electrocardiogram
The electrocardiogram ( EKG ) (in ancient Greek καρδία kardía , German 'heart' , and γράμμα grámma , German 'written' ) is the recording of the sum of the electrical activities of all heart muscle fibers using an electrocardiograph (also called EKG device ). The recording process is called electrocardiography . The electrocardiogram is also known as the heart voltage curve in German, and it is sometimes also called the heart writing .
Every contraction of the heart muscle is preceded by an electrical excitation, which normally comes from the sinus node . It runs to the other heart muscle cells via the heart's own electrical wiring system made up of specialized heart muscle cells. These electrical voltage changes in the heart can be measured on the body surface and recorded over time. The result is a recurring picture of the electrical heart action. The EKG can be used to make a variety of statements about the properties and health of the heart. It should be noted that the surface EKG only shows the electrical activity of the heart muscle, but does not reflect the actual ejection performance. Usually, the ECG is evaluated by increasingly reliable computer programs , which, however, does not make the doctor's assessment of the recording on paper or on the screen unnecessary.
history
In 1843 Carlo Matteucci realized through experiments on pigeon hearts that the heart's activity is based on electrical processes. In 1882 the physiologist Augustus Desiré Waller conducted an EKG on his dog Jimmy for the first time by dipping its four paws in conductive sodium chloride solution . In 1887 he was able to record heart currents for the first time with the help of a capillary electrometer.
The instruments were significantly improved in 1903 by Willem Einthoven , who, based on his string galvanometer, developed from 1895, developed the EKG into a useful diagnostic method and introduced it in the clinic. The terminology he introduced is still used today. At first he wanted to standardize on a single lead in which the patient dips both arms in separate solutions (Einthoven I). Since that was not enough, the other limb leads Einthoven II (right arm - left leg) and III (left arm - left leg) and later the Wilson leads on the chest wall (after Frank Norman Wilson , 1934) and the Goldberger leads ( according to Emanuel Goldberger , 1942), which are explained below.
Use
The EKG is a painless, non-invasive (non-invasive) examination method that can be repeated at any time and performed almost anywhere.
Heart rate , heart rhythm and the type of position ( electrical heart axis , see Cabrera circle ) can be determined from the EKG and the electrical activity of the auricles and ventricles can be read. The ECG is just as indispensable for diagnosing cardiac arrhythmias such as extra beats ( extrasystoles ) and disorders of conduction and propagation (e.g. bundle branch block and AV block ) as it is for detecting myocardial ischemia or a heart attack . Disturbances in the regression of excitation ( repolarization ) can lead to so-called chamber end changes (changes in the ST segment or the T wave). The activity of a pacemaker is represented as a very narrow, vertical line (spike) .
The ECG can also references to a thickening of the heart wall ( hypertrophy of the myocardium ), an abnormal load of the right or left heart, inflammation of the pericardium ( pericarditis ) or cardiac muscle ( myocarditis ) and electrolyte disturbances supply and adverse drug reactions.
With regard to most diagnoses, the ECG only provides information and must not be assessed independently of the clinical picture (e.g. myocardial infarction, signs of hypertrophy, myocarditis). Only in the case of disorders of the heart rhythm or the conduction of excitation can a clear diagnosis be made from the ECG alone.
Physical basics
Heart muscle cells have a negative membrane potential in the resting state (like all cells) , i. H. the outside of the membrane is positively charged while the inside is negatively charged. In the case of electrically excited cells, it is the other way round, here the extracellular space is negatively charged. The EKG measures voltages on the body surface that result from the charge distribution in the extracellular space; intracellular charges are not recorded. An extracellular voltage measurement between two points over the plasma membrane of a heart muscle cell would only result in an electrical voltage unequal to zero if the membrane is depolarized on exactly one of the two electrodes , because there is no potential difference between positive and positive or negative and negative .
To simplify the mathematical description, the charge distribution in this small part of the heart muscle should be idealized to the electrical dipole . The entire negative charge is thought to be concentrated on one point on the excited membrane section, while the entire positive charge is assigned to the non-excited section in the same way. The distance vector d from the negative to the positive charge multiplied by the charge q is then equal to the electric dipole moment vector p :
The equation applies to the electrical potential in the field of a dipole at distances r which by far exceed the distance between the charges
- .
The voltage thus exists between points A and B, which are at the same distance r from the center of the dipole (the vectors to the two points can still differ)
- .
The formation of the scalar product
can be understood as the projection of the vector p onto the straight line through A and B. Since all other quantities are constant over time, the key finding for understanding the EKG is that the measured voltage is proportional to the projected portion of the dipole moment:
Considering the entire heart of course, many of these dipole moments must be considered, however, the relationships described still apply when p by the sum of all the dipole moments P replaced. Instead of points A and B, leads are used in the practice of the EKG, the corresponding vectors of which can be read in the Cabrera circle . For example, lead I, measured between the right and left arms, includes a vector pointing horizontally to the left.
Conversely, the vector of the summed dipole moment can also be calculated from measured voltages . This requires at least three derivatives whose vectors are linearly independent , i.e. not all of them lie in one plane. The resulting representation of the EKG by an arrow rotating over time in 3D space and changing in length is called a vector EKG.
species

Resting ECG
The normal resting ECG is usually made while lying down. Since it only takes a few seconds, it can also be done well in emergencies. As a basic cardiological examination, it is the variant with the greatest informative value. Only intermittent cardiac arrhythmias (e.g. extrasystoles, salvos, nocturnal breaks) may not be recorded.
Long-term ECG
To record the long-term ECG (syn .: Holter Monitor or Holter for short ; named after its inventor Norman Jefferis Holter ), the patient usually carries a portable ECG device with him for 24, sometimes 48 or 72 hours. Usually two or three channels are continuously derived. It is primarily used for rhythm diagnosis and answers questions as to whether there is a continuous sinus rhythm and whether this is variable according to the physical load, whether there are pauses or bradycardias (e.g. temporary sinus bradycardia in sick sinus syndrome, AV blockages, bradycardic atrial fibrillation), or can be used to detect malignant cardiac arrhythmias (e.g. ventricular salvos or ventricular tachycardias). - This is to be distinguished from the event recorder , which is switched on and off by the patient during certain events. He saves the data. As with the Holter, the electrodes are stuck to the skin for several days; There are also implantable event recorders which can be left in place for several years and read out via magnetic coils.
Exercise ECG
In ergometry , the patient is usually stressed in a defined manner in accordance with the WHO scheme. This is used to determine the maximum level of exercise, as well as increases in blood pressure and heart rate during exercise. Furthermore, exercise-induced cardiac arrhythmias as well as arousal regression disorders can be provoked and documented. The stress ECG should be interrupted if the blood pressure rises too high, if there is no rise or fall in blood pressure, if there is angina pectoris , if the patient is generally exhausted ( dizziness , shortness of breath , pain in the legs, etc.) and if the maximum heart rate has been reached ( rule of thumb for calculation : [220 minus age in years] per minute). Blood pressure and heart rate should also be measured during a recovery phase.
Fetal EKG
The fetal electrocardiogram is a method rarely used in prenatal diagnosis for the prenatal analysis of the child's heart activity. After the rupture of the bladder, the ECG can be recorded directly from the scalp of the fetus via special electrodes or indirectly via the abdominal wall or rectum of the pregnant woman.
Telemetry
A telemetry (short message) is a monitoring facility in the hospital. Similar to the long-term EKG, the ambulatory patient has a mobile device with him, which does not record the EKG but sends it to a computer via radio. The data is continuously displayed there and analyzed automatically. According to adjustable specifications (alarm limits), the computer alerts the staff acoustically and visually. - Swimming telemetry (also called water telemetry), for example, must be distinguished from this. Here the cardiac actions are either stored discontinuously as with the Holter monitor or continuously sent to a central unit as with telemetry.
monitor
Similar to telemetry, a monitor monitors a patient lying down in the hospital. In contrast to the Tele, however, this device not only registers the EKG, but also a number of other parameters (blood pressure, oxygen saturation, body temperature and many more). The process is called monitoring .
Implantable heart monitor
The implantable heart monitor ( insertable cardiac monitor or implantable loop recorder , ILR) is an ECG device that monitors the heart rhythm 24 hours a day for up to three years and records irregularities. The stored ECG can provide information about whether fainting spells have a cardiac cause. The heart monitor is the size of a USB stick and is pushed through a small incision under the skin during routine surgery under local anesthesia.
Intracardiac ECG (mapping)
As part of an electrophysiological examination (abbreviated EPU), an intracardiac EKG is recorded using electrodes, which are usually advanced to the heart via a venous access (groin or arm). It is used to more precisely differentiate cardiac arrhythmias. This enables the examiner to create a precise electrical image of the heart. This creates a map of the heart, so to speak.
Esophageal EKG
Filtered bipolar transesophageal electrocardiographic recordings at the level of the left ventricle can be used as part of a cardiac resynchronization therapy to visualize interventricular conduction delays. Transesophageal leads at the level of the middle left atrium are useful for the differential diagnosis of arrhythmias. With carriers of atrial pacemakers and defibrillators, they enable the determination of interatrial conduction times, which can be used as the basis for an individual optimization of hemodynamic pacemaker parameters (AV intervals).
Smartphone / smartwatch ECG
A single-channel electrocardiogram is recorded via a sensor in a smartphone case or a smart watch and transferred to software. The ECG rhythm is displayed and the software detects the presence of atrial fibrillation and normal sinus rhythms. Such systems are intended for use by medical professionals, patients with known or suspected heart disease, and interested laypeople. The detection accuracy for atrial fibrillation is high.
Derivatives
Electrical voltages are always measured between two points, which in medicine are called dissipation points. Electrodes are stuck to the skin at these points and are connected to the EKG device via electrical measuring cables. The measured electrical potentials are called derivatives .
polarity
A distinction is made between bipolar and unipolar leads:
- With bipolar leads, the voltage is registered between two equal points on the body surface.
- In the case of unipolar leads, the measurement takes place between a different and an indifferent (almost potential constant) reference electrode (which is either implemented over a large area or is created by averaging several electrode voltages). Since there is practically nowhere a zero potential, it is often called semi-unipolar.
Defined derivatives
In cardiology, there are various agreements about where on the body one should derive the time-varying tensions of the heart.
- With Einthoven's bipolar lead , the change in electrical potential is measured using three electrodes, which are usually glued according to the traffic light scheme : right arm: red, left arm: yellow, left leg: green. The potentials are measured
- Einthoven I (right arm - left arm),
- Einthoven II (right arm - left leg) and
- Einthoven III (left arm - left leg).
- With the unipolar lead according to Goldberger , the three electrodes are located on the same body parts. The potentials are measured between two lead points connected as an indifferent electrode and the third, the different electrode. It surrender
- aVR (augmented voltage right) as potential against the electrode on the right arm,
- aVL (augmented voltage left) as potential against the electrode on the left arm and
- aVF (augmented voltage foot) as potential against the electrode on the left leg.
-
The Wilson unipolar chest wall leads use six or nine electrodes.
- Electrode V1 is placed in the 4th intercostal space (ICR) (under the 4th rib ) to the right of the breastbone ,
- V2 in the 4th intercostal space on the left sternal margin.
- V4 lies in the 5th ICR in the left medioclavicular line, i.e. halfway along the clavicle ,
- V3 lies between V2 and V4 (on the 5th left rib).
- V5 and V6 are each glued at the level of V4 (regardless of the intercostal space, the illustration "Chest wall leads according to Wilson" does not show this exactly), with V5 on the anterior and V6 on the middle left axillary line .
- These leads can be supplemented by leads V7 – V9, which are also all located in the 5th left intercostal space. V7 lies in the posterior axillary line, V8 in the scapular line and V9 in the paravertebral line.
The voltage against the interconnected electrodes according to Goldberger (unipolar) is measured by a resistor network, which thus become an indifferent electrode. These additional leads are often used when a high posterior infarction is suspected. The leads V3R1, 2, 3 to the right of V3 also serve as evidence of an exclusive posterior wall infarction.
- The Nehb lead is a bipolar chest lead that is used primarily for diagnosing posterior heart wall infarction . For these leads, three lead points N st (sternal attachment of the second right rib), N ap (5th ICR, left medioclavicular line) and N ax (5th ICR, posterior left axillary line) are used. The electrodes are bonded in the following sequence: red, green, yellow. This derivation shows the small heart triangle and is used to represent potential changes in the heart's posterior wall. From a technical point of view, it is just a shift of the Einthoven derivation points to the chest wall. The three Nehb's derivatives are
- Nehb D (for dorsal , originally Nehb's derivative I ): right arm - left arm
- Nehb A (for anterior , originally Nehb's derivative II ): right arm - left leg
- Nehb I (for inferior , originally Nehb's derivative III ): left arm - left leg
- The original names with Roman numerals should not be used in order to avoid confusion between Nehb's derivative I (Roman 1) and Nehb I ( uppercase i for inferior ).
This large number of different recordings is necessary in order to record currents in different directions and thus changes in different areas of the heart muscle. This is used to localize infarcts, conduction blocks and location types (see below). The chest wall leads V2-V6 point to the anterior wall, I and aVL to the side wall of the left ventricle and II, III, aVF to its posterior wall. In general, the right ventricle is rarely important. In addition to the standard leads, there are other additional leads, for example to diagnose right heart hypertrophy or a situs inversus with dextrocardia .
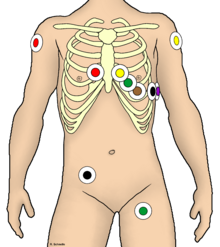
Correct electrode position is also important under the conditions of preclinical emergency medicine. For various reasons, the extremity electrodes cannot be attached completely distally , but rather in the proximal area of the extremities. To find the chest wall leads, it is recommended to feel the sternal angle (Angulus sterni or Ludovici, between the handle and the body of the sternum ), at the level of which the 2nd rib is attached. Below is the 2nd intercostal space.
Measures to minimize disturbance variables
- Electrical interference fields:
- As symmetrical as possible (measuring cable and conductor tracks close together and of the same length, use the same electrodes)
- Shielding of drainage cables ( coaxial cables )
- Galvanic separation of the control and operating unit from the (analog) measuring circuit
- High (4th or 5th) order bandpass filter in the signal path to suppress interfering frequencies
- Increase the distance between the source of interference and the measuring arrangement
- Shielding of the housing and the patient by a Faraday cage
- Magnetic interference fields:
- Twisting the test lead
- Shielding of the measuring lines with ferromagnetic material (steel pipe)
- Increase the distance between the source of interference and the measuring arrangement
- Change in patient position
- Electrodes:
- Exactly the same electrode impedances as possible
- Minimum electrode impedances through prior degreasing, scaling of the skin and large contact surfaces
- Fixation of the electrodes against movement (especially with ECG-triggered imaging)
- Electrode contact pressure as high as can reasonably be achieved
- Amplifier:
- High input resistance / impedance (> 10 8 Ohm), therefore a better useful signal compared to the interference component
- Low input capacitance (e.g. due to the connected cable) (<2000 pF), otherwise the input signal will be corrupted by the low-pass effect
- Specialized instrument amplifiers with very high common mode rejection
- Decoupling the patient from the medical device and its phase-related switching parts by means of galvanic separation has advantages:
- Increase in common mode rejection
- Increase in insulation resistance
- Reduction of patient leakage currents
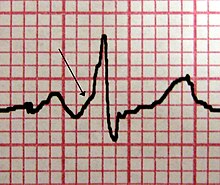
Nomenclature and standard values
The EKG is recorded on graph paper or electronically. The ( horizontal ) writing speed is usually 25 mm / s or 50 mm / s and the (vertical) deflection 10 mm / mV. At a feed rate of 50 mm / s, one millimeter, i.e. in the writing direction, corresponds to 0.02 s and 0.1 mV in height. Before recording, most devices output a calibration spike that corresponds to a deflection of 1 mV over 100 ms. In normal operation, this calibration prong is 1 cm high and 5 mm wide; at a writing speed of 25 mm / s, on the other hand, it is only 2.5 mm wide. The calibration spike thus serves as a reference for the following derivation and allows the device function to be checked ( calibration and adjustment ). In older manually operated devices, the calibration spikes were generated by pressing a button and applying a voltage of 1 mV, the duration of which was irrelevant. With these older devices, repeated pressing during the ECG registration showed which lead had been written, and the recorded curves were only labeled afterwards.
Name and meaning of the individual sections:
waves
P wave
The P wave corresponds to the atrial excitation. It usually arises from stimulation in the sinus node . The electrical stimulus spreads from the high right atrium towards the AV node. Normal configuration:
- Alignment: largely positive, also negative in III, aVR and V1, biphasic in right-precordial leads
- Duration: max. 100 ms
- Amplitude: 0.1-0.3 mV
If the electrical excitation does not arise in the area of the sinus node but, for example, caused by an extra blow in the atrial area (supraventricular extrasystole ), the configuration can differ significantly from the above. Usually there is also an atypical PQ time .
QRS complex
→ Main article: QRS complex .
The QRS complex (max. 100 ms) (without pathological change, values up to 120 ms can be found in up to 21% of the population) corresponds to ventricular excitation, with
- Q the first negative rash, with
- R is the first positive rash and with
- S denotes the negative deflection after the R wave.
T-wave
The T wave corresponds to the regression of excitation in the chambers. Since it runs from the apex of the heart to the base of the heart (and thus in the opposite direction of the ventricular excitation) due to the different conduction speeds in different ventricular regions, it generates a positive rash in the EKG. In children (except newborns) it is usually negative in the chest wall leads V1, V2 and V3 - and in 25% of the individuals in lead III.
In hypokalemia , the T waves flatten; in hyperkalaemia , they become high and pointed.
U-wave
The U-wave is a possible appearance after the T-wave; it corresponds to post-fluctuations in ventricular excitation regression, for example in the case of electrolyte disorders such. B. Hypokalemia.
Intervals
PQ interval
PQ interval or PQ time (max. 200 ms): Distance from the start of the P wave to the start of the Q wave, expression of the atrioventricular conduction time, i.e. the time between the start of excitation of the atria and the ventricles (excitation conduction time ). If there was no Q-wave, it is called a PR interval (or PR time).
QT interval
QT interval (or QT time) is the distance from the beginning of the Q wave to the end of the T wave. Its upper normal limit is variable because it decreases with increasing heart rate. The QT time describes the total intraventricular excitation time. The QT time is measured as an absolute QT time (standard values up to a maximum of 440 ms) and corrected mathematically using the heart rate.
ST segment
The ST segment is zero or isoelectric because both chambers are fully excited. It should not have a lift above 0.2 mV in two adjacent leads. Their starting point also defines the zero line in the ECG. Its end marks the beginning of the repolarization of the heart. A possible ST segment elevation indicates a lack of oxygen and an impending heart attack.
The ECG contains the name of the person examined with the date and time. Usually the values of the heart rate and the routes described above or computer-generated diagnoses are also printed.
Diagnosis
The diagnosis of the ECG produced during an electrocardiographic examination should be carried out according to a fixed scheme. An EKG ruler is helpful for interpretation .
Interpretation scheme (example)
rhythm
- Sinus rhythm: regular P waves present and P waves positive in leads II and III
- No P-waves or sawtooth-like atrial excitation
- regularly
- narrow chamber complex: e.g. B. atrial flutter or AV nodal reentry tachycardia
- wide chamber complex: e.g. B. Ventricular tachycardia
- irregular: atrial fibrillation
- regularly
frequency
- Normal 60 to 100 beats / min
- over 100 beats / min → tachycardia
- less than 60 beats / min → bradycardia
Reconciliation
The transition between atrium and ventricle
- in the event of a lengthening (PQ> 0.2 s) or failure of conduits, one speaks of AV blockage
Form of the chamber complex
- Incomplete bundle branch block with widening over 0.1 s, complete bundle branch block over 0.12 s?
- R-Loss or Q as a sign of past myocardial damage
- S in leads I, II, and III (S I S II S III -type) or S in I and Q in III (S I Q III -type) as a sign of acute right heart strain (e.g. as a pulmonary embolism )
Arousal regression
-
Signs of ischemia
- Heart attack? (ST segment elevation> 0.1 mV above the rear wall or> 0.2 mV above the front wall in two adjacent leads. Asphyxiation T)
- Angina pectoris (ST segment depression)
- Electrolyte imbalances
- QT interval duration, if prolonged there is a risk of malignant arrhythmias
Zero line
The zero line is also known as the permanent isoelectric line . It occurs when there is no potential difference between two recording points (no electrical activity of the heart) and therefore neither a positive nor a negative rash is recognizable. It is typical of asystole .
Location type
The position type describes the direction in which the electrical excitation propagates from the base of the heart to the apex relative to the body axis (electrical heart axis). On the one hand, it can provide information about the anatomical position of the heart in the chest, on the other hand, about asymmetrical thickening of the heart muscle in the case of chronic stress or as a sign of an increase in size in the case of acute stress (e.g. right-hand position type in an acute pulmonary embolism ).
Physiologically, there is a steep to a left type, with a steep type predominating in newborns. With increasing age, the electrical axis of the heart rotates to the left, so that older people usually have a left type.
The easiest and fastest way to determine the type of position is to look at the limb leads I and aVF. If both are positive, only physiological situation types can be considered and only in certain questions it is still relevant to differentiate them exactly from one another, which one still does in any case. For emergency diagnostics, however, this is a very helpful approach for the quick evaluation of an ECG. If I or aVF or even both are negative, either the ECG can be reversed, i.e. H. incorrectly applied, or more or less serious pathologies must be taken into account and the following scheme used to determine the exact location type.
With the help of the Cabrera circle , which is usually applied to every EKG ruler, as a picture in front of your eyes, you first look for the lead with the largest R-wave in the limb leads (Einthoven and Goldberger). For example, if this is the lead aVF, it is compared with the R waves of the leads adjacent to the Cabrera circle, in this case II and III. If derivative II is greater than III, there is a steep type, conversely a right type. Alternatively, you look for the vertical line to aVF, i.e. the I, and see whether this is positive or negative, if this is positive then it is again a steep type, otherwise a right type. In order to be able to include the derivative aVR in the determination of the location type, it is mirrored on the isoelectric line. Some ECGs independently record the resulting −aVR lead, but mostly only the R-wave is measured.
A very special, but not necessarily pathological case is the so-called sagittal type, which occurs when the electrical axis of the heart moves out of the normal frontal plane and begins to stand perpendicular to it. This is noticeable by S or Q waves in I, II and / or III, e.g. B. the so-called S1Q3 type or the S1S2S3 type. The method outlined above would also generate a classic type of position in this case, but this would be objectively incorrect, so such changes must be observed especially in the suspected area of a possible pulmonary embolism or in the case of right heart stress.
Arousal disorders
Atrial fibrillation
An atrial fibrillation can be recognized by an absolute arrhythmia of the chamber, the QRS complexes follow randomly varying intervals to each other. The P-wave is not present, instead one often sees a slight trembling of the baseline, which occasionally differs little from the normal, measurement-related trembling of the curve. With long-standing atrial fibrillation, the isoelectric line can also run smoothly.
Atrial flutter
In typical atrial flutter , leads II, III and aVF usually have a very characteristic sawtooth pattern of the baseline.
Conduction disorders
Atrioventricular block (AV block)
An AV block I ° (first degree) can be recognized by the extension of the PQ interval to over 0.2 s.
In the case of AV block II ° type 1 (also called Wenckebach or Mobitz I), the PQ interval becomes longer from time to time, then a QRS complex fails completely and another P wave follows, this time with a QRS complex . With AV block II ° type 2 (also called Mobitz or Mobitz II) (named after the cardiologist Woldemar Mobitz ), a QRS complex suddenly fails without the PQ interval becoming longer. If every second QRS complex fails, both Wenckebach and Mobitz blocks can be present.
With AV block III °, the atrial excitation (P wave) is not transferred to the ventricle. If it exists, a secondary pacemaker steps in in the area of the heart chamber ( AV node , bundle of His , if it is defective, Tawara thigh ). This alternate ventricular rhythm only has a rate around 40 beats per minute or slower. The patient's pulse is correspondingly low. The ECG shows regular P waves and, independently of this and much more slowly, relatively wide ventricular complexes.
Since an AV block II ° Mobitz can degenerate into an AV block III °, a supply with a pacemaker may be necessary. However, it depends on other factors, such as the occurrence of symptoms such as dizziness, etc., whether a pacemaker should actually be used. Endurance athletes are increasingly diagnosed with Grade I and II AV blockages (the latter very sporadically, often occurring at night), which are related to changes in the autonomic nervous system and only require regular follow-up checks, but do not result in any restrictions in sporting activity.
AV blocks III. The use of a pacemaker is essential.
Bundle branch block
A complete bundle branch block is used if the QRS complex duration is> 0.12 s; the block is incomplete if the QRS width is 0.1 to 0.12 s. It can, depending on the blocked bundle branch , right bundle branch block , left bundle branch block and left anterior and linksposteriorer hemiblock be distinguished.
Pre-excitation syndromes
If there is an additional electrical connection between the atria and ventricles next to the AV node, the ventricle can be prematurely excited. In the EKG there is a small positive wave (ramp-shaped upstroke) directly in front of the QRS complex, the so-called delta wave. An example of AV reentry tachycardia with pre-excitation is WPW syndrome .
Arousal regression
EKG signs of regression are the ST segment and the T wave and, if present, the U wave.
Heart attack
An extensive (transmural) acute myocardial infarction usually manifests itself in a horizontal ST elevation (ST elevation myocardial infarction, a myocardial infarction with ST elevation). Heart attacks without ST elevation are also possible, so-called non-transmural infarcts (or non-ST elevation myocardial infarction, NSTEMI ).
With the help of the EKG, the infarct can be localized. Leads I, aVL, V1–5 indicate the anterior wall, II, III and avF indicate the inferior wall. A corresponding ST depression appears in the leads that are not affected. In addition, the time course of the infarction can be determined, which shows typical changes in different stages.
Electrolyte imbalances
Hypercalcemia manifests itself in a shortened QT segment, hypocalcemia in a longer QT segment.
A hyperkalemia can (tent-shaped) increased T-wave and to shorten the QT interval lead. A hypokalemia may lead to an ST-segment depression with occurrence of a U-Wave, a QRS widening to a flattening of the T-wave and a prolongation of the QT interval (caution: Torsade de pointes ).
Medication
A whole range of drugs can alter the regression of arousal. Extensions of the QT duration (e.g. amiodarone ) are often associated with the risk of dangerous arrhythmias. Digitalis causes harmless trough-shaped ST segment subsidence.
QT syndrome
A frequency-corrected prolongation of the QT interval, the QT syndrome or long QT syndrome , can lead to threatening cardiac arrhythmias. The short QT syndrome , which is also associated with malignant arrhythmias, is much less common .
Heart size
Atrial hypertrophy
The atria are excited evenly and approximately radially via the working muscles, without a specific conduction system as in the heart chambers. The distance from the sinus node is decisive: the first part of the P wave reflects the activity of the right atrium, the second that of the left atrium.
- P-dextroatriale (= P-pulmonale): In the case of right atrial hypertrophy, the P-wave in II, III, aVF and V1 is increased over 0.20 mV and not broadened.
- P-sinistroatriale: With hypertrophy of the left atrium, the P-area (vector ÂP) increases proportionally to the atrial hypertrophy; Due to the lengthened conduction paths, however, the P duration (P width) is lengthened by 0.11 sec, the P wave often has double peaks (especially in I, II, V6), while the P height usually does not increase .
- P-biatriale: If both atria are affected, besides the elevation of the first part of the P-wave, there is a very pronounced P-wave lengthening and double peaks. In the chest wall leads V1 and V2, the angle α between the two P components becomes steeper (over 45 °) as the load on the right atrium increases.
The domains of the echocardiogram (USKG) are the measurement of the atrial dilatation and the diagnosis of masses, valve and septal defects. In contrast to the electroriogram (atrial EKG), no limit values for atrial hypertrophy can be specified for the USKG, nor for the volumetry of the right atrium.
Ventricular hypertrophy
The sign of the enlargement of the ventricles is the Sokolow-Lyon index . The Lewis index (left ventricular) and the Whitebock index (right ventricular hypertrophy) are less common .
Special features in children
Most of the normal values described above refer to adults. During the child's development, functional and structural changes occur in the heart. Normal ECG values in children and adolescents are generally to be assessed based on age. There are typical percentile curves for many norm values . The two most noticeable differences in children are heart rate and posture type. Children usually have significantly higher heart rates than adults. In newborns, a heart rate <100 beats / min is known as bradycardia . Due to the higher heart rate, the PQ interval, QRS width and QT time are shortened to different degrees compared to adults. While newborns still show a right type of position as a position type, in the course of development up to puberty this migrates further and further to the left until a position type normal for adults is reached (see above).
literature
- Marc Gertsch: The EKG . Springer, Berlin 2008, ISBN 978-3-540-79121-8 .
- Rainer Klinge: The electrocardiogram . Thieme, Stuttgart 2002, ISBN 3-13-554008-1 .
- Rainer Klinge, Sybille Klinge: Practice of EKG evaluation . Thieme, Stuttgart 2003, ISBN 3-13-596805-7 .
- Thomas Horacek: The EKG trainer: A didactically guided self-study course with 200 example EKGs . Thieme, Stuttgart 2007, ISBN 978-3-13-110832-6 .
- Hans-Peter Schuster, Hans-Joachim Trappe: EKG course for Isabel . Thieme, Stuttgart 2005, ISBN 3-13-127284-8 .
- Susanne Hahn: EKG. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. de Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 339 f.
Web links
- EKG - online
- Focus EKG
- Online basic course in ECG interpretation
- ECGpedia: EKG course and textbook
- Instructions for a 3-channel ECG with serial interface
- Historical outline of the Institute for Medical Ethics and the History of Medicine ( Ruhr University Bochum )
- A (not so) brief history of electrocardiography
- PysioBank - a free scientific database with physiologic signals (here ecg)
- EKG training
Individual evidence
- ^ Pschyrembel Clinical Dictionary. CD-ROM version 2002.
- ^ AD Krahn u. a .: Cost implications of testing strategy in patients with syncope: randomized assessment of syncope trial (RAST). In: J Am Coll Cardiol . 42 (3), 2003, pp. 495-501.
- ^ B. Ismer: Utilization of the Esophageal Left Heart Electrogram in Cardiac Resynchronization and AV Block Patients. Offenburg University, Offenburg 2013, ISBN 978-3-943301-08-3 .
- ^ Andrew RJ Mitchell, Pierre Le Page: Living with the handheld ECG . In: BMJ Innovations . tape 1 , no. 2 , April 1, 2015, ISSN 2055-8074 , p. 46–48 , doi : 10.1136 / bmjinnov-2014-000029 ( bmj.com [accessed September 23, 2018]).
- ↑ Deutscher Ärzteverlag GmbH, editorial office of Deutsches Ärzteblatt: EKG measuring device and fall detection built into the new Apple Watch . ( aerzteblatt.de [accessed on September 23, 2018]).
- ↑ AliveCor. Retrieved September 23, 2018 .
- ^ Feasibility of Using Mobile ECG Recording Technology to Detect Atrial Fibrillation in Low-Resource Settings . In: Global Heart . tape 12 , no. 4 , December 1, 2017, ISSN 2211-8160 , p. 285–289 , doi : 10.1016 / j.gheart.2016.12.003 ( sciencedirect.com [accessed September 23, 2018]).
- ^ DocCheck-Flexikon: P-wave .
- ↑ Th. Horacek: The EKG trainer. Thieme, 2003, ISBN 3-13-110831-2 .
- ^ Hans-Christian Pape, Armin Kurtz, Stefan Silbernagl: Physiology. 5th edition. Georg Thieme Verlag, Stuttgart 2007, p. 166.
- ↑ Keller / Wiskott (ed.): Textbook of paediatrics . 5th edition. Georg Thieme, Stuttgart / New York 1984, ISBN 3-13-358905-9 , pp. 22.5 .
- ^ Herbert Renz-Polster, Steffen Krautzig: Basic textbook internal medicine. 4th edition. Elsevier, 2008, ISBN 978-3-437-41055-0 .
- ^ A b F. Praetorius, G. Neuhaus: To assess the hemodynamic situation from the atrial electrocardiogram . Special print. In: Archive for Circulatory Research . tape 53 , 1967, p. 131–146 ( gmxhome.de [PDF; 338 kB ; accessed on September 23, 2010] English summary): “6. On the basis of electrophysiological considerations, the potential increase in P is interpreted as a consequence of the atrial hypertrophy itself "
- ↑ W. Voelker u. a .: Structured data set for documentation of findings in echocardiography - version 2004 . In: German Society for Cardiology - Heart and Circulatory Research e. V. on behalf of the Commission for Clinical Cardiology (Ed.): Zeitschrift für Kardiologie . tape 93 , December 13, 2004, p. 987–1004 , doi : 10.1007 / s00392-004-0182-1 ( dgk.org [PDF; 569 kB ; accessed on September 23, 2010] English summary).
- ↑ Roberto M. Lang u. a .: Recommendations for chamber quantification . In: European Society of Cardiology (Ed.): Eur J Echocardiography . tape 7 , no. 2 , February 17, 2006, p. 101 , doi : 10.1016 / j.euje.2005.12.014 (English, oxfordjournals.org [PDF; 3.2 MB ; retrieved on September 23, 2010] Free Full Text): “there is too little peer reviewed validated literature to recommend normal RA (right atrium) volumetric values at this time”
- ^ Rainer Klinge: The electrocardiogram . 7th edition. Thieme, Cologne 1997, ISBN 3-13-554007-3 , p. 161 ff .
- ↑ Angelika Lindinger, Thomas Paul (Hrsg.): EKG in children and adolescents: EKG basic information, cardiac arrhythmias, congenital heart defects in children, adolescents and adults . 7., completely revised. Edition. Thieme, Stuttgart 2015, ISBN 978-3-13-475807-8 .