Mycobacterium tuberculosis
| Mycobacterium tuberculosis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Mycobacterium tuberculosis |
||||||||||||
| Systematics | ||||||||||||
|
||||||||||||
| Scientific name | ||||||||||||
| Mycobacterium tuberculosis | ||||||||||||
| ( Zopf 1883) Lehmann & Neumann 1896 |
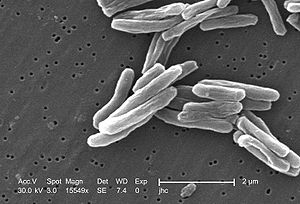
Mycobacterium tuberculosis , also known as tubercle bacillus in German, is a bacterium from the Mycobacteriaceae (mycobacteria) family. It is the major causative agent of tuberculosis in humans. Animals can alsodevelop tuberculosisthrough M. tuberculosis .
properties
M. tuberculosis is a rod-shaped bacterium incapable of active movement. The bacteria are acid-fast and can therefore be differentiated microscopically from non-acid-fast bacteria and other non-acid-fast objects using the Ziehl-Neelsen stain and special fluorescent dye stains (e.g. auramine stain). The bacterial cell wall contains, among other things, arabinogalactan and mycolic acids , which, along with other lipophilic cell wall components, are responsible for acid resistance.
Other characteristic features are its extremely slow growth (15-20 hours to division), the ability to withstand weak disinfectants, aerobics and intracellular pathogenesis. The bacterium is able to survive dormant in macrophages (scavenger cells of the immune system) and, after years of waking up, then to divide ( dormancy ). At the genomic level, an unusually large part of its genes encodes the enzymes for the production of lipolysis (fat-splitting) and lipogenesis (fat synthesis) enzymes. The lipids in the cell wall mask underlying molecular structures that induce a suitable immune response in other bacteria. In addition, the bacterium is not only able to live on its own fat layer deposited in the cell wall, but also to collect and use external cholesterol that is found in humans during the infection.
Intracellular Pathogenesis
M. tuberculosis has developed several mechanisms in order to be able to survive in the phagosome : it initially has a waxy, fat-rich cell wall, which enables it to defend itself against its destruction within the immune system. The phagosome is unable to split open the outer layer of the pathogen's cell wall. In addition, the outer wax layer contains lipoarabinomannan (LAM), a glycolipid that, together with a phosphatase, disrupts the signal transduction of the phagosome so that it does not go through the full destruction program.
Furthermore, several enzymes ( catalase , superoxide dismutase and others) are excreted by the bacterium , which eliminate any danger from reactive oxygen and nitrogen species (the catalase also acts as peroxynitritase ). Finally, the bacterium brings itself into a hibernation-like state ( dormancy ), in which no DNA replication and cell division takes place, and the organism lives anaerobically on its own fat layer on the back burner. As a result, many antibiotics that otherwise interfere with normal cell processes become ineffective.
In addition, there is an increased mutation rate due to reading errors in the DNA polymerase and reactive oxygen species (ROS) generated by the macrophages , which damage the DNA of the bacterium and lead to mutations even in the case of latent infection . This means that the bacterium can develop resistance even if it does not divide.
Infection, disease, therapy in humans
The transmission usually takes place through a droplet infection . The main entry point is the lungs. Infection of the lungs leads to the formation of nodules and destruction of the lung tissue, as well as the spread of tuberculous foci in the body. Malnourished and debilitated people are particularly susceptible to the disease. Today about every third person in the world is infected with Mycobacterium tuberculosis. In third world countries in particular, antibiotic treatment is difficult because it takes months. In addition, there are more and more cases in which the pathogen is resistant to many antibiotics. Tuberculosis kills 2 million people every year and, along with AIDS and malaria, it is the most widespread infectious disease in the world.
Infection and disease in farm animals and domestic animals
Animals are always infected by people suffering from overt tuberculosis. As a result, cattle are not only affected by the M. bovis variant ; In Ethiopia, for example, M. tuberculosis was found in up to a quarter of free-range animals , while fenced animals were partially infected with M. bovis . The cause is probably the habit of the shepherds there to spit chewed tobacco into the mouth of cattle to fight parasites.
A disease was also observed in pigs , horses , sheep and goats . Chickens are largely resistant to M. tuberculosis . Diseased animals usually only develop a local process that heals quickly. In such cases, it is advisable to check the caregivers for tuberculosis.
The infection of domestic animals that live in close household with humans is much more serious. Dogs , cats and possibly parrots are first infected by openly tuberculous people, develop mostly open tuberculosis themselves and thus form a dangerous source of infection for people who come into contact with them.
Antibiotic resistance
Due to several properties, M. tuberculosis is able to render antibiotics harmless. In particular, the impermeability of the outer waxy cell wall means that foreign substances are only absorbed via transport proteins, which can be very selective. Furthermore, several of the functioning antibiotics are dependent on activation by bacterial enzymes ( prodrug ). Many others are effectively removed from the cell by efflux pumps . Finally, the antibiotics' targets are all enzymes or ribosomes. Since proteins are involved in all of these processes, a mutation at the corresponding position in the protein is often sufficient either to eliminate a point of attack, to deactivate activating enzymes, to overexpress inhibited enzymes and efflux pumps, or to specialize in importing an antibiotic to its effect the bacterium loses and resistance develops. The following is a table of the known antibiotics for M. tuberculosis with their mechanisms of action and resistance:
| antibiotic | Site of action | Resistance gene (s) |
Mechanism of Resistance |
|---|---|---|---|
| Isoniazid , ethionamide | (Prodrug) fatty acid synthesis | katG, ahpC, ndh | Loss of activation |
| content | Mutation at the point of attack | ||
| Rifampicin | Elongation of mRNA transcription | rpoB | Mutation at the point of attack |
| Pyrazinamide | (Prodrug) trans-translation | pncA | Loss of activation |
| Streptomycin | Initiation of translation | rpsL | Mutation at the point of attack |
| Ethambutol | Arabinogalactan Biosynthesis | embB,? | Mutation at the point of attack |
| Fluoroquinolones | DNA replication | gyrA, gyrB | Mutation at the point of attack |
| ? | Efflux pumps | ||
| MfpA | ? | ||
| Kanamycin | Translation | rrs | Loss of ribose methylation |
| ice cream | Breakdown of the antibiotic | ||
| 4-aminosalicylic acid | (Prodrug)? | thyA? | ? |
| Macrolides | Translation | erm37 | Ribosome methylation |
| Linezolid , PNU100480 | Initiation of translation | (23S rRNA) | Mutation at the point of attack |
| D-cycloserine | Peptidoglycan synthesis | alr | Mutation at the point of attack |
| TMC207 | ATP synthesis | atpE,? | Mutation at the point of attack |
| PA-824 , OPC-67683 | (Prodrug) lipid synthesis? | Rv3547 | Loss of activation |
| MetSox | Glutamate Synthesis | glnA1, glnA3 | Deletion of a base with the following overexpression |
| Halicin ( drug approval not yet granted .) |
Multi-resistance
Common abbreviations:
- MDR-TB : multi-resistant tuberculosis bacterium
- XDR-TB : extremely resistant tuberculosis bacterium
M. tuberculosis strains that show at least one resistance to the TB standard antibiotics isoniazid and rifampicin are referred to as multi- resistant . The first major MDR-TB epidemic occurred in New York in the early 1990s and mainly affected people infected with HIV and medical personnel. In 2007 around 20 percent of all isolates worldwide were multi-resistant.
Those MDR-TB strains with additional resistance to at least one fluoroquinolone antibiotic and at least one of the drugs capreomycin , kanamycin or amikacin are called extremely resistant . One of the first XDR-TB outbreaks occurred in a rural hospital in KwaZulu-Natal in 2005 . The risk of such epidemics is not limited to Africa, as XDR-TB is now found on six continents and averaged around 10 percent of MDR-TB cases in 2007.
In the meantime, linezolid is also becoming more and more resistant.
The term TDR-TB ( totally drug resistant tuberculosis ), which inter alia. brought up for discussion in connection with tuberculosis cases in India is not recognized by the World Health Organization.
proof
The gold standard for detection is cultivation in the laboratory on a selective culture medium such as Lowenstein-Jensen agar and microscopic detection using Ziehl-Neelsen staining . It is possible to accelerate growth in Middlebrook 7H10 Agar . Unconventional approaches are microcaloric detection of slow growth or the detection of very small amounts of typical volatile esters (methylphenyl acetate, methyl p-anisate, methyl nicotinate) by honey bees .
The analysis of heat-sterilized material by means of mass spectrometry could develop as the new gold standard . Due to the different lipid profile, among other things, it is possible to differentiate between individual Mycobacterium species in a short time and with a high degree of certainty .
story
The French doctor Jean-Antoine Villemin (1827-1892) showed as early as 1865 that tuberculosis can be transmitted. However, it was still mostly mistaken for a constitutional disease. The bacterium was discovered by Robert Koch in 1882 and isolated for the first time, with which Koch had definitively proven transmission by a living microorganism. Through pure culture and animal experiments, he was able to prove in the form of Koch's postulates that tuberculosis is caused by M. tuberculosis .
Mycobacterium tuberculosis is traced back to a 40,000 year old predecessor to which Mycobacterium leprae and Mycobacterium bovis are also traced back.
In 2019, a potentially effective antibiotic against Mycobacterium tuberculosis was found with the molecule halicin .
Reporting requirement
In Germany, the direct detection of Mycobacterium tuberculosis must be reported by name in accordance with Section 7 of the Infection Protection Act . The reporting obligation only applies if the direct evidence indicates an acute infection and, subsequently, for the result of the resistance determination; in advance also for the detection of acid-fast rods in the sputum. The obligation to notify primarily concerns the management of laboratories ( § 8 IfSG).
In Switzerland, the positive and negative laboratory-analytical findings of pathogens from the Mycobacterium tuberculosis complex must be reported to laboratories in accordance with the Epidemics Act (EpG) in conjunction with the Epidemics Ordinance and Annex 3 of the Ordinance of the FDHA on the reporting of observations of communicable diseases in humans .
literature
- Karl Bernhard Lehmann, Rudolf Otto Neumann: Atlas and outline of bacteriology and textbook of special bacteriological diagnostics . Lehmann, Munich 1896.
- W. Köhler et al .: Medical Microbiology. Urban & Fischer-Verlag Munich / Jena 2001, 8th edition. ISBN 3-437-41640-5
- I. Comas, S. Gagneux: The past and future of tuberculosis research. In: PLoS Pathog . Volume 5, number 10, October 2009, p. E1000600, doi: 10.1371 / journal.ppat.1000600 , PMID 19855821 , PMC 2745564 (free full text) (review).
- Ulrike Roll: tubercle bacillus. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1423 f.
- S. Hähner-Rombach: The great death - epidemics make history. Berlin 1995, p. 278 ff.
Web links
- Genome of Mtu ATCC 25618 / H37Rv at the Sanger Institute (first sequenced genome)
- TubercuList at EPFL (genome database; last update 2011)
- TubercuList at the Pasteur Institute (genome database; last update 2008-Oct)
- TB Database (comparative genomics database)
Individual evidence
- ↑ CJ Cambier, Kevin K. Takaki et al .: Mycobacteria manipulate macrophage recruitment through coordinated use of membrane lipids. In: Nature. 2013, S., doi: 10.1038 / nature12799 .
- ↑ A. Brzostek, J. Pawelczyk et al .: Mycobacterium tuberculosis is able to accumulate and utilize cholesterol. In: J. Bacteriol. Volume 191, Number 21, November 2009, pp. 6584-6591, ISSN 1098-5530 . doi: 10.1128 / JB.00488-09 . PMID 19717592 . PMC 2795286 (free full text).
- ↑ Briken V, Porcelli SA, Besra GS, Kremer L: Mycobacterial lipoarabinomannan and related lipoglycans: from biogenesis to modulation of the immune response . In: Mol. Microbiol. . 53, No. 2, July 2004, pp. 391-403. doi : 10.1111 / j.1365-2958.2004.04183.x . PMID 15228522 .
- ↑ Hestvik AL, Hmama Z, Av-Gay Y: Mycobacterial manipulation of the host cell . In: FEMS Microbiol. Rev. . 29, No. 5, November 2005, pp. 1041-50. doi : 10.1016 / j.femsre.2005.04.013 . PMID 16040149 .
- ↑ Deretic V, Singh S, Master S, et al. : Mycobacterium tuberculosis inhibition of phagolysosome biogenesis and autophagy as a host defense mechanism . In: Cell. Microbiol. . 8, No. 5, May 2006, pp. 719-27. doi : 10.1111 / j.1462-5822.2006.00705.x . PMID 16611222 .
- ↑ CB Ford, PL Lin et al .: Use of whole genome sequencing to estimate the mutation rate of Mycobacterium tuberculosis during latent infection. In: Nat. Genet. Volume 43, Number 5, May 2011, pp. 482-486, ISSN 1546-1718 . doi: 10.1038 / ng.811 . PMID 21516081 . PMC 310187 (free full text).
- ↑ G. Ameni, M. Vordermeier et al .: Mycobacterium tuberculosis infection in grazing cattle in central Ethiopia. In: Veterinary journal (London, England: 1997) Volume 188, Number 3, June 2011, pp. 359-361. doi: 10.1016 / j.tvjl.2010.05.005 . PMID 20965132 . PMC 310382 (free full text).
- ↑ PE Almeida Da Silva, JC Palomino: Molecular basis and mechanisms of drug resistance in Mycobacterium tuberculosis: classical and new drugs. In: Journal of Antimicrobial Chemotherapy . Volume 66, Number 7, July 2011, pp. 1417-1430, ISSN 1460-2091 . doi: 10.1093 / jac / dkr173 . PMID 21558086 . (Review).
- ↑ W. Shi, X. Zhang et al .: Pyrazinamide inhibits trans-translation in Mycobacterium tuberculosis. In: Science . Volume 333, Number 6049, September 2011, pp. 1630-1632, ISSN 1095-9203 . doi: 10.1126 / science.1208813 . PMID 21835980 .
- ↑ W. Chen, T. Biswas et al .: Unusual regioversatility of acetyltransferase ice, a cause of drug resistance in XDR-TB. In: Proceedings of the National Academy of Sciences of the United States of America . Volume 108, Number 24, June 2011, pp. 9804-9808. doi: 10.1073 / pnas.1105379108 . PMID 21628583 . PMC 3116390 (free full text).
- ↑ P. Carroll, SJ Waddell et al .: Methionine sulfoximine resistance in Mycobacterium tuberculosis is due to a single nucleotide deletion resulting in increased expression of the major glutamine synthetase, GlnA1. In: Microbial Drug Resistance Volume 17, Number 3, September 2011, pp. 351-355, ISSN 1931-8448 . doi: 10.1089 / mdr.2010.0125 . PMID 21875360 . PMC 3161625 (free full text).
- ^ TR Frieden, LF Sherman et al .: A multi-institutional outbreak of highly drug-resistant tuberculosis: epidemiology and clinical outcomes. In: JAMA Volume 276, Number 15, October 1996, pp. 1229-1235, ISSN 0098-7484 . PMID 8849750 .
- ↑ a b N. S. Shah, A. Wright et al .: Worldwide emergence of extensively drug-resistant tuberculosis. In: Emerging Infect. Dis. Volume 13, Number 3, March 2007, pp. 380-387, ISSN 1080-6040 . PMID 17552090 . PMC 272591 (free full text).
- ↑ MC Raviglione, IM Smith: XDR tuberculosis implications for global public health. In: N. Engl. J. Med. Volume 356, Number 7, February 2007, pp. 656-659, ISSN 1533-4406 . doi: 10.1056 / NEJMp068273 . PMID 17301295 .
- ^ NR Gandhi, A. Moll et al .: Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. In: The Lancet Volume 368, Number 9547, November 2006, pp. 1575-1580, ISSN 1474-547X . doi: 10.1016 / S0140-6736 (06) 69573-1 . PMID 17084757 .
- ^ Katherine Rowland: Totally drug-resistant TB emerges in India - Discovery of a deadly form of TB highlights crisis of mismanagement . Nature magazine website . Retrieved February 18, 2012.
- ↑ WHO: Drug-resistant tuberculosis - Frequently asked questions ( Memento of February 23, 2012 in the Internet Archive ). World Health Organization website. Retrieved February 18, 2012
- ↑ O. Braissant, D. Wirz et al .: "The heat is on": rapid microcalorimetric detection of mycobacteria in culture. In: Tuberculosis. Volume 90, Number 1, January 2010, pp. 57-59. doi: 10.1016 / j.tube.2009.11.001 . PMID 19969505 .
- ↑ DM Suckling, RL Sagar: Honeybees Apis mellifera can detect the scent of Mycobacterium tuberculosis. In: Tuberculosis. Volume 91, Number 4, July 2011, pp. 327-328. doi: 10.1016 / j.tube.2011.04.008 . PMID 21546308 .
- ↑ A. El Khéchine, C. Couderc et al .: Matrix-assisted laser desorption / ionization time-of-flight mass spectrometry identification of mycobacteria in routine clinical practice. In: PLOS ONE . Volume 6, number 9, 2011, p. E24720, ISSN 1932-6203 . doi: 10.1371 / journal.pone.0024720 . PMID 21935444 . PMC 3172293 (free full text).
- ↑ Z Djelouadji, D Raoult, M Drancourt: Palaeogenomics of Mycobacterium tuberculosis: epidemic bursts with a degrading genome. Lancet Infect Dis . 13 June 2011, doi: 10.1016 / S1473-3099 (11) 70093-7 .
- ↑ Julia Merlot, DER SPIEGEL: Fighting Resistance: Artificial Intelligence Discovers Promising Antibiotic - DER SPIEGEL - Science. Retrieved February 22, 2020 .
- ↑ tuberculosis. RKI advisor. In: rki.de. Robert Koch Institute, February 21, 2013, accessed on March 18, 2020 (mandatory notification according to IfSG).
