West Nile Virus
| West Nile Virus | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|

West Nile Virus |
||||||||||||||||||
| Systematics | ||||||||||||||||||
|
||||||||||||||||||
| Taxonomic characteristics | ||||||||||||||||||
|
||||||||||||||||||
| Scientific name | ||||||||||||||||||
| West Nile virus | ||||||||||||||||||
| Short name | ||||||||||||||||||
| WNV | ||||||||||||||||||
| Left | ||||||||||||||||||
|
The West Nile virus ( scientifically West Nile virus , WNV ) is an enveloped RNA virus of the type ss (+) -RNA from the Flaviviridae family known since 1937 , which occurs in both tropical and temperate areas. The virus mainly infects birds , but can also spread to humans , horses and other mammals . WNV infection in humans is symptom-free in the majority of cases (approx. 80%). The clinical symptoms are called West Nile fever .
transmission
The virus is transmitted from one host to the next by mosquitoes . A large number of different species of mosquito, especially of the genera Culex , Aedes and Ochlerotatus, are possible carriers (or vectors ) . In terms of human medical significance, however, species that transmit the virus from their reservoir hosts (i.e. mostly birds) to humans (so-called bridge vectors) are particularly important. In the genus Culex , these are mainly species from the Culex pipiens complex ( Culex pipiens / molestus and Culex pipiens / quinquefasciatus ). Another possible bridge vector is the Asian tiger mosquito ( Aedes albopictus ). This spreads as a neozoon in Europe and stings both humans and birds.
In a study published in January 2006 in the Journal of Experimental Medicine , the assumption is made that a mutation in the CCR5 gene called CCR5Δ32 (CCR5-Delta32) massively increases a person's susceptibility to the West Nile virus. This assumption was confirmed in 2008 by a meta-analysis of the serum samples from cases of West Nile fever outbreaks in 2005 and 2006 in the USA. The linked with the gene mutation elimination of 32 base pairs causes also a limited resistance against at ordinary CCR5 receptors docking end HIV . Since its discovery in 1996, this mutation has therefore formed the basis for the development of new CCR5 fusion inhibitors in the fight against AIDS . No negative effects have been known to date. It has not yet been clarified whether the CCR5Δ32 mutation affects not only susceptibility but also the severity of the course of the disease after infection with the West Nile virus. The WNV binds to integrin β-3 .
West Nile fever
West Nile fever is an infectious disease caused by the West Nile virus that occurs mainly in birds but occasionally also in mammals (including humans ).
Clinical picture in humans
The majority of WNV infections are symptom-free . About 20 percent of those infected develop flu-like , febrile symptoms with an abrupt onset that lasts for about 3–6 days. The period between infection and the onset of symptoms is 2–14 days.
Only one in 150 infected people becomes seriously ill. Older and previously ill people are usually affected by the severe course . Meningitis occurs in only some of the seriously ill and is usually benign. In rare cases, encephalitis develops , which can lead to late effects (in 50% of encephalitis cases ), inflammation of the heart or inflammation of the liver .
West Nile fever usually heals without complications.
therapy
West Nile fever is treated symptomatically . There is no specific antiviral therapy. Isolation of the sick is not necessary. If the disease is severe, it makes sense to be monitored in the hospital in order to be able to react quickly if complications arise.
History and epidemiology
During periods of drought and hot weather, the spread can increase dramatically, as the lack of flushing in the sewer system and river beds means that there is more stagnant water, e.g. B. in the form of puddles, which are used by mosquitoes as breeding water. As a countermeasure, attempts are being made to control mosquitoes, which carry the virus, with pesticides . The use of insecticides in the cargo and passenger areas of intercontinental aircraft before landing has also increased significantly worldwide.
First record (1937)
The West Nile virus was isolated for the first time in 1937 in the West Nile District of Uganda in a sick elderly woman, hence the name. It appeared in Israel in 1957 and has continued to be found in horses in France and Egypt since 1960 .
In recent years there have been epidemic clusters of encephalitis caused by the West Nile virus in Algeria (1994), Romania (1996/97), the Czech Republic (1997), the Democratic Republic of the Congo (1998), Russia (1999) and Israel (2000) have been documented. It was detected in Hungary in 2004 and in Austria in 2008 .
USA (since 1999)
With the first appearance of the West Nile virus in North America in 1999, the topic moved into the media spotlight. In the United States, the virus outbreak began in the New York City area . The first signs were birds falling dead from the trees in Central Park . Soon afterwards, the elderly in the area became infected and fell ill. Deborah Asnis (1956–2015), a doctor from the New York Bronx with experience of the tropics, believed she recognized West Nile fever and contacted USAMRIID military researchers who were able to confirm the suspicion. It has since spread across the North American continent. In the United States, which continues to be hardest hit in North America, the virus reached the west coast in annual waves until 2004. Large regional outbreaks occurred particularly in the central states in 2002 and in the Rocky Mountain states in 2003. Between 2004 and 2011, many smaller and some larger regional outbreaks with strong fluctuations were recorded, with the number of cases being interpreted as tending to decrease. However, in 2012 there was again an unexpectedly large epidemic, which particularly affected Texas with almost 40% of all cases, especially in Dallas and the surrounding area. With 236 deaths, the epidemic is considered to be the one with the most deaths to date. In addition, about half of all cases were neuroinvasive.
Statistics USA
The Centers for Disease Control and Prevention has documented the following numbers for infections and deaths in humans since 1999:
| year | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Infections | 62 | 21st | 66 | 4156 | 9862 | 2539 | 3000 | 4269 | 3630 | 1356 | 720 | 1021 | 712 | 5674 | 2469 | 2205 | 2175 | 2149 | 2097 |
| dead | 7th | 2 | 10 | 284 | 264 | 100 | 119 | 177 | 124 | 44 | 32 | 57 | 43 | 286 | 119 | 97 | 146 | 106 | 146 |

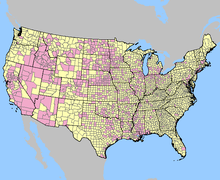
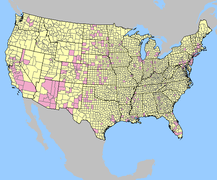
- Reported West Nile Virus Infections in the United States by Counties
Europe (since 1960)
According to the first evidence in Europe since 1960 ( see section above ), the virus caused a total of 33 deaths in 197 people in Greece in 2010 and reappeared in other parts of the country in the following year 2011. An increase in infections was also observed in Romania in 2010, with 5 deaths in 50 documented diseases. In July and August 2012, cases of West Nile fever reappeared in Greece. There were three fatalities, 44 other people fell ill.
2018
In 2018, the virus was able to spread again in some EU countries; in August, eleven deaths occurred within a week. In Serbia , 21 deaths have been confirmed since the beginning of the year, the authorities announced. There is a risk of infection there, especially in the capital Belgrade . In Greece , the number of people who died rose by 5 to 16 within a week, as the Keelpno authority told the ANA-MPA news agency. Most of the cases were recorded in the Peloponnese peninsula and in the rural areas around Athens and in the area around the port city of Thessaloniki. In Italy there were ten deaths between the beginning of June and August 23, according to the health authority Istituto Superiore di Sanità . The north and parts of Sardinia are particularly hard hit. A total of around 400 other infections were detected in the three countries.
In Italy, however, according to the health authority, the pathogen spreads to the nervous system in a relatively large number of patients . In total, 103 of the 255 confirmed infections were severe. For comparison, according to the Ansa news agency, only 55 infections were recorded in Italy in 2017, 27 with severe course. A person there died of the infection that year. 26 people died across Europe at the time.
In total, the EU health authority registered more than 1,460 human infections across Europe by the end of October 2018, at least 170 people died (all of 2017: 200 infections, 25 deaths); In addition, the pathogen was detected in birds and horses for the first time in Germany in 2018 ( see following section ).
2019
Since the start of the 2019 broadcast season, 33 human cases have been reported in EU member states. Three of them with fatal outcome. For the first time a case became known in France. Three cases have been reported in horses in the same area. In neighboring EU countries, no infections were known until they became known in Germany in September 2019.
Germany (since 2018)
2018
In Germany, the virus was first detected at the end of August 2018 in three bearded owls from an aviary in the Halle (Saale) zoo , one of which did not survive the infection. After the virus was detected, experts began collecting mosquitoes there. According to the Friedrich Loeffler Institute, mosquito traps with attractants were set up and water surfaces were searched for eggs and mosquito larvae. In Bavaria, the West Nile virus was detected in mid-September 2018 - also in a dead great gray owl - in a wildlife park in Poing in the Upper Bavarian district of Ebersberg . The virus was also detected in a goshawk kept in Bad Düben ( Saxony ) in mid-September 2018, as well as in a snowy owl and several thrushes in Berlin . In Plessa ( Brandenburg ), the virus was discovered in several horses in mid-September 2018 and in the Rostock district ( Mecklenburg-Western Pomerania ) at the end of September 2018 in a dead thrush. The probability of being infected as a person in Germany is low. The Federal Ministry of Health considers it possible that the West Nile virus will occur seasonally in humans in Germany in the future (as of 2018).
2019
In the summer of 2019, the virus was repeatedly detected in various birds and horses in the eastern federal states; two sick horses were also detected in Bavaria in September 2019. At the end of September 2019, the first case of a human infection acquired in Germany became known. "Apparently the unusually warm summers of the last two years caused by climate change have contributed to the West Nile virus establishing itself north of the Alps," said Jonas Schmidt-Chanasit, head of virus diagnostics at the Bernhard Nocht Institute .
Reporting requirement
The occurrence of birds or horses is a notifiable animal disease in Germany . Since 2016, according to Section 7 of the German Infection Protection Act , direct or indirect pathogen detection in humans has to be reported to the health department by name if the evidence indicates an acute infection.
In Austria, illnesses and deaths are subject to reporting.
In Switzerland, the positive laboratory analysis findings for is West Nile Virus a notifiable disease and that after the Epidemics Act (EpG) in connection with the epidemic Regulation and Annex 3 of the Regulation of EDI on the reporting of observations of communicable diseases of man .
Consequences for blood donation
West Nile virus can be transmitted through blood products that have not been virus- inactivated . In individual cases, a low virus concentration in the blood products is sufficient.
In order to prevent the pathogen from being transmitted via blood products, measures must be taken by the pharmaceutical company that extracts the blood product. Infected people are not allowed to donate blood . People who have returned from a risk area for the transmission of the WNV in the last 28 days must be deferred. Alternatively, the donated blood of such persons can be tested for the pathogen or a pathogen-inactivating measure can be carried out.
literature
- European Center for Disease Prevention and Control : Early large increase in West Nile virus infections in the EU / EEA and EU neighboring countries . - August 13, 2018, Stockholm, ECDC.
- 1st floor: The West Nile virus. In: Chemotherapy Journal. Volume 13, No. 4, 2004, pp. 166-173, ISSN 0940-6735 ( Wissenschaft-verlagsgesellschaft.de PDF).
- Helge Kampen: vector-borne infectious diseases on the rise? How environmental changes pave the way for disease carriers and pathogens . In: Naturwissenschaftliche Rundschau . Volume 58, No. 4, 2005, pp. 181-189, ISSN 0028-1050 .
- Hermann Feldmeier: Threat West Nile Virus . In: Naturwissenschaftliche Rundschau. Volume 58, No. 6, 2005, pp. 335-337, ISSN 0028-1050 .
- R. Zell, P. Wutzler: The West Nile virus. Institute for Virology and Antiviral Therapy, Friedrich Schiller University Clinic. 2004 ( PDF, 190 kB ( Memento from April 26, 2005 in the Internet Archive ))
- West Nile Virus - Statements of the Blood Working Group of the Federal Ministry of Health . In: Federal Health Gazette - Health Research - Health Protection . tape 55 , no. 8 . Springer-Verlag, August 2012, p. 1024-1043 , doi : 10.1007 / s00103-012-1507-2 ( online ).
Web links
- Richard L. Crawford, Kristina M. Adams: West Nile Virus Bibliography, 1965-2007. (No longer available online.) In: nal.usda.gov. US Department of Agriculture - Agricultural Research Service - National Agricultural Library - Animal Welfare Information Center, June 2007, archived from the original on February 25, 2015 .
Individual evidence
- ↑ ICTV Master Species List 2018b.v2 . MSL # 34, March 2019
- ↑ a b c d ICTV: ICTV Taxonomy history: Yellow fever virus , EC 51, Berlin, Germany, July 2019; Email ratification March 2020 (MSL # 35)
- ↑ a b FLI finds West Nile virus infection in a bird in Germany for the first time. In: fli.de. August 29, 2018. Retrieved August 30, 2018 .
- ↑ MJ Turell et al. (2005): An Update on the Potential of North American Mosquitoes (Diptera: Culicidae) to Transmit West Nile Virus. In: J Med Entomol Volume 42, No. 1, 2005, pp. 57-62.
- ↑ MS Godsey et al. (2005): West Nile Virus-infected Mosquitoes. Louisiana, 2002; In: Emerging Infectious Diseases . Volume 11, No. 9, 2005, pp. 1399-1404.
- ↑ Z. Hubalek & J. Halouzka (1999): West Nile Fever-a reemerging mosquito-borne viral disease in Europe . In: Emerging Infectious Diseases. Volume 5, No. 5, 1999, pp. 643-650.
- ^ NG Gratz (2004): Critical review of the vector status of "Aedes albopictus" . In: Med Vet Entomol. No. 18, 2004, pp. 215-227.
- ↑ Jean K. Lim, Christine Y. Louie, Carol Glaser, Cynthia Jean, Bernard Johnson, Hope Johnson, David H. McDermott, Philip M. Murphy: Genetic deficiency of chemokine receptor CCR5 is a strong risk factor for symptomatic West Nile virus infection : a meta-analysis of 4 cohorts in the US epidemic . In: The Journal of Infectious Diseases . tape 197 , no. 2 , January 15, 2008, ISSN 0022-1899 , p. 262-265 , doi : 10.1086 / 524691 , PMID 18179388 .
- ↑ a b c d e West Nile fever at a glance. In: rki.de. Robert Koch Institute, October 11, 2018, accessed on July 10, 2019 .
- ↑ a b Mark N. Frühwein: West Nile fever. In: apotheken-umschau.de. Wort & Bild Verlag Konradshöhe GmbH & Co. KG, October 15, 2018, accessed on July 10, 2019 .
- ↑ Philip M. Armstrong, Theodore G. Andreadis: Eastern Equine Encephalitis Virus - Old Enemy, New Threat. In: New England Journal of Medicine. Volume 368, Issue 18 of May 2, 2013, pp. 1670–1673.
- ^ West Nile Virus in Austria. (No longer available online.) In: wienerzeitung.at. Wiener Zeitung, February 13, 2009, archived from the original on August 9, 2016 ; Retrieved November 25, 2013 .
- ↑ Sam Roberts: Dr. Deborah Asnis, Who Sounded Alert on West Nile Virus Outbreak, Dies at 59. In: The New York Times . September 16, 2015, accessed on September 21, 2015 .
- ^ Lyle R. Petersen, Marc Fischer: Unpredictable and Difficult to Control - The Adolescence of West Nile Virus. In: New England Journal of Medicine. Volume 367, Issue 14 of October 4, 2012, pp. 1283-1285, doi: 10.1056 / NEJMp1210537 .
- ↑ Jatin M. Vyas, R. Gilberto González, Virginia M. Pierce: Case 15-2013 - A 76-Year-Old Man with Fever, Worsening Renal Function, and Altered Mental Status. In: New England Journal of Medicine. Volume 368, issue 20 of May 16, 2013, pp. 1919–1927, doi: 10.1056 / NEJMcpc1302330 .
- ↑ Wendy M. Chung: The 2012 West Nile Encephalitis Epidemic in Dallas, Texas. In: JAMA. Volume 310, 2013, p. 297, doi: 10.1001 / jama.2013.8267 .
- ^ A b West Nile Virus - Statistics & Maps. On: Centers for Disease Control and Prevention. Retrieved October 1, 2018.
- ↑ Kostas Danis, Anna Papa, George Theocharopoulos, Georgios Dougas, Maria Athanasiou, Marios Detsis, Agoritsa Baka, Theodoros Lytras, Kassiani Mellou, Stefanos Bonovas, Takis Panagiotopoulos: Outbreak of West Nile virus infection in Greece, 2010 . In: Emerging Infectious Diseases . tape 17 , no. 10 , 2011, ISSN 1080-6059 , p. 1868–1872 , doi : 10.3201 / eid1710.110525 , PMC 3310677 (free full text).
- ↑ K. Danis, A. Papa, E. Papanikolaou, G. Dougas, I. Terzaki, A. Baka, G. Vrioni, V. Kapsimali, A. Tsakris, A. Kansouzidou, S. Tsiodras, N. Vakalis, S. Bonovas, J. Kremastinou: Ongoing outbreak of West Nile virus infection in humans, Greece, July to August 2011 . In: Euro Surveillance: Bulletin Européen Sur Les Maladies Transmissibles = European Communicable Disease Bulletin . tape 16 , no. 34 , 2011, ISSN 1560-7917 , PMID 21903037 .
- Jump up ↑ Adriana M. Neghina, Raul Neghina: Reemergence of human infections with West Nile virus in Romania, 2010: an epidemiological study and brief review of the past situation . In: Vector Borne and Zoonotic Diseases (Larchmont, NY) . tape 11 , no. 9 , 2011, ISSN 1557-7759 , p. 1289-1292 , doi : 10.1089 / vbz.2010.0206 , PMID 21395408 .
- ↑ Doctors newspaper: Three dead: West Nile fever in Greece . In: www.aerztezeitung.de .
- ↑ Benedikt Theiler: Virus in Italy: West Nile fever is spreading in Europe. In: nau.ch . August 12, 2018. Retrieved August 13, 2018 .
- ^ A b c d West Nile fever: 47 deaths in Greece, Italy and Serbia - health. In: Spiegel Online . August 29, 2018. Retrieved August 30, 2018 .
- ^ A b Deutscher Ärzteverlag GmbH, editorial office of the Deutsches Ärzteblatt: West Nile Fever: Deaths in Greece, Italy and Serbia .
- ↑ John Palmisano, Karin Podolak: West Nile fever: Eleven cases of infection in Austria. In: krone.at. September 1, 2018, accessed September 1, 2018 .
- ↑ DLF 24 , West Nile Virus - Spread in Europe . In: Deutschlandfunk . ( deutschlandfunk.de [accessed November 4, 2018]).
- ↑ Weekly updates: 2019 West Nile virus transmission season. In: ecdc.europa.eu. European Center for Disease Prevention and Control, August 2, 2019, accessed on August 3, 2019 .
- ↑ Immediate notification report. REF OIE 27940, Report Date: 13/09/2018, Country: Germany. On: oie.int of September 13, 2018
- ↑ Deutscher Ärzteverlag GmbH, editorial office of Deutsches Ärzteblatt: Mosquito traps set up in Halle Zoo due to West Nile virus .
- ↑ West Nile virus detected in great gray owl in Bavaria. In: welt.de. September 13, 2018, accessed September 15, 2018 .
-
↑ Immediate notification report. REF OIE 28051, Report Date: 24/09/2018, Country: Germany. On: oie.int of September 24, 2018
West Nile virus detected in a hawk in Bad Düben. On: landkreis-nordsachsen.de from September 19, 2018 - ↑ Immediate notification report. REF OIE 28069, Report Date: 25/09/2018, Country: Germany. On: oie.int from September 25, 2018
- ↑ Immediate notification report. REF OIE 28071, Report Date: 25/09/2018, Country: Germany. On: oie.int from September 25, 2018
- ↑ Immediate notification report. REF OIE 28113, Report Date: 28/09/2018, Country: Germany. On: oie.int of September 28, 2018
- ↑ a b c d Ruth Offergeld, Karina Preußel: West-Nil-Virus - Amendment 2018 - Statements of the Blood Working Group of the Federal Ministry of Health . In: Federal Health Gazette - Health Research - Health Protection . Volume 62, Issue 4. Springer, Berlin / Heidelberg April 2019, p. 516–518 , doi : 10.1007 / s00103-019-02903-3 ( online [PDF; accessed July 10, 2019]).
-
↑ Friedrich-Loeffler-Institur: West Nile Virus. On: fli.de , accessed on September 17, 2019.
Daniela Albat: West Nile Virus : Wintered with us for the first time? On: scinexx.de from September 16, 2019 - ↑ Immediate notification report of the OIE of October 4, 2019, Report reference: WNV 2019 BY REF OIE 32017.
- ^ Robert Koch Institute: First mosquito-borne West Nile virus disease in humans in Germany. On: rki.de from September 27, 2019.
- ↑ West Nile virus was first transmitted from mosquitoes to humans in Germany. In: Spiegel Online . September 27, 2019, accessed September 27, 2019 .
- ↑ Animal Disease Report 2011 by the BMELV . In: Deutsches Tierärzteblatt. (DTBL) Volume 60, May 2012, pp. 714–715.
- ↑ Federal Law Gazette for the Republic of Austria, Part II, 224th Ordinance, August 13, 2015 .
- ↑ COMMISSION DIRECTIVE 2014/110 / EU . In: Official Journal of the European Union . Volume 57, December 20, 2014, ISSN 1977-0642 ( online [accessed July 10, 2019]).
- ↑ Ordering the use of an online database of the Paul Ehrlich Institute to exclude blood donations for the production of blood preparations by travelers after returning from endemic areas. (PDF) Paul Ehrlich Institute, August 31, 2018, accessed on July 10, 2019 .