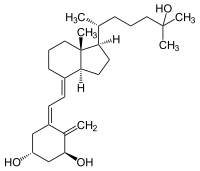
Calcitriol
| Structural formula | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||
| General | |||||||||||||||||||
| Non-proprietary name | Calcitriol | ||||||||||||||||||
| other names |
|
||||||||||||||||||
| Molecular formula | C 27 H 44 O 3 | ||||||||||||||||||
| External identifiers / databases | |||||||||||||||||||
|
|||||||||||||||||||
| Drug information | |||||||||||||||||||
| ATC code | |||||||||||||||||||
| Drug class |
vitamin |
||||||||||||||||||
| properties | |||||||||||||||||||
| Molar mass | 416.64 g mol −1 | ||||||||||||||||||
| Physical state |
firmly |
||||||||||||||||||
| Melting point |
113 ° C |
||||||||||||||||||
| safety instructions | |||||||||||||||||||
|
|||||||||||||||||||
| Toxicological data | |||||||||||||||||||
| As far as possible and customary, SI units are used. Unless otherwise noted, the data given apply to standard conditions . | |||||||||||||||||||
Calcitriol , also 1 α , 25 (OH) 2 -Cholecalciferol (1 α , 25 (OH) 2 vitamin D 3 ) or 1,25 (OH) 2 D 3 and vitamin D for short , is a highly effective secosteroid with structural similarities to the Steroid hormones identified by Michael F. Holick . It is the physiologically active form of the prohormone vitamin D 3 . It is hydroxylated by the 1 α -hydroxylase , especially in the kidneys, but also in other tissues from the 25 (OH) vitamin D 3 or, in rare cases, prescribed as a drug.
Calcitriol is bound to an intracellular receptor protein , the vitamin D receptor (VDR), and transported into the cell nucleus . There the vitamin-receptor complex associates with the DNA and changes the transcription of different hormone-sensitive genes, which ultimately leads to changes in protein synthesis with corresponding biological effects. Calcitriol acts u. a .:
- anti-osteoporotic ,
- modulating the immune system (improved defense against many infections, e.g. tuberculosis , protection against many autoimmune diseases ),
- as protection against many types of cancer ,
- against psoriasis (psoriasis) and alopecia areata ,
- stimulating the motility of the sperm .
Its effectiveness is finely regulated in the body.
Originates in the liver and kidneys
The calcitriol precursor 25 (OH) vitamin D 3 is activated to calcitriol by the 1 α -hydroxylase in the kidneys for endocrine (affecting the whole organism) tasks and in various other cells for autocrine tasks (locally affecting the activating tissue). These activations are regulated differently.
kidney
The vitamin D metabolites are primarily filtered in the glomerula of the kidneys together with the VDBP , then reabsorbed in the proximal tubular cells with the help of the megaline and released there. In the mitochondria of the cells of the proximal tubule of the kidneys, the 25 (OH) vitamin D 3 can :
- further hydroxylated by 1 α -hydroxylase to the biologically active 1,25 (OH) 2 vitamin D 3 , (calcitriol),
- be inactivated by the oppositely regulated 24-hydroxylase to 24R, 25 (OH) vitamin D 3 or
- leave the kidney cells unchanged into the blood (to be bound again to VDBP).
The formation of 1,25 (OH) 2 vitamin D 3 in the kidneys is finely regulated: the most important factors that directly promote its enzymatic formation via activation of 1 α -hydroxylase are, independently of one another, an increased parathyroid hormone , a decreased calcium level and low blood phosphate levels . 1,25 (OH) 2 D 3 itself inhibits the 1 α -hydroxylase and activates the 24-hydroxylase. Indirectly, mostly via the parathyroid hormone, calcium, estrogen , glucocorticoids , calcitonin , somatotropin and prolactin influence the formation of calcitriol. All of these regulations serve to synthesize just enough of the vitamin that the body can meet its calcium and phosphate requirements in its current situation. The regulation of 24R, 25 (OH) 2 D 3 formation takes place by the same factors, but in the opposite direction.
Other tissues
Here, the 1 α -hydroxylase for vitamin D activation is locally regulated by growth factors and cytokines, how exactly this happens is still being researched.
1α, 25 (OH) 2 D 3 is in much lower concentration than 25 (OH) D 3 and also mainly bound to VDBP in the blood. The concentration in particular of free 1,25 (OH) 2 D 3 is strictly regulated and largely correlated with its activity. It is also largely independent of the concentration of its precursor 25 (OH) vitamin D 3 or the VDBP.
When calcitriol is taken as a drug, it is quickly absorbed in the small intestine .
Binding to the vitamin D receptor
In the cells of the target organs, 1,25 (OH) 2 D 3 or calcitriol acts like a steroid hormone: It is bound to an intracellular receptor protein, the vitamin D receptor (VDR), and transported into the cell nucleus . The effectiveness of vitamin D is therefore also dependent on the receptor density, which is regulated differently in different tissues. In the cell nucleus, the vitamin-receptor complex associates with the DNA and changes the transcription of various vitamin D-sensitive genes , which ultimately leads to changes in protein synthesis with corresponding biological effects.
Role in calcium balance
First the connection between vitamin D and the calcium balance became known, since the most visible effects of a serious vitamin D deficiency are the bone diseases rickets and osteomalacia . With regard to calcium homeostasis , calcitriol has four target organs: the intestines , bones , kidneys, and parathyroid .
Calcium absorption in the intestine
Vitamin D is essential to enable the absorption of calcium and phosphate in the small intestine. Calcium is absorbed into the small intestine cell by two calcium channel proteins ( TRPV6 - formerly CaT1 or ECaC2 and TRPV5 - formerly called CaT2 or ECaC1), which may together form the functional calcium channel), transported by calbindin D through the cell and on the blood side through a membrane-bound one Ca 2+ -ATPase (PMCA1b) or a Na + / Ca 2+ -exchanger (NCX1) are released into the blood.
The initial calcium uptake is the speed-limiting step of the overall process and this is highly dependent on sufficient occurrence of the calcitriol-VDR complex, which induces the transcription of the calcium channels TRPV5 and TRPV6 in the intestinal cells. Calcium absorption in the intestine reaches a maximum from a 25 (OH) vitamin D 3 level of> 32 ng / ml in the blood (see cholecalciferol and).
Furthermore, 1,25 (OH) 2 D 3 increases the active phosphate absorption (uptake) by increasing the expression of the Na-P i cotransporter. The exact mechanisms of phosphate transport through the intestinal cells are less known.
Bone mineralization
The second important target organ for 1,25 (OH) 2 D 3 is the bone ; 1.25 (OH) 2 D 3 is essential for the development and maintenance of a healthy, mineralized skeleton .
Under normal conditions, bone tissue is subject to constant breakdown by osteoclasts and rebuilding by osteoblasts . The 1,25 (OH) 2 D 3 VDR complex, the parathyroid hormone and the calcium blood level work together in a complex manner. If one examines the effect of an isolated 1,25 (OH) 2 D 3 VDR complex deficiency in animal experiments, the following becomes apparent:
- The 1,25 (OH) 2 D 3 VDR complex isolated (with normal parathyroid hormone and calcium levels) is essential for normal, regulated bone formation and breakdown. So if you compensate for a parathyroid hormone excess occurring as a secondary occurrence in a 1,25 (OH) 2 D 3 VDR complex deficiency and a hypocalcemia and thus the actual effect of a 1,25 (OH) 2 D 3 VDR complex deficiency on the Unmasking the bone shows that the number of osteoblasts, calcium apposition rates and bone volume decrease.
- On the other hand, 1,25 (OH) 2 D 3 in the osteoblasts induces the formation of osteocalcin , which is activated post-translationally by the gamma-glutamyl carboxylase with the help of vitamin K and promotes the incorporation of calcium into the bones.
- In the same way, in the case of an isolated 1,25 (OH) 2 D 3 VDR complex deficiency, the bone loss by osteoclasts also decreases. The interaction between osteoblasts and osteoclasts is regulated as follows: osteoblasts form a ligand ( RANKL ) on their cell surface , which can bind to two different receptors: 1. to a soluble receptor osteoprotegerin (OPG), which is also formed in the osteoblast, or 2. to a receptor (RANK) on the surface of osteoclast progenitor cells. In the first case RANKL remains ineffective, in the second case it causes the osteoclast progenitor cells to mature into osteoclasts. 1,25 (OH) 2 D 3 -VDR complex in the osteoblasts increases the formation of RANKL and suppresses the formation of OPG and thus promotes bone resorption. This effect of the 1,25 (OH) 2 D 3 -VDR complex can be suppressed by vitamin K 1 .
- The apparent stimulation of bone mineralization by 1.25 (OH) 2 VitD 3 , which is given in the event of a vitamin D deficiency (e.g. rickets ), is only indirect 1. by the increased provision of calcium and phosphate due to the through 1,25 (OH) 2 D 3 increased absorption in the intestines and kidneys and 2. through the suppression of parathyroid hormone . If vitamin D is given in severe overdoses (then 25 (OH) Vit 3 gets the effectiveness of 1.25 (OH) 2 VitD 3 to a small but sufficient extent without being just as controllable by the body), the bone degradation is also evident Effect of vitamin D.
Parathyroid
The endocrine vitamin D system is a potent modulator of parathyroid function . Vitamin D deficiency leads to parathyroid hyperplasia and, via other mechanisms, to increased parathyroid hormone synthesis and excretion. 1,25 (OH) 2 D 3 can inhibit anything. The 1,25 (OH) 2 D 3 VDR complex suppresses, among other things, the transcription of the parathyroid hormone gene. 1,25 (OH) 2 D 3 itself induces the increased formation of its own VDR receptor in the parathyroid gland. The formation of parathyroid hormones is also indirectly suppressed by the increase in serum calcium (which is caused by the increased absorption of calcium by 1,25 (OH) 2 D 3 in the intestine and kidneys). Both effects complement each other and can stand up for each other.
The relationship between 1,25 (OH) 2 D 3 and the target organ parathyroid reciprocally total: parathyroid hormone stimulates the 1 α -hydroxylase in the kidney; In return, increased 1,25 (OH) 2 D 3 reduces the release of parathyroid hormone in the parathyroid gland.
kidney
The most important effect of 1,25 (OH) 2 D 3 on the kidneys is the strict control of its own homeostasis via the inhibition of its own formation via the 1 α -hydroxylase and the simultaneous stimulation of its deactivation by the 24-hydroxylase .
The direct role of 1,25 (OH) 2 D 3 in the kidney's handling of calcium and phosphate is not easy to explain because of the simultaneous effects of 1,25 (OH) 2 D 3 on serum parathyroid hormone and calcium blood levels and phosphate blood levels:
- 1,25 (OH) 2 D 3 increases the calcium reabsorption in the renal tubule by activating the transcription of the renal TRPV5 and calbindin (analogous to the #calcium uptake in the intestine ).
- 1,25 (OH) 2 D 3 accelerates the parathyroid hormone-dependent calcium reabsorption in the distal tubule (at the location of the highest VDR concentration).
- 1,25 (OH) 2 D 3 improves phosphate absorption in the presence of parathyroid hormone. This may not be a direct effect of 1.25 (OH) 2 D 3 .
Effects on other organs - empirically found higher mortality
An eight-year study at the University of Graz has empirically shown that there should be a correlation between calcitriol deficiency and overall mortality. The researchers found a - albeit not quantified - connection between a low vitamin D status and increased strokes, cancer and heart failure. The results found were also published in the US journal "Archives of Internal Medicine".
However, the above-mentioned study is not a recognized standardized procedure like the double-blind study. The above study does not yet provide scientifically useful evidence of the direct causality between low calcitriol values and the increasing number of diseases due to the low level.
In addition to the classic target organs, a large number of tissues and cells have been found that have the vitamin D receptor and 1 α -hydroxylase since the late 1980s . In the pancreas it influences the release of insulin , in certain parts of the brain it increases the activity of choline acetyltransferase , in muscles it has a direct effect on calcium transport, in the skin it inhibits the proliferation of keratocytes and promotes their differentiation. In addition, calcitriol promotes the formation of red blood cells and the survival and activity of macrophages and monocytes . It also inhibits the proliferation and activity of T lymphocytes and thus suppresses the immune system. It also has an inhibitory effect on cell proliferation in a wide variety of tumor cells. These different functions make it appear very important for different prevention considerations and should therefore be considered in more detail below:
Suppression of malignant cell growth
A protective role of UVB light and vitamin D for cancer is supported by a sometimes strong and consistent correlation between vitamin D deficiency and the (later) occurrence of 17 types of cancer estimated to date, including breast cancer , ovarian cancer , and non-Hodgkin's lymphoma , Colon and prostate cancer.
Physiologically, this can be explained as follows:
- 1,25 (OH) 2 D 3 induces the transcription of CDK inhibitor 1 and of p27, which inhibit the cyclin-dependent kinases and thus slows down the cell cycle by moving the cells from the G1 phase to the G0 phase and back leads to greater differentiation and maturation (e.g. in cells in the monocyte-macrophage series).
- In tumors whose growth is triggered by overexpression of an epidermal growth factor receptor ( EGFR ) activated by transforming growth factor (TGF-α) , 1,25 (OH) 2 D 3 inhibits this activated EGFR (which is in the same cell contributes to an increased transcription of oncogenic cyclin-1 , which drives cell proliferation). This can e.g. B. used in the treatment of psoriasis , because psoriatic keratinocytes overexpress TGF-α.
- In the monocytic cell line HL60 and in osteoblasts, 1,25 (OH) 2 D 3 induces the formation of C / EBPβ, a potent suppressor of oncogenic cyclin-1 in human epithelial cell tumors .
- Most of the anti-proliferation effects of 1,25 (OH) 2 D 3 are likely to be of an autocrine rather than endocrine nature. In prostate cancer cells the activity of the 1 drops α -hydroxylase with increasing malignancy .
- Various alleles of the gene for the vitamin D receptor (VDR) correlate with the genetic risk of cancer.
- At the beginning of August 2015, a research group at the UMG Institute for Human Genetics in Göttingen , together with colleagues from the Helmholtz Center in Munich, published the results of a study in which the causal relationship between calcitriol as an inhibitor of the Hedgehog signaling pathway was first demonstrated. They also examined potentiators and found the antimycotic itrakonazole to be potentially promising on cultivated cells.
Regulation of apoptosis
Vitamin D has pro-apoptotic and anti-apoptotic properties, depending on the cells and tissues. While it protects normal tissues from apoptosis under some conditions (e.g. skin cells under UV radiation), it has a proapoptotic effect on tumor tissue and in non-malignant proliferative diseases.
Modulation of the immune response
1,25 (OH) 2 D 3 (calcitriol) has differentiating effects on monocytes , macrophages , antigen-presenting cells, dendritic cells and lymphocytes . There is a causal relationship between the function of 1,25 (OH) 2 D 3 - VDR complex and the innate and adaptive immunity to infection: In a rickets and a 1,25 (OH) 2 D 3 deficiency in renal insufficiency is the susceptibility to infection usually increases. 1,25 (OH) 2 D 3 induces the formation of CDK inhibitor 1 and C / EBPβ . CDK inhibitor 1 can support the maturation of monocytes into mature macrophages and C / EBPβ is a transcription factor that is important for the immune functions of the macrophages (antibacterial, antiviral, antitumor functions and synthesis of interleukin-12 ).
In disease-activated macrophages, locally increased 1.25 (OH) 2 D 3 is converted from 25 (OH) D 3 . γ-interferon induces powerful transcription of 1 α -hydroxylase in macrophages and also the increased activation of 25 (OH) D 3 in 1,25 (OH) 2 D 3 . γ-interferon is e.g. B. increased in relation to the severity of tuberculosis . This can possibly explain why a deficiency of prohormone 25 (OH) D 3 (basically “lack of light”) with an increased susceptibility to e.g. B. tuberculosis is associated. In the presence of γ-interferon , the downregulation is 1 α -hydroxylase by their product 1,25 (OH) 2 D 3 is set in the macrophages suspended.
In contrast to the immune-stimulating effects on the monocyte-macrophage system, 1.25 (OH) 2 D 3 has an immunosuppressive effect on the lymphocytes : Various cytokines that influence T cell function are caused by 1.25 (OH) 2 D 3 , among other things, the formation of interleukin-2 is suppressed by the 1,25 (OH) 2 D 3 -VDR complex.
Dendritic cells are kept in a state of immaturity by 1,25 (OH) 2 D 3 , which plays an important role in immune tolerance , i.e. immunological self-tolerance.
1,25 (OH) 2 D 3 inhibits the development of some autoimmune diseases such as B. chronic inflammatory bowel disease , thyroiditis , insulin-dependent diabetes mellitus type 1, multiple sclerosis or systemic lupus erythematosus .
1,25 (OH) 2 D 3 also inhibits the rejection of transplanted tissue (in an animal experiment with experimental heart transplant rats with a higher potency than cyclosporin A, but without increasing the susceptibility to fungal or viral infections).
Control of differentiation and function in the skin
In normal keratinocytes , locally produced 1,25 (OH) 2 D 3 induces a number of proteins that are important for their further differentiation.
In psoriatic keratinocytes 1,25 (OH) 2 D 3 inhibits the mitogenic signals of the TGF-α / EGFR circuit and thus has an antiproliferative effect (see above).
On Langerhans cells , the antigen-presenting cells of the epidermis, 1,25 (OH) 2 D 3 has an immunosuppressive effect and can thus influence the course of melanoma and scleroderma .
Control of the renin-angiotensin system
The renin-angiotensin-aldosterone system plays a central role in the regulation of blood pressure , serum electrolytes and blood volume . An inhibition of the 1,25 (OH) 2 D 3 activity causes an activation of the renin . There is an epidemiological relationship between a lack of light or low 1,25 (OH) 2 D 3 blood levels and high blood pressure or increased renin activity.
Control of muscle function
A 25 (OH) D 3 deficiency in rickets , as a side effect of anticonvulsants or in chronic kidney disease is associated with muscle weakness and / or atrophy. In the heart muscle, 1,25 (OH) 2 D 3 controls the hypertrophy of the heart muscle cells and the synthesis and release of atrial natriuretic factor (ANF). In end-stage kidney disease, therapy with 25 (OH) D 3 or even 1.25 (OH) 2 D 3 can improve the function of the heart and muscles. The mechanisms of action are unclear.
Control of the nervous system
1.25 (OH) 2 D 3 increases the nerve conduction velocity in motor neurons . It induces the increased synthesis of neurotropic factors such as nerve growth factor in nerve cells and glial cells . In the embryo it influences the proper development of the brain. Low 1.25 (OH) 2 D 3 during pregnancy leads to increased brain volume, enlarged ventricles and reduced expression of nerve growth factor in newborn rats and to motor hyperactivity when they are adults.
Effects on the embryo during pregnancy
Women have less natural skin pigmentation than men, which makes it easier for them to produce vitamin D and meet the higher requirements during pregnancy and breastfeeding.
Vitamin D deficiency during pregnancy leads to an increased risk of intrauterine growth retardation, premature labor, high blood pressure and too light newborns (light for gestational age infants).
A sufficient supply of vitamin D to the mother and the newborn child considerably reduces the later risk of developing type 1 diabetes mellitus . This applies in particular to the supply of the mother with vitamin D in the 3rd to 6th centuries. Month of pregnancy, when the pancreas is developing. Children with type 1 diabetes mellitus have their birthday more often in summer.
There are similar assumptions for other illnesses with an accumulation in certain birthday months of the sick: bipolar depression , anxiety neuroses and other mental illnesses.
Calcitriol as a medicinal substance
- Indication : psoriasis (topical), vitamin D-dependent rickets , renal osteodystrophy , hypoparathyroidism
- Half-life : 5-8 hours
Veterinary aspects
Meadow golden oats ( Trisetum flavescens ) have a specialty in ruminants : they do not contain vitamin D (calciol alias cholecalciferol) as a precursor of the vitamin D hormone (calcitriol) that is actually active in the body, but rather calcitriol itself. Golden oat is a type of grass that occurs mainly in the alpine region, as this grass is more competitive here than high-quality grasses. Ruminants that have a good supply of grass select enough and therefore do not eat golden oats. The golden oats are only consumed in larger quantities when the supply is scarce, which leads to calcinosis : The animals become more immobile because more and more calcium is stored in the joints. It can also lead to hardening of the arteries and calcification of the lungs.
See also
- Cholecalciferol , this article describes the path of the calcitriol precursors (light, food, metabolism).
Trade names
Typical monopreparations : Calcijex (A), Decostriol (D), Osteotriol (D), Rocaltrol (D, A, CH), Silkis (D, CH).
Web links
- Compound - C01673 in the Kyoto Encyclopedia of Genes and Genomes
- Vitamin D (English)
Individual evidence
- ↑ a b Entry on calcitriol in the ChemIDplus database of the United States National Library of Medicine (NLM)
- ↑ a b Calcitriol data sheet from Sigma-Aldrich , accessed on March 15, 2011 ( PDF ).
- ↑ MF Holick, HK Schnoes, HF Deluca, T Suda, RJ Cousins: Isolation and identification of 1,25-dihydroxycholecalciferol. A metabolite of vitamin D active in intestine . In: Biochemistry . 10, No. 14, 1971, pp. 2799-804. doi : 10.1021 / bi00790a023 . PMID 4326883 .
- ↑ AA Çerman, SS Solak, Altunay, NA Küçükü: Topical Calcipotriol Therapy for Mild-to-Moderate Alopecia Areata: A Retrospective Study. In: Journal of Drugs in Dermatology . Volume 14, Number 6, June 2015, pp. 616-620, PMID 26091388 .
- ↑ Martin Blomberg Jensen, Steen Dissing: Non-genomic effects of vitamin D in human spermatozoa . In: Steroids . 77, No. 10, August 2012, pp. 903-909. doi : 10.1016 / j.steroids.2012.02.020 . PMID 22414629 .
- ↑ a b c d e f g h i j k l m n Adriana S. Dusso, Alex J. Brown, Eduardo Slatopolsky: Vitamin D . In: American Journal of Physiology-Renal Physiology . tape 289 , no. 1 , 2005, p. F8 – F28 , doi : 10.1152 / ajprenal.00336.2004 .
- ↑ Hoenderop, JG; Voets, T .; Hoefs, S .; Weidema, F .; Prenen, J .; Nilius, B .; Bindels, RJ (2003): Homo- and heterotetrameric architecture of the epithelial Ca2 + channels TRPV5 and TRPV6 . EMBO J. 22 (4): 776-785.
- ↑ Hollis, BW (2005): Circulating 25-hydroxyvitamin D levels Indicative of Vitamin D Sufficiency: Implications for Establishing a New Effective Dietary Intake Recommendation for Vitamin D . J Nutr 135: 317-322.
- ↑ SM Plaza, DW Lamson: Vitamin K2 in bone metabolism and osteoporosis. In: Alternative medicine review: a journal of clinical therapeutic. Volume 10, Number 1, March 2005, pp. 24-35, PMID 15771560 (review).
- ↑ Medical University of Graz: Connection between vitamin D deficiency and increased mortality has been proven ( Memento from February 17, 2011 in the Internet Archive )
- ↑ a b c d Grant, WB and Holick, FH (2005): Benefits and Requirements of Vitamin D for Optimal Health: A Review. (PDF; 268 kB) Alternative Medicine Review 10 (2): 94-111.
- ↑ Göttinger Tageblatt: Researchers from Göttingen have discovered other functions of vitamin D3 , August 6, 2015.
- ↑ Red List online, as of October 2009.
- ↑ AM comp. d. Switzerland, as of October 2009.
- ↑ AGES-PharmMed, as of October 2009.