas with the purpose of reducing the incidence of bovine TB. The UK government has not committed itself on the issue, not least because it fears public opinion: badgers are a protected species. The effectiveness of culling on the incidence of TB in cattle is a contentious issue, with proponents and opponents citing their own studies to support their position.<ref>The Department of Agriculture & Food (Ireland). [http://www.agriculture.ie/index.jsp?file=animal_health/TB.xml Disease Eradication Schemes - Bovine Tuberculosis and Brucellosis.] Retrieved on 8 May 2006.</ref><ref>Cassidy, Martin. [http://news.bbc.co.uk/1/hi/northern_ireland/4044897.stm Badgers targeted over bovine TB.] ''[[BBC News]]'' 2 December, 2004. Retrieved on 8 May 2006.</ref><ref>National Federation of Badger Groups (Ireland). [http://www.badger-killers.co.uk/Ireland/Ireland_news.html Cattle blamed for massive increase in bovine TB.] Retrieved on 8 May 2006.</ref> |
|||
== |
=== Public health === |
||
*[[2007 tuberculosis scare]] |
|||
*[[Abreugraphy]] |
|||
*[[ATC code J04]] Drugs for treatment of TB |
|||
*[[Buruli ulcer]] and [[leprosy]]: other diseases caused by mycobacteria |
|||
*[[Latent tuberculosis]] |
|||
*[[List of tuberculosis victims]] |
|||
*[[Mycobacterium Tuberculosis Structural Genomics Consortium]] |
|||
*[[National Center for HIV, STD, and TB Prevention]] |
|||
*[[Nontuberculous mycobacteria]] |
|||
*[[Overcrowding]] |
|||
*[[Philip D'Arcy Hart]] |
|||
*[[Tuberculosis in history and art]] |
|||
*[[UNITAID]] |
|||
* [[Nosocomial infection]] |
|||
Public health campaigns which have focused on overcrowding, public spitting and regular sanitation (including hand washing) during the 1800s helped to either interrupt or slow spread which when combined with contact tracing, isolation and treatment helped to dramatically curb the transmission of both tuberculosis and other airborne diseases which led to the [[Tuberculosis elimination|elimination of tuberculosis]] as a major public health issue in most developed economies.<ref>{{cite journal | vauthors = Clark M, Riben P, Nowgesic E | title = The association of housing density, isolation and tuberculosis in Canadian First Nations communities | journal = International Journal of Epidemiology | volume = 31 | issue = 5 | pages = 940–945 | date = October 2002 | pmid = 12435764 | doi = 10.1093/ije/31.5.940 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Barberis I, Bragazzi NL, Galluzzo L, Martini M | title = The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus | journal = Journal of Preventive Medicine and Hygiene | volume = 58 | issue = 1 | pages = E9–E12 | date = March 2017 | pmid = 28515626 | pmc = 5432783 }}</ref> Other risk factors which worsened TB spread such as malnutrition were also ameliorated, but since the emergence of [[HIV]] a new population of immunocompromised individuals was available for TB to infect. |
|||
==References== |
|||
<!-- --------------------------------------------------------------- |
|||
See http://en.wikipedia.org/wiki/Wikipedia:Footnotes for a |
|||
discussion of different citation methods and how to generate |
|||
footnotes using the <ref> & </ref> tags and the {{Reflist}} template |
|||
-------------------------------------------------------------------- --> |
|||
{{reflist|2}} |
|||
The World Health Organization (WHO) declared TB a "global health emergency" in 1993,<ref name="Lancet11" /> and in 2006, the Stop TB Partnership developed a [[Global Plan to Stop Tuberculosis]] that aimed to save 14 million lives between its launch and 2015.<ref>{{cite web|url=http://www.stoptb.org/global/plan/|title=The Global Plan to Stop TB|publisher=[[World Health Organization]] (WHO)|year=2011|access-date=13 June 2011|url-status=live|archive-url=https://web.archive.org/web/20110612030924/http://www.stoptb.org/global/plan/|archive-date=12 June 2011}}</ref> A number of targets they set were not achieved by 2015, mostly due to the increase in HIV-associated tuberculosis and the emergence of multiple drug-resistant tuberculosis.<ref name="Lancet11" /> A [[tuberculosis classification]] system developed by the [[American Thoracic Society]] is used primarily in public health programs.<ref>{{cite book| vauthors = Warrell DA, Cox TM, Firth JD, Benz EJ |title=Sections 1–10|year=2005|publisher=Oxford Univ. Press|location=Oxford [u.a.]|isbn=978-0-19-857014-1|page=560|url=https://books.google.com/books?id=EhjX517cGVsC&pg=PA560|edition=4. ed., paperback|url-status=live|archive-url=https://web.archive.org/web/20150906210011/https://books.google.com/books?id=EhjX517cGVsC&pg=PA560|archive-date=6 September 2015}}</ref> In 2015, it launched the [[End TB Strategy]] to reduce deaths by 95% and incidence by 90% before 2035. The goal of tuberculosis elimination is being hampered by the lack of rapid testing, short and effective treatment courses, and [[tuberculosis vaccine|completely effective vaccines]].<ref>{{cite journal | vauthors = Uplekar M, Weil D, Lonnroth K, Jaramillo E, Lienhardt C, Dias HM, Falzon D, Floyd K, Gargioni G, Getahun H, Gilpin C, Glaziou P, Grzemska M, Mirzayev F, Nakatani H, Raviglione M | title = WHO's new end TB strategy | journal = Lancet | volume = 385 | issue = 9979 | pages = 1799–1801 | date = May 2015 | pmid = 25814376 | doi = 10.1016/S0140-6736(15)60570-0 | s2cid = 39379915 }}</ref> |
|||
==Further reading== |
|||
<div class="references-small" style="-moz-column-count:2; column-count:2;"> |
|||
* {{cite journal | author = Blumberg HM, Leonard MK, Jasmer RM | title = Update on the treatment of tuberculosis and latent tuberculosis infection | journal = JAMA | volume = 293 | issue = 22 | pages = 2776-84 | year = 2005 | pmid = 15941808 | doi = 10.1001/jama.293.22.2776}} |
|||
* {{cite book | last = Dormandy | first = Thomas | title = The White Death | publisher = New York University Press | location = New York | year = 2000 | isbn = 0814719279 }} |
|||
* {{cite journal | author = Joint Tuberculosis Committee of the British Thoracic Society | title = Control and prevention of tuberculosis in the United Kingdom: code of practice 2000. | journal = Thorax | volume = 55 | issue = 11 | pages = 887-901 | year = 2000 | pmid = 11050256 | url = http://thorax.bmjjournals.com/cgi/content/abstract/55/11/887}} |
|||
* {{cite book | last = Kidder | first = Tracy | title = Mountains beyond Mountains | publisher = Random House Trade Paperbacks | location = New York | year = 2004 | isbn = 0812973011 }} A nonfiction account of treating TB in Haiti, Peru, and elsewhere. |
|||
* {{cite book | last = Lawlor | first = Clark | title = Consumption and Literature | publisher = Palgrave Macmillan | location = Basingstoke | year = 2007 | isbn = 0230020038 }} |
|||
* {{cite journal | author = Nemery B, Yew WW, Albert R, ''et al'' | title = Tuberculosis, nontuberculous lung infection, pleural disorders, pulmonary function, respiratory muscles, occupational lung disease, pulmonary infections, and social issues in AJRCCM in 2004 | journal = Am. J. Respir. Crit. Care Med. | volume = 171 | issue = 6 | pages = 554-62 | year = 2005 | pmid = 15753485 | doi = 10.1164/rccm.2412009}} |
|||
*{{cite journal | author = Walton D, Farmer P | title = MSJAMA: the new white plague | journal = JAMA | volume = 284 | issue = 21 | pages = 2789 | year = 2000 | pmid = 11105192 | url = http://jama.ama-assn.org/cgi/content/full/284/21/2789}} |
|||
</div> |
|||
The benefits and risks of giving anti-tubercular drugs to those exposed to MDR-TB is unclear.<ref>{{cite journal | vauthors = Fraser A, Paul M, Attamna A, Leibovici L | title = Drugs for preventing tuberculosis in people at risk of multiple-drug-resistant pulmonary tuberculosis | journal = The Cochrane Database of Systematic Reviews | issue = 2 | pages = CD005435 | date = April 2006 | volume = 2006 | pmid = 16625639 | pmc = 6532726 | doi = 10.1002/14651858.CD005435.pub2 | collaboration = Cochrane Infectious Diseases Group }}</ref> Making HAART therapy available to HIV-positive individuals significantly reduces the risk of progression to an active TB infection by up to 90% and can mitigate the spread through this population.<ref>{{cite journal | vauthors = Piggott DA, Karakousis PC | title = Timing of antiretroviral therapy for HIV in the setting of TB treatment | journal = Clinical & Developmental Immunology | volume = 2011 | pages = 103917 | date = 27 December 2010 | pmid = 21234380 | pmc = 3017895 | doi = 10.1155/2011/103917 | doi-access = free }}</ref> |
|||
==External links== |
|||
{{commonscat|Tuberculosis}} |
|||
* {{dmoz|Health/Conditions_and_Diseases/Infectious_Diseases/Mycobacterial/Tuberculosis/}} |
|||
*[[Centers for Disease Control and Prevention]] (CDC), Division of Tuberculosis Elimination. [http://www.cdc.gov/tb/pubs/corecurr/default.htm Core Curriculum on Tuberculosis: What the Clinician Should Know.] 4th edition (2000). Updated Aug 2003. |
|||
*(CDC) - Division of Tuberculosis Elimination [http://www.cdc.gov/nchstp/tb/default.htm News and updates.] |
|||
*(CDC) - [http://www.cdc.gov/nchstp/tb/faqs/qa.htm Questions and Answers About TB, 2005.] |
|||
*BioHealthBase Bioinformatics Resource Center. [http://www.biohealthbase.org/ Database of ''Mycobacterium tuberculosis''] genome sequences and related information. |
|||
*Kaiser Family Foundation. [http://www.globalhealthfacts.org/topic.jsp?i=9 Tuberculosis.] Globalhealthfacts.org. |
|||
*[[Nobel Prize|The Nobel Prize Website.]] [http://nobelprize.org/educational_games/medicine/tuberculosis/tbc/index.html Tuberculosis Educational Game] |
|||
*[[United States Agency for International Development]] (USAID). [http://www.tbcta.org/Pages/home.php/ The Tuberculosis Coalition for Technical Assistance (TBCTA).] |
|||
*[[World Health Organization]] (WHO). [http://www.who.int/tb/en/ Tuberculosis.] |
|||
== Treatment == |
|||
{{featured article}} |
|||
{{Main|Tuberculosis management}} |
|||
{{Bacterial diseases }} |
|||
[[File:Tubi - 1234,0186.jpg|thumb|Tuberculosis phototherapy treatment on 3 March 1934, in [[Kuopio]], [[Finland]]]] |
|||
<!-- interwikik --> |
|||
Treatment of TB uses antibiotics to kill the bacteria. Effective TB treatment is difficult, due to the unusual structure and chemical composition of the mycobacterial [[Cord factor|cell wall]], which hinders the entry of drugs and makes many antibiotics ineffective.<ref>{{cite journal | vauthors = Brennan PJ, Nikaido H | title = The envelope of mycobacteria | journal = Annual Review of Biochemistry | volume = 64 | pages = 29–63 | year = 1995 | pmid = 7574484 | doi = 10.1146/annurev.bi.64.070195.000333 }}</ref> |
|||
<!-- en-US --> |
|||
Active TB is best treated with combinations of several antibiotics to reduce the risk of the bacteria developing [[antibiotic resistance]].<ref name=Lancet11/> The routine use of [[rifabutin]] instead of [[rifampicin]] in HIV-positive people with tuberculosis is of unclear benefit {{as of|2007|lc=yes}}.<ref>{{cite journal | vauthors = Davies G, Cerri S, Richeldi L | title = Rifabutin for treating pulmonary tuberculosis | journal = The Cochrane Database of Systematic Reviews | issue = 4 | pages = CD005159 | date = October 2007 | volume = 2007 | pmid = 17943842 | pmc = 6532710 | doi = 10.1002/14651858.CD005159.pub2 }}</ref> |
|||
[[Category:Deaths by tuberculosis| ]] |
|||
[[Category:Bacterial diseases]] |
|||
[[Category:Pulmonology]] |
|||
[[Category:Tuberculosis|Tuberculosis]] |
|||
[[Category:Health problems in India]] |
|||
Acetylsalicylic acid (aspirin) at a dose of 100 mg per day has been shown to improve clinical signs and symptoms, reduce cavitary lesions, lower inflammatory markers, and increase the rate of sputum-negative conversion in patients with pulmonary tuberculosis.<ref>{{cite journal | vauthors = Di Bella S, Luzzati R, Principe L, Zerbato V, Meroni E, Giuffrè M, Crocè LS, Merlo M, Perotto M, Dolso E, Maurel C, Lovecchio A, Dal Bo E, Lagatolla C, Marini B, Ippodrino R, Sanson G | title = Aspirin and Infection: A Narrative Review | journal = Biomedicines | volume = 10 | issue = 2 | pages = 263 | date = January 2022 | pmid = 35203473 | pmc = 8868581 | doi = 10.3390/biomedicines10020263 | doi-access = free }}</ref> |
|||
=== Latent TB === |
|||
{{Link FA|de}} |
|||
{{Link FA|pt}} |
|||
Latent TB is treated with either [[isoniazid]] or [[rifampin]] alone, or a combination of isoniazid with either rifampicin or rifapentine.<ref name="WHOlatent2018">{{cite book | publisher=[[World Health Organization]] (WHO) | title=Latent tuberculosis infection | year=2018 | page=23 | isbn=978-92-4-155023-9 | url=http://apps.who.int/iris/bitstream/handle/10665/260233/9789241550239-eng.pdf;jsessionid=E08401544A59BE3F84C645C9A9A7B0E5?sequence=1 | access-date=25 July 2018 | archive-date=2 June 2021 | archive-url=https://web.archive.org/web/20210602215123/http://apps.who.int/iris/bitstream/handle/10665/260233/9789241550239-eng.pdf;jsessionid=E08401544A59BE3F84C645C9A9A7B0E5?sequence=1 | url-status=live }}</ref><ref>{{cite journal | vauthors = Borisov AS, Bamrah Morris S, Njie GJ, Winston CA, Burton D, Goldberg S, Yelk Woodruff R, Allen L, LoBue P, Vernon A | title = Update of Recommendations for Use of Once-Weekly Isoniazid-Rifapentine Regimen to Treat Latent Mycobacterium tuberculosis Infection | journal = MMWR. Morbidity and Mortality Weekly Report | volume = 67 | issue = 25 | pages = 723–726 | date = June 2018 | pmid = 29953429 | pmc = 6023184 | doi = 10.15585/mmwr.mm6725a5 }}</ref><ref name=Ste2020>{{cite journal | vauthors = Sterling TR, Njie G, Zenner D, Cohn DL, Reves R, Ahmed A, Menzies D, Horsburgh CR, Crane CM, Burgos M, LoBue P, Winston CA, Belknap R | title = Guidelines for the Treatment of Latent Tuberculosis Infection: Recommendations from the National Tuberculosis Controllers Association and CDC, 2020 | language = en-us | journal = MMWR. Recommendations and Reports | volume = 69 | issue = 1 | pages = 1–11 | date = February 2020 | pmid = 32053584 | pmc = 7041302 | doi = 10.15585/mmwr.rr6901a1 }}</ref> |
|||
[[af:Tuberkulose]] |
|||
[[ar:سل]] |
|||
The treatment takes three to nine months depending on the medications used.<ref name=CDCcourse/><ref name="WHOlatent2018"/><ref>{{cite journal | vauthors = Njie GJ, Morris SB, Woodruff RY, Moro RN, Vernon AA, Borisov AS | title = Isoniazid-Rifapentine for Latent Tuberculosis Infection: A Systematic Review and Meta-analysis | journal = American Journal of Preventive Medicine | volume = 55 | issue = 2 | pages = 244–252 | date = August 2018 | pmid = 29910114 | pmc = 6097523 | doi = 10.1016/j.amepre.2018.04.030 }}</ref><ref name=Ste2020/> People with latent infections are treated to prevent them from progressing to active TB disease later in life.<ref name=Latent2011>{{cite journal | vauthors = Menzies D, Al Jahdali H, Al Otaibi B | title = Recent developments in treatment of latent tuberculosis infection | journal = The Indian Journal of Medical Research | volume = 133 | issue = 3 | pages = 257–66 | date = March 2011 | pmid = 21441678 | pmc = 3103149 }}</ref> |
|||
[[ast:Tuberculosis]] |
|||
[[az:Vərəm]] |
|||
Education or counselling may improve the latent tuberculosis treatment completion rates.<ref>{{cite journal | vauthors = M'imunya JM, Kredo T, Volmink J | title = Patient education and counselling for promoting adherence to treatment for tuberculosis | journal = The Cochrane Database of Systematic Reviews | issue = 5 | pages = CD006591 | date = May 2012 | volume = 2012 | pmid = 22592714 | pmc = 6532681 | doi = 10.1002/14651858.CD006591.pub2 | collaboration = Cochrane Infectious Diseases Group }}</ref> |
|||
[[bn:যক্ষ্মা]] |
|||
[[zh-min-nan:Hì-lô-pēⁿ]] |
|||
=== New onset === |
|||
[[bs:Tuberkuloza]] |
|||
[[bg:Туберкулоза]] |
|||
The recommended treatment of new-onset pulmonary tuberculosis, {{as of|2010|lc=yes}}, is six months of a combination of antibiotics containing rifampicin, isoniazid, [[pyrazinamide]], and [[ethambutol]] for the first two months, and only rifampicin and isoniazid for the last four months.<ref name=Lancet11/> Where resistance to isoniazid is high, ethambutol may be added for the last four months as an alternative.<ref name="Lancet11" /> Treatment with anti-TB drugs for at least 6 months results in higher success rates when compared with treatment less than 6 months, even though the difference is small. Shorter treatment regimen may be recommended for those with compliance issues.<ref name="Gelband_1999">{{cite journal | vauthors = Gelband H | title = Regimens of less than six months for treating tuberculosis | journal = The Cochrane Database of Systematic Reviews | issue = 2 | pages = CD001362 | date = 25 October 1999 | volume = 1999 | pmid = 10796641 | pmc = 6532732 | doi = 10.1002/14651858.CD001362 | collaboration = Cochrane Infectious Diseases Group }}</ref> There is also no evidence to support shorter anti-tuberculosis treatment regimens when compared to a 6-month treatment regimen.<ref>{{cite journal | vauthors = Grace AG, Mittal A, Jain S, Tripathy JP, Satyanarayana S, Tharyan P, Kirubakaran R | title = Shortened treatment regimens versus the standard regimen for drug-sensitive pulmonary tuberculosis | journal = The Cochrane Database of Systematic Reviews | volume = 12 | pages = CD012918 | date = December 2019 | issue = 12 | pmid = 31828771 | pmc = 6953336 | doi = 10.1002/14651858.CD012918.pub2 | collaboration = Cochrane Infectious Diseases Group }}</ref> However, results presented in 2020 from an international, randomized, controlled clinical trial indicate that a four-month daily treatment regimen containing high-dose, or "optimized", rifapentine with moxifloxacin (2PHZM/2PHM) is as safe and effective as the existing standard six-month daily regimen at curing drug-susceptible tuberculosis (TB) disease.<ref>{{cite web |title=Landmark TB Trial Identifies Shorter-Course Treatment Regimen |url=https://www.cdc.gov/nchhstp/newsroom/2020/landmark-tb-trial-media-statement.html |website=CDC |date=20 October 2020 |publisher=NCHHSTP Media Team Centers for Disease Control and Prevention |access-date=27 November 2021 |archive-date=27 November 2021 |archive-url=https://web.archive.org/web/20211127171700/https://www.cdc.gov/nchhstp/newsroom/2020/landmark-tb-trial-media-statement.html |url-status=live }}</ref> |
|||
[[ca:Tuberculosi]] |
|||
[[cs:Tuberkulóza]] |
|||
=== Recurrent disease === |
|||
[[da:Tuberkulose]] |
|||
[[de:Tuberkulose]] |
|||
If tuberculosis recurs, testing to determine which antibiotics it is sensitive to is important before determining treatment.<ref name="Lancet11" /> If [[Multidrug-resistant TB|multiple drug-resistant TB]] (MDR-TB) is detected, treatment with at least four effective antibiotics for 18 to 24 months is recommended.<ref name="Lancet11" /> |
|||
[[es:Tuberculosis]] |
|||
[[eo:Tuberkulozo]] |
|||
=== Medication administration === |
|||
[[eu:Tuberkulosi]] |
|||
[[fa:سل]] |
|||
[[Directly observed therapy]], i.e., having a health care provider watch the person take their medications, is recommended by the World Health Organization (WHO) in an effort to reduce the number of people not appropriately taking antibiotics.<ref>{{cite book |vauthors = Mainous III AB |title=Management of Antimicrobials in Infectious Diseases: Impact of Antibiotic Resistance |publisher=Humana Press |location=Totowa, NJ |year=2010 |page=69 |isbn=978-1-60327-238-4 |url=https://books.google.com/books?id=hwVFAPLYznsC&pg=PA69 |url-status=live |archive-url=https://web.archive.org/web/20150906215558/https://books.google.com/books?id=hwVFAPLYznsC&pg=PA69 |archive-date=6 September 2015 }}</ref> The evidence to support this practice over people simply taking their medications independently is of poor quality.<ref name=Karumbi2015 /> There is no strong evidence indicating that directly observed therapy improves the number of people who were cured or the number of people who complete their medicine.<ref name=Karumbi2015>{{cite journal | vauthors = Karumbi J, Garner P | title = Directly observed therapy for treating tuberculosis | journal = The Cochrane Database of Systematic Reviews | issue = 5 | page= CD003343 | date = May 2015 | volume = 2015 | pmid = 26022367 | pmc = 4460720 | doi = 10.1002/14651858.CD003343.pub4 }}</ref> Moderate quality evidence suggests that there is also no difference if people are observed at home versus at a clinic, or by a family member versus a health care worker.<ref name=Karumbi2015 /> Methods to remind people of the importance of treatment and appointments may result in a small but important improvement.<ref>{{cite journal | vauthors = Liu Q, Abba K, Alejandria MM, Sinclair D, Balanag VM, Lansang MA | title = Reminder systems to improve patient adherence to tuberculosis clinic appointments for diagnosis and treatment | journal = The Cochrane Database of Systematic Reviews | issue = 11 | pages = CD006594 | date = November 2014 | volume = 2014 | pmid = 25403701 | pmc = 4448217 | doi = 10.1002/14651858.CD006594.pub3 | collaboration = Cochrane Infectious Diseases Group }}</ref> There is also not enough evidence to support intermittent rifampicin-containing therapy given two to three times a week has equal effectiveness as daily dose regimen on improving cure rates and reducing relapsing rates.<ref>{{cite journal | vauthors = Mwandumba HC, Squire SB | title = Fully intermittent dosing with drugs for treating tuberculosis in adults | journal = The Cochrane Database of Systematic Reviews | issue = 4 | pages = CD000970 | date = 23 October 2001 | pmid = 11687088 | pmc = 6532565 | doi = 10.1002/14651858.CD000970 | collaboration = Cochrane Infectious Diseases Group }}</ref> There is also not enough evidence on effectiveness of giving intermittent twice or thrice weekly short course regimen compared to daily dosing regimen in treating children with tuberculosis.<ref>{{cite journal | vauthors = Bose A, Kalita S, Rose W, Tharyan P | title = Intermittent versus daily therapy for treating tuberculosis in children | journal = The Cochrane Database of Systematic Reviews | issue = 1 | pages = CD007953 | date = January 2014 | volume = 2014 | pmid = 24470141 | pmc = 6532685 | doi = 10.1002/14651858.CD007953.pub2 | collaboration = Cochrane Infectious Diseases Group }}</ref> |
|||
[[fr:Tuberculose]] |
|||
[[ga:Eitinn]] |
|||
=== Medication resistance === |
|||
[[gd:A' Chaitheamh]] |
|||
[[gl:Tuberculose]] |
|||
Primary resistance occurs when a person becomes infected with a resistant strain of TB. A person with fully susceptible [[Mycobacterium tuberculosis|MTB]] may develop secondary (acquired) resistance during therapy because of inadequate treatment, not taking the prescribed regimen appropriately (lack of compliance), or using low-quality medication.<ref name=OBrien>{{cite journal | vauthors = O'Brien RJ | title = Drug-resistant tuberculosis: etiology, management and prevention | journal = Seminars in Respiratory Infections | volume = 9 | issue = 2 | pages = 104–12 | date = June 1994 | pmid = 7973169 }}</ref> Drug-resistant TB is a serious public health issue in many developing countries, as its treatment is longer and requires more expensive drugs. MDR-TB is defined as resistance to the two most effective first-line TB drugs: rifampicin and isoniazid. Extensively drug-resistant TB is also resistant to three or more of the six classes of second-line drugs.<ref name="MMWR2006">{{cite journal | author = Centers for Disease Control and Prevention (CDC) | title = Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs--worldwide, 2000-2004 | journal = MMWR. Morbidity and Mortality Weekly Report | volume = 55 | issue = 11 | pages = 301–5 | date = March 2006 | pmid = 16557213 | url = https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5511a2.htm | url-status = live | archive-url = https://web.archive.org/web/20170522030229/https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5511a2.htm | archive-date = 22 May 2017 }}</ref> Totally drug-resistant TB is resistant to all currently used drugs.<ref name="TR2012">{{Cite magazine|title=Totally Resistant TB: Earliest Cases in Italy|magazine=Wired|url=https://www.wired.com/wiredscience/2012/01/tdr-first-Italy/| vauthors = McKenna M |date=12 January 2012|access-date=12 January 2012|url-status=live|archive-url=https://web.archive.org/web/20120114214156/http://www.wired.com/wiredscience/2012/01/tdr-first-Italy/|archive-date=14 January 2012}}</ref> It was first observed in 2003 in Italy,<ref>{{cite journal | vauthors = Migliori GB, De Iaco G, Besozzi G, Centis R, Cirillo DM | title = First tuberculosis cases in Italy resistant to all tested drugs | journal = Euro Surveillance | volume = 12 | issue = 5 | pages = E070517.1 | date = May 2007 | pmid = 17868596 | doi = 10.2807/esw.12.20.03194-en | doi-access = free }}</ref> but not widely reported until 2012,<ref name="TR2012" /><ref>{{cite web|title=Totally Drug-Resistant TB: a WHO consultation on the diagnostic definition and treatment options|url=https://www.who.int/tb/challenges/xdr/Report_Meeting_totallydrugresistantTB_032012.pdf?ua=1|publisher=World Health Organization (WHO)|access-date=25 March 2016|url-status=live|archive-url=https://web.archive.org/web/20161021151601/http://www.who.int/tb/challenges/xdr/Report_Meeting_totallydrugresistantTB_032012.pdf?ua=1|archive-date=21 October 2016}}</ref> and has also been found in Iran and India.<ref name="EIU 2014">{{cite news | title = Ancient enemy, modern imperative – A time for greater action against tuberculosis | newspaper = The Economist |url=http://www.economistinsights.com/sites/default/files/Ancient%20enemy%20modern%20imperative.pdf |publisher=[[Economist Intelligence Unit]]|access-date=22 January 2022|date=30 June 2014| vauthors = Kielstra P | veditors = Tabary Z |url-status=dead|archive-url=https://web.archive.org/web/20140810101716/http://www.economistinsights.com/sites/default/files/Ancient%20enemy%20modern%20imperative.pdf |archive-date=10 August 2014}}</ref> There is some efficacy for [[linezolid]] to treat those with XDR-TB but side effects and discontinuation of medications were common.<ref>{{cite journal | vauthors = Singh B, Cocker D, Ryan H, Sloan DJ | title = Linezolid for drug-resistant pulmonary tuberculosis | journal = The Cochrane Database of Systematic Reviews | volume = 3 | pages = CD012836 | date = March 2019 | issue = 3 | pmid = 30893466 | pmc = 6426281 | doi = 10.1002/14651858.CD012836.pub2 | collaboration = Cochrane Infectious Diseases Group }}</ref><ref>{{cite journal | vauthors = Velayati AA, Masjedi MR, Farnia P, Tabarsi P, Ghanavi J, ZiaZarifi AH, Hoffner SE | title = Emergence of new forms of totally drug-resistant tuberculosis bacilli: super extensively drug-resistant tuberculosis or totally drug-resistant strains in Iran | journal = Chest | volume = 136 | issue = 2 | pages = 420–425 | date = August 2009 | pmid = 19349380 | doi = 10.1378/chest.08-2427 }}</ref> [[Bedaquiline]] is tentatively supported for use in multiple drug-resistant TB.<ref>{{cite web|title=Provisional CDC Guidelines for the Use and Safety Monitoring of Bedaquiline Fumarate (Sirturo) for the Treatment of Multidrug-Resistant Tuberculosis|url=https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6209a1.htm?s_cid=rr6209a1_x|url-status=live|archive-url=https://web.archive.org/web/20140104204359/http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6209a1.htm?s_cid=rr6209a1_x|archive-date=4 January 2014}}</ref> |
|||
[[ko:결핵]] |
|||
[[hi:तपेदिक]] |
|||
XDR-TB is a term sometimes used to define ''extensively resistant'' TB, and constitutes one in ten cases of MDR-TB. Cases of XDR TB have been identified in more than 90% of countries.<ref name="EIU 2014"/> |
|||
[[hr:Tuberkuloza]] |
|||
[[io:Tuberkulozo]] |
|||
For those with known rifampicin or MDR-TB, molecular tests such as the Genotype MTBDRsl Assay (performed on culture isolates or smear positive specimens) may be useful to detect second-line anti-tubercular drug resistance.<ref>{{cite journal | vauthors = Theron G, Peter J, Richardson M, Warren R, Dheda K, Steingart KR | title = ® MTBDRsl assay for resistance to second-line anti-tuberculosis drugs | journal = The Cochrane Database of Systematic Reviews | volume = 2016 | pages = CD010705 | date = September 2016 | issue = 9 | pmid = 27605387 | pmc = 5034505 | doi = 10.1002/14651858.CD010705.pub3 | collaboration = Cochrane Infectious Diseases Group }}</ref><ref>{{cite web |url=https://www.who.int/tb/WHOPolicyStatementSLLPA.pdf |title=The use of molecular line probe assays for the detection of resistance to second-line anti-tuberculosis drugs |website=World Health Organization |access-date=18 June 2021 |archive-date=22 September 2021 |archive-url=https://web.archive.org/web/20210922003541/https://www.who.int/tb/WHOPolicyStatementSLLPA.pdf |url-status=live }}</ref> |
|||
[[id:Tuberkulosa]] |
|||
[[ia:Tuberculosis]] |
|||
== Prognosis == |
|||
[[it:Tubercolosi]] |
|||
[[he:שחפת]] |
|||
[[File:Tuberculosis world map - DALY - WHO2004.svg|thumb|upright=1.4|[[Age adjustment|Age-standardized]] [[disability-adjusted life year]]s caused by tuberculosis per 100,000 inhabitants in 2004.<ref>{{cite web |url=https://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html |title=WHO Disease and injury country estimates |year=2004 |publisher=World Health Organization (WHO) |access-date=11 November 2009 |url-status=live |archive-url=https://web.archive.org/web/20091111101009/http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html |archive-date=11 November 2009 }}</ref> |
|||
[[ka:ტუბერკულიოზი]] |
|||
{{Col-begin}} |
|||
[[ku:Tûberkûloz]] |
|||
{{Col-break}} |
|||
[[la:Phthisis]] |
|||
{{legend|#b3b3b3|no data|size=60%}} |
|||
[[lt:Tuberkuliozė]] |
|||
{{legend|#ffff65|≤10|size=60%}} |
|||
[[ln:Tuberculose]] |
|||
{{legend|#fff200|10–25|size=60%}} |
|||
[[hu:Tuberkulózis]] |
|||
{{legend|#ffdc00|25–50|size=60%}} |
|||
[[mt:Tuberkulożi]] |
|||
{{legend|#ffc600|50–75|size=60%}} |
|||
[[ms:Penyakit Batuk Kering]] |
|||
{{legend|#ffb000|75–100|size=60%}} |
|||
[[nl:Tuberculose]] |
|||
{{legend|#ff9a00|100–250|size=60%}} |
|||
[[ja:結核]] |
|||
{{Col-break}} |
|||
[[no:Tuberkulose]] |
|||
{{legend|#ff8400|250–500|size=60%}} |
|||
[[nn:Tuberkulose]] |
|||
{{legend|#ff6e00|500–750|size=60%}} |
|||
[[pl:Gruźlica]] |
|||
{{legend|#ff5800|750–1000|size=60%}} |
|||
[[pt:Tuberculose]] |
|||
{{legend|#ff4200|1000–2000|size=60%}} |
|||
[[qu:Qhaqya unquy]] |
|||
{{legend|#ff2c00|2000–3000|size=60%}} |
|||
[[ru:Туберкулёз]] |
|||
{{legend|#cb0000|≥ 3000|size=60%}} |
|||
[[simple:Tuberculosis]] |
|||
{{col-end}}]] |
|||
[[sl:Tuberkuloza]] |
|||
Progression from TB infection to overt TB disease occurs when the bacilli overcome the immune system defenses and begin to multiply. In primary TB disease (some 1–5% of cases), this occurs soon after the initial infection.<ref name=Robbins/> However, in the majority of cases, a [[Latent tuberculosis|latent infection]] occurs with no obvious symptoms.<ref name=Robbins/> These dormant bacilli produce active tuberculosis in 5–10% of these latent cases, often many years after infection.<ref name=Pet2005/> |
|||
[[sr:Туберкулоза]] |
|||
[[sh:Tuberkuloza]] |
|||
The risk of reactivation increases with [[immunosuppression]], such as that caused by infection with HIV. In people coinfected with ''M. tuberculosis'' and HIV, the risk of reactivation increases to 10% per year.<ref name=Robbins/> Studies using [[DNA fingerprinting]] of ''M. tuberculosis'' strains have shown reinfection contributes more substantially to recurrent TB than previously thought,<ref>{{cite journal | vauthors = Lambert ML, Hasker E, Van Deun A, Roberfroid D, Boelaert M, Van der Stuyft P | title = Recurrence in tuberculosis: relapse or reinfection? | journal = The Lancet. Infectious Diseases | volume = 3 | issue = 5 | pages = 282–7 | date = May 2003 | pmid = 12726976 | doi = 10.1016/S1473-3099(03)00607-8 }}</ref> with estimates that it might account for more than 50% of reactivated cases in areas where TB is common.<ref>{{cite journal | vauthors = Wang JY, Lee LN, Lai HC, Hsu HL, Liaw YS, Hsueh PR, Yang PC | title = Prediction of the tuberculosis reinfection proportion from the local incidence | journal = The Journal of Infectious Diseases | volume = 196 | issue = 2 | pages = 281–8 | date = July 2007 | pmid = 17570116 | doi = 10.1086/518898 | doi-access = free }}</ref> The chance of death from a case of tuberculosis is about 4% {{as of|2008|lc=yes}}, down from 8% in 1995.<ref name=Lancet11/> |
|||
[[su:Tuberkulosis]] |
|||
[[fi:Tuberkuloosi]] |
|||
In people with smear-positive pulmonary TB (without HIV co-infection), after 5 years without treatment, 50-60% die while 20-25% achieve spontaneous resolution (cure). TB is almost always fatal in those with untreated HIV co-infection and death rates are increased even with antiretroviral treatment of HIV.<ref>{{Cite web|title=1.4 Prognosis - Tuberculosis|url=https://medicalguidelines.msf.org/viewport/TUB/latest/1-4-prognosis-20320185.html|access-date=25 August 2020|website=medicalguidelines.msf.org|archive-date=2 June 2021|archive-url=https://web.archive.org/web/20210602215007/https://medicalguidelines.msf.org/viewport/TUB/latest/1-4-prognosis-20320185.html|url-status=live}}</ref> |
|||
[[sv:Tuberkulos]] |
|||
[[ta:காச நோய்]] |
|||
== Epidemiology == |
|||
[[th:วัณโรค]] |
|||
[[vi:Lao]] |
|||
Roughly one-quarter of the world's population has been infected with ''M. tuberculosis'',<ref name=WHO2018Fact/> with new infections occurring in about 1% of the population each year.<ref name=WHO2002/> However, most infections with ''M. tuberculosis'' do not cause disease,<ref name=CDC>{{cite web|publisher=[[Centers for Disease Control and Prevention]] (CDC)|url=https://www.cdc.gov/tb/publications/factsheets/general/LTBIandActiveTB.htm|title=Fact Sheets: The Difference Between Latent TB Infection and Active TB Disease|date=20 June 2011|access-date=26 July 2011|url-status=live|archive-url=https://web.archive.org/web/20110804005502/http://www.cdc.gov/tb/publications/factsheets/general/LTBIandActiveTB.htm|archive-date=4 August 2011}}</ref> and 90–95% of infections remain asymptomatic.<ref name=Book90/> In 2012, an estimated 8.6 million chronic cases were active.<ref>{{cite web|title=Global tuberculosis report 2013|url=https://www.who.int/tb/publications/global_report/en/index.html|publisher=World Health Organization (WHO)|year=2013|url-status=live|archive-url=https://web.archive.org/web/20061212123736/http://www.who.int/tb/publications/global_report/en/index.html|archive-date=12 December 2006}}</ref> In 2010, 8.8 million new cases of tuberculosis were diagnosed, and 1.20–1.45 million deaths occurred (most of these occurring in [[Developing nation|developing countries]]).<ref name=WHO2011/><ref name=Loz2012>{{cite journal | vauthors = Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, etal | s2cid = 1541253 | title = Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010 | journal = Lancet | volume = 380 | issue = 9859 | pages = 2095–128 | date = December 2012 | pmid = 23245604 | doi = 10.1016/S0140-6736(12)61728-0 | pmc = 10790329 | hdl = 10536/DRO/DU:30050819 | url = https://zenodo.org/record/2557786 | hdl-access = free | access-date = 18 March 2020 | archive-date = 19 May 2020 | archive-url = https://web.archive.org/web/20200519152712/https://zenodo.org/record/2557786 | url-status = live }}</ref> Of these, about 0.35 million occur in those also infected with HIV.<ref name=WHO2011Control>{{cite web|title=Global Tuberculosis Control 2011 |url=https://www.who.int/tb/publications/global_report/2011/gtbr11_full.pdf |publisher=World Health Organization (WHO) |access-date=15 April 2012 |url-status=dead |archive-url=https://web.archive.org/web/20120617064025/http://www.who.int/tb/publications/global_report/2011/gtbr11_full.pdf |archive-date=17 June 2012 }}</ref> In 2018, tuberculosis was the leading cause of death worldwide from a single infectious agent.<ref>{{cite web |title=Tuberculosis |url=https://www.who.int/news-room/fact-sheets/detail/tuberculosis |website=WHO |date=24 March 2020 |access-date=31 May 2020 |archive-date=30 July 2020 |archive-url=https://web.archive.org/web/20200730165218/https://www.who.int/news-room/fact-sheets/detail/tuberculosis |url-status=live }}</ref> The total number of tuberculosis cases has been decreasing since 2005, while new cases have decreased since 2002.<ref name="WHO2011" /> |
|||
[[tr:Tüberküloz]] |
|||
[[uk:Туберкульоз]] |
|||
Tuberculosis{{Clarify|reason=Which one? Pulmonary?|date=December 2022}} incidence is seasonal, with peaks occurring every spring and summer.<ref>{{cite journal | vauthors = Douglas AS, Strachan DP, Maxwell JD | title = Seasonality of tuberculosis: the reverse of other respiratory diseases in the UK | journal = Thorax | volume = 51 | issue = 9 | pages = 944–946 | date = September 1996 | pmid = 8984709 | pmc = 472621 | doi = 10.1136/thx.51.9.944 }}</ref><ref>{{cite journal | vauthors = Martineau AR, Nhamoyebonde S, Oni T, Rangaka MX, Marais S, Bangani N, Tsekela R, Bashe L, de Azevedo V, Caldwell J, Venton TR, Timms PM, Wilkinson KA, Wilkinson RJ | title = Reciprocal seasonal variation in vitamin D status and tuberculosis notifications in Cape Town, South Africa | journal = Proceedings of the National Academy of Sciences of the United States of America | volume = 108 | issue = 47 | pages = 19013–19017 | date = November 2011 | pmid = 22025704 | pmc = 3223428 | doi = 10.1073/pnas.1111825108 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Parrinello CM, Crossa A, Harris TG | title = Seasonality of tuberculosis in New York City, 1990-2007 | journal = The International Journal of Tuberculosis and Lung Disease | volume = 16 | issue = 1 | pages = 32–37 | date = January 2012 | pmid = 22236842 | doi = 10.5588/ijtld.11.0145 }}</ref><ref name="Korthals2012">{{cite journal | vauthors = Korthals Altes H, Kremer K, Erkens C, van Soolingen D, Wallinga J | title = Tuberculosis seasonality in the Netherlands differs between natives and non-natives: a role for vitamin D deficiency? | journal = The International Journal of Tuberculosis and Lung Disease | volume = 16 | issue = 5 | pages = 639–644 | date = May 2012 | pmid = 22410705 | doi = 10.5588/ijtld.11.0680 }}</ref> The reasons for this are unclear, but may be related to vitamin D deficiency during the winter.<ref name="Korthals2012"/><ref>{{cite journal | vauthors = Koh GC, Hawthorne G, Turner AM, Kunst H, Dedicoat M | title = Tuberculosis incidence correlates with sunshine: an ecological 28-year time series study | journal = PLOS ONE | volume = 8 | issue = 3 | pages = e57752 | year = 2013 | pmid = 23483924 | pmc = 3590299 | doi = 10.1371/journal.pone.0057752 | doi-access = free | bibcode = 2013PLoSO...857752K }}</ref> There are also studies linking tuberculosis to different weather conditions like low temperature, low humidity and low rainfall. It has been suggested that tuberculosis incidence rates may be connected to climate change.<ref>{{cite journal | vauthors = Kuddus MA, McBryde ES, Adegboye OA | title = Delay effect and burden of weather-related tuberculosis cases in Rajshahi province, Bangladesh, 2007-2012 | journal = Scientific Reports | volume = 9 | issue = 1 | pages = 12720 | date = September 2019 | pmid = 31481739 | pmc = 6722246 | doi = 10.1038/s41598-019-49135-8 | bibcode = 2019NatSR...912720K }}</ref> |
|||
[[wa:Pitizeye des djins]] |
|||
[[yi:טובערקולאסיס]] |
|||
=== At-risk groups === |
|||
[[zh:肺結核]] |
|||
Tuberculosis is closely linked to both overcrowding and [[malnutrition]], making it one of the principal [[diseases of poverty]].<ref name="Lancet11" /> Those at high risk thus include: people who inject illicit drugs, inhabitants and employees of locales where vulnerable people gather (e.g., prisons and homeless shelters), medically underprivileged and resource-poor communities, high-risk ethnic minorities, children in close contact with high-risk category patients, and health-care providers serving these patients.<ref name="Griffith_1996">{{cite journal|vauthors=Griffith DE, Kerr CM|date=August 1996|title=Tuberculosis: disease of the past, disease of the present|journal=Journal of PeriAnesthesia Nursing|volume=11|issue=4|pages=240–45|doi=10.1016/S1089-9472(96)80023-2|pmid=8964016}}</ref> |
|||
The rate of tuberculosis varies with age. In Africa, it primarily affects adolescents and young adults.<ref>{{cite web|title=Global Tuberculosis Control Report, 2006 – Annex 1 Profiles of high-burden countries|url=https://www.who.int/tb/publications/global_report/2006/pdf/full_report_correctedversion.pdf|url-status=dead|archive-url=https://web.archive.org/web/20090726124358/http://www.who.int/tb/publications/global_report/2006/pdf/full_report_correctedversion.pdf|archive-date=26 July 2009|access-date=13 October 2006|publisher=World Health Organization (WHO)}}</ref> However, in countries where incidence rates have declined dramatically (such as the United States), tuberculosis is mainly a disease of the elderly and [[immunocompromise]]d (risk factors are listed above).<ref name="Robbins" /><ref>{{cite web|date=12 September 2006|title=2005 Surveillance Slide Set|url=https://www.cdc.gov/nchstp/tb/pubs/slidesets/surv/surv2005/default.htm|url-status=live|archive-url=https://web.archive.org/web/20061123122326/http://www.cdc.gov/nchstp/tb/pubs/slidesets/surv/surv2005/default.htm|archive-date=23 November 2006|access-date=13 October 2006|publisher=Centers for Disease Control and Prevention}}</ref> Worldwide, 22 "high-burden" states or countries together experience 80% of cases as well as 83% of deaths.<ref name="EIU 2014" /> |
|||
In Canada and Australia, tuberculosis is many times more common among the [[Indigenous peoples]], especially in remote areas.<ref>{{cite journal|vauthors=FitzGerald JM, Wang L, Elwood RK|date=February 2000|title=Tuberculosis: 13. Control of the disease among aboriginal people in Canada|journal=[[Canadian Medical Association Journal]]|volume=162|issue=3|pages=351–55|pmc=1231016|pmid=10693593}}</ref><ref>{{cite book| vauthors = Quah SR, Carrin G, Buse K, Heggenhougen K |url=https://books.google.com/books?id=IEXUrc0tr1wC&pg=PA424|title=Health Systems Policy, Finance, and Organization|publisher=Academic Press|year=2009|isbn=978-0-12-375087-7|location=Boston|page=424 |archive-url=https://web.archive.org/web/20150906220918/https://books.google.com/books?id=IEXUrc0tr1wC&pg=PA424|archive-date=6 September 2015|url-status=live}}</ref> Factors contributing to this include higher prevalence of predisposing health conditions and behaviours, and overcrowding and poverty. In some Canadian Indigenous groups, genetic susceptibility may play a role.<ref name=":0" /> |
|||
Socioeconomic status (SES) strongly affects TB risk. People of low SES are both more likely to contract TB and to be more severely affected by the disease. Those with low SES are more likely to be affected by risk factors for developing TB (e.g., malnutrition, indoor air pollution, HIV co-infection, etc.), and are additionally more likely to be exposed to crowded and poorly ventilated spaces. Inadequate healthcare also means that people with active disease who facilitate spread are not diagnosed and treated promptly; sick people thus remain in the infectious state and (continue to) spread the infection.<ref name=":0" /> |
|||
=== Geographical epidemiology === |
|||
The distribution of tuberculosis is not uniform across the globe; about 80% of the population in many African, Caribbean, South Asian, and eastern European countries test positive in tuberculin tests, while only 5–10% of the U.S. population test positive.<ref name="Robbins" /> Hopes of totally controlling the disease have been dramatically dampened because of many factors, including the difficulty of developing an effective vaccine, the expensive and time-consuming diagnostic process, the necessity of many months of treatment, the increase in HIV-associated tuberculosis, and the emergence of drug-resistant cases in the 1980s.<ref name="Lancet11" /> |
|||
In developed countries, tuberculosis is less common and is found mainly in urban areas. In Europe, deaths from TB fell from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. Improvements in public health were reducing tuberculosis even before the arrival of antibiotics, although the disease remained a significant threat to public health, such that when the [[Medical Research Council (UK)|Medical Research Council]] was formed in Britain in 1913 its initial focus was tuberculosis research.<ref>{{cite web | work = [[Medical Research Council (UK)|Medical Research Council]] | url = http://www.mrc.ac.uk/index/about/about-history/about-history-2.htm | title = Origins of the MRC. | archive-url = https://web.archive.org/web/20080411164838/http://www.mrc.ac.uk/index/about/about-history/about-history-2.htm | archive-date=11 April 2008 | access-date = 7 October 2006 }}</ref> |
|||
In 2010, rates per 100,000 people in different areas of the world were: globally 178, Africa 332, the Americas 36, Eastern Mediterranean 173, Europe 63, Southeast Asia 278, and Western Pacific 139.<ref name="WHO2011Control" /> |
|||
==== Russia ==== |
|||
Russia has achieved particularly dramatic progress with a decline in its TB mortality rate—from 61.9 per 100,000 in 1965 to 2.7 per 100,000 in 1993;<ref>{{Cite book |vauthors=Shkolnikov VM, Meslé F |chapter=The Russian Epidemiological Crisis as Mirrored by Mortality Trends |page=142 |year=1996 |url=https://www.rand.org/pubs/conf_proceedings/CF124.html |language=en |veditors=DaVanzo J, Farnsworth G |title=Russia's Demographic "Crisis" |publisher=RAND Corporation |isbn=0-8330-2446-9 |access-date=20 February 2023 |archive-date=20 February 2023 |archive-url=https://web.archive.org/web/20230220171629/https://www.rand.org/pubs/conf_proceedings/CF124.html |url-status=live }}</ref><ref name=WHO2011a>{{cite web | url = https://www.who.int/tb/publications/global_report/en/index.html | title = Global Tuberculosis Control | archive-url = https://web.archive.org/web/20061212123736/http://www.who.int/tb/publications/global_report/en/index.html | archive-date=12 December 2006 | publisher = World Health Organization | date = 2011 }}</ref> however, mortality rate increased to 24 per 100,000 in 2005 and then recoiled to 11 per 100,000 by 2015.<ref>{{Cite web|url=https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=RU&LAN=EN&outtype=html|title=WHO global tuberculosis report 2016. Annex 2. Country profiles: Russian Federation|access-date=22 August 2020|archive-date=14 July 2017|archive-url=https://web.archive.org/web/20170714043942/https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=RU&LAN=EN&outtype=html|url-status=dead}}</ref> |
|||
==== China ==== |
|||
China has achieved particularly dramatic progress, with about an 80% reduction in its TB mortality rate between 1990 and 2010.<ref name=WHO2011Control/> The number of new cases has declined by 17% between 2004 and 2014.<ref name="EIU 2014"/> |
|||
==== Africa ==== |
|||
In 2007, the country with the highest estimated incidence rate of TB was [[Eswatini]], with 1,200 cases per 100,000 people. In 2017, the country with the highest estimated [[Incidence (epidemiology)|incidence rate]] as a % of the population was [[Lesotho]], with 665 cases per 100,000 people.<ref name="Global tuberculosis report 2018">{{cite web|title=Global Tuberculosis Report 2018|url=http://apps.who.int/iris/bitstream/handle/10665/274453/9789241565646-eng.pdf?ua=1|access-date=27 September 2019|archive-date=7 August 2020|archive-url=https://web.archive.org/web/20200807121356/https://apps.who.int/iris/bitstream/handle/10665/274453/9789241565646-eng.pdf?ua=1|url-status=live}}</ref> |
|||
In South Africa, 54 200 people died in 2022 from TB. The incidence rate was 468 per 100 000 people; in 2015, this was 988 per 100 000. The total incidence was 280 000 in 2022; in 2015, this was 552 000.<ref>{{Cite web | vauthors = Tomlinson C |date=2023-11-10 |title=In-depth: What new WHO TB numbers mean for South Africa |url=https://www.spotlightnsp.co.za/2023/11/10/in-depth-what-new-who-tb-numbers-mean-for-sa/ |access-date=2024-03-27 |website=Spotlight |language=en-US}}</ref> |
|||
==== India ==== |
|||
As of 2017, India had the largest total incidence, with an estimated 2,740,000 cases.<ref name="Global tuberculosis report 2018"/> According to the [[World Health Organization]] (WHO), in 2000–2015, India's estimated mortality rate dropped from 55 to 36 per 100,000 population per year with estimated 480 thousand people died of TB in 2015.<ref>{{Cite web|url=https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=IN&LAN=EN&outtype=html|title=WHO Global tuberculosis report 2016: India|access-date=22 August 2020|archive-date=6 February 2018|archive-url=https://web.archive.org/web/20180206193815/https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=IN&LAN=EN&outtype=html|url-status=dead}}</ref><ref>{{cite web|url=http://www.dnaindia.com/health/report-govt-revisits-strategy-to-combat-tuberculosis-nadda-2388967|title=Govt revisits strategy to combat tuberculosis|work=Daily News and Analysis|date=8 April 2017|access-date=22 August 2020|archive-date=3 June 2021|archive-url=https://web.archive.org/web/20210603072417/https://www.dnaindia.com/health/report-govt-revisits-strategy-to-combat-tuberculosis-nadda-2388967|url-status=live}}</ref> In India a major proportion of tuberculosis patients are being treated by private partners and private hospitals. Evidence indicates that the tuberculosis national survey does not represent the number of cases that are diagnosed and recorded by private clinics and hospitals in India.<ref>{{cite journal | vauthors = Mahla RS | title = Prevalence of drug-resistant tuberculosis in South Africa | journal = The Lancet. Infectious Diseases | volume = 18 | issue = 8 | pages = 836 | date = August 2018 | pmid = 30064674 | doi = 10.1016/S1473-3099(18)30401-8 | doi-access = free }}</ref> |
|||
==== North America ==== |
|||
In the United States, [[Native Americans in the United States|Native Americans]] have a fivefold greater mortality from TB,<ref>{{cite book | vauthors = Birn AE |title= Textbook of International Health: Global Health in a Dynamic World |year= 2009 |page= 261 |publisher= Oxford University Press |isbn= 978-0-19-988521-3 |url= https://books.google.com/books?id=2XBB4-eYGZIC&pg=PT261 |url-status=live |archive-url= https://web.archive.org/web/20150906213750/https://books.google.com/books?id=2XBB4-eYGZIC&pg=PT261 |archive-date= 6 September 2015 }}</ref> and racial and ethnic minorities accounted for 84% of all reported TB cases.<ref>{{cite web|publisher=Centers for Disease Control and Prevention|url=https://www.cdc.gov/tb/statistics/surv/surv2012/slides/surv12.htm|title=CDC Surveillance Slides 2012 – TB|url-status=dead|archive-url=https://web.archive.org/web/20131109150519/http://www.cdc.gov/tb/statistics/surv/surv2012/slides/surv12.htm|archive-date=9 November 2013|date=24 October 2018|access-date=17 September 2017}}</ref> The overall tuberculosis case rate in the United States was 3 per 100,000 persons in 2017.<ref name="Global tuberculosis report 2018"/> |
|||
In Canada, tuberculosis was endemic in some rural areas as of 1998.<ref>{{cite journal|url=http://gateway.nlm.nih.gov/MeetingAbstracts/ma?f=102188560.html|title=Rural outbreaks of ''Mycobacterium tuberculosis'' in a Canadian province|journal=Abstr Intersci Conf Antimicrob Agents Chemother|year=1998|volume=38|page=555 |id=abstract no. L-27|vauthors=Al-Azem A, Kaushal Sharma M, Turenne C, Hoban D, Hershfield E, MacMorran J, Kabani A|url-status=dead|archive-url=https://web.archive.org/web/20111118161808/http://gateway.nlm.nih.gov/MeetingAbstracts/ma?f=102188560.html |archive-date=18 November 2011 }}</ref> |
|||
==== Western Europe ==== |
|||
In 2017, in the United Kingdom, the national average was 9 per 100,000 and the highest incidence rates in [[Western Europe]] were 20 per 100,000 in Portugal. |
|||
<gallery widths="300" heights="210"> |
|||
File:Tuberculosis incidence (per 100,000 people), OWID.svg|alt=Number of new cases of tuberculosis per 100,000 people in 2016.|Number of new cases of tuberculosis per 100,000 people in 2016<ref>{{cite web |title=Tuberculosis incidence (per 100,000 people) |url=https://ourworldindata.org/grapher/incidence-of-tuberculosis-sdgs |website=Our World in Data |access-date=7 March 2020 |archive-date=26 September 2019 |archive-url=https://web.archive.org/web/20190926041419/https://ourworldindata.org/grapher/incidence-of-tuberculosis-sdgs |url-status=live }}</ref> |
|||
File:Tuberculosis world map-Deaths per million persons-WHO2012.svg|Tuberculosis deaths per million persons in 2012 |
|||
File:Tuberculosis deaths by region, OWID.svg|alt=Tuberculosis deaths by region, 1990 to 2017.|Tuberculosis deaths by region, 1990 to 2017<ref>{{cite web |title=Tuberculosis deaths by region |url=https://ourworldindata.org/grapher/tuberculosis-deaths-region |website=Our World in Data |access-date=7 March 2020 |archive-date=8 May 2020 |archive-url=https://web.archive.org/web/20200508204644/https://ourworldindata.org/grapher/tuberculosis-deaths-region |url-status=live }}</ref> |
|||
</gallery> |
|||
== Society and culture == |
|||
=== Names === |
|||
Tuberculosis has been known by many names from the technical to the familiar.<ref name=Lawlor/> {{Lang|grc-latn|Phthisis}} ({{Lang|grc|Φθισις}}) is a Greek word for consumption, an old term for pulmonary tuberculosis;<ref name=Cha1998/> around 460 BCE, [[Hippocrates]] described phthisis as a disease of dry seasons.<ref>{{cite web |title=Hippocrates 3.16 Classics, MIT |url=https://classics.mit.edu/Hippocrates/aphorisms.mb.txt |access-date=15 December 2015 |archive-url=https://web.archive.org/web/20050211173218/http://classics.mit.edu/Hippocrates/aphorisms.mb.txt |archive-date=11 February 2005}}</ref> The abbreviation ''TB'' is short for ''tubercle [[Bacillus (shape)|bacillus]]''. ''Consumption'' was the most common nineteenth century English word for the disease, and was also in use well into the twentieth century. The Latin root {{Lang|la|con}} meaning 'completely' is linked to {{Lang|la|sumere}} meaning 'to take up from under'.<ref>{{cite book| vauthors = Caldwell M |title=The Last Crusade|date=1988|publisher=Macmillan|location=New York|isbn=978-0-689-11810-4|page=[https://archive.org/details/isbn_9780689118104/page/21 21]|url-access=registration|url=https://archive.org/details/isbn_9780689118104/page/21}}</ref> In ''[[The Life and Death of Mr Badman]]'' by [[John Bunyan]], the author calls consumption "the captain of all these men of death."<ref>{{cite book| vauthors = Bunyan J |date=1808 |title=The Life and Death of Mr. Badman|url=https://archive.org/details/lifeanddeathmrb01bunygoog |quote=captain. |page=[https://archive.org/details/lifeanddeathmrb01bunygoog/page/n238 244] |location=London |publisher=W. Nicholson |via=Internet Archive |access-date=28 September 2016}}</ref> "Great white plague" has also been used.<ref name=Lawlor/> |
|||
=== Art and literature === |
|||
[[File:Munch Det Syke Barn 1885-86.jpg|thumb|Painting ''[[The Sick Child (Munch)|The Sick Child]]'' by [[Edvard Munch]], 1885–1886, depicts the illness of his sister Sophie, who died of tuberculosis when Edvard was 14; his mother also died of the disease.]] |
|||
{{main|Cultural depictions of tuberculosis}} |
|||
Tuberculosis was for centuries associated with [[poet]]ic and [[art]]istic qualities among those infected, and was also known as "the romantic disease".<ref name=Lawlor>{{cite web| vauthors = Lawlor C |title=Katherine Byrne, Tuberculosis and the Victorian Literary Imagination|url=http://www.bsls.ac.uk/reviews/romantic-and-victorian/katherine-byrne-tuberculosis-and-the-victorian-literary-imagination/|publisher=British Society for Literature and Science|access-date=11 June 2017|archive-date=6 November 2020|archive-url=https://web.archive.org/web/20201106070752/http://www.bsls.ac.uk/reviews/romantic-and-victorian/katherine-byrne-tuberculosis-and-the-victorian-literary-imagination/|url-status=live}}</ref><ref>{{cite book | vauthors = Byrne K | title=Tuberculosis and the Victorian Literary Imagination |publisher=Cambridge University Press |year=2011 |isbn=978-1-107-67280-2}}</ref> Major artistic figures such as the poets [[John Keats]], [[Percy Bysshe Shelley]], and [[Edgar Allan Poe]], the composer [[Frédéric Chopin]],<ref name=IOE>{{cite web|title=About Chopin's illness|url=http://www.iconsofeurope.com/chopin.tuberculosis.htm|publisher=Icons of Europe|access-date=11 June 2017|archive-date=28 September 2017|archive-url=https://web.archive.org/web/20170928150213/http://www.iconsofeurope.com/chopin.tuberculosis.htm|url-status=live}}</ref> the playwright [[Anton Chekhov]], the novelists [[Franz Kafka]], [[Katherine Mansfield]],<ref name="Vilaplana2017">{{cite journal | vauthors = Vilaplana C | title = A literary approach to tuberculosis: lessons learned from Anton Chekhov, Franz Kafka, and Katherine Mansfield | journal = International Journal of Infectious Diseases | volume = 56 | pages = 283–85 | date = March 2017 | pmid = 27993687 | doi = 10.1016/j.ijid.2016.12.012 | doi-access = free }}</ref> [[Charlotte Brontë]], [[Fyodor Dostoevsky]], [[Thomas Mann]], [[W. Somerset Maugham]],<ref name=Rogal1997>{{cite book |vauthors=Rogal SJ |title=A William Somerset Maugham Encyclopedia |url=https://books.google.com/books?id=H0MqigagKTkC&pg=PA245 |year=1997 |publisher=Greenwood Publishing |isbn=978-0-313-29916-2 |page=245 |access-date=4 October 2017 |archive-date=2 June 2021 |archive-url=https://web.archive.org/web/20210602212607/https://books.google.com/books?id=H0MqigagKTkC&pg=PA245 |url-status=live }}</ref> [[George Orwell]],<ref>{{cite web | vauthors = Eschner K |title=George Orwell Wrote '1984' While Dying of Tuberculosis |url=https://www.smithsonianmag.com/smart-news/george-orwell-wrote-1984-while-dying-tuberculosis-180962608/ |website=Smithsonian |access-date=25 March 2019 |archive-date=24 March 2019 |archive-url=https://web.archive.org/web/20190324161820/https://www.smithsonianmag.com/smart-news/george-orwell-wrote-1984-while-dying-tuberculosis-180962608/ |url-status=live }}</ref> and [[Robert Louis Stevenson]], and the artists [[Alice Neel]],<ref name=JAMA2005>{{cite journal |journal=Journal of the American Medical Association |url=http://jamanetwork.com/journals/jama/issue/293/22 |page=cover |date=8 June 2005 |volume=293 |issue=22 |title=Tuberculosis (whole issue) |access-date=4 October 2017 |archive-date=24 August 2020 |archive-url=https://web.archive.org/web/20200824105736/https://jamanetwork.com/journals/jama/issue/293/22 |url-status=live }}</ref> [[Jean-Antoine Watteau]], [[Elizabeth Siddal]], [[Marie Bashkirtseff]], [[Edvard Munch]], [[Aubrey Beardsley]] and [[Amedeo Modigliani]] either had the disease or were surrounded by people who did. A widespread belief was that tuberculosis assisted artistic talent. Physical mechanisms proposed for this effect included the slight fever and toxaemia that it caused, allegedly helping them to see life more clearly and to act decisively.<ref name=Lemlein1981>{{cite journal |vauthors=Lemlein RF |s2cid=191371443 |title=Influence of Tuberculosis on the Work of Visual Artists: Several Prominent Examples |journal=Leonardo |date=1981 |volume=14 |issue=2 |pages=114–11 |jstor=1574402 |doi=10.2307/1574402 }}</ref><ref name=Wilsey>{{cite thesis | vauthors = Wilsey AM | title = 'Half in Love with Easeful Death:' Tuberculosis in Literature | date = May 2012 | work = Humanities Capstone Projects | degree = PhD Thesis | publisher = Pacific University | ref = Paper 11 | url = http://commons.pacificu.edu/cgi/viewcontent.cgi?article=1010&context=cashu | access-date = 28 September 2017 | archive-url = https://web.archive.org/web/20171011220904/http://commons.pacificu.edu/cgi/viewcontent.cgi?article=1010&context=cashu | archive-date = 11 October 2017 | url-status = dead }}</ref><ref name="Morens2002">{{cite journal | vauthors = Morens DM | title = At the deathbed of consumptive art | journal = Emerging Infectious Diseases | volume = 8 | issue = 11 | pages = 1353–8 | date = November 2002 | pmid = 12463180 | pmc = 2738548 | doi = 10.3201/eid0811.020549 }}</ref> |
|||
Tuberculosis formed an often-reused theme in [[literature]], as in [[Thomas Mann]]'s ''[[The Magic Mountain]]'', set in a [[sanatorium]];<ref name=McMasterUni>{{cite web |url=http://hsl.mcmaster.libguides.com/c.php?g=306775&p=2045587 |title=Pulmonary Tuberculosis/In Literature and Art| publisher=McMaster University History of Diseases |access-date=9 June 2017}}</ref> in [[music]], as in [[Van Morrison]]'s song "[[T.B. Sheets]]";<ref>{{cite news| vauthors = Thomson G |title=Van Morrison – 10 of the best|url=https://www.theguardian.com/music/musicblog/2016/jun/01/van-morrison-10-of-the-best|work=[[The Guardian]]|date=1 June 2016|access-date=28 September 2017|archive-date=14 August 2020|archive-url=https://web.archive.org/web/20200814152313/https://www.theguardian.com/music/musicblog/2016/jun/01/van-morrison-10-of-the-best|url-status=live}}</ref> in [[opera]], as in [[Giacomo Puccini|Puccini]]'s ''[[La bohème]]'' and [[Giuseppe Verdi|Verdi]]'s ''[[La Traviata]]'';<ref name="Morens2002"/> in [[art]], as in [[Edvard Munch|Munch]]'s painting of his ill sister;<ref name=USAID>{{cite web|title=Tuberculosis Throughout History: The Arts|url=https://www.usaid.gov/sites/default/files/documents/1864/art_poster.pdf|publisher=[[United States Agency for International Development]] (USAID)|access-date=12 June 2017|archive-date=30 June 2017|archive-url=https://web.archive.org/web/20170630123411/https://www.usaid.gov/sites/default/files/documents/1864/art_poster.pdf|url-status=live}}</ref> and in [[film]], such as the 1945 ''[[The Bells of St. Mary's]]'' starring [[Ingrid Bergman]] as a nun with tuberculosis.<ref name=Corliss2008>{{Cite magazine | vauthors = Corliss R |title=Top 10 Worst Christmas Movies |magazine=Time |url=http://entertainment.time.com/2011/12/20/top-10-worst-christmas-movies/ |date=22 December 2008 |quote='If you don't cry when Bing Crosby tells Ingrid Bergman she has tuberculosis', Joseph McBride wrote in 1973, 'I never want to meet you, and that's that.' |access-date=28 September 2017 |archive-date=22 September 2020 |archive-url=https://web.archive.org/web/20200922042323/https://entertainment.time.com/2011/12/20/top-10-worst-christmas-movies/ |url-status=live }}</ref> |
|||
=== Public health efforts === |
|||
{{Further information|Tuberculosis elimination}} |
|||
In 2014, the WHO adopted the "End TB" strategy which aims to reduce TB incidence by 80% and TB deaths by 90% by 2030.<ref name="who_end_tb">{{Cite web|url=https://www.who.int/teams/global-tuberculosis-programme/the-end-tb-strategy|title=The End TB Strategy|website=who.int|access-date=22 July 2021|archive-date=22 July 2021|archive-url=https://web.archive.org/web/20210722170507/https://www.who.int/teams/global-tuberculosis-programme/the-end-tb-strategy|url-status=live}}</ref> The strategy contains a milestone to reduce TB incidence by 20% and TB deaths by 35% by 2020.<ref name="2020_TB_report">{{Cite book |url=https://apps.who.int/iris/rest/bitstreams/1312164/retrieve |title=Global tuberculosis report 2020 |year=2020 | publisher = World Health Organization | isbn = 978-92-4-001313-1 |access-date=22 July 2021 |archive-date=22 July 2021 |archive-url= https://web.archive.org/web/20210722172009/https://apps.who.int/iris/rest/bitstreams/1312164/retrieve |url-status=live }}</ref> However, by 2020 only a 9% reduction in incidence per population was achieved globally, with the European region achieving 19% and the African region achieving 16% reductions.<ref name="2020_TB_report"/> Similarly, the number of deaths only fell by 14%, missing the 2020 milestone of a 35% reduction, with some regions making better progress (31% reduction in Europe and 19% in Africa).<ref name="2020_TB_report"/> Correspondingly, also treatment, prevention and funding milestones were missed in 2020, for example only 6.3 million people were started on TB prevention short of the target of 30 million.<ref name="2020_TB_report"/> |
|||
The World Health Organization (WHO), the [[Bill and Melinda Gates Foundation]], and the U.S. government are subsidizing a fast-acting diagnostic tuberculosis test for use in low- and middle-income countries as of 2012.<ref name=PressRelease2012/><ref name=Xpert2011>{{cite journal | vauthors = Lawn SD, Nicol MP | title = Xpert® MTB/RIF assay: development, evaluation and implementation of a new rapid molecular diagnostic for tuberculosis and rifampicin resistance | journal = Future Microbiology | volume = 6 | issue = 9 | pages = 1067–82 | date = September 2011 | pmid = 21958145 | pmc = 3252681 | doi = 10.2217/fmb.11.84 }}</ref><ref>{{cite news |url=https://www.reuters.com/article/idUSTRE6B71RF20101208 |title=WHO says Cepheid rapid test will transform TB care |work=[[Reuters]] |date=8 December 2010 |url-status=live |archive-url=https://web.archive.org/web/20101211140847/http://www.reuters.com/article/idUSTRE6B71RF20101208 |archive-date=11 December 2010 }}</ref> In addition to being fast-acting, the test can determine if there is resistance to the antibiotic rifampicin which may indicate multi-drug resistant tuberculosis and is accurate in those who are also infected with HIV.<ref name=PressRelease2012>{{cite web|title=Public–Private Partnership Announces Immediate 40 Percent Cost Reduction for Rapid TB Test|url=https://www.who.int/tb/features_archive/GeneXpert_press_release_final.pdf|publisher=World Health Organization (WHO)|date=6 August 2012|url-status=live|archive-url=https://web.archive.org/web/20131029234310/http://www.who.int/tb/features_archive/GeneXpert_press_release_final.pdf|archive-date=29 October 2013}}</ref><ref>{{cite web|title=The Stop TB Partnership, which operates through a secretariat hosted by the World Health Organization (WHO) in Geneva, Switzerland|url=http://www.stoptb.org/wg/gli/assets/documents/map/XpertPublications.pdf|author=STOPTB|date=5 April 2013|url-status=live|archive-url=https://web.archive.org/web/20140124041952/http://www.stoptb.org/wg/gli/assets/documents/map/XpertPublications.pdf|archive-date=24 January 2014}}</ref> Many resource-poor places {{as of|2011|lc=yes}} have access to only sputum microscopy.<ref>{{cite journal | vauthors = Lienhardt C, Espinal M, Pai M, Maher D, Raviglione MC | title = What research is needed to stop TB? Introducing the TB Research Movement | journal = PLOS Medicine | volume = 8 | issue = 11 | pages = e1001135 | date = November 2011 | pmid = 22140369 | pmc = 3226454 | doi = 10.1371/journal.pmed.1001135 | doi-access = free }}</ref> |
|||
India had the highest total number of TB cases worldwide in 2010, in part due to poor disease management within the private and public health care sector.<ref>{{Cite journal| vauthors = Sandhu GK |date=2011|title=Tuberculosis: Current Situation, Challenges and Overview of its Control Programs in India|journal=Journal of Global Infectious Diseases|volume=3|issue=2|pages=143–150|doi=10.4103/0974-777X.81691|issn=0974-777X|pmc=3125027|pmid=21731301 |doi-access=free }}</ref> Programs such as the [[Revised National Tuberculosis Control Program]] are working to reduce TB levels among people receiving public health care.<ref name="Bhargava">{{cite journal | vauthors = Bhargava A, Pinto L, Pai M |title=Mismanagement of tuberculosis in India: Causes, consequences, and the way forward |journal=Hypothesis |volume=9 |issue=1 |page=e7 |year=2011 |url=https://www.paitbgroup.org/wp-content/uploads/Papers/2011/2011-XX-BhargavaA-Hyp.pdf |archive-url=https://web.archive.org/web/20221024060219/https://www.paitbgroup.org/wp-content/uploads/Papers/2011/2011-XX-BhargavaA-Hyp.pdf |archive-date=24 October 2022 }}</ref><ref>{{cite journal | vauthors = Amdekar Y | s2cid = 41788291 | title = Changes in the management of tuberculosis | journal = Indian Journal of Pediatrics | volume = 76 | issue = 7 | pages = 739–42 | date = July 2009 | pmid = 19693453 | doi = 10.1007/s12098-009-0164-4 }}</ref> |
|||
A 2014 [[Economist Intelligence Unit|EIU]]-healthcare report finds there is a need to address apathy and urges for increased funding. The report cites among others Lucica Ditui "[TB] is like an orphan. It has been neglected even in countries with a high burden and often forgotten by donors and those investing in health interventions."<ref name="EIU 2014"/> |
|||
Slow progress has led to frustration, expressed by the executive director of the [[Global Fund to Fight AIDS, Tuberculosis and Malaria]] – Mark Dybul: "we have the tools to end TB as a pandemic and public health threat on the planet, but we are not doing it."<ref name="EIU 2014"/> Several international organizations are pushing for more transparency in treatment, and more countries are implementing mandatory reporting of cases to the government as of 2014, although adherence is often variable. Commercial treatment providers may at times overprescribe second-line drugs as well as supplementary treatment, promoting demands for further regulations.<ref name="EIU 2014"/> The government of Brazil provides universal TB care, which reduces this problem.<ref name="EIU 2014"/> Conversely, falling rates of TB infection may not relate to the number of programs directed at reducing infection rates but may be tied to an increased level of education, income, and health of the population.<ref name="EIU 2014"/> Costs of the disease, as calculated by the [[World Bank]] in 2009 may exceed US$150 billion per year in "high burden" countries.<ref name="EIU 2014"/> Lack of progress eradicating the disease may also be due to lack of patient follow-up – as among the 250 million [[migration in China|rural migrants in China]].<ref name="EIU 2014"/> |
|||
There is insufficient data to show that active contact tracing helps to improve case detection rates for tuberculosis.<ref>{{cite journal | vauthors = Fox GJ, Dobler CC, Marks GB | title = Active case finding in contacts of people with tuberculosis | journal = The Cochrane Database of Systematic Reviews | issue = 9 | pages = CD008477 | date = September 2011 | volume = 2011 | pmid = 21901723 | pmc = 6532613 | doi = 10.1002/14651858.CD008477.pub2 }}</ref> Interventions such as house-to-house visits, educational leaflets, mass media strategies, educational sessions may increase tuberculosis detection rates in short-term.<ref>{{cite journal | vauthors = Mhimbira FA, Cuevas LE, Dacombe R, Mkopi A, Sinclair D | title = Interventions to increase tuberculosis case detection at primary healthcare or community-level services | journal = The Cochrane Database of Systematic Reviews | volume = 2017 | pages = CD011432 | date = November 2017 | issue = 11 | pmid = 29182800 | pmc = 5721626 | doi = 10.1002/14651858.CD011432.pub2 | collaboration = Cochrane Infectious Diseases Group }}</ref> There is no study that compares new methods of contact tracing such as social network analysis with existing contact tracing methods.<ref>{{cite journal | vauthors = Braganza Menezes D, Menezes B, Dedicoat M | title = Contact tracing strategies in household and congregate environments to identify cases of tuberculosis in low- and moderate-incidence populations | journal = The Cochrane Database of Systematic Reviews | volume = 2019 | pages = CD013077 | date = August 2019 | issue = 8 | pmid = 31461540 | pmc = 6713498 | doi = 10.1002/14651858.CD013077.pub2 | collaboration = Cochrane Infectious Diseases Group }}</ref> |
|||
=== Stigma === |
|||
Slow progress in preventing the disease may in part be due to [[social stigma|stigma]] associated with TB.<ref name="EIU 2014"/> Stigma may be due to the fear of transmission from affected individuals. This stigma may additionally arise due to links between TB and poverty, and in [[AIDS in Africa|Africa, AIDS]].<ref name="EIU 2014"/> Such stigmatization may be both real and perceived; for example, in Ghana, individuals with TB are banned from attending public gatherings.<ref name="Courtwright 2010">{{cite journal | vauthors = Courtwright A, Turner AN | title = Tuberculosis and stigmatization: pathways and interventions | journal = Public Health Reports | volume = 125 | issue = 4_suppl | pages = 34–42 | date = Jul–Aug 2010 | pmid = 20626191 | pmc = 2882973 | doi = 10.1177/00333549101250S407 }}</ref> |
|||
Stigma towards TB may result in delays in seeking treatment,<ref name="EIU 2014"/> lower treatment compliance, and family members keeping cause of death secret<ref name="Courtwright 2010"/> – allowing the disease to spread further.<ref name="EIU 2014"/> In contrast, in Russia stigma was associated with increased treatment compliance.<ref name="Courtwright 2010"/> TB stigma also affects socially marginalized individuals to a greater degree and varies between regions.<ref name="Courtwright 2010"/> |
|||
One way to decrease stigma may be through the promotion of "TB clubs", where those infected may share experiences and offer support, or through counseling.<ref name="Courtwright 2010"/> Some studies have shown TB education programs to be effective in decreasing stigma, and may thus be effective in increasing treatment adherence.<ref name="Courtwright 2010"/> Despite this, studies on the relationship between reduced stigma and mortality are lacking {{as of|2010|lc=yes}}, and similar efforts to decrease stigma surrounding AIDS have been minimally effective.<ref name="Courtwright 2010"/> Some have claimed the stigma to be worse than the disease, and healthcare providers may unintentionally reinforce stigma, as those with TB are often perceived as difficult or otherwise undesirable.<ref name="EIU 2014"/> A greater understanding of the social and cultural dimensions of tuberculosis may also help with stigma reduction.<ref>{{cite journal | vauthors = Mason PH, Roy A, Spillane J, Singh P | title = Social, Historical and Cultural Dimensions of Tuberculosis | journal = Journal of Biosocial Science | volume = 48 | issue = 2 | pages = 206–32 | date = March 2016 | pmid = 25997539 | doi = 10.1017/S0021932015000115 | doi-access = free }}</ref> |
|||
== Research == |
|||
{{see also|International Congress on Tuberculosis}} |
|||
The BCG vaccine has limitations, and research to develop new TB vaccines is ongoing.<ref name=VacRes2011>{{cite journal | vauthors = Martín Montañés C, Gicquel B | title = New tuberculosis vaccines | journal = Enfermedades Infecciosas y Microbiologia Clinica | volume = 29 | pages = 57–62 | date = March 2011 | issue = Suppl 1 | pmid = 21420568 | doi = 10.1016/S0213-005X(11)70019-2 }}</ref> A number of potential candidates are currently in [[clinical trial|phase I and II clinical trials]].<ref name=VacRes2011/><ref>{{cite journal | vauthors = Zhu B, Dockrell HM, Ottenhoff TH, Evans TG, Zhang Y | title = Tuberculosis vaccines: Opportunities and challenges | journal = Respirology | volume = 23 | issue = 4 | pages = 359–368 | date = April 2018 | pmid = 29341430 | doi = 10.1111/resp.13245 | doi-access = free | hdl = 1887/77156 | hdl-access = free }}</ref> Two main approaches are used to attempt to improve the efficacy of available vaccines. One approach involves adding a subunit vaccine to BCG, while the other strategy is attempting to create new and better live vaccines.<ref name=VacRes2011/> [[MVA85A]], an example of a subunit vaccine, is in trials in South Africa as of 2006, is based on a genetically modified [[vaccinia]] virus.<ref name=Ibanga_2006>{{cite journal | vauthors = Ibanga HB, Brookes RH, Hill PC, Owiafe PK, Fletcher HA, Lienhardt C, Hill AV, Adegbola RA, McShane H | title = Early clinical trials with a new tuberculosis vaccine, MVA85A, in tuberculosis-endemic countries: issues in study design | journal = The Lancet. Infectious Diseases | volume = 6 | issue = 8 | pages = 522–8 | date = August 2006 | pmid = 16870530 | doi = 10.1016/S1473-3099(06)70552-7 }}</ref> Vaccines are hoped to play a significant role in treatment of both latent and active disease.<ref>{{cite journal | vauthors = Kaufmann SH | title = Future vaccination strategies against tuberculosis: thinking outside the box | journal = Immunity | volume = 33 | issue = 4 | pages = 567–77 | date = October 2010 | pmid = 21029966 | doi = 10.1016/j.immuni.2010.09.015 | doi-access = free }}</ref> |
|||
To encourage further discovery, researchers and policymakers are promoting new economic models of vaccine development as of 2006, including prizes, tax incentives, and [[advance market commitments]].<ref>{{cite journal| vauthors = Webber D, Kremer M |url=https://www.who.int/bulletin/archives/79(8)735.pdf |title=Stimulating Industrial R&D for Neglected Infectious Diseases: Economic Perspectives|journal=Bulletin of the World Health Organization|volume=79|issue=8|year=2001|pages=693–801|url-status=live|archive-url=https://web.archive.org/web/20070926012031/http://www.who.int/bulletin/archives/79(8)735.pdf|archive-date=26 September 2007}}</ref><ref>{{cite journal| vauthors = Barder O, Kremer M, Williams H |s2cid=154454583|url=http://www.bepress.com/ev/vol3/iss3/art1|title=Advance Market Commitments: A Policy to Stimulate Investment in Vaccines for Neglected Diseases|journal=The Economists' Voice|volume=3|year=2006|issue=3|doi=10.2202/1553-3832.1144|url-status=dead|archive-url=https://web.archive.org/web/20061105083659/http://www.bepress.com/ev/vol3/iss3/art1|archive-date=5 November 2006}}</ref> A number of groups, including the [[Stop TB Partnership]],<ref>{{cite book | author = Department of Economic and Social Affairs |title=Achieving the global public health agenda: dialogues at the Economic and Social Council|year=2009|publisher=[[United Nations]]|location=New York|isbn=978-92-1-104596-3|page=103|url=https://books.google.com/books?id=VeF9dv74C4MC&pg=PA103 |url-status=live|archive-url=https://web.archive.org/web/20150906212013/https://books.google.com/books?id=VeF9dv74C4MC&pg=PA103|archive-date=6 September 2015}}</ref> the South African Tuberculosis Vaccine Initiative, and the Aeras Global TB Vaccine Foundation, are involved with research.<ref>{{cite book| vauthors = Jong EC, Zuckerman JN |title=Travelers' vaccines|year=2010|publisher=People's Medical Publishing House|location=Shelton, CT|isbn=978-1-60795-045-5|page=319|url=https://books.google.com/books?id=BKRpWFEy66wC&pg=PA319|edition=2nd|url-status=live|archive-url=https://web.archive.org/web/20150906203627/https://books.google.com/books?id=BKRpWFEy66wC&pg=PA319|archive-date=6 September 2015}}</ref> Among these, the Aeras Global TB Vaccine Foundation received a gift of more than $280 million (US) from the [[Bill and Melinda Gates Foundation]] to develop and license an improved vaccine against tuberculosis for use in high burden countries.<ref>{{Cite web|last=Bill and Melinda Gates Foundation Announcement |title=Gates Foundation Commits $82.9 Million to Develop New Tuberculosis Vaccines |date=12 February 2004 |url=http://www.globalhealth.org/news/article/4134 |url-status=dead |archive-url=https://web.archive.org/web/20091010163118/http://www.globalhealth.org/news/article/4134 |archive-date=10 October 2009 }}</ref><ref>{{Cite web| vauthors = Nightingale K |title=Gates foundation gives US$280 million to fight TB|date=19 September 2007|url=http://www.scidev.net/en/news/gates-foundation-gives-us280-million-to-fight-tb.html|url-status=live|archive-url=https://web.archive.org/web/20081201175618/http://www.scidev.net/en/news/gates-foundation-gives-us280-million-to-fight-tb.html|archive-date=1 December 2008}}</ref> |
|||
In 2012 a new medication regimen was approved in the US for multidrug-resistant tuberculosis, using [[bedaquiline]] as well as existing drugs. There were initial concerns about the safety of this drug,<ref name="Zumla2012">{{cite journal | vauthors = Zumla A, Hafner R, Lienhardt C, Hoelscher M, Nunn A | title = Advancing the development of tuberculosis therapy | journal = Nature Reviews. Drug Discovery | volume = 11 | issue = 3 | pages = 171–172 | date = March 2012 | pmid = 22378254 | doi = 10.1038/nrd3694 | url = http://www.nature.com/articles/nrd3694 | url-status = live | access-date = 8 May 2020 | s2cid = 7232434 | archive-url = https://web.archive.org/web/20200112192759/https://www.nature.com/articles/nrd3694 | archive-date = 12 January 2020 }}</ref><ref>{{cite news |date=31 December 2012 |title=J&J Sirturo Wins FDA Approval to Treat Drug-Resistant TB |url=https://www.bloomberg.com/news/2012-12-31/j-j-sirturo-wins-fda-approval-to-treat-drug-resistant-tb.html |url-status=live |archive-url=https://web.archive.org/web/20130104110903/http://www.bloomberg.com/news/2012-12-31/j-j-sirturo-wins-fda-approval-to-treat-drug-resistant-tb.html |archive-date=4 January 2013 |access-date=1 January 2013 |newspaper=[[Bloomberg News]]}}</ref><ref name="Avorn 2013 1349–1350">{{cite journal | vauthors = Avorn J | title = Approval of a tuberculosis drug based on a paradoxical surrogate measure | journal = JAMA | volume = 309 | issue = 13 | pages = 1349–1350 | date = April 2013 | pmid = 23430122 | doi = 10.1001/jama.2013.623 }}</ref><ref name="US Food and Drug Administration website">{{cite web |last=US Food and Drug Administration |title=Briefing Package: NDA 204–384: Sirturo |url=https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/Anti-%20InfectiveDrugsAdvisoryCommittee/UCM329258.pdf |url-status=live |archive-url=https://web.archive.org/web/20140104212835/https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/Anti-%20InfectiveDrugsAdvisoryCommittee/UCM329258.pdf |archive-date=4 January 2014 |website=[[Food and Drug Administration]]}}</ref><ref>{{cite journal |vauthors=Zuckerman D, Yttri J |date=January 2013 |title=Antibiotics: When science and wishful thinking collide |url=https://www.healthaffairs.org/do/10.1377/forefront.20130125.027503 |url-status=live |journal=Health Affairs |doi=10.1377/forefront.20130125.027503 |archive-url=https://web.archive.org/web/20220329211404/https://www.healthaffairs.org/do/10.1377/forefront.20130125.027503 |archive-date=29 March 2022 |access-date=29 March 2022}}</ref> but later research on larger groups found that this regimen improved health outcomes.<ref>{{cite journal | vauthors = Mbuagbaw L, Guglielmetti L, Hewison C, Bakare N, Bastard M, Caumes E, Fréchet-Jachym M, Robert J, Veziris N, Khachatryan N, Kotrikadze T, Hayrapetyan A, Avaliani Z, Schünemann HJ, Lienhardt C | title = Outcomes of Bedaquiline Treatment in Patients with Multidrug-Resistant Tuberculosis | journal = Emerging Infectious Diseases | volume = 25 | issue = 5 | pages = 936–943 | date = May 2019 | pmid = 31002070 | pmc = 6478224 | doi = 10.3201/eid2505.181823 }}</ref> By 2017 the drug was used in at least 89 countries.<ref>{{cite journal | vauthors = Khoshnood S, Taki E, Sadeghifard N, Kaviar VH, Haddadi MH, Farshadzadeh Z, Kouhsari E, Goudarzi M, Heidary M | title = Mechanism of Action, Resistance, Synergism, and Clinical Implications of Delamanid Against Multidrug-Resistant <i>Mycobacterium tuberculosis</i> | journal = Frontiers in Microbiology | volume = 12 | pages = 717045 | date = 2021-10-07 | pmid = 34690963 | pmc = 8529252 | doi = 10.3389/fmicb.2021.717045 | doi-access = free }}</ref> Another new drug is [[delamanid]], which was first approved by the European Medicines Agency in 2013 to be used in multidrug-resistant tuberculosis patients,<ref>{{Cite web |date=2013-12-03 |title=European Medicines Agency - News and Events - European Medicines Agency recommends two new treatment options for tuberculosis |url=http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2013/11/news_detail_001972.jsp&mid=WC0b01ac058004d5c1 |access-date=2024-04-09 |archive-url=https://web.archive.org/web/20131203022613/http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2013/11/news_detail_001972.jsp&mid=WC0b01ac058004d5c1 |archive-date=3 December 2013 }}</ref> and by 2017 was used in at least 54 countries.<ref>{{cite journal | vauthors = Khoshnood S, Taki E, Sadeghifard N, Kaviar VH, Haddadi MH, Farshadzadeh Z, Kouhsari E, Goudarzi M, Heidary M | title = Mechanism of Action, Resistance, Synergism, and Clinical Implications of Delamanid Against Multidrug-Resistant <i>Mycobacterium tuberculosis</i> | journal = Frontiers in Microbiology | volume = 12 | pages = 717045 | date = 2021-10-07 | pmid = 34690963 | pmc = 8529252 | doi = 10.3389/fmicb.2021.717045 | doi-access = free }}</ref> |
|||
Steroids add-on therapy has not shown any benefits for active pulmonary tuberculosis infection.<ref>{{cite journal | vauthors = Critchley JA, Orton LC, Pearson F | title = Adjunctive steroid therapy for managing pulmonary tuberculosis | journal = The Cochrane Database of Systematic Reviews | issue = 11 | pages = CD011370 | date = November 2014 | volume = 2014 | pmid = 25387839 | pmc = 6532561 | doi = 10.1002/14651858.CD011370 }}</ref> |
|||
== Other animals == |
|||
Mycobacteria infect many different animals, including birds,<ref>{{cite journal | vauthors = Shivaprasad HL, Palmieri C | title = Pathology of mycobacteriosis in birds | journal = The Veterinary Clinics of North America. Exotic Animal Practice | volume = 15 | issue = 1 | pages = 41–55, v–vi | date = January 2012 | pmid = 22244112 | doi = 10.1016/j.cvex.2011.11.004 }}</ref> fish, rodents,<ref>{{cite journal | vauthors = Reavill DR, Schmidt RE | title = Mycobacterial lesions in fish, amphibians, reptiles, rodents, lagomorphs, and ferrets with reference to animal models | journal = The Veterinary Clinics of North America. Exotic Animal Practice | volume = 15 | issue = 1 | pages = 25–40, v | date = January 2012 | pmid = 22244111 | doi = 10.1016/j.cvex.2011.10.001 }}</ref> and reptiles.<ref>{{cite journal | vauthors = Mitchell MA | title = Mycobacterial infections in reptiles | journal = The Veterinary Clinics of North America. Exotic Animal Practice | volume = 15 | issue = 1 | pages = 101–11, vii | date = January 2012 | pmid = 22244116 | doi = 10.1016/j.cvex.2011.10.002 }}</ref> The subspecies ''Mycobacterium tuberculosis'', though, is rarely present in wild animals.<ref>{{cite book| vauthors = Wobeser GA |title=Essentials of disease in wild animals|year=2006|publisher=Blackwell Publishing|location=Ames, IO [u.a.]|isbn=978-0-8138-0589-4|page=170|url=https://books.google.com/books?id=JgyS6fxVasYC&pg=PA170|edition=1st|url-status=live|archive-url=https://web.archive.org/web/20150906172856/https://books.google.com/books?id=JgyS6fxVasYC&pg=PA170|archive-date=6 September 2015}}</ref> An effort to eradicate bovine tuberculosis caused by ''[[Mycobacterium bovis]]'' from the cattle and deer herds of [[New Zealand]] has been relatively successful.<ref>{{cite journal | vauthors = Ryan TJ, Livingstone PG, Ramsey DS, de Lisle GW, Nugent G, Collins DM, Buddle BM | title = Advances in understanding disease epidemiology and implications for control and eradication of tuberculosis in livestock: the experience from New Zealand | journal = Veterinary Microbiology | volume = 112 | issue = 2–4 | pages = 211–19 | date = February 2006 | pmid = 16330161 | doi = 10.1016/j.vetmic.2005.11.025 }}</ref> Efforts in Great Britain have been less successful.<ref>{{cite journal | vauthors = White PC, Böhm M, Marion G, Hutchings MR | title = Control of bovine tuberculosis in British livestock: there is no 'silver bullet' | journal = Trends in Microbiology | volume = 16 | issue = 9 | pages = 420–7 | date = September 2008 | pmid = 18706814 | doi = 10.1016/j.tim.2008.06.005 | citeseerx = 10.1.1.566.5547 }}</ref><ref>{{cite journal | vauthors = Ward AI, Judge J, Delahay RJ | title = Farm husbandry and badger behaviour: opportunities to manage badger to cattle transmission of Mycobacterium bovis? | journal = Preventive Veterinary Medicine | volume = 93 | issue = 1 | pages = 2–10 | date = January 2010 | pmid = 19846226 | doi = 10.1016/j.prevetmed.2009.09.014 }}</ref> |
|||
{{As of|2015}}, tuberculosis appears to be widespread among captive [[elephant]]s in the US. It is believed that the animals originally acquired the disease from humans, a process called [[reverse zoonosis]]. Because the disease can spread through the air to infect both humans and other animals, it is a public health concern affecting [[circus]]es and [[zoo]]s.<ref name="Holt">{{cite web | vauthors = Holt N |title=The Infected Elephant in the Room |url= http://www.slate.com/blogs/wild_things/2015/03/24/elephant_tuberculosis_epidemic_zoo_and_circus_animals_passing_tb_to_humans.html|website=[[Slate (magazine)|Slate]]|access-date=5 April 2016|date=24 March 2015|url-status=live|archive-url=https://web.archive.org/web/20160414151050/http://www.slate.com/blogs/wild_things/2015/03/24/elephant_tuberculosis_epidemic_zoo_and_circus_animals_passing_tb_to_humans.html|archive-date=14 April 2016}}</ref><ref name="Mikota">{{cite web| vauthors = Mikota SK |title=A Brief History of TB in Elephants |url= https://www.aphis.usda.gov/animal_welfare/downloads/elephant/A%20Brief%20History%20of%20TB%20in%20Elephants.pdf|publisher=[[Animal and Plant Health Inspection Service]] (APHIS)|access-date=5 April 2016|url-status=live|archive-url=https://web.archive.org/web/20161006125349/https://www.aphis.usda.gov/animal_welfare/downloads/elephant/A%20Brief%20History%20of%20TB%20in%20Elephants.pdf|archive-date=6 October 2016}}</ref> |
|||
== See also == |
|||
* [[List of deaths due to tuberculosis]] |
|||
== Notes == |
|||
{{notelist}} |
|||
== References == |
|||
{{Reflist}} |
|||
== External links == |
|||
<!-- Please DO ''not'' add new external links! Instead please submit them on the Talk page for discussion about their proposed inclusion. Thank you. --> |
|||
{{Sisterlinks|d=Q12204|wikt=tuberculosis|q=Tuberculosis|c=Category:Tuberculosis|n=no|b=no|v=no|voy=no|m=no|mw=no|s=no|species=Mycobacterium tuberculosis}} |
|||
{{Offline|med}} |
|||
* {{curlie|Health/Conditions_and_Diseases/Infectious_Diseases/Mycobacterial/Tuberculosis/}} |
|||
* {{cite web |url=https://www.cdc.gov/tb/default.htm |publisher=Centers for Disease Control and Prevention (CDC) |title=Tuberculosis (TB)|date=24 October 2018 }} |
|||
* {{cite web |url=http://www.hpa.org.uk/infections/topics_az/tb/menu.htm |publisher=[[Health Protection Agency]] |location=London |title=Tuberculosis (TB) |url-status=dead |archive-url=https://web.archive.org/web/20070705100742/http://www.hpa.org.uk/infections/topics_az/tb/menu.htm |archive-date=5 July 2007 }} |
|||
* [https://www.who.int/tb/global-tb-report-infographic.pdf?ua=1 WHO global 2016 TB report (infographic)] |
|||
* [https://www.who.int/tb/country/data/profiles/en/ WHO tuberculosis country profiles] |
|||
* [https://americanarchive.org/catalog/cpb-aacip_529-1c1td9p67s "Tuberculosis Among African Americans"], 1990-11-01, ''[[In Black America]]''; [[KUT|KUT Radio]], [[American Archive of Public Broadcasting]] ([[WGBH Educational Foundation|WGBH]] and the Library of Congress) |
|||
* [https://www.newtbdrugs.org/ Working Group on New TB drugs], tracking clinical trials and drug candidates |
|||
{{Medical condition classification and resources |
|||
| DiseasesDB = 8515 |
|||
| ICD11 = {{ICD11|1B10}}-{{ICD11|1B1Z}} |
|||
| ICD10 = {{ICD10|A15-A19}} |
|||
| ICD9 = {{ICD9|010}}–{{ICD9|018}} |
|||
| OMIM = 607948 |
|||
| MedlinePlus = 000077 |
|||
| MedlinePlus_mult = {{MedlinePlus2|000624}} |
|||
| eMedicineSubj = med |
|||
| eMedicineTopic = 2324 |
|||
| eMedicine_mult = {{eMedicine2|emerg|618}} {{eMedicine2|radio|411}} |
|||
| MeshID = D014376 |
|||
| Orphanet=3389 |
|||
| Scholia=Q12204 |
|||
}} |
|||
{{Gram-positive actinobacteria diseases}} |
|||
{{Tuberculosis}} |
|||
{{Diseases of Poverty}} |
|||
{{Portal bar | Medicine}} |
|||
{{Authority control}} |
|||
[[Category:Tuberculosis| ]] |
|||
[[Category:Airborne diseases]] |
|||
[[Category:Articles containing video clips]] |
|||
[[Category:Health in Africa]] |
|||
[[Category:Healthcare-associated infections]] |
|||
[[Category:Infectious causes of cancer]] |
|||
[[Category:Mycobacterium-related cutaneous conditions]] |
|||
[[Category:Vaccine-preventable diseases]] |
|||
[[Category:Wikipedia infectious disease articles ready to translate]] |
|||
[[Category:Wikipedia medicine articles ready to translate (full)]] |
|||
Latest revision as of 09:50, 5 June 2024
| Tuberculosis | |
|---|---|
| Other names | Phthisis, phthisis pulmonalis, consumption, great white plague |
 | |
| Chest X-ray of a person with advanced tuberculosis: Infection in both lungs is marked by white arrow-heads, and the formation of a cavity is marked by black arrows. | |
| Specialty | Infectious disease, pulmonology |
| Symptoms | Chronic cough, fever, cough with bloody mucus, weight loss[1] |
| Causes | Mycobacterium tuberculosis[1] |
| Risk factors | Smoking, HIV/AIDS[1] |
| Diagnostic method | CXR, culture, tuberculin skin test, QuantiFERON[1] |
| Differential diagnosis | Pneumonia, histoplasmosis, sarcoidosis, coccidioidomycosis[2] |
| Prevention | Screening those at high risk, treatment of those infected, vaccination with bacillus Calmette-Guérin (BCG)[3][4][5] |
| Treatment | Antibiotics[1] |
| Frequency | 25% of people (latent TB)[6] |
| Deaths | 1.3 million (2022)[6] |
Tuberculosis (TB), also known colloquially as the "white death", or historically as consumption,[7] is an infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria.[1] Tuberculosis generally affects the lungs, but it can also affect other parts of the body.[1] Most infections show no symptoms, in which case it is known as latent tuberculosis.[1] Around 10% of latent infections progress to active disease which, if left untreated, kill about half of those affected.[1] Typical symptoms of active TB are chronic cough with blood-containing mucus, fever, night sweats, and weight loss.[1] Infection of other organs can cause a wide range of symptoms.[8]
Tuberculosis is spread from one person to the next through the air when people who have active TB in their lungs cough, spit, speak, or sneeze.[1][9] People with latent TB do not spread the disease.[1] Active infection occurs more often in people with HIV/AIDS and in those who smoke.[1] Diagnosis of active TB is based on chest X-rays, as well as microscopic examination and culture of body fluids.[10] Diagnosis of latent TB relies on the tuberculin skin test (TST) or blood tests.[10]
Prevention of TB involves screening those at high risk, early detection and treatment of cases, and vaccination with the bacillus Calmette-Guérin (BCG) vaccine.[3][4][5] Those at high risk include household, workplace, and social contacts of people with active TB.[4] Treatment requires the use of multiple antibiotics over a long period of time.[1] Antibiotic resistance is a growing problem, with increasing rates of multiple drug-resistant tuberculosis (MDR-TB).[1]
In 2018, one quarter of the world's population was thought to have a latent infection of TB.[6] New infections occur in about 1% of the population each year.[11] In 2022, an estimated 10.6 million people developed active TB, resulting in 1.3 million deaths, making it the second leading cause of death from an infectious disease after COVID-19.[12] As of 2018, most TB cases occurred in the regions of South-East Asia (44%), Africa (24%), and the Western Pacific (18%), with more than 50% of cases being diagnosed in seven countries: India (27%), China (9%), Indonesia (8%), the Philippines (6%), Pakistan (6%), Nigeria (4%), and Bangladesh (4%).[13] By 2021, the number of new cases each year was decreasing by around 2% annually.[12][1] About 80% of people in many Asian and African countries test positive, while 5–10% of people in the United States test positive via the tuberculin test.[14] Tuberculosis has been present in humans since ancient times.[15]
History

Tuberculosis has existed since antiquity.[15] The oldest unambiguously detected M. tuberculosis gives evidence of the disease in the remains of bison in Wyoming dated to around 17,000 years ago.[16] However, whether tuberculosis originated in bovines, then transferred to humans, or whether both bovine and human tuberculosis diverged from a common ancestor, remains unclear.[17] A comparison of the genes of M. tuberculosis complex (MTBC) in humans to MTBC in animals suggests humans did not acquire MTBC from animals during animal domestication, as researchers previously believed. Both strains of the tuberculosis bacteria share a common ancestor, which could have infected humans even before the Neolithic Revolution.[18] Skeletal remains show some prehistoric humans (4000 BC) had TB, and researchers have found tubercular decay in the spines of Egyptian mummies dating from 3000 to 2400 BC.[19] Genetic studies suggest the presence of TB in the Americas from about AD 100.[20]
Before the Industrial Revolution, folklore often associated tuberculosis with vampires. When one member of a family died from the disease, the other infected members would lose their health slowly. People believed this was caused by the original person with TB draining the life from the other family members.[21]
Identification
Although Richard Morton established the pulmonary form associated with tubercles as a pathology in 1689,[22][23] due to the variety of its symptoms, TB was not identified as a single disease until the 1820s. Benjamin Marten conjectured in 1720 that consumptions were caused by microbes which were spread by people living close to each other.[24] In 1819, René Laennec claimed that tubercles were the cause of pulmonary tuberculosis.[25] J. L. Schönlein first published the name "tuberculosis" (German: Tuberkulose) in 1832.[26][27] Between 1838 and 1845, John Croghan, the owner of Mammoth Cave in Kentucky from 1839 onwards, brought a number of people with tuberculosis into the cave in the hope of curing the disease with the constant temperature and purity of the cave air; each died within a year.[28] Hermann Brehmer opened the first TB sanatorium in 1859 in Görbersdorf (now Sokołowsko) in Silesia.[29] In 1865, Jean Antoine Villemin demonstrated that tuberculosis could be transmitted, via inoculation, from humans to animals and among animals.[30] (Villemin's findings were confirmed in 1867 and 1868 by John Burdon-Sanderson.[31])

Robert Koch identified and described the bacillus causing tuberculosis, M. tuberculosis, on 24 March 1882.[32][33] In 1905, he was awarded the Nobel Prize in Physiology or Medicine for this discovery.[34]
Development of treatments
In Europe, rates of tuberculosis began to rise in the early 1600s to a peak level in the 1800s, when it caused nearly 25% of all deaths.[35] In the 18th and 19th century, tuberculosis had become epidemic in Europe, showing a seasonal pattern.[36][37] Tuberculosis caused widespread public concern in the 19th and early 20th centuries as the disease became common among the urban poor. In 1815, one in four deaths in England was due to "consumption". By 1918, TB still caused one in six deaths in France.[citation needed] After TB was determined to be contagious, in the 1880s, it was put on a notifiable-disease list in Britain; campaigns started to stop people from spitting in public places, and the infected poor were "encouraged" to enter sanatoria that resembled prisons (the sanatoria for the middle and upper classes offered excellent care and constant medical attention).[29] Whatever the benefits of the "fresh air" and labor in the sanatoria, even under the best conditions, 50% of those who entered died within five years (c. 1916).[29]
Robert Koch did not believe the cattle and human tuberculosis diseases were similar, which delayed the recognition of infected milk as a source of infection. During the first half of the 1900s, the risk of transmission from this source was dramatically reduced after the application of the pasteurization process. Koch announced a glycerine extract of the tubercle bacilli as a "remedy" for tuberculosis in 1890, calling it "tuberculin". Although it was not effective, it was later successfully adapted as a screening test for the presence of pre-symptomatic tuberculosis.[38] World Tuberculosis Day is marked on 24 March each year, the anniversary of Koch's original scientific announcement. When the Medical Research Council formed in Britain in 1913, it initially focused on tuberculosis research.[39]
Albert Calmette and Camille Guérin achieved the first genuine success in immunization against tuberculosis in 1906, using attenuated bovine-strain tuberculosis. It was called bacille Calmette–Guérin (BCG). The BCG vaccine was first used on humans in 1921 in France,[40] but achieved widespread acceptance in the US, Great Britain, and Germany only after World War II.[41]
By the 1950s mortality in Europe had decreased about 90%.[42] Improvements in sanitation, vaccination, and other public-health measures began significantly reducing rates of tuberculosis even before the arrival of streptomycin and other antibiotics, although the disease remained a significant threat.[42] In 1946, the development of the antibiotic streptomycin made effective treatment and cure of TB a reality. Prior to the introduction of this medication, the only treatment was surgical intervention, including the "pneumothorax technique", which involved collapsing an infected lung to "rest" it and to allow tuberculous lesions to heal.[43]
Current reemergence
Because of the emergence of multidrug-resistant tuberculosis (MDR-TB), surgery has been re-introduced for certain cases of TB infections. It involves the removal of infected chest cavities ("bullae") in the lungs to reduce the number of bacteria and to increase exposure of the remaining bacteria to antibiotics in the bloodstream.[44] Hopes of eliminating TB ended with the rise of drug-resistant strains in the 1980s. The subsequent resurgence of tuberculosis resulted in the declaration of a global health emergency by the World Health Organization (WHO) in 1993.[45]
Signs and symptoms

Tuberculosis may infect any part of the body, but most commonly occurs in the lungs (known as pulmonary tuberculosis).[8] Extrapulmonary TB occurs when tuberculosis develops outside of the lungs, although extrapulmonary TB may coexist with pulmonary TB.[8]
General signs and symptoms include fever, chills, night sweats, loss of appetite, weight loss, and fatigue.[8] Significant nail clubbing may also occur.[47]
Pulmonary
If a tuberculosis infection does become active, it most commonly involves the lungs (in about 90% of cases).[15][48] Symptoms may include chest pain and a prolonged cough producing sputum. About 25% of people may not have any symptoms (i.e., they remain asymptomatic).[15] Occasionally, people may cough up blood in small amounts, and in very rare cases, the infection may erode into the pulmonary artery or a Rasmussen's aneurysm, resulting in massive bleeding.[8][49] Tuberculosis may become a chronic illness and cause extensive scarring in the upper lobes of the lungs. The upper lung lobes are more frequently affected by tuberculosis than the lower ones.[8] The reason for this difference is not clear.[14] It may be due to either better air flow,[14] or poor lymph drainage within the upper lungs.[8]
Extrapulmonary
In 15–20% of active cases, the infection spreads outside the lungs, causing other kinds of TB.[50] These are collectively denoted as extrapulmonary tuberculosis.[51] Extrapulmonary TB occurs more commonly in people with a weakened immune system and young children. In those with HIV, this occurs in more than 50% of cases.[51] Notable extrapulmonary infection sites include the pleura (in tuberculous pleurisy), the central nervous system (in tuberculous meningitis), the lymphatic system (in scrofula of the neck), the genitourinary system (in urogenital tuberculosis), and the bones and joints (in Pott disease of the spine), among others. A potentially more serious, widespread form of TB is called "disseminated tuberculosis"; it is also known as miliary tuberculosis.[8] Miliary TB currently makes up about 10% of extrapulmonary cases.[52]
Causes
Mycobacteria

The main cause of TB is Mycobacterium tuberculosis (MTB), a small, aerobic, nonmotile bacillus.[8] The high lipid content of this pathogen accounts for many of its unique clinical characteristics.[53] It divides every 16 to 20 hours, which is an extremely slow rate compared with other bacteria, which usually divide in less than an hour.[54] Mycobacteria have an outer membrane lipid bilayer.[55] If a Gram stain is performed, MTB either stains very weakly "Gram-positive" or does not retain dye as a result of the high lipid and mycolic acid content of its cell wall.[56] MTB can withstand weak disinfectants and survive in a dry state for weeks. In nature, the bacterium can grow only within the cells of a host organism, but M. tuberculosis can be cultured in the laboratory.[57]
Using histological stains on expectorated samples from phlegm (also called sputum), scientists can identify MTB under a microscope. Since MTB retains certain stains even after being treated with acidic solution, it is classified as an acid-fast bacillus.[14][56] The most common acid-fast staining techniques are the Ziehl–Neelsen stain[58] and the Kinyoun stain, which dye acid-fast bacilli a bright red that stands out against a blue background.[59] Auramine-rhodamine staining[60] and fluorescence microscopy[61] are also used.
The M. tuberculosis complex (MTBC) includes four other TB-causing mycobacteria: M. bovis, M. africanum, M. canettii, and M. microti.[62] M. africanum is not widespread, but it is a significant cause of tuberculosis in parts of Africa.[63][64] M. bovis was once a common cause of tuberculosis, but the introduction of pasteurized milk has almost eliminated this as a public health problem in developed countries.[14][65] M. canettii is rare and seems to be limited to the Horn of Africa, although a few cases have been seen in African emigrants.[66][67] M. microti is also rare and is seen almost only in immunodeficient people, although its prevalence may be significantly underestimated.[68]
Other known pathogenic mycobacteria include M. leprae, M. avium, and M. kansasii. The latter two species are classified as "nontuberculous mycobacteria" (NTM) or atypical mycobacteria. NTM cause neither TB nor leprosy, but they do cause lung diseases that resemble TB.[69]

Transmission
When people with active pulmonary TB cough, sneeze, speak, sing, or spit, they expel infectious aerosol droplets 0.5 to 5.0 μm in diameter. A single sneeze can release up to 40,000 droplets.[70] Each one of these droplets may transmit the disease, since the infectious dose of tuberculosis is very small (the inhalation of fewer than 10 bacteria may cause an infection).[71]
Risk of transmission
People with prolonged, frequent, or close contact with people with TB are at particularly high risk of becoming infected, with an estimated 22% infection rate.[72] A person with active but untreated tuberculosis may infect 10–15 (or more) other people per year.[73] Transmission should occur from only people with active TB – those with latent infection are not thought to be contagious.[14] The probability of transmission from one person to another depends upon several factors, including the number of infectious droplets expelled by the carrier, the effectiveness of ventilation, the duration of exposure, the virulence of the M. tuberculosis strain, the level of immunity in the uninfected person, and others.[74] The cascade of person-to-person spread can be circumvented by segregating those with active ("overt") TB and putting them on anti-TB drug regimens. After about two weeks of effective treatment, subjects with nonresistant active infections generally do not remain contagious to others.[72] If someone does become infected, it typically takes three to four weeks before the newly infected person becomes infectious enough to transmit the disease to others.[75]
Risk factors
A number of factors make individuals more susceptible to TB infection and/or disease.[76]
Active disease risk
The most important risk factor globally for developing active TB is concurrent HIV infection; 13% of those with TB are also infected with HIV.[77] This is a particular problem in sub-Saharan Africa, where HIV infection rates are high.[78][79] Of those without HIV infection who are infected with tuberculosis, about 5–10% develop active disease during their lifetimes;[47] in contrast, 30% of those co-infected with HIV develop the active disease.[47]
Use of certain medications, such as corticosteroids and infliximab (an anti-αTNF monoclonal antibody), is another important risk factor, especially in the developed world.[15]
Other risk factors include: alcoholism,[15] diabetes mellitus (3-fold increased risk),[80] silicosis (30-fold increased risk),[81] tobacco smoking (2-fold increased risk),[82] indoor air pollution, malnutrition, young age,[76] recently acquired TB infection, recreational drug use, severe kidney disease, low body weight, organ transplant, head and neck cancer,[83] and genetic susceptibility[84] (the overall importance of genetic risk factors remains undefined[15]).
Infection susceptibility
Tobacco smoking increases the risk of infections (in addition to increasing the risk of active disease and death). Additional factors increasing infection susceptibility include young age.[76]
Pathogenesis

About 90% of those infected with M. tuberculosis have asymptomatic, latent TB infections (sometimes called LTBI),[86] with only a 10% lifetime chance that the latent infection will progress to overt, active tuberculous disease.[87] In those with HIV, the risk of developing active TB increases to nearly 10% a year.[87] If effective treatment is not given, the death rate for active TB cases is up to 66%.[73]
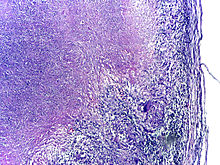
TB infection begins when the mycobacteria reach the alveolar air sacs of the lungs, where they invade and replicate within endosomes of alveolar macrophages.[14][88][89] Macrophages identify the bacterium as foreign and attempt to eliminate it by phagocytosis. During this process, the bacterium is enveloped by the macrophage and stored temporarily in a membrane-bound vesicle called a phagosome. The phagosome then combines with a lysosome to create a phagolysosome. In the phagolysosome, the cell attempts to use reactive oxygen species and acid to kill the bacterium. However, M. tuberculosis has a thick, waxy mycolic acid capsule that protects it from these toxic substances. M. tuberculosis is able to reproduce inside the macrophage and will eventually kill the immune cell.
The primary site of infection in the lungs, known as the Ghon focus, is generally located in either the upper part of the lower lobe, or the lower part of the upper lobe.[14] Tuberculosis of the lungs may also occur via infection from the blood stream. This is known as a Simon focus and is typically found in the top of the lung.[90] This hematogenous transmission can also spread infection to more distant sites, such as peripheral lymph nodes, the kidneys, the brain, and the bones.[14][91] All parts of the body can be affected by the disease, though for unknown reasons it rarely affects the heart, skeletal muscles, pancreas, or thyroid.[92]
Tuberculosis is classified as one of the granulomatous inflammatory diseases. Macrophages, epithelioid cells, T lymphocytes, B lymphocytes, and fibroblasts aggregate to form granulomas, with lymphocytes surrounding the infected macrophages. When other macrophages attack the infected macrophage, they fuse together to form a giant multinucleated cell in the alveolar lumen. The granuloma may prevent dissemination of the mycobacteria and provide a local environment for interaction of cells of the immune system.[93] However, more recent evidence suggests that the bacteria use the granulomas to avoid destruction by the host's immune system. Macrophages and dendritic cells in the granulomas are unable to present antigen to lymphocytes; thus the immune response is suppressed.[94] Bacteria inside the granuloma can become dormant, resulting in latent infection. Another feature of the granulomas is the development of abnormal cell death (necrosis) in the center of tubercles. To the naked eye, this has the texture of soft, white cheese and is termed caseous necrosis.[93]
If TB bacteria gain entry to the blood stream from an area of damaged tissue, they can spread throughout the body and set up many foci of infection, all appearing as tiny, white tubercles in the tissues.[95] This severe form of TB disease, most common in young children and those with HIV, is called miliary tuberculosis.[96] People with this disseminated TB have a high fatality rate even with treatment (about 30%).[52][97]
In many people, the infection waxes and wanes. Tissue destruction and necrosis are often balanced by healing and fibrosis.[93] Affected tissue is replaced by scarring and cavities filled with caseous necrotic material. During active disease, some of these cavities are joined to the air passages (bronchi) and this material can be coughed up. It contains living bacteria and thus can spread the infection. Treatment with appropriate antibiotics kills bacteria and allows healing to take place. Upon cure, affected areas are eventually replaced by scar tissue.[93]
Diagnosis

Active tuberculosis
Diagnosing active tuberculosis based only on signs and symptoms is difficult,[98] as is diagnosing the disease in those who have a weakened immune system.[99] A diagnosis of TB should, however, be considered in those with signs of lung disease or constitutional symptoms lasting longer than two weeks.[99] A chest X-ray and multiple sputum cultures for acid-fast bacilli are typically part of the initial evaluation.[99] Interferon-γ release assays (IGRA) and tuberculin skin tests are of little use in most of the developing world.[100][101] IGRA have similar limitations in those with HIV.[101][102]
A definitive diagnosis of TB is made by identifying M. tuberculosis in a clinical sample (e.g., sputum, pus, or a tissue biopsy). However, the difficult culture process for this slow-growing organism can take two to six weeks for blood or sputum culture.[103] Thus, treatment is often begun before cultures are confirmed.[104]
Nucleic acid amplification tests and adenosine deaminase testing may allow rapid diagnosis of TB.[98] Blood tests to detect antibodies are not specific or sensitive, so they are not recommended.[105]
Latent tuberculosis

The Mantoux tuberculin skin test is often used to screen people at high risk for TB.[99] Those who have been previously immunized with the Bacille Calmette-Guerin vaccine may have a false-positive test result.[106] The test may be falsely negative in those with sarcoidosis, Hodgkin's lymphoma, malnutrition, and most notably, active tuberculosis.[14] Interferon gamma release assays, on a blood sample, are recommended in those who are positive to the Mantoux test.[104] These are not affected by immunization or most environmental mycobacteria, so they generate fewer false-positive results.[107] However, they are affected by M. szulgai, M. marinum, and M. kansasii.[108] IGRAs may increase sensitivity when used in addition to the skin test, but may be less sensitive than the skin test when used alone.[109]
The US Preventive Services Task Force (USPSTF) has recommended screening people who are at high risk for latent tuberculosis with either tuberculin skin tests or interferon-gamma release assays.[110] While some have recommend testing health care workers, evidence of benefit for this is poor as of 2019[update].[111] The Centers for Disease Control and Prevention (CDC) stopped recommending yearly testing of health care workers without known exposure in 2019.[112]
Prevention

Tuberculosis prevention and control efforts rely primarily on the vaccination of infants and the detection and appropriate treatment of active cases.[15] The World Health Organization (WHO) has achieved some success with improved treatment regimens, and a small decrease in case numbers.[15] Some countries have legislation to involuntarily detain or examine those suspected to have tuberculosis, or involuntarily treat them if infected.[113]
Vaccines
The only available vaccine as of 2021[update] is bacillus Calmette-Guérin (BCG).[114][115] In children it decreases the risk of getting the infection by 20% and the risk of infection turning into active disease by nearly 60%.[116]
It is the most widely used vaccine worldwide, with more than 90% of all children being vaccinated.[15] The immunity it induces decreases after about ten years.[15] As tuberculosis is uncommon in most of Canada, Western Europe, and the United States, BCG is administered to only those people at high risk.[117][118][119] Part of the reasoning against the use of the vaccine is that it makes the tuberculin skin test falsely positive, reducing the test's usefulness as a screening tool.[119] Several vaccines are being developed.[15]
Intradermal MVA85A vaccine in addition to BCG injection is not effective in preventing tuberculosis.[120]
Public health
Public health campaigns which have focused on overcrowding, public spitting and regular sanitation (including hand washing) during the 1800s helped to either interrupt or slow spread which when combined with contact tracing, isolation and treatment helped to dramatically curb the transmission of both tuberculosis and other airborne diseases which led to the elimination of tuberculosis as a major public health issue in most developed economies.[121][122] Other risk factors which worsened TB spread such as malnutrition were also ameliorated, but since the emergence of HIV a new population of immunocompromised individuals was available for TB to infect.
The World Health Organization (WHO) declared TB a "global health emergency" in 1993,[15] and in 2006, the Stop TB Partnership developed a Global Plan to Stop Tuberculosis that aimed to save 14 million lives between its launch and 2015.[123] A number of targets they set were not achieved by 2015, mostly due to the increase in HIV-associated tuberculosis and the emergence of multiple drug-resistant tuberculosis.[15] A tuberculosis classification system developed by the American Thoracic Society is used primarily in public health programs.[124] In 2015, it launched the End TB Strategy to reduce deaths by 95% and incidence by 90% before 2035. The goal of tuberculosis elimination is being hampered by the lack of rapid testing, short and effective treatment courses, and completely effective vaccines.[125]
The benefits and risks of giving anti-tubercular drugs to those exposed to MDR-TB is unclear.[126] Making HAART therapy available to HIV-positive individuals significantly reduces the risk of progression to an active TB infection by up to 90% and can mitigate the spread through this population.[127]
Treatment

Treatment of TB uses antibiotics to kill the bacteria. Effective TB treatment is difficult, due to the unusual structure and chemical composition of the mycobacterial cell wall, which hinders the entry of drugs and makes many antibiotics ineffective.[128]
Active TB is best treated with combinations of several antibiotics to reduce the risk of the bacteria developing antibiotic resistance.[15] The routine use of rifabutin instead of rifampicin in HIV-positive people with tuberculosis is of unclear benefit as of 2007[update].[129]
Acetylsalicylic acid (aspirin) at a dose of 100 mg per day has been shown to improve clinical signs and symptoms, reduce cavitary lesions, lower inflammatory markers, and increase the rate of sputum-negative conversion in patients with pulmonary tuberculosis.[130]
Latent TB
Latent TB is treated with either isoniazid or rifampin alone, or a combination of isoniazid with either rifampicin or rifapentine.[131][132][133]
The treatment takes three to nine months depending on the medications used.[74][131][134][133] People with latent infections are treated to prevent them from progressing to active TB disease later in life.[135]
Education or counselling may improve the latent tuberculosis treatment completion rates.[136]
New onset
The recommended treatment of new-onset pulmonary tuberculosis, as of 2010[update], is six months of a combination of antibiotics containing rifampicin, isoniazid, pyrazinamide, and ethambutol for the first two months, and only rifampicin and isoniazid for the last four months.[15] Where resistance to isoniazid is high, ethambutol may be added for the last four months as an alternative.[15] Treatment with anti-TB drugs for at least 6 months results in higher success rates when compared with treatment less than 6 months, even though the difference is small. Shorter treatment regimen may be recommended for those with compliance issues.[137] There is also no evidence to support shorter anti-tuberculosis treatment regimens when compared to a 6-month treatment regimen.[138] However, results presented in 2020 from an international, randomized, controlled clinical trial indicate that a four-month daily treatment regimen containing high-dose, or "optimized", rifapentine with moxifloxacin (2PHZM/2PHM) is as safe and effective as the existing standard six-month daily regimen at curing drug-susceptible tuberculosis (TB) disease.[139]
Recurrent disease
If tuberculosis recurs, testing to determine which antibiotics it is sensitive to is important before determining treatment.[15] If multiple drug-resistant TB (MDR-TB) is detected, treatment with at least four effective antibiotics for 18 to 24 months is recommended.[15]
Medication administration
Directly observed therapy, i.e., having a health care provider watch the person take their medications, is recommended by the World Health Organization (WHO) in an effort to reduce the number of people not appropriately taking antibiotics.[140] The evidence to support this practice over people simply taking their medications independently is of poor quality.[141] There is no strong evidence indicating that directly observed therapy improves the number of people who were cured or the number of people who complete their medicine.[141] Moderate quality evidence suggests that there is also no difference if people are observed at home versus at a clinic, or by a family member versus a health care worker.[141] Methods to remind people of the importance of treatment and appointments may result in a small but important improvement.[142] There is also not enough evidence to support intermittent rifampicin-containing therapy given two to three times a week has equal effectiveness as daily dose regimen on improving cure rates and reducing relapsing rates.[143] There is also not enough evidence on effectiveness of giving intermittent twice or thrice weekly short course regimen compared to daily dosing regimen in treating children with tuberculosis.[144]
Medication resistance
Primary resistance occurs when a person becomes infected with a resistant strain of TB. A person with fully susceptible MTB may develop secondary (acquired) resistance during therapy because of inadequate treatment, not taking the prescribed regimen appropriately (lack of compliance), or using low-quality medication.[145] Drug-resistant TB is a serious public health issue in many developing countries, as its treatment is longer and requires more expensive drugs. MDR-TB is defined as resistance to the two most effective first-line TB drugs: rifampicin and isoniazid. Extensively drug-resistant TB is also resistant to three or more of the six classes of second-line drugs.[146] Totally drug-resistant TB is resistant to all currently used drugs.[147] It was first observed in 2003 in Italy,[148] but not widely reported until 2012,[147][149] and has also been found in Iran and India.[150] There is some efficacy for linezolid to treat those with XDR-TB but side effects and discontinuation of medications were common.[151][152] Bedaquiline is tentatively supported for use in multiple drug-resistant TB.[153]
XDR-TB is a term sometimes used to define extensively resistant TB, and constitutes one in ten cases of MDR-TB. Cases of XDR TB have been identified in more than 90% of countries.[150]
For those with known rifampicin or MDR-TB, molecular tests such as the Genotype MTBDRsl Assay (performed on culture isolates or smear positive specimens) may be useful to detect second-line anti-tubercular drug resistance.[154][155]
Prognosis

| no data ≤10 10–25 25–50 50–75 75–100 100–250 | 250–500 500–750 750–1000 1000–2000 2000–3000 ≥ 3000 |
Progression from TB infection to overt TB disease occurs when the bacilli overcome the immune system defenses and begin to multiply. In primary TB disease (some 1–5% of cases), this occurs soon after the initial infection.[14] However, in the majority of cases, a latent infection occurs with no obvious symptoms.[14] These dormant bacilli produce active tuberculosis in 5–10% of these latent cases, often many years after infection.[47]
The risk of reactivation increases with immunosuppression, such as that caused by infection with HIV. In people coinfected with M. tuberculosis and HIV, the risk of reactivation increases to 10% per year.[14] Studies using DNA fingerprinting of M. tuberculosis strains have shown reinfection contributes more substantially to recurrent TB than previously thought,[157] with estimates that it might account for more than 50% of reactivated cases in areas where TB is common.[158] The chance of death from a case of tuberculosis is about 4% as of 2008[update], down from 8% in 1995.[15]
In people with smear-positive pulmonary TB (without HIV co-infection), after 5 years without treatment, 50-60% die while 20-25% achieve spontaneous resolution (cure). TB is almost always fatal in those with untreated HIV co-infection and death rates are increased even with antiretroviral treatment of HIV.[159]
Epidemiology
Roughly one-quarter of the world's population has been infected with M. tuberculosis,[6] with new infections occurring in about 1% of the population each year.[11] However, most infections with M. tuberculosis do not cause disease,[160] and 90–95% of infections remain asymptomatic.[86] In 2012, an estimated 8.6 million chronic cases were active.[161] In 2010, 8.8 million new cases of tuberculosis were diagnosed, and 1.20–1.45 million deaths occurred (most of these occurring in developing countries).[77][162] Of these, about 0.35 million occur in those also infected with HIV.[163] In 2018, tuberculosis was the leading cause of death worldwide from a single infectious agent.[164] The total number of tuberculosis cases has been decreasing since 2005, while new cases have decreased since 2002.[77]
Tuberculosis[clarification needed] incidence is seasonal, with peaks occurring every spring and summer.[165][166][167][168] The reasons for this are unclear, but may be related to vitamin D deficiency during the winter.[168][169] There are also studies linking tuberculosis to different weather conditions like low temperature, low humidity and low rainfall. It has been suggested that tuberculosis incidence rates may be connected to climate change.[170]
At-risk groups
Tuberculosis is closely linked to both overcrowding and malnutrition, making it one of the principal diseases of poverty.[15] Those at high risk thus include: people who inject illicit drugs, inhabitants and employees of locales where vulnerable people gather (e.g., prisons and homeless shelters), medically underprivileged and resource-poor communities, high-risk ethnic minorities, children in close contact with high-risk category patients, and health-care providers serving these patients.[171]
The rate of tuberculosis varies with age. In Africa, it primarily affects adolescents and young adults.[172] However, in countries where incidence rates have declined dramatically (such as the United States), tuberculosis is mainly a disease of the elderly and immunocompromised (risk factors are listed above).[14][173] Worldwide, 22 "high-burden" states or countries together experience 80% of cases as well as 83% of deaths.[150]
In Canada and Australia, tuberculosis is many times more common among the Indigenous peoples, especially in remote areas.[174][175] Factors contributing to this include higher prevalence of predisposing health conditions and behaviours, and overcrowding and poverty. In some Canadian Indigenous groups, genetic susceptibility may play a role.[76]
Socioeconomic status (SES) strongly affects TB risk. People of low SES are both more likely to contract TB and to be more severely affected by the disease. Those with low SES are more likely to be affected by risk factors for developing TB (e.g., malnutrition, indoor air pollution, HIV co-infection, etc.), and are additionally more likely to be exposed to crowded and poorly ventilated spaces. Inadequate healthcare also means that people with active disease who facilitate spread are not diagnosed and treated promptly; sick people thus remain in the infectious state and (continue to) spread the infection.[76]
Geographical epidemiology
The distribution of tuberculosis is not uniform across the globe; about 80% of the population in many African, Caribbean, South Asian, and eastern European countries test positive in tuberculin tests, while only 5–10% of the U.S. population test positive.[14] Hopes of totally controlling the disease have been dramatically dampened because of many factors, including the difficulty of developing an effective vaccine, the expensive and time-consuming diagnostic process, the necessity of many months of treatment, the increase in HIV-associated tuberculosis, and the emergence of drug-resistant cases in the 1980s.[15]
In developed countries, tuberculosis is less common and is found mainly in urban areas. In Europe, deaths from TB fell from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. Improvements in public health were reducing tuberculosis even before the arrival of antibiotics, although the disease remained a significant threat to public health, such that when the Medical Research Council was formed in Britain in 1913 its initial focus was tuberculosis research.[176]
In 2010, rates per 100,000 people in different areas of the world were: globally 178, Africa 332, the Americas 36, Eastern Mediterranean 173, Europe 63, Southeast Asia 278, and Western Pacific 139.[163]
Russia
Russia has achieved particularly dramatic progress with a decline in its TB mortality rate—from 61.9 per 100,000 in 1965 to 2.7 per 100,000 in 1993;[177][178] however, mortality rate increased to 24 per 100,000 in 2005 and then recoiled to 11 per 100,000 by 2015.[179]
China
China has achieved particularly dramatic progress, with about an 80% reduction in its TB mortality rate between 1990 and 2010.[163] The number of new cases has declined by 17% between 2004 and 2014.[150]
Africa
In 2007, the country with the highest estimated incidence rate of TB was Eswatini, with 1,200 cases per 100,000 people. In 2017, the country with the highest estimated incidence rate as a % of the population was Lesotho, with 665 cases per 100,000 people.[180]
In South Africa, 54 200 people died in 2022 from TB. The incidence rate was 468 per 100 000 people; in 2015, this was 988 per 100 000. The total incidence was 280 000 in 2022; in 2015, this was 552 000.[181]
India
As of 2017, India had the largest total incidence, with an estimated 2,740,000 cases.[180] According to the World Health Organization (WHO), in 2000–2015, India's estimated mortality rate dropped from 55 to 36 per 100,000 population per year with estimated 480 thousand people died of TB in 2015.[182][183] In India a major proportion of tuberculosis patients are being treated by private partners and private hospitals. Evidence indicates that the tuberculosis national survey does not represent the number of cases that are diagnosed and recorded by private clinics and hospitals in India.[184]
North America
In the United States, Native Americans have a fivefold greater mortality from TB,[185] and racial and ethnic minorities accounted for 84% of all reported TB cases.[186] The overall tuberculosis case rate in the United States was 3 per 100,000 persons in 2017.[180]
In Canada, tuberculosis was endemic in some rural areas as of 1998.[187]
Western Europe
In 2017, in the United Kingdom, the national average was 9 per 100,000 and the highest incidence rates in Western Europe were 20 per 100,000 in Portugal.
-
Number of new cases of tuberculosis per 100,000 people in 2016[188]
-
Tuberculosis deaths per million persons in 2012
-
Tuberculosis deaths by region, 1990 to 2017[189]
Society and culture
Names
Tuberculosis has been known by many names from the technical to the familiar.[190] Phthisis (Φθισις) is a Greek word for consumption, an old term for pulmonary tuberculosis;[7] around 460 BCE, Hippocrates described phthisis as a disease of dry seasons.[191] The abbreviation TB is short for tubercle bacillus. Consumption was the most common nineteenth century English word for the disease, and was also in use well into the twentieth century. The Latin root con meaning 'completely' is linked to sumere meaning 'to take up from under'.[192] In The Life and Death of Mr Badman by John Bunyan, the author calls consumption "the captain of all these men of death."[193] "Great white plague" has also been used.[190]
Art and literature

Tuberculosis was for centuries associated with poetic and artistic qualities among those infected, and was also known as "the romantic disease".[190][194] Major artistic figures such as the poets John Keats, Percy Bysshe Shelley, and Edgar Allan Poe, the composer Frédéric Chopin,[195] the playwright Anton Chekhov, the novelists Franz Kafka, Katherine Mansfield,[196] Charlotte Brontë, Fyodor Dostoevsky, Thomas Mann, W. Somerset Maugham,[197] George Orwell,[198] and Robert Louis Stevenson, and the artists Alice Neel,[199] Jean-Antoine Watteau, Elizabeth Siddal, Marie Bashkirtseff, Edvard Munch, Aubrey Beardsley and Amedeo Modigliani either had the disease or were surrounded by people who did. A widespread belief was that tuberculosis assisted artistic talent. Physical mechanisms proposed for this effect included the slight fever and toxaemia that it caused, allegedly helping them to see life more clearly and to act decisively.[200][201][202]
Tuberculosis formed an often-reused theme in literature, as in Thomas Mann's The Magic Mountain, set in a sanatorium;[203] in music, as in Van Morrison's song "T.B. Sheets";[204] in opera, as in Puccini's La bohème and Verdi's La Traviata;[202] in art, as in Munch's painting of his ill sister;[205] and in film, such as the 1945 The Bells of St. Mary's starring Ingrid Bergman as a nun with tuberculosis.[206]
Public health efforts
In 2014, the WHO adopted the "End TB" strategy which aims to reduce TB incidence by 80% and TB deaths by 90% by 2030.[207] The strategy contains a milestone to reduce TB incidence by 20% and TB deaths by 35% by 2020.[208] However, by 2020 only a 9% reduction in incidence per population was achieved globally, with the European region achieving 19% and the African region achieving 16% reductions.[208] Similarly, the number of deaths only fell by 14%, missing the 2020 milestone of a 35% reduction, with some regions making better progress (31% reduction in Europe and 19% in Africa).[208] Correspondingly, also treatment, prevention and funding milestones were missed in 2020, for example only 6.3 million people were started on TB prevention short of the target of 30 million.[208]
The World Health Organization (WHO), the Bill and Melinda Gates Foundation, and the U.S. government are subsidizing a fast-acting diagnostic tuberculosis test for use in low- and middle-income countries as of 2012.[209][210][211] In addition to being fast-acting, the test can determine if there is resistance to the antibiotic rifampicin which may indicate multi-drug resistant tuberculosis and is accurate in those who are also infected with HIV.[209][212] Many resource-poor places as of 2011[update] have access to only sputum microscopy.[213]
India had the highest total number of TB cases worldwide in 2010, in part due to poor disease management within the private and public health care sector.[214] Programs such as the Revised National Tuberculosis Control Program are working to reduce TB levels among people receiving public health care.[215][216]
A 2014 EIU-healthcare report finds there is a need to address apathy and urges for increased funding. The report cites among others Lucica Ditui "[TB] is like an orphan. It has been neglected even in countries with a high burden and often forgotten by donors and those investing in health interventions."[150]
Slow progress has led to frustration, expressed by the executive director of the Global Fund to Fight AIDS, Tuberculosis and Malaria – Mark Dybul: "we have the tools to end TB as a pandemic and public health threat on the planet, but we are not doing it."[150] Several international organizations are pushing for more transparency in treatment, and more countries are implementing mandatory reporting of cases to the government as of 2014, although adherence is often variable. Commercial treatment providers may at times overprescribe second-line drugs as well as supplementary treatment, promoting demands for further regulations.[150] The government of Brazil provides universal TB care, which reduces this problem.[150] Conversely, falling rates of TB infection may not relate to the number of programs directed at reducing infection rates but may be tied to an increased level of education, income, and health of the population.[150] Costs of the disease, as calculated by the World Bank in 2009 may exceed US$150 billion per year in "high burden" countries.[150] Lack of progress eradicating the disease may also be due to lack of patient follow-up – as among the 250 million rural migrants in China.[150]
There is insufficient data to show that active contact tracing helps to improve case detection rates for tuberculosis.[217] Interventions such as house-to-house visits, educational leaflets, mass media strategies, educational sessions may increase tuberculosis detection rates in short-term.[218] There is no study that compares new methods of contact tracing such as social network analysis with existing contact tracing methods.[219]
Stigma
Slow progress in preventing the disease may in part be due to stigma associated with TB.[150] Stigma may be due to the fear of transmission from affected individuals. This stigma may additionally arise due to links between TB and poverty, and in Africa, AIDS.[150] Such stigmatization may be both real and perceived; for example, in Ghana, individuals with TB are banned from attending public gatherings.[220]
Stigma towards TB may result in delays in seeking treatment,[150] lower treatment compliance, and family members keeping cause of death secret[220] – allowing the disease to spread further.[150] In contrast, in Russia stigma was associated with increased treatment compliance.[220] TB stigma also affects socially marginalized individuals to a greater degree and varies between regions.[220]
One way to decrease stigma may be through the promotion of "TB clubs", where those infected may share experiences and offer support, or through counseling.[220] Some studies have shown TB education programs to be effective in decreasing stigma, and may thus be effective in increasing treatment adherence.[220] Despite this, studies on the relationship between reduced stigma and mortality are lacking as of 2010[update], and similar efforts to decrease stigma surrounding AIDS have been minimally effective.[220] Some have claimed the stigma to be worse than the disease, and healthcare providers may unintentionally reinforce stigma, as those with TB are often perceived as difficult or otherwise undesirable.[150] A greater understanding of the social and cultural dimensions of tuberculosis may also help with stigma reduction.[221]
Research
The BCG vaccine has limitations, and research to develop new TB vaccines is ongoing.[222] A number of potential candidates are currently in phase I and II clinical trials.[222][223] Two main approaches are used to attempt to improve the efficacy of available vaccines. One approach involves adding a subunit vaccine to BCG, while the other strategy is attempting to create new and better live vaccines.[222] MVA85A, an example of a subunit vaccine, is in trials in South Africa as of 2006, is based on a genetically modified vaccinia virus.[224] Vaccines are hoped to play a significant role in treatment of both latent and active disease.[225]
To encourage further discovery, researchers and policymakers are promoting new economic models of vaccine development as of 2006, including prizes, tax incentives, and advance market commitments.[226][227] A number of groups, including the Stop TB Partnership,[228] the South African Tuberculosis Vaccine Initiative, and the Aeras Global TB Vaccine Foundation, are involved with research.[229] Among these, the Aeras Global TB Vaccine Foundation received a gift of more than $280 million (US) from the Bill and Melinda Gates Foundation to develop and license an improved vaccine against tuberculosis for use in high burden countries.[230][231]
In 2012 a new medication regimen was approved in the US for multidrug-resistant tuberculosis, using bedaquiline as well as existing drugs. There were initial concerns about the safety of this drug,[232][233][234][235][236] but later research on larger groups found that this regimen improved health outcomes.[237] By 2017 the drug was used in at least 89 countries.[238] Another new drug is delamanid, which was first approved by the European Medicines Agency in 2013 to be used in multidrug-resistant tuberculosis patients,[239] and by 2017 was used in at least 54 countries.[240]
Steroids add-on therapy has not shown any benefits for active pulmonary tuberculosis infection.[241]
Other animals
Mycobacteria infect many different animals, including birds,[242] fish, rodents,[243] and reptiles.[244] The subspecies Mycobacterium tuberculosis, though, is rarely present in wild animals.[245] An effort to eradicate bovine tuberculosis caused by Mycobacterium bovis from the cattle and deer herds of New Zealand has been relatively successful.[246] Efforts in Great Britain have been less successful.[247][248]
As of 2015[update], tuberculosis appears to be widespread among captive elephants in the US. It is believed that the animals originally acquired the disease from humans, a process called reverse zoonosis. Because the disease can spread through the air to infect both humans and other animals, it is a public health concern affecting circuses and zoos.[249][250]
See also
Notes
References
- ^ a b c d e f g h i j k l m n o p "Tuberculosis (TB)". who.int. Archived from the original on 30 July 2020. Retrieved 8 May 2020.
- ^ Ferri FF (2010). Ferri's differential diagnosis : a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Philadelphia, PA: Elsevier/Mosby. p. Chapter T. ISBN 978-0-323-07699-9.
- ^ a b Hawn TR, Day TA, Scriba TJ, Hatherill M, Hanekom WA, Evans TG, et al. (December 2014). "Tuberculosis vaccines and prevention of infection". Microbiology and Molecular Biology Reviews. 78 (4): 650–71. doi:10.1128/MMBR.00021-14. PMC 4248657. PMID 25428938.
- ^ a b c Implementing the WHO Stop TB Strategy: a handbook for national TB control programmes. Geneva: World Health Organization (WHO). 2008. p. 179. ISBN 978-92-4-154667-6. Archived from the original on 2 June 2021. Retrieved 17 September 2017.
- ^ a b Harris RE (2013). "Epidemiology of Tuberculosis". Epidemiology of chronic disease: global perspectives. Burlington, MA: Jones & Bartlett Learning. p. 682. ISBN 978-0-7637-8047-0. Archived from the original on 7 February 2024. Retrieved 17 September 2017.
- ^ a b c d "Tuberculosis (TB)". World Health Organization (WHO). 16 February 2018. Archived from the original on 30 December 2013. Retrieved 15 September 2018.
- ^ a b The Chambers Dictionary. New Delhi: Allied Chambers India Ltd. 1998. p. 352. ISBN 978-81-86062-25-8. Archived from the original on 6 September 2015.
- ^ a b c d e f g h i Adkinson NF, Bennett JE, Douglas RG, Mandell GL (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases (7th ed.). Philadelphia, PA: Churchill Livingstone/Elsevier. p. Chapter 250. ISBN 978-0-443-06839-3.
- ^ "Basic TB Facts". Centers for Disease Control and Prevention (CDC). 13 March 2012. Archived from the original on 6 February 2016. Retrieved 11 February 2016.
- ^ a b Konstantinos A (2010). "Testing for tuberculosis". Australian Prescriber. 33 (1): 12–18. doi:10.18773/austprescr.2010.005.
- ^ a b "Tuberculosis". World Health Organization (WHO). 2002. Archived from the original on 17 June 2013.
- ^ a b "Tuberculosis (TB)". WHO. Archived from the original on 30 July 2020. Retrieved 16 October 2021.
- ^ "Global tuberculosis report". World Health Organization (WHO). Archived from the original on 30 December 2013. Retrieved 9 November 2017.
- ^ a b c d e f g h i j k l m n o Kumar V, Robbins SL (2007). Robbins Basic Pathology (8th ed.). Philadelphia: Elsevier. ISBN 978-1-4160-2973-1. OCLC 69672074.
- ^ a b c d e f g h i j k l m n o p q r s t u v Lawn SD, Zumla AI (July 2011). "Tuberculosis". Lancet. 378 (9785): 57–72. doi:10.1016/S0140-6736(10)62173-3. PMID 21420161. S2CID 208791546.
- ^ Rothschild BM, Martin LD, Lev G, Bercovier H, Bar-Gal GK, Greenblatt C, et al. (August 2001). "Mycobacterium tuberculosis complex DNA from an extinct bison dated 17,000 years before the present". Clinical Infectious Diseases. 33 (3): 305–11. doi:10.1086/321886. PMID 11438894.
- ^ Pearce-Duvet JM (August 2006). "The origin of human pathogens: evaluating the role of agriculture and domestic animals in the evolution of human disease". Biological Reviews of the Cambridge Philosophical Society. 81 (3): 369–82. doi:10.1017/S1464793106007020. PMID 16672105. S2CID 6577678.
- ^ Comas I, Gagneux S (October 2009). Manchester M (ed.). "The past and future of tuberculosis research". PLOS Pathogens. 5 (10): e1000600. doi:10.1371/journal.ppat.1000600. PMC 2745564. PMID 19855821.
- ^ Zink AR, Sola C, Reischl U, Grabner W, Rastogi N, Wolf H, et al. (January 2003). "Characterization of Mycobacterium tuberculosis complex DNAs from Egyptian mummies by spoligotyping". Journal of Clinical Microbiology. 41 (1): 359–67. doi:10.1128/JCM.41.1.359-367.2003. PMC 149558. PMID 12517873.
- ^ Konomi N, Lebwohl E, Mowbray K, Tattersall I, Zhang D (December 2002). "Detection of mycobacterial DNA in Andean mummies". Journal of Clinical Microbiology. 40 (12): 4738–40. doi:10.1128/JCM.40.12.4738-4740.2002. PMC 154635. PMID 12454182.
- ^ Sledzik PS, Bellantoni N (June 1994). "Brief communication: bioarcheological and biocultural evidence for the New England vampire folk belief" (PDF). American Journal of Physical Anthropology. 94 (2): 269–74. doi:10.1002/ajpa.1330940210. PMID 8085617. Archived (PDF) from the original on 18 February 2017.
- ^ Léon Charles Albert Calmette at Who Named It?
- ^ Trail RR (April 1970). "Richard Morton (1637-1698)". Medical History. 14 (2): 166–74. doi:10.1017/S0025727300015350. PMC 1034037. PMID 4914685.
- ^ Marten B (1720). A New Theory of Consumptions—More Especially a Phthisis or Consumption of the Lungs. London, England: T. Knaplock. Archived from the original on 26 March 2023. Retrieved 8 December 2020. P. 51: "The Original and Essential Cause ... may possibly be some certain Species of Animalcula or wonderfully minute living Creatures, ... " P. 79: "It may be therefore very likely, that by an habitual lying in the same Bed with a Consumptive Patient, constantly Eating and Drinking with him, or by very frequently conversing so nearly, as to draw in part of the Breath he emits from his Lungs, a Consumption may be caught by a sound Person; ... "
- ^ Laennec RT (1819). De l'auscultation médiate ... (in French). Vol. 1. Paris, France: J.-A. Brosson et J.-S Chaudé. p. 20. Archived from the original on 2 June 2021. Retrieved 6 December 2020. From p. 20: "L'existence des tubercules dans le poumon est la cause et constitue le charactère anatomique propre de la phthisie pulmonaire (a). (a) ... l'effet dont cette maladie tire son nom, c'est-à-dire, la consumption." (The existence of tubercles in the lung is the cause and constitutes the unique anatomical characteristic of pulmonary tuberculosis (a). (a) ... the effect from which this malady [pulmonary tuberculosis] takes its name, that is, consumption.)
- ^ Schönlein JL (1832). Allgemeine und specielle Pathologie und Therapie [General and Special Pathology and Therapy] (in German). Vol. 3. Würzburg, (Germany): C. Etlinger. p. 103. Archived from the original on 2 June 2021. Retrieved 6 December 2020.
- ^ The word "tuberculosis" first appeared in Schönlein's clinical notes in 1829. See: Jay SJ, Kırbıyık U, Woods JR, Steele GA, Hoyt GR, Schwengber RB, et al. (November 2018). "Modern theory of tuberculosis: culturomic analysis of its historical origin in Europe and North America". The International Journal of Tuberculosis and Lung Disease. 22 (11): 1249–1257. doi:10.5588/ijtld.18.0239. PMID 30355403. S2CID 53027676. See especially Appendix, p. iii.
- ^ "Kentucky: Mammoth Cave long on history". CNN. 27 February 2004. Archived from the original on 13 August 2006. Retrieved 8 October 2006.
- ^ a b c McCarthy OR (August 2001). "The key to the sanatoria". Journal of the Royal Society of Medicine. 94 (8): 413–17. doi:10.1177/014107680109400813. PMC 1281640. PMID 11461990. Archived from the original on 3 August 2012. Retrieved 28 September 2011.
- ^ Villemin JA (1865). "Cause et nature de la tuberculose" [Cause and nature of tuberculosis]. Bulletin de l'Académie Impériale de Médecine (in French). 31: 211–216. Archived from the original on 9 December 2021. Retrieved 6 December 2020.
- See also: Villemin JA (1868). Etudes sur la tuberculose: preuves rationnelles et expérimentales de sa spécificité et de son inoculabilité [Studies of tuberculosis: rational and experimental evidence of its specificity and inoculability] (in French). Paris, France: J.-B. Baillière et fils. Archived from the original on 7 February 2024. Retrieved 6 December 2020.
- ^ Burdon-Sanderson, John Scott. (1870) "Introductory Report on the Intimate Pathology of Contagion." Appendix to: Twelfth Report to the Lords of Her Majesty's Most Honourable Privy Council of the Medical Officer of the Privy Council [for the year 1869], Parliamentary Papers (1870), vol. 38, 229–256.
- ^ Koch R (24 March 1882). "Die Ätiologie der Tuberkulose (1882)". Robert Koch: Zentrale Texte [The Etiology of Tuberculosis]. Klassische Texte der Wissenschaft. Vol. 19. Berlin, Heidelberg: Springer Spektrum. pp. 221–30. doi:10.1007/978-3-662-56454-7_4. ISBN 978-3-662-56454-7. Archived from the original on 6 November 2018. Retrieved 15 June 2021.
- ^ "History: World TB Day". Centers for Disease Control and Prevention (CDC). 12 December 2016. Archived from the original on 7 December 2018. Retrieved 23 March 2019.
- ^ "The Nobel Prize in Physiology or Medicine 1905". www.nobelprize.org. Archived from the original on 10 December 2006. Retrieved 7 October 2006.
- ^ Bloom BR (1994). Tuberculosis: pathogenesis, protection, and control. Washington, DC: ASM Press. ISBN 978-1-55581-072-6.
- ^ Frith J. "History of Tuberculosis. Part 1 – Phthisis, consumption and the White Plague". Journal of Military and Veterans' Health. Archived from the original on 8 April 2021. Retrieved 26 February 2021.
- ^ Zürcher K, Zwahlen M, Ballif M, Rieder HL, Egger M, Fenner L (5 October 2016). "Influenza Pandemics and Tuberculosis Mortality in 1889 and 1918: Analysis of Historical Data from Switzerland". PLOS ONE. 11 (10): e0162575. Bibcode:2016PLoSO..1162575Z. doi:10.1371/journal.pone.0162575. PMC 5051959. PMID 27706149.
- ^ Waddington K (January 2004). "To stamp out 'so terrible a malady': bovine tuberculosis and tuberculin testing in Britain, 1890–1939". Medical History. 48 (1): 29–48. doi:10.1017/S0025727300007043. PMC 546294. PMID 14968644.
- ^ Hannaway C (2008). Biomedicine in the twentieth century: practices, policies, and politics. Amsterdam: IOS Press. p. 233. ISBN 978-1-58603-832-8. Archived from the original on 7 September 2015.
- ^ Bonah C (December 2005). "The 'experimental stable' of the BCG vaccine: safety, efficacy, proof, and standards, 1921–1933". Studies in History and Philosophy of Biological and Biomedical Sciences. 36 (4): 696–721. doi:10.1016/j.shpsc.2005.09.003. PMID 16337557.
- ^ Comstock GW (September 1994). "The International Tuberculosis Campaign: a pioneering venture in mass vaccination and research". Clinical Infectious Diseases. 19 (3): 528–40. doi:10.1093/clinids/19.3.528. PMID 7811874.
- ^ a b Persson S (2010). Smallpox, Syphilis and Salvation: Medical Breakthroughs That Changed the World. ReadHowYouWant.com. p. 141. ISBN 978-1-4587-6712-7. Archived from the original on 6 September 2015.
- ^ Shields T (2009). General thoracic surgery (7th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 792. ISBN 978-0-7817-7982-1. Archived from the original on 6 September 2015.
- ^ Lalloo UG, Naidoo R, Ambaram A (May 2006). "Recent advances in the medical and surgical treatment of multi-drug resistant tuberculosis". Current Opinion in Pulmonary Medicine. 12 (3): 179–85. doi:10.1097/01.mcp.0000219266.27439.52. PMID 16582672. S2CID 24221563.
- ^ "Frequently asked questions about TB and HIV". World Health Organization (WHO). Archived from the original on 8 August 2011. Retrieved 15 April 2012.
- ^ Schiffman G (15 January 2009). "Tuberculosis Symptoms". eMedicine Health. Archived from the original on 16 May 2009.
- ^ a b c d Gibson PG, Abramson M, Wood-Baker R, Volmink J, Hensley M, Costabel U, eds. (2005). Evidence-Based Respiratory Medicine (1st ed.). BMJ Books. p. 321. ISBN 978-0-7279-1605-1. Archived from the original on 8 December 2015.
- ^ Behera D (2010). Textbook of Pulmonary Medicine (2nd ed.). New Delhi: Jaypee Brothers Medical Publishers. p. 457. ISBN 978-81-8448-749-7. Archived from the original on 6 September 2015.
- ^ Halezeroğlu S, Okur E (March 2014). "Thoracic surgery for haemoptysis in the context of tuberculosis: what is the best management approach?". Journal of Thoracic Disease. 6 (3): 182–85. doi:10.3978/j.issn.2072-1439.2013.12.25. PMC 3949181. PMID 24624281.
- ^ Jindal SK, ed. (2011). Textbook of Pulmonary and Critical Care Medicine. New Delhi: Jaypee Brothers Medical Publishers. p. 549. ISBN 978-93-5025-073-0. Archived from the original on 7 September 2015.
- ^ a b Golden MP, Vikram HR (November 2005). "Extrapulmonary tuberculosis: an overview". American Family Physician. 72 (9): 1761–68. PMID 16300038.
- ^ a b Habermann TM, Ghosh A (2008). Mayo Clinic internal medicine: concise textbook. Rochester, MN: Mayo Clinic Scientific Press. p. 789. ISBN 978-1-4200-6749-1. Archived from the original on 6 September 2015.
- ^ Southwick F (2007). "Chapter 4: Pulmonary Infections". Infectious Diseases: A Clinical Short Course, 2nd ed. McGraw-Hill Medical Publishing Division. pp. 104, 313–14. ISBN 978-0-07-147722-2.
- ^ Jindal SK (2011). Textbook of Pulmonary and Critical Care Medicine. New Delhi: Jaypee Brothers Medical Publishers. p. 525. ISBN 978-93-5025-073-0. Archived from the original on 6 September 2015.
- ^ Niederweis M, Danilchanka O, Huff J, Hoffmann C, Engelhardt H (March 2010). "Mycobacterial outer membranes: in search of proteins". Trends in Microbiology. 18 (3): 109–16. doi:10.1016/j.tim.2009.12.005. PMC 2931330. PMID 20060722.
- ^ a b Madison BM (May 2001). "Application of stains in clinical microbiology". Biotechnic & Histochemistry. 76 (3): 119–25. doi:10.1080/714028138. PMID 11475314.
- ^ Parish T, Stoker NG (December 1999). "Mycobacteria: bugs and bugbears (two steps forward and one step back)". Molecular Biotechnology. 13 (3): 191–200. doi:10.1385/MB:13:3:191. PMID 10934532. S2CID 28960959.
- ^ Medical Laboratory Science: Theory and Practice. New Delhi: Tata McGraw-Hill. 2000. p. 473. ISBN 978-0-07-463223-9. Archived from the original on 6 September 2015.
- ^ "Acid-Fast Stain Protocols". 21 August 2013. Archived from the original on 1 October 2011. Retrieved 26 March 2016.
- ^ Kommareddi S, Abramowsky CR, Swinehart GL, Hrabak L (November 1984). "Nontuberculous mycobacterial infections: comparison of the fluorescent auramine-O and Ziehl-Neelsen techniques in tissue diagnosis". Human Pathology. 15 (11): 1085–9. doi:10.1016/S0046-8177(84)80253-1. PMID 6208117.
- ^ van Lettow M, Whalen C (2008). Semba RD, Bloem MW (eds.). Nutrition and health in developing countries (2nd ed.). Totowa, N.J.: Humana Press. p. 291. ISBN 978-1-934115-24-4. Archived from the original on 6 September 2015.
- ^ van Soolingen D, Hoogenboezem T, de Haas PE, Hermans PW, Koedam MA, Teppema KS, et al. (October 1997). "A novel pathogenic taxon of the Mycobacterium tuberculosis complex, Canetti: characterization of an exceptional isolate from Africa". International Journal of Systematic Bacteriology. 47 (4): 1236–45. doi:10.1099/00207713-47-4-1236. PMID 9336935.
- ^ Niemann S, Rüsch-Gerdes S, Joloba ML, Whalen CC, Guwatudde D, Ellner JJ, et al. (September 2002). "Mycobacterium africanum subtype II is associated with two distinct genotypes and is a major cause of human tuberculosis in Kampala, Uganda". Journal of Clinical Microbiology. 40 (9): 3398–405. doi:10.1128/JCM.40.9.3398-3405.2002. PMC 130701. PMID 12202584.
- ^ Niobe-Eyangoh SN, Kuaban C, Sorlin P, Cunin P, Thonnon J, Sola C, et al. (June 2003). "Genetic biodiversity of Mycobacterium tuberculosis complex strains from patients with pulmonary tuberculosis in Cameroon". Journal of Clinical Microbiology. 41 (6): 2547–53. doi:10.1128/JCM.41.6.2547-2553.2003. PMC 156567. PMID 12791879.
- ^ Thoen C, Lobue P, de Kantor I (February 2006). "The importance of Mycobacterium bovis as a zoonosis". Veterinary Microbiology. 112 (2–4): 339–45. doi:10.1016/j.vetmic.2005.11.047. PMID 16387455.
- ^ Acton QA (2011). Mycobacterium Infections: New Insights for the Healthcare Professional. ScholarlyEditions. p. 1968. ISBN 978-1-4649-0122-5. Archived from the original on 6 September 2015.
- ^ Pfyffer GE, Auckenthaler R, van Embden JD, van Soolingen D (1998). "Mycobacterium canettii, the smooth variant of M. tuberculosis, isolated from a Swiss patient exposed in Africa". Emerging Infectious Diseases. 4 (4): 631–4. doi:10.3201/eid0404.980414. PMC 2640258. PMID 9866740.
- ^ Panteix G, Gutierrez MC, Boschiroli ML, Rouviere M, Plaidy A, Pressac D, et al. (August 2010). "Pulmonary tuberculosis due to Mycobacterium microti: a study of six recent cases in France". Journal of Medical Microbiology. 59 (Pt 8): 984–989. doi:10.1099/jmm.0.019372-0. PMID 20488936.
- ^ American Thoracic Society (August 1997). "Diagnosis and treatment of disease caused by nontuberculous mycobacteria". American Journal of Respiratory and Critical Care Medicine. 156 (2 Pt 2): S1–25. doi:10.1164/ajrccm.156.2.atsstatement. PMID 9279284.
- ^ Cole EC, Cook CE (August 1998). "Characterization of infectious aerosols in health care facilities: an aid to effective engineering controls and preventive strategies". American Journal of Infection Control. 26 (4): 453–64. doi:10.1016/S0196-6553(98)70046-X. PMC 7132666. PMID 9721404.
- ^ Nicas M, Nazaroff WW, Hubbard A (March 2005). "Toward understanding the risk of secondary airborne infection: emission of respirable pathogens". Journal of Occupational and Environmental Hygiene. 2 (3): 143–54. doi:10.1080/15459620590918466. PMC 7196697. PMID 15764538.
- ^ a b Ahmed N, Hasnain SE (September 2011). "Molecular epidemiology of tuberculosis in India: moving forward with a systems biology approach". Tuberculosis. 91 (5): 407–13. doi:10.1016/j.tube.2011.03.006. PMID 21514230.
- ^ a b "Tuberculosis Fact sheet N°104". World Health Organization (WHO). November 2010. Archived from the original on 4 October 2006. Retrieved 26 July 2011.
- ^ a b "Core Curriculum on Tuberculosis: What the Clinician Should Know" (PDF) (5th ed.). Centers for Disease Control and Prevention (CDC), Division of Tuberculosis Elimination. 2011. p. 24. Archived (PDF) from the original on 19 May 2012.
- ^ "Causes of Tuberculosis". Mayo Clinic. 21 December 2006. Archived from the original on 18 October 2007. Retrieved 19 October 2007.
- ^ a b c d e Narasimhan P, Wood J, Macintyre CR, Mathai D (2013). "Risk factors for tuberculosis". Pulmonary Medicine. 2013: 828939. doi:10.1155/2013/828939. PMC 3583136. PMID 23476764.
- ^ a b c "The sixteenth global report on tuberculosis" (PDF). World Health Organization (WHO). 2011. Archived from the original (PDF) on 6 September 2012.
- ^ "Global tuberculosis control–surveillance, planning, financing WHO Report 2006". World Health Organization (WHO). Archived from the original on 12 December 2006. Retrieved 13 October 2006.
- ^ Chaisson RE, Martinson NA (March 2008). "Tuberculosis in Africa – combating an HIV-driven crisis". The New England Journal of Medicine. 358 (11): 1089–92. doi:10.1056/NEJMp0800809. PMID 18337598.
- ^ Restrepo BI (August 2007). "Convergence of the tuberculosis and diabetes epidemics: renewal of old acquaintances". Clinical Infectious Diseases. 45 (4): 436–438. doi:10.1086/519939. PMC 2900315. PMID 17638190.
- ^ "Targeted tuberculin testing and treatment of latent tuberculosis infection. American Thoracic Society". MMWR. Recommendations and Reports. 49 (RR-6): 1–51. June 2000. PMID 10881762. Archived from the original on 17 December 2004.
- ^ van Zyl Smit RN, Pai M, Yew WW, Leung CC, Zumla A, Bateman ED, et al. (January 2010). "Global lung health: the colliding epidemics of tuberculosis, tobacco smoking, HIV and COPD". The European Respiratory Journal. 35 (1): 27–33. doi:10.1183/09031936.00072909. PMC 5454527. PMID 20044459.
These analyses indicate that smokers are almost twice as likely to be infected with TB and to progress to active disease (RR of about 1.5 for latent TB infection (LTBI) and RR of ~2.0 for TB disease). Smokers are also twice as likely to die from TB (RR of about 2.0 for TB mortality), but data are difficult to interpret because of heterogeneity in the results across studies.
- ^ "TB Risk Factors". CDC. 18 March 2016. Archived from the original on 30 August 2020. Retrieved 25 August 2020.
- ^ Möller M, Hoal EG (March 2010). "Current findings, challenges and novel approaches in human genetic susceptibility to tuberculosis". Tuberculosis. 90 (2): 71–83. doi:10.1016/j.tube.2010.02.002. PMID 20206579.
- ^ Good JM, Cooper S, Doane AS (1835). The Study of Medicine. Harper. p. 32. Archived from the original on 10 August 2016.
- ^ a b Skolnik R (2011). Global health 101 (2nd ed.). Burlington, MA: Jones & Bartlett Learning. p. 253. ISBN 978-0-7637-9751-5.
- ^ a b Mainous III AR, Pomeroy C (2009). Management of antimicrobials in infectious diseases: impact of antibiotic resistance (2nd rev. ed.). Totowa, NJ: Humana Press. p. 74. ISBN 978-1-60327-238-4. Archived from the original on 6 September 2015.
- ^ Houben EN, Nguyen L, Pieters J (February 2006). "Interaction of pathogenic mycobacteria with the host immune system". Current Opinion in Microbiology. 9 (1): 76–85. doi:10.1016/j.mib.2005.12.014. PMID 16406837.
- ^ Queval CJ, Brosch R, Simeone R (2017). "Mycobacterium tuberculosis". Frontiers in Microbiology. 8: 2284. doi:10.3389/fmicb.2017.02284. PMC 5703847. PMID 29218036.
- ^ Khan MR (2011). Essence of Paediatrics. Elsevier India. p. 401. ISBN 978-81-312-2804-3. Archived from the original on 6 September 2015.
- ^ Herrmann JL, Lagrange PH (February 2005). "Dendritic cells and Mycobacterium tuberculosis: which is the Trojan horse?". Pathologie-Biologie. 53 (1): 35–40. doi:10.1016/j.patbio.2004.01.004. PMID 15620608.
- ^ Agarwal R, Malhotra P, Awasthi A, Kakkar N, Gupta D (April 2005). "Tuberculous dilated cardiomyopathy: an under-recognized entity?". BMC Infectious Diseases. 5 (1): 29. doi:10.1186/1471-2334-5-29. PMC 1090580. PMID 15857515.
- ^ a b c d Grosset J (March 2003). "Mycobacterium tuberculosis in the extracellular compartment: an underestimated adversary". Antimicrobial Agents and Chemotherapy. 47 (3): 833–36. doi:10.1128/AAC.47.3.833-836.2003. PMC 149338. PMID 12604509.
- ^ Bozzano F, Marras F, De Maria A (2014). "Immunology of tuberculosis". Mediterranean Journal of Hematology and Infectious Diseases. 6 (1): e2014027. doi:10.4084/MJHID.2014.027. PMC 4010607. PMID 24804000.
- ^ Crowley LV (2010). An introduction to human disease: pathology and pathophysiology correlations (8th ed.). Sudbury, MA: Jones and Bartlett. p. 374. ISBN 978-0-7637-6591-0. Archived from the original on 6 September 2015.
- ^ Harries AD, Maher D, Graham S (2005). TB/HIV a Clinical Manual (2nd ed.). Geneva: World Health Organization (WHO). p. 75. ISBN 978-92-4-154634-8. Archived from the original on 6 September 2015.
- ^ Jacob JT, Mehta AK, Leonard MK (January 2009). "Acute forms of tuberculosis in adults". The American Journal of Medicine. 122 (1): 12–17. doi:10.1016/j.amjmed.2008.09.018. PMID 19114163.
- ^ a b Bento J, Silva AS, Rodrigues F, Duarte R (2011). "[Diagnostic tools in tuberculosis]". Acta Médica Portuguesa. 24 (1): 145–54. doi:10.20344/amp.333. PMID 21672452. S2CID 76156550.
- ^ a b c d Escalante P (June 2009). "In the clinic. Tuberculosis". Annals of Internal Medicine. 150 (11): ITC61-614, quiz ITV616. doi:10.7326/0003-4819-150-11-200906020-01006. PMID 19487708. S2CID 639982.
- ^ Metcalfe JZ, Everett CK, Steingart KR, Cattamanchi A, Huang L, Hopewell PC, et al. (November 2011). "Interferon-γ release assays for active pulmonary tuberculosis diagnosis in adults in low- and middle-income countries: systematic review and meta-analysis". The Journal of Infectious Diseases. 204 (suppl_4): S1120-9. doi:10.1093/infdis/jir410. PMC 3192542. PMID 21996694.
- ^ a b Sester M, Sotgiu G, Lange C, Giehl C, Girardi E, Migliori GB, et al. (January 2011). "Interferon-γ release assays for the diagnosis of active tuberculosis: a systematic review and meta-analysis". The European Respiratory Journal. 37 (1): 100–11. doi:10.1183/09031936.00114810. PMID 20847080.
- ^ Chen J, Zhang R, Wang J, Liu L, Zheng Y, Shen Y, et al. (2011). Vermund SH (ed.). "Interferon-gamma release assays for the diagnosis of active tuberculosis in HIV-infected patients: a systematic review and meta-analysis". PLOS ONE. 6 (11): e26827. Bibcode:2011PLoSO...626827C. doi:10.1371/journal.pone.0026827. PMC 3206065. PMID 22069472.
- ^ Special Programme for Research & Training in Tropical Diseases (2006). Diagnostics for tuberculosis: global demand and market potential. Geneva: World Health Organization (WHO). p. 36. ISBN 978-92-4-156330-7. Archived from the original on 6 September 2015.
- ^ a b National Institute for Health and Clinical Excellence. Clinical guideline 117: Tuberculosis. London, 2011.
- ^ Steingart KR, Flores LL, Dendukuri N, Schiller I, Laal S, Ramsay A, et al. (August 2011). Evans C (ed.). "Commercial serological tests for the diagnosis of active pulmonary and extrapulmonary tuberculosis: an updated systematic review and meta-analysis". PLOS Medicine. 8 (8): e1001062. doi:10.1371/journal.pmed.1001062. PMC 3153457. PMID 21857806.
- ^ Rothel JS, Andersen P (December 2005). "Diagnosis of latent Mycobacterium tuberculosis infection: is the demise of the Mantoux test imminent?". Expert Review of Anti-Infective Therapy. 3 (6): 981–93. doi:10.1586/14787210.3.6.981. PMID 16307510. S2CID 25423684.
- ^ Pai M, Zwerling A, Menzies D (August 2008). "Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update". Annals of Internal Medicine. 149 (3): 177–84. doi:10.7326/0003-4819-149-3-200808050-00241. PMC 2951987. PMID 18593687.
- ^ Jindal SK, ed. (2011). Textbook of Pulmonary and Critical Care Medicine. New Delhi: Jaypee Brothers Medical Publishers. p. 544. ISBN 978-93-5025-073-0. Archived from the original on 6 September 2015.
- ^ Amicosante M, Ciccozzi M, Markova R (April 2010). "Rational use of immunodiagnostic tools for tuberculosis infection: guidelines and cost effectiveness studies". The New Microbiologica. 33 (2): 93–107. PMID 20518271.
- ^ Bibbins-Domingo K, Grossman DC, Curry SJ, Bauman L, Davidson KW, Epling JW, et al. (September 2016). "Screening for Latent Tuberculosis Infection in Adults: US Preventive Services Task Force Recommendation Statement". JAMA. 316 (9): 962–9. doi:10.1001/jama.2016.11046. PMID 27599331.
- ^ Gill J, Prasad V (November 2019). "Testing Healthcare Workers for Latent Tuberculosis: Is It Evidence Based, Bio-Plausible, Both, Or Neither?". The American Journal of Medicine. 132 (11): 1260–1261. doi:10.1016/j.amjmed.2019.03.017. PMID 30946831.
- ^ Sosa LE, Njie GJ, Lobato MN, Bamrah Morris S, Buchta W, Casey ML, et al. (May 2019). "Tuberculosis Screening, Testing, and Treatment of U.S. Health Care Personnel: Recommendations from the National Tuberculosis Controllers Association and CDC, 2019". MMWR. Morbidity and Mortality Weekly Report. 68 (19): 439–443. doi:10.15585/mmwr.mm6819a3. PMC 6522077. PMID 31099768.
- ^ Coker R, Thomas M, Lock K, Martin R (2007). "Detention and the evolving threat of tuberculosis: evidence, ethics, and law". The Journal of Law, Medicine & Ethics. 35 (4): 609–15, 512. doi:10.1111/j.1748-720X.2007.00184.x. PMID 18076512. S2CID 19924571.
- ^ McShane H (October 2011). "Tuberculosis vaccines: beyond bacille Calmette-Guerin". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 366 (1579): 2782–89. doi:10.1098/rstb.2011.0097. PMC 3146779. PMID 21893541.
- ^ "Vaccines | Basic TB Facts". CDC. 16 June 2021. Archived from the original on 30 December 2021. Retrieved 30 December 2021.
- ^ Roy A, Eisenhut M, Harris RJ, Rodrigues LC, Sridhar S, Habermann S, et al. (August 2014). "Effect of BCG vaccination against Mycobacterium tuberculosis infection in children: systematic review and meta-analysis". BMJ. 349: g4643. doi:10.1136/bmj.g4643. PMC 4122754. PMID 25097193.
- ^ "Vaccine and Immunizations: TB Vaccine (BCG)". Centers for Disease Control and Prevention. 2011. Archived from the original on 17 November 2011. Retrieved 26 July 2011.
- ^ "BCG Vaccine Usage in Canada – Current and Historical". Public Health Agency of Canada. September 2010. Archived from the original on 30 March 2012. Retrieved 30 December 2011.
- ^ a b Teo SS, Shingadia DV (June 2006). "Does BCG have a role in tuberculosis control and prevention in the United Kingdom?". Archives of Disease in Childhood. 91 (6): 529–31. doi:10.1136/adc.2005.085043. PMC 2082765. PMID 16714729.
- ^ Kashangura R, Jullien S, Garner P, Johnson S, et al. (Cochrane Infectious Diseases Group) (April 2019). "MVA85A vaccine to enhance BCG for preventing tuberculosis". The Cochrane Database of Systematic Reviews. 2019 (4): CD012915. doi:10.1002/14651858.CD012915.pub2. PMC 6488980. PMID 31038197.
- ^ Clark M, Riben P, Nowgesic E (October 2002). "The association of housing density, isolation and tuberculosis in Canadian First Nations communities". International Journal of Epidemiology. 31 (5): 940–945. doi:10.1093/ije/31.5.940. PMID 12435764.
- ^ Barberis I, Bragazzi NL, Galluzzo L, Martini M (March 2017). "The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus". Journal of Preventive Medicine and Hygiene. 58 (1): E9–E12. PMC 5432783. PMID 28515626.
- ^ "The Global Plan to Stop TB". World Health Organization (WHO). 2011. Archived from the original on 12 June 2011. Retrieved 13 June 2011.
- ^ Warrell DA, Cox TM, Firth JD, Benz EJ (2005). Sections 1–10 (4. ed., paperback ed.). Oxford [u.a.]: Oxford Univ. Press. p. 560. ISBN 978-0-19-857014-1. Archived from the original on 6 September 2015.
- ^ Uplekar M, Weil D, Lonnroth K, Jaramillo E, Lienhardt C, Dias HM, et al. (May 2015). "WHO's new end TB strategy". Lancet. 385 (9979): 1799–1801. doi:10.1016/S0140-6736(15)60570-0. PMID 25814376. S2CID 39379915.
- ^ Fraser A, Paul M, Attamna A, Leibovici L, et al. (Cochrane Infectious Diseases Group) (April 2006). "Drugs for preventing tuberculosis in people at risk of multiple-drug-resistant pulmonary tuberculosis". The Cochrane Database of Systematic Reviews. 2006 (2): CD005435. doi:10.1002/14651858.CD005435.pub2. PMC 6532726. PMID 16625639.
- ^ Piggott DA, Karakousis PC (27 December 2010). "Timing of antiretroviral therapy for HIV in the setting of TB treatment". Clinical & Developmental Immunology. 2011: 103917. doi:10.1155/2011/103917. PMC 3017895. PMID 21234380.
- ^ Brennan PJ, Nikaido H (1995). "The envelope of mycobacteria". Annual Review of Biochemistry. 64: 29–63. doi:10.1146/annurev.bi.64.070195.000333. PMID 7574484.
- ^ Davies G, Cerri S, Richeldi L (October 2007). "Rifabutin for treating pulmonary tuberculosis". The Cochrane Database of Systematic Reviews. 2007 (4): CD005159. doi:10.1002/14651858.CD005159.pub2. PMC 6532710. PMID 17943842.
- ^ Di Bella S, Luzzati R, Principe L, Zerbato V, Meroni E, Giuffrè M, et al. (January 2022). "Aspirin and Infection: A Narrative Review". Biomedicines. 10 (2): 263. doi:10.3390/biomedicines10020263. PMC 8868581. PMID 35203473.
- ^ a b Latent tuberculosis infection. World Health Organization (WHO). 2018. p. 23. ISBN 978-92-4-155023-9. Archived from the original on 2 June 2021. Retrieved 25 July 2018.
- ^ Borisov AS, Bamrah Morris S, Njie GJ, Winston CA, Burton D, Goldberg S, et al. (June 2018). "Update of Recommendations for Use of Once-Weekly Isoniazid-Rifapentine Regimen to Treat Latent Mycobacterium tuberculosis Infection". MMWR. Morbidity and Mortality Weekly Report. 67 (25): 723–726. doi:10.15585/mmwr.mm6725a5. PMC 6023184. PMID 29953429.
- ^ a b Sterling TR, Njie G, Zenner D, Cohn DL, Reves R, Ahmed A, et al. (February 2020). "Guidelines for the Treatment of Latent Tuberculosis Infection: Recommendations from the National Tuberculosis Controllers Association and CDC, 2020". MMWR. Recommendations and Reports. 69 (1): 1–11. doi:10.15585/mmwr.rr6901a1. PMC 7041302. PMID 32053584.
- ^ Njie GJ, Morris SB, Woodruff RY, Moro RN, Vernon AA, Borisov AS (August 2018). "Isoniazid-Rifapentine for Latent Tuberculosis Infection: A Systematic Review and Meta-analysis". American Journal of Preventive Medicine. 55 (2): 244–252. doi:10.1016/j.amepre.2018.04.030. PMC 6097523. PMID 29910114.
- ^ Menzies D, Al Jahdali H, Al Otaibi B (March 2011). "Recent developments in treatment of latent tuberculosis infection". The Indian Journal of Medical Research. 133 (3): 257–66. PMC 3103149. PMID 21441678.
- ^ M'imunya JM, Kredo T, Volmink J, et al. (Cochrane Infectious Diseases Group) (May 2012). "Patient education and counselling for promoting adherence to treatment for tuberculosis". The Cochrane Database of Systematic Reviews. 2012 (5): CD006591. doi:10.1002/14651858.CD006591.pub2. PMC 6532681. PMID 22592714.
- ^ Gelband H, et al. (Cochrane Infectious Diseases Group) (25 October 1999). "Regimens of less than six months for treating tuberculosis". The Cochrane Database of Systematic Reviews. 1999 (2): CD001362. doi:10.1002/14651858.CD001362. PMC 6532732. PMID 10796641.
- ^ Grace AG, Mittal A, Jain S, Tripathy JP, Satyanarayana S, Tharyan P, et al. (Cochrane Infectious Diseases Group) (December 2019). "Shortened treatment regimens versus the standard regimen for drug-sensitive pulmonary tuberculosis". The Cochrane Database of Systematic Reviews. 12 (12): CD012918. doi:10.1002/14651858.CD012918.pub2. PMC 6953336. PMID 31828771.
- ^ "Landmark TB Trial Identifies Shorter-Course Treatment Regimen". CDC. NCHHSTP Media Team Centers for Disease Control and Prevention. 20 October 2020. Archived from the original on 27 November 2021. Retrieved 27 November 2021.
- ^ Mainous III AB (2010). Management of Antimicrobials in Infectious Diseases: Impact of Antibiotic Resistance. Totowa, NJ: Humana Press. p. 69. ISBN 978-1-60327-238-4. Archived from the original on 6 September 2015.
- ^ a b c Karumbi J, Garner P (May 2015). "Directly observed therapy for treating tuberculosis". The Cochrane Database of Systematic Reviews. 2015 (5): CD003343. doi:10.1002/14651858.CD003343.pub4. PMC 4460720. PMID 26022367.
- ^ Liu Q, Abba K, Alejandria MM, Sinclair D, Balanag VM, Lansang MA, et al. (Cochrane Infectious Diseases Group) (November 2014). "Reminder systems to improve patient adherence to tuberculosis clinic appointments for diagnosis and treatment". The Cochrane Database of Systematic Reviews. 2014 (11): CD006594. doi:10.1002/14651858.CD006594.pub3. PMC 4448217. PMID 25403701.
- ^ Mwandumba HC, Squire SB, et al. (Cochrane Infectious Diseases Group) (23 October 2001). "Fully intermittent dosing with drugs for treating tuberculosis in adults". The Cochrane Database of Systematic Reviews (4): CD000970. doi:10.1002/14651858.CD000970. PMC 6532565. PMID 11687088.
- ^ Bose A, Kalita S, Rose W, Tharyan P, et al. (Cochrane Infectious Diseases Group) (January 2014). "Intermittent versus daily therapy for treating tuberculosis in children". The Cochrane Database of Systematic Reviews. 2014 (1): CD007953. doi:10.1002/14651858.CD007953.pub2. PMC 6532685. PMID 24470141.
- ^ O'Brien RJ (June 1994). "Drug-resistant tuberculosis: etiology, management and prevention". Seminars in Respiratory Infections. 9 (2): 104–12. PMID 7973169.
- ^ Centers for Disease Control and Prevention (CDC) (March 2006). "Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs--worldwide, 2000-2004". MMWR. Morbidity and Mortality Weekly Report. 55 (11): 301–5. PMID 16557213. Archived from the original on 22 May 2017.
- ^ a b McKenna M (12 January 2012). "Totally Resistant TB: Earliest Cases in Italy". Wired. Archived from the original on 14 January 2012. Retrieved 12 January 2012.
- ^ Migliori GB, De Iaco G, Besozzi G, Centis R, Cirillo DM (May 2007). "First tuberculosis cases in Italy resistant to all tested drugs". Euro Surveillance. 12 (5): E070517.1. doi:10.2807/esw.12.20.03194-en. PMID 17868596.
- ^ "Totally Drug-Resistant TB: a WHO consultation on the diagnostic definition and treatment options" (PDF). World Health Organization (WHO). Archived (PDF) from the original on 21 October 2016. Retrieved 25 March 2016.
- ^ a b c d e f g h i j k l m n o p Kielstra P (30 June 2014). Tabary Z (ed.). "Ancient enemy, modern imperative – A time for greater action against tuberculosis" (PDF). The Economist. Economist Intelligence Unit. Archived from the original (PDF) on 10 August 2014. Retrieved 22 January 2022.
- ^ Singh B, Cocker D, Ryan H, Sloan DJ, et al. (Cochrane Infectious Diseases Group) (March 2019). "Linezolid for drug-resistant pulmonary tuberculosis". The Cochrane Database of Systematic Reviews. 3 (3): CD012836. doi:10.1002/14651858.CD012836.pub2. PMC 6426281. PMID 30893466.
- ^ Velayati AA, Masjedi MR, Farnia P, Tabarsi P, Ghanavi J, ZiaZarifi AH, et al. (August 2009). "Emergence of new forms of totally drug-resistant tuberculosis bacilli: super extensively drug-resistant tuberculosis or totally drug-resistant strains in Iran". Chest. 136 (2): 420–425. doi:10.1378/chest.08-2427. PMID 19349380.
- ^ "Provisional CDC Guidelines for the Use and Safety Monitoring of Bedaquiline Fumarate (Sirturo) for the Treatment of Multidrug-Resistant Tuberculosis". Archived from the original on 4 January 2014.
- ^ Theron G, Peter J, Richardson M, Warren R, Dheda K, Steingart KR, et al. (Cochrane Infectious Diseases Group) (September 2016). "® MTBDRsl assay for resistance to second-line anti-tuberculosis drugs". The Cochrane Database of Systematic Reviews. 2016 (9): CD010705. doi:10.1002/14651858.CD010705.pub3. PMC 5034505. PMID 27605387.
- ^ "The use of molecular line probe assays for the detection of resistance to second-line anti-tuberculosis drugs" (PDF). World Health Organization. Archived (PDF) from the original on 22 September 2021. Retrieved 18 June 2021.
- ^ "WHO Disease and injury country estimates". World Health Organization (WHO). 2004. Archived from the original on 11 November 2009. Retrieved 11 November 2009.
- ^ Lambert ML, Hasker E, Van Deun A, Roberfroid D, Boelaert M, Van der Stuyft P (May 2003). "Recurrence in tuberculosis: relapse or reinfection?". The Lancet. Infectious Diseases. 3 (5): 282–7. doi:10.1016/S1473-3099(03)00607-8. PMID 12726976.
- ^ Wang JY, Lee LN, Lai HC, Hsu HL, Liaw YS, Hsueh PR, et al. (July 2007). "Prediction of the tuberculosis reinfection proportion from the local incidence". The Journal of Infectious Diseases. 196 (2): 281–8. doi:10.1086/518898. PMID 17570116.
- ^ "1.4 Prognosis - Tuberculosis". medicalguidelines.msf.org. Archived from the original on 2 June 2021. Retrieved 25 August 2020.
- ^ "Fact Sheets: The Difference Between Latent TB Infection and Active TB Disease". Centers for Disease Control and Prevention (CDC). 20 June 2011. Archived from the original on 4 August 2011. Retrieved 26 July 2011.
- ^ "Global tuberculosis report 2013". World Health Organization (WHO). 2013. Archived from the original on 12 December 2006.
- ^ Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMC 10790329. PMID 23245604. S2CID 1541253. Archived from the original on 19 May 2020. Retrieved 18 March 2020.
- ^ a b c "Global Tuberculosis Control 2011" (PDF). World Health Organization (WHO). Archived from the original (PDF) on 17 June 2012. Retrieved 15 April 2012.
- ^ "Tuberculosis". WHO. 24 March 2020. Archived from the original on 30 July 2020. Retrieved 31 May 2020.
- ^ Douglas AS, Strachan DP, Maxwell JD (September 1996). "Seasonality of tuberculosis: the reverse of other respiratory diseases in the UK". Thorax. 51 (9): 944–946. doi:10.1136/thx.51.9.944. PMC 472621. PMID 8984709.
- ^ Martineau AR, Nhamoyebonde S, Oni T, Rangaka MX, Marais S, Bangani N, et al. (November 2011). "Reciprocal seasonal variation in vitamin D status and tuberculosis notifications in Cape Town, South Africa". Proceedings of the National Academy of Sciences of the United States of America. 108 (47): 19013–19017. doi:10.1073/pnas.1111825108. PMC 3223428. PMID 22025704.
- ^ Parrinello CM, Crossa A, Harris TG (January 2012). "Seasonality of tuberculosis in New York City, 1990-2007". The International Journal of Tuberculosis and Lung Disease. 16 (1): 32–37. doi:10.5588/ijtld.11.0145. PMID 22236842.
- ^ a b Korthals Altes H, Kremer K, Erkens C, van Soolingen D, Wallinga J (May 2012). "Tuberculosis seasonality in the Netherlands differs between natives and non-natives: a role for vitamin D deficiency?". The International Journal of Tuberculosis and Lung Disease. 16 (5): 639–644. doi:10.5588/ijtld.11.0680. PMID 22410705.
- ^ Koh GC, Hawthorne G, Turner AM, Kunst H, Dedicoat M (2013). "Tuberculosis incidence correlates with sunshine: an ecological 28-year time series study". PLOS ONE. 8 (3): e57752. Bibcode:2013PLoSO...857752K. doi:10.1371/journal.pone.0057752. PMC 3590299. PMID 23483924.
- ^ Kuddus MA, McBryde ES, Adegboye OA (September 2019). "Delay effect and burden of weather-related tuberculosis cases in Rajshahi province, Bangladesh, 2007-2012". Scientific Reports. 9 (1): 12720. Bibcode:2019NatSR...912720K. doi:10.1038/s41598-019-49135-8. PMC 6722246. PMID 31481739.
- ^ Griffith DE, Kerr CM (August 1996). "Tuberculosis: disease of the past, disease of the present". Journal of PeriAnesthesia Nursing. 11 (4): 240–45. doi:10.1016/S1089-9472(96)80023-2. PMID 8964016.
- ^ "Global Tuberculosis Control Report, 2006 – Annex 1 Profiles of high-burden countries" (PDF). World Health Organization (WHO). Archived from the original (PDF) on 26 July 2009. Retrieved 13 October 2006.
- ^ "2005 Surveillance Slide Set". Centers for Disease Control and Prevention. 12 September 2006. Archived from the original on 23 November 2006. Retrieved 13 October 2006.
- ^ FitzGerald JM, Wang L, Elwood RK (February 2000). "Tuberculosis: 13. Control of the disease among aboriginal people in Canada". Canadian Medical Association Journal. 162 (3): 351–55. PMC 1231016. PMID 10693593.
- ^ Quah SR, Carrin G, Buse K, Heggenhougen K (2009). Health Systems Policy, Finance, and Organization. Boston: Academic Press. p. 424. ISBN 978-0-12-375087-7. Archived from the original on 6 September 2015.
- ^ "Origins of the MRC". Medical Research Council. Archived from the original on 11 April 2008. Retrieved 7 October 2006.
- ^ Shkolnikov VM, Meslé F (1996). "The Russian Epidemiological Crisis as Mirrored by Mortality Trends". In DaVanzo J, Farnsworth G (eds.). Russia's Demographic "Crisis". RAND Corporation. p. 142. ISBN 0-8330-2446-9. Archived from the original on 20 February 2023. Retrieved 20 February 2023.
- ^ "Global Tuberculosis Control". World Health Organization. 2011. Archived from the original on 12 December 2006.
- ^ "WHO global tuberculosis report 2016. Annex 2. Country profiles: Russian Federation". Archived from the original on 14 July 2017. Retrieved 22 August 2020.
- ^ a b c "Global Tuberculosis Report 2018" (PDF). Archived (PDF) from the original on 7 August 2020. Retrieved 27 September 2019.
- ^ Tomlinson C (10 November 2023). "In-depth: What new WHO TB numbers mean for South Africa". Spotlight. Retrieved 27 March 2024.
- ^ "WHO Global tuberculosis report 2016: India". Archived from the original on 6 February 2018. Retrieved 22 August 2020.
- ^ "Govt revisits strategy to combat tuberculosis". Daily News and Analysis. 8 April 2017. Archived from the original on 3 June 2021. Retrieved 22 August 2020.
- ^ Mahla RS (August 2018). "Prevalence of drug-resistant tuberculosis in South Africa". The Lancet. Infectious Diseases. 18 (8): 836. doi:10.1016/S1473-3099(18)30401-8. PMID 30064674.
- ^ Birn AE (2009). Textbook of International Health: Global Health in a Dynamic World. Oxford University Press. p. 261. ISBN 978-0-19-988521-3. Archived from the original on 6 September 2015.
- ^ "CDC Surveillance Slides 2012 – TB". Centers for Disease Control and Prevention. 24 October 2018. Archived from the original on 9 November 2013. Retrieved 17 September 2017.
- ^ Al-Azem A, Kaushal Sharma M, Turenne C, Hoban D, Hershfield E, MacMorran J, et al. (1998). "Rural outbreaks of Mycobacterium tuberculosis in a Canadian province". Abstr Intersci Conf Antimicrob Agents Chemother. 38: 555. abstract no. L-27. Archived from the original on 18 November 2011.
- ^ "Tuberculosis incidence (per 100,000 people)". Our World in Data. Archived from the original on 26 September 2019. Retrieved 7 March 2020.
- ^ "Tuberculosis deaths by region". Our World in Data. Archived from the original on 8 May 2020. Retrieved 7 March 2020.
- ^ a b c Lawlor C. "Katherine Byrne, Tuberculosis and the Victorian Literary Imagination". British Society for Literature and Science. Archived from the original on 6 November 2020. Retrieved 11 June 2017.
- ^ "Hippocrates 3.16 Classics, MIT". Archived from the original on 11 February 2005. Retrieved 15 December 2015.
- ^ Caldwell M (1988). The Last Crusade. New York: Macmillan. p. 21. ISBN 978-0-689-11810-4.
- ^ Bunyan J (1808). The Life and Death of Mr. Badman. London: W. Nicholson. p. 244. Retrieved 28 September 2016 – via Internet Archive.
captain.
- ^ Byrne K (2011). Tuberculosis and the Victorian Literary Imagination. Cambridge University Press. ISBN 978-1-107-67280-2.
- ^ "About Chopin's illness". Icons of Europe. Archived from the original on 28 September 2017. Retrieved 11 June 2017.
- ^ Vilaplana C (March 2017). "A literary approach to tuberculosis: lessons learned from Anton Chekhov, Franz Kafka, and Katherine Mansfield". International Journal of Infectious Diseases. 56: 283–85. doi:10.1016/j.ijid.2016.12.012. PMID 27993687.
- ^ Rogal SJ (1997). A William Somerset Maugham Encyclopedia. Greenwood Publishing. p. 245. ISBN 978-0-313-29916-2. Archived from the original on 2 June 2021. Retrieved 4 October 2017.
- ^ Eschner K. "George Orwell Wrote '1984' While Dying of Tuberculosis". Smithsonian. Archived from the original on 24 March 2019. Retrieved 25 March 2019.
- ^ "Tuberculosis (whole issue)". Journal of the American Medical Association. 293 (22): cover. 8 June 2005. Archived from the original on 24 August 2020. Retrieved 4 October 2017.
- ^ Lemlein RF (1981). "Influence of Tuberculosis on the Work of Visual Artists: Several Prominent Examples". Leonardo. 14 (2): 114–11. doi:10.2307/1574402. JSTOR 1574402. S2CID 191371443.
- ^ Wilsey AM (May 2012). 'Half in Love with Easeful Death:' Tuberculosis in Literature. Humanities Capstone Projects (PhD Thesis thesis). Pacific University. Archived from the original on 11 October 2017. Retrieved 28 September 2017.
- ^ a b Morens DM (November 2002). "At the deathbed of consumptive art". Emerging Infectious Diseases. 8 (11): 1353–8. doi:10.3201/eid0811.020549. PMC 2738548. PMID 12463180.
- ^ "Pulmonary Tuberculosis/In Literature and Art". McMaster University History of Diseases. Retrieved 9 June 2017.
- ^ Thomson G (1 June 2016). "Van Morrison – 10 of the best". The Guardian. Archived from the original on 14 August 2020. Retrieved 28 September 2017.
- ^ "Tuberculosis Throughout History: The Arts" (PDF). United States Agency for International Development (USAID). Archived (PDF) from the original on 30 June 2017. Retrieved 12 June 2017.
- ^ Corliss R (22 December 2008). "Top 10 Worst Christmas Movies". Time. Archived from the original on 22 September 2020. Retrieved 28 September 2017.
'If you don't cry when Bing Crosby tells Ingrid Bergman she has tuberculosis', Joseph McBride wrote in 1973, 'I never want to meet you, and that's that.'
- ^ "The End TB Strategy". who.int. Archived from the original on 22 July 2021. Retrieved 22 July 2021.
- ^ a b c d Global tuberculosis report 2020. World Health Organization. 2020. ISBN 978-92-4-001313-1. Archived from the original on 22 July 2021. Retrieved 22 July 2021.
- ^ a b "Public–Private Partnership Announces Immediate 40 Percent Cost Reduction for Rapid TB Test" (PDF). World Health Organization (WHO). 6 August 2012. Archived (PDF) from the original on 29 October 2013.
- ^ Lawn SD, Nicol MP (September 2011). "Xpert® MTB/RIF assay: development, evaluation and implementation of a new rapid molecular diagnostic for tuberculosis and rifampicin resistance". Future Microbiology. 6 (9): 1067–82. doi:10.2217/fmb.11.84. PMC 3252681. PMID 21958145.
- ^ "WHO says Cepheid rapid test will transform TB care". Reuters. 8 December 2010. Archived from the original on 11 December 2010.
- ^ STOPTB (5 April 2013). "The Stop TB Partnership, which operates through a secretariat hosted by the World Health Organization (WHO) in Geneva, Switzerland" (PDF). Archived (PDF) from the original on 24 January 2014.
- ^ Lienhardt C, Espinal M, Pai M, Maher D, Raviglione MC (November 2011). "What research is needed to stop TB? Introducing the TB Research Movement". PLOS Medicine. 8 (11): e1001135. doi:10.1371/journal.pmed.1001135. PMC 3226454. PMID 22140369.
- ^ Sandhu GK (2011). "Tuberculosis: Current Situation, Challenges and Overview of its Control Programs in India". Journal of Global Infectious Diseases. 3 (2): 143–150. doi:10.4103/0974-777X.81691. ISSN 0974-777X. PMC 3125027. PMID 21731301.
- ^ Bhargava A, Pinto L, Pai M (2011). "Mismanagement of tuberculosis in India: Causes, consequences, and the way forward" (PDF). Hypothesis. 9 (1): e7. Archived from the original (PDF) on 24 October 2022.
- ^ Amdekar Y (July 2009). "Changes in the management of tuberculosis". Indian Journal of Pediatrics. 76 (7): 739–42. doi:10.1007/s12098-009-0164-4. PMID 19693453. S2CID 41788291.
- ^ Fox GJ, Dobler CC, Marks GB (September 2011). "Active case finding in contacts of people with tuberculosis". The Cochrane Database of Systematic Reviews. 2011 (9): CD008477. doi:10.1002/14651858.CD008477.pub2. PMC 6532613. PMID 21901723.
- ^ Mhimbira FA, Cuevas LE, Dacombe R, Mkopi A, Sinclair D, et al. (Cochrane Infectious Diseases Group) (November 2017). "Interventions to increase tuberculosis case detection at primary healthcare or community-level services". The Cochrane Database of Systematic Reviews. 2017 (11): CD011432. doi:10.1002/14651858.CD011432.pub2. PMC 5721626. PMID 29182800.
- ^ Braganza Menezes D, Menezes B, Dedicoat M, et al. (Cochrane Infectious Diseases Group) (August 2019). "Contact tracing strategies in household and congregate environments to identify cases of tuberculosis in low- and moderate-incidence populations". The Cochrane Database of Systematic Reviews. 2019 (8): CD013077. doi:10.1002/14651858.CD013077.pub2. PMC 6713498. PMID 31461540.
- ^ a b c d e f g Courtwright A, Turner AN (July–August 2010). "Tuberculosis and stigmatization: pathways and interventions". Public Health Reports. 125 (4_suppl): 34–42. doi:10.1177/00333549101250S407. PMC 2882973. PMID 20626191.
- ^ Mason PH, Roy A, Spillane J, Singh P (March 2016). "Social, Historical and Cultural Dimensions of Tuberculosis". Journal of Biosocial Science. 48 (2): 206–32. doi:10.1017/S0021932015000115. PMID 25997539.
- ^ a b c Martín Montañés C, Gicquel B (March 2011). "New tuberculosis vaccines". Enfermedades Infecciosas y Microbiologia Clinica. 29 (Suppl 1): 57–62. doi:10.1016/S0213-005X(11)70019-2. PMID 21420568.
- ^ Zhu B, Dockrell HM, Ottenhoff TH, Evans TG, Zhang Y (April 2018). "Tuberculosis vaccines: Opportunities and challenges". Respirology. 23 (4): 359–368. doi:10.1111/resp.13245. hdl:1887/77156. PMID 29341430.
- ^ Ibanga HB, Brookes RH, Hill PC, Owiafe PK, Fletcher HA, Lienhardt C, et al. (August 2006). "Early clinical trials with a new tuberculosis vaccine, MVA85A, in tuberculosis-endemic countries: issues in study design". The Lancet. Infectious Diseases. 6 (8): 522–8. doi:10.1016/S1473-3099(06)70552-7. PMID 16870530.
- ^ Kaufmann SH (October 2010). "Future vaccination strategies against tuberculosis: thinking outside the box". Immunity. 33 (4): 567–77. doi:10.1016/j.immuni.2010.09.015. PMID 21029966.
- ^ Webber D, Kremer M (2001). "Stimulating Industrial R&D for Neglected Infectious Diseases: Economic Perspectives" (PDF). Bulletin of the World Health Organization. 79 (8): 693–801. Archived (PDF) from the original on 26 September 2007.
- ^ Barder O, Kremer M, Williams H (2006). "Advance Market Commitments: A Policy to Stimulate Investment in Vaccines for Neglected Diseases". The Economists' Voice. 3 (3). doi:10.2202/1553-3832.1144. S2CID 154454583. Archived from the original on 5 November 2006.
- ^ Department of Economic and Social Affairs (2009). Achieving the global public health agenda: dialogues at the Economic and Social Council. New York: United Nations. p. 103. ISBN 978-92-1-104596-3. Archived from the original on 6 September 2015.
- ^ Jong EC, Zuckerman JN (2010). Travelers' vaccines (2nd ed.). Shelton, CT: People's Medical Publishing House. p. 319. ISBN 978-1-60795-045-5. Archived from the original on 6 September 2015.
- ^ Bill and Melinda Gates Foundation Announcement (12 February 2004). "Gates Foundation Commits $82.9 Million to Develop New Tuberculosis Vaccines". Archived from the original on 10 October 2009.
- ^ Nightingale K (19 September 2007). "Gates foundation gives US$280 million to fight TB". Archived from the original on 1 December 2008.
- ^ Zumla A, Hafner R, Lienhardt C, Hoelscher M, Nunn A (March 2012). "Advancing the development of tuberculosis therapy". Nature Reviews. Drug Discovery. 11 (3): 171–172. doi:10.1038/nrd3694. PMID 22378254. S2CID 7232434. Archived from the original on 12 January 2020. Retrieved 8 May 2020.
- ^ "J&J Sirturo Wins FDA Approval to Treat Drug-Resistant TB". Bloomberg News. 31 December 2012. Archived from the original on 4 January 2013. Retrieved 1 January 2013.
- ^ Avorn J (April 2013). "Approval of a tuberculosis drug based on a paradoxical surrogate measure". JAMA. 309 (13): 1349–1350. doi:10.1001/jama.2013.623. PMID 23430122.
- ^ US Food and Drug Administration. "Briefing Package: NDA 204–384: Sirturo" (PDF). Food and Drug Administration. Archived (PDF) from the original on 4 January 2014.
- ^ Zuckerman D, Yttri J (January 2013). "Antibiotics: When science and wishful thinking collide". Health Affairs. doi:10.1377/forefront.20130125.027503. Archived from the original on 29 March 2022. Retrieved 29 March 2022.
- ^ Mbuagbaw L, Guglielmetti L, Hewison C, Bakare N, Bastard M, Caumes E, et al. (May 2019). "Outcomes of Bedaquiline Treatment in Patients with Multidrug-Resistant Tuberculosis". Emerging Infectious Diseases. 25 (5): 936–943. doi:10.3201/eid2505.181823. PMC 6478224. PMID 31002070.
- ^ Khoshnood S, Taki E, Sadeghifard N, Kaviar VH, Haddadi MH, Farshadzadeh Z, et al. (7 October 2021). "Mechanism of Action, Resistance, Synergism, and Clinical Implications of Delamanid Against Multidrug-Resistant Mycobacterium tuberculosis". Frontiers in Microbiology. 12: 717045. doi:10.3389/fmicb.2021.717045. PMC 8529252. PMID 34690963.
- ^ "European Medicines Agency - News and Events - European Medicines Agency recommends two new treatment options for tuberculosis". 3 December 2013. Archived from the original on 3 December 2013. Retrieved 9 April 2024.
- ^ Khoshnood S, Taki E, Sadeghifard N, Kaviar VH, Haddadi MH, Farshadzadeh Z, et al. (7 October 2021). "Mechanism of Action, Resistance, Synergism, and Clinical Implications of Delamanid Against Multidrug-Resistant Mycobacterium tuberculosis". Frontiers in Microbiology. 12: 717045. doi:10.3389/fmicb.2021.717045. PMC 8529252. PMID 34690963.
- ^ Critchley JA, Orton LC, Pearson F (November 2014). "Adjunctive steroid therapy for managing pulmonary tuberculosis". The Cochrane Database of Systematic Reviews. 2014 (11): CD011370. doi:10.1002/14651858.CD011370. PMC 6532561. PMID 25387839.
- ^ Shivaprasad HL, Palmieri C (January 2012). "Pathology of mycobacteriosis in birds". The Veterinary Clinics of North America. Exotic Animal Practice. 15 (1): 41–55, v–vi. doi:10.1016/j.cvex.2011.11.004. PMID 22244112.
- ^ Reavill DR, Schmidt RE (January 2012). "Mycobacterial lesions in fish, amphibians, reptiles, rodents, lagomorphs, and ferrets with reference to animal models". The Veterinary Clinics of North America. Exotic Animal Practice. 15 (1): 25–40, v. doi:10.1016/j.cvex.2011.10.001. PMID 22244111.
- ^ Mitchell MA (January 2012). "Mycobacterial infections in reptiles". The Veterinary Clinics of North America. Exotic Animal Practice. 15 (1): 101–11, vii. doi:10.1016/j.cvex.2011.10.002. PMID 22244116.
- ^ Wobeser GA (2006). Essentials of disease in wild animals (1st ed.). Ames, IO [u.a.]: Blackwell Publishing. p. 170. ISBN 978-0-8138-0589-4. Archived from the original on 6 September 2015.
- ^ Ryan TJ, Livingstone PG, Ramsey DS, de Lisle GW, Nugent G, Collins DM, et al. (February 2006). "Advances in understanding disease epidemiology and implications for control and eradication of tuberculosis in livestock: the experience from New Zealand". Veterinary Microbiology. 112 (2–4): 211–19. doi:10.1016/j.vetmic.2005.11.025. PMID 16330161.
- ^ White PC, Böhm M, Marion G, Hutchings MR (September 2008). "Control of bovine tuberculosis in British livestock: there is no 'silver bullet'". Trends in Microbiology. 16 (9): 420–7. CiteSeerX 10.1.1.566.5547. doi:10.1016/j.tim.2008.06.005. PMID 18706814.
- ^ Ward AI, Judge J, Delahay RJ (January 2010). "Farm husbandry and badger behaviour: opportunities to manage badger to cattle transmission of Mycobacterium bovis?". Preventive Veterinary Medicine. 93 (1): 2–10. doi:10.1016/j.prevetmed.2009.09.014. PMID 19846226.
- ^ Holt N (24 March 2015). "The Infected Elephant in the Room". Slate. Archived from the original on 14 April 2016. Retrieved 5 April 2016.
- ^ Mikota SK. "A Brief History of TB in Elephants" (PDF). Animal and Plant Health Inspection Service (APHIS). Archived (PDF) from the original on 6 October 2016. Retrieved 5 April 2016.
External links
- Tuberculosis at Curlie
- "Tuberculosis (TB)". Centers for Disease Control and Prevention (CDC). 24 October 2018.
- "Tuberculosis (TB)". London: Health Protection Agency. Archived from the original on 5 July 2007.
- WHO global 2016 TB report (infographic)
- WHO tuberculosis country profiles
- "Tuberculosis Among African Americans", 1990-11-01, In Black America; KUT Radio, American Archive of Public Broadcasting (WGBH and the Library of Congress)
- Working Group on New TB drugs, tracking clinical trials and drug candidates