Heart attack
| Classification according to ICD-10 | |
|---|---|
| I21 | Acute myocardial infarction |
| I22 | Recurrent myocardial infarction |
| ICD-10 online (WHO version 2019) | |

The heart attack or (more precisely) myocardial infarction , and coronary infarction , acute and is a life-threatening event due to a disease of the heart , moved or one of its tributaries in a coronary artery or is more concentrated. The abbreviations used in human medicine are HI, MI ( myocardial infarction ) or AMI ( acute myocardial infarction ).
It is a persistent circulatory disorder ( ischemia ) of parts of the heart muscle (myocardium), which in most cases is caused by blood clots in an arteriosclerotic constriction of a coronary artery . The main symptom of myocardial infarction is a sudden, persistent and usually severe pain in the chest area, which can radiate mainly to the left into the shoulders , arms , lower jaw , back and upper abdomen . It is often accompanied by sweats / cold sweats , nausea and possibly vomiting . In around 25% of all heart attacks, there are little or no symptoms (so-called silent heart attack). In the acute phase of a heart attack, dangerous cardiac arrhythmias often occur; even smaller infarcts often lead to sudden cardiac death via ventricular fibrillation . About 30% of all deaths from heart attacks occur before any lay assistance or medical therapy.
The article deals essentially with myocardial infarction in humans; Myocardial infarctions in animals are described separately at the end.
Epidemiology
Heart attack is one of the main causes of death in industrialized nations . The incidence in Austria / Germany is around 300 infarcts per 100,000 inhabitants (in Japan <100; Mediterranean, Switzerland, France <200; 300 to 400 in Scandinavia; 400 to 500 in England, Hungary), in Germany around 280,000 suffer every year People have a heart attack. According to the cause of death statistics from the Federal Statistical Office , over 49,000 people died in Germany in 2015 as a result of acute heart attacks. Acute myocardial infarction has therefore always been the second most common cause of death in Germany since 1998. Both the absolute number of deaths as a result of a heart attack and the relative frequency have been steadily declining in Germany for years (see table).
| year | absolute number | male | Female |
|---|---|---|---|
| 2000 | 67,282 | 36,458 | 30,824 |
| 2001 | 65,228 | 35,473 | 29,755 |
| 2002 | 64,218 | 34,907 | 29,311 |
| 2003 | 64,229 | 34,679 | 29,550 |
| 2004 | 61,736 | 33,348 | 28,388 |
| 2005 | 61,056 | 32,973 | 28,083 |
| 2006 | 59,938 | 32,471 | 27,467 |
| 2007 | 57,788 | 31,195 | 26,593 |
| 2008 | 56,775 | 30,559 | 26,216 |
| 2009 | 56,226 | 30,934 | 25,292 |
| 2010 | 55,541 | 30,651 | 24,890 |
| 2011 | 52,113 | 28,621 | 23,492 |
| 2012 | 52,516 | 28,951 | 23,565 |
| 2013 | 52,044 | 28,991 | 23,053 |
| 2014 | 48.181 | 27,188 | 20,993 |
| 2015 | 49.210 | 27,835 | 21,375 |
| 2016 | 48,669 | 28,130 | 20,539 |
| 2017 | 46,966 | 27,130 | 19,836 |
| 2018 | 46.207 | 26,884 | 19,323 |
Heart attacks are much more common in socially poorer parts of the city. In addition, in contrast to patients from more socially privileged districts, the patients from these neighborhoods are younger and have a higher risk of dying within a year of the heart attack.
Terminology and pathology
The understanding of heart attacks has changed fundamentally over the past thirty years. New diagnostic and therapeutic methods have contributed important findings to the pathophysiology, especially in the first hours after the onset of symptoms , and have changed the definition and terminology of myocardial infarction.
terminology
There is no definition of a heart attack that is valid in every situation. It is generally accepted that the term myocardial infarction describes the cell death of myocardial cells due to a prolonged circulatory disorder ( ischemia ). The more difficult question is which criteria are used for such cell death. The measuring instruments used differ considerably:
- Emergency services define the infarction based on symptoms and EKG changes,
- Intensive care physicians additionally with the help of laboratory tests ,
- Pathologists exclusively on the basis of macroscopic or, more rarely, microscopic tissue changes and
- Finally, epidemiologists mostly use more or less exact statistics on the cause of death (cf. after-the- fact examination ) or discharge diagnoses from hospitals.
In the case of chest pain that is typical of an infarct that lasts longer than 20 minutes, an acute coronary syndrome is initially spoken of, which includes the possibility of a heart attack. If an electrocardiogram (EKG) to be prepared as quickly as possible shows elevation of the ST segment (cf. EKG nomenclature ), the term ST elevation infarction ( STEMI for ST elevation myocardial infarction ) is used. In patients without such a ST elevation can only after three to four hours with the help of laboratory tests between non-ST-elevation myocardial infarction (abbr. NSTEMI for non-ST-elevation myocardial infarction ) and unstable angina are distinguished. While STEMI and NSTEMI are regarded as the final diagnoses in the guidelines for Germany, the US guidelines differentiate between Q-wave myocardial infarction (Qw MI) and non-Q-wave myocardial infarction (NQMI) as the final diagnosis. This distinction between transmural (affecting the entire thickness of the wall layer of the heart) and non-transmural myocardial infarction is also common in German-speaking countries and is made on the basis of changes in the QRS complex in the ECG, which usually only occurs after twelve hours, often also only after one day are recognizable.
Pathophysiology
The majority of heart attacks result from coronary heart disease (CHD). Like all acute coronary syndromes in humans, they are almost always caused by a sudden reduced blood flow in a coronary artery, which is due to an arteriosclerotic vascular change with additional blood clots ("coronary thrombosis") and can be accompanied by a convulsive constriction of the blood vessels (coronary spasm). The clinical picture that develops from this depends on the localization, severity and duration of the circulatory disorder of the heart muscle. In the acute stage of ST elevation myocardial infarction, over 90% of the patients have a coronary artery blocked by blood clots ( thrombi ) . With NSTEMI, thrombi in the coronary vessels are only detectable in about 50% of cases.
65–75% of ST elevation myocardial infarcts result from the rupture of a “vulnerable” plaque , ie the tear in the thin fibrous cap of an inflammatory, lipid- rich vascular wall change. About 75% of the infarcts occur in only slightly or moderately changed sections of the coronary vessels.
A heart attack is the result of another disease much less often. Occlusions of the coronary arteries due to other causes, such as long-lasting "cramps" ( spasms ) in the case of Prinzmetal's angina or in the context of an allergic reaction ( Kounis syndrome ) and embolisms in the case of endocarditis or disseminated intravascular coagulopathy (DIC) are possible . Bleeding or tumors in the heart as well as tears in the inner wall of the blood vessels ( intima ) during an aortic dissection can also lead to the closure of a coronary vessel and thus to a heart attack.
If its blood supply is completely cut off, the heart muscle begins to die after 15-30 minutes. This process of infarction begins inside, in the layer facing the heart chambers, and continues, depending on the time, outwards, towards the pericardium.
Infarct localization
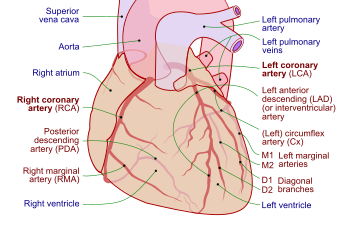
Heart attacks occur in different areas of the heart muscle, depending on which vessel is affected and which section of the heart muscle is supplied with blood by the respective vessel. Since there is great variability in the cardiac arteries, no strict rules can be established for the location of the infarct. Often occlusions of the right coronary artery (RCA - Right Coronary Artery) lead to so-called posterior wall infarcts and pathological changes in the left coronary artery (LCA - Left Coronary Artery) lead to anterior wall infarcts. The usual term posterior wall infarction is misleading insofar as it is mostly an inferior infarction, i.e. in a lower area facing the diaphragm (for strictly posterior infarction see below). The closer the occlusion is to the exit of the respective artery from the aorta (they say proximal), the larger the infarct area; the further away (they say distal), the smaller the under-supplied muscle area.
In detail, a distinction is made between proximal occlusions of the RCA, which lead to a right ventricular infarction or an inferior posterior wall infarction (at the apex of the heart) and processes in a branch of the RCA, the Ramus posterolateralis dexter, which lead to a posterior wall myocardial infarction. The classification is more complicated when the left cardiac artery (LCA) is affected, as it has more branches. The so-called main trunk of the LCA is very short and divides equally into the Ramus circumflexus (RCX) and the Ramus interventricularis anterior (RIVA). The RIVA is called LAD (Left Anterior Descending) in English-speaking countries. But also in German-speaking countries (for example in cardiac surgery) the term LAD is often used instead of RIVA. Occlusions of the RCX often lead to a posterior (back) posterior wall infarction. The posterior back wall infarction is called in the nomenclature of the pathologists sidewall or edge infarction. Proximal occlusions of the RIVA lead to a large anterior wall infarction, distal RIVA occlusions lead to an anteroseptal infarction; the heart septum is affected. A closure of the diagonal branch of the RIVA leads to a lateral infarction. The different types of infarction cause characteristic changes in the ECG. If, for example, one sees direct infarct signs (ST elevations) in all chest wall leads (V1-V6), it is a large anterior infarction (in relation to the vascular supply area). Then there is usually a proximal closure of the RIVA. The corresponding assignment based on the ECG is provisional and can only be proven by coronary angiography. Since the muscle mass and thus the supply area of the right ventricle is smaller than that of the left and consequently a longer vascular path is necessary for its blood flow, which can become diseased, the left coronary artery is statistically predominantly affected in heart attacks.
Risk factors
Since heart attacks are the result of atherosclerosis of the coronary arteries ( coronary artery disease ), the main risk factors are those that lead to atherosclerosis:
- Tobacco consumption ,
- Diabetes mellitus (diabetes)
- high blood pressure
- Hypercholesterolemia
- Family history (early onset of cardiovascular diseases such as infarction or stroke in close blood relatives )
- inherited or acquired lipid metabolism disorder . Higher LDL , increased IDL , low HDL and increased triglycerides are particularly problematic.
Some of the above-mentioned risk factors increase with overweight , malnutrition and lack of exercise . There is software such as the Arriba calculator for calculating the individual risk . Despite the tendency towards weight gain when quitting smoking, this reduces the risk of developing cardiovascular disease.
Stress and anger
The triggering factors for a heart attack can be sudden stress and stressful situations with strong blood pressure fluctuations; 40% of all heart attacks occur in the early morning hours (between 6 and 10 a.m.). Heart attacks occur more often on Mondays than on other days of the week, even among retirees over the age of 60.
In Japan, Karōshi describes "death from overwork", which usually occurs as a heart attack or stroke.
The proportion of psychosocial factors such as depression, anxiety, personality, character, social isolation and chronic stress in the development of CHD has been studied for decades without any clear results. Harmful behavior, stress, smoking, too much nutrition, etc. undoubtedly have an influence. The extent to which, for example, activation of blood platelets or the neuroendocrine system with the release of stress hormones with the consequences of constriction of the blood vessels, deterioration in the flow properties of the blood and an increase in heart rate and blood pressure has additional triggering qualities is discussed. A 2006 study at the time of the soccer World Cup showed that the emotions associated with soccer greatly increase the risk of a heart attack and that this is especially true for people who have known coronary artery disease. However, this finding is controversial in the scientific literature: A second study in the same time interval in the same region (Bavaria) could not prove any influence of the 2006 soccer World Cup on the risk of myocardial infarction.
Other emotional factors also contribute to the disease. It has been shown that habitual, poorly managed anger is a powerful predictor of heart attacks. Infarct patients who underwent anti-aggressiveness training suffered less frequently a second infarction than people in the comparison group under study conditions.
alcohol
Excessive alcohol consumption increases the risk of heart attacks and other serious illnesses. However, there is evidence that regular consumption of small and even more “moderate” amounts of alcohol reduces the risk of heart attack.
infection
An acute infectious disease increases the risk of a heart attack. As early as the 1920s it was recognized that the heart attack rate increased during an influenza epidemic. The same observation has been made with pneumonia, acute bronchitis and other respiratory infections. A more recent study found a six-fold increased risk of a heart attack after an influenza infection, a four -fold increased risk of a heart attack after an RSV infection and a three-fold increased risk of a heart attack after other virus-related respiratory diseases. An increase in the infarct rate has also been demonstrated for bacterial infections with pneumococci and Haemophilus influenzae. Urinary tract infections and bacterial chemistries also increase the risk of heart attacks. The explanation is believed to be that an atherosclerotic plaque contains numerous inflammatory cells. When infected, numerous cytokines such as IL1 , IL6 , IL8 and TNF-alpha are released . These stimulate the inflammatory cells in the atheroscleroic plaques and promote destabilization with subsequent thrombosis and occlusion.
Other risk factors
An increased blood level of homocysteine ( hyperhomocysteinemia ) is also an independent risk factor, but the available therapeutic approaches for lowering the homocysteine level do not lead to a reduction in the cardiovascular risk.
A low blood level of vitamin D3 (25-hydroxy-cholecalciferol) may also correlate with an increased risk of heart attack. In a prospective case-control study it could be shown that men with lower vitamin D3 levels had twice as high a risk of heart attack as those with higher ones. Men with medium levels of vitamin D3 (15.0–22.5 ng / ml) were evidently more at risk of infarction than those with higher levels. It was not investigated whether this is due to a deficient supply of vitamin D or a reduced conversion of 7-dehydrocholesterol or 25-hydroxy-cholecalciferol in the liver and skin, which could be due to a predisposition that is also responsible for myocardial infarction.
Poor compliance is a risk factor for disease progression. An analysis of the use of fat-lowering drugs ( statins ), beta blockers and calcium channel blockers after myocardial infarction showed that poor compliance resulted in an increase in mortality within 2.4 years for statins by 25% and for beta blockers by 13%. There was no relationship between mortality and collaboration with the calcium channel blockers.
Carriers of blood group AB are most at risk of heart attack, while those of group 0 are least likely.
Another risk factor is the presence of a migraine with aura . According to a study, this risk factor is the second most important risk factor for heart attack and stroke after arterial hypertension .
A tendency to allergies can also increase the risk of a cardiac event ( Kounis syndrome ).
Epidemiological studies on the economic crisis in Greece and on tropical storm Katrina in New Orleans also show that heart attacks occur more frequently after a crisis. This could either be due to a lack of medication or post-traumatic stress that people are exposed to.
The place of residence could also play a certain role. A new European cohort study shows that particulate matter pollution already below the EU limit values leads to a higher risk of a coronary event.
Clinical picture
Symptoms
Most patients complain of chest pain of varying degrees and quality. Typical is a strong feeling of pressure behind the breastbone ( retrosternal ) or a feeling of tightness in the whole chest (as if "someone was sitting on you"). Stinging or tearing pains are also described. The pain can radiate to the arms (more often on the left), neck, shoulder, upper abdomen, and back. Often one speaks of a " pain of destruction " which is accompanied by shortness of breath , nausea and a feeling of fear ("fear of death").
In contrast to the angina pectoris attack, these symptoms often do not improve with the use of nitroglycerin .
Women and older patients show atypical, more diffuse symptoms more frequently than men or younger patients; Often it is shortness of breath, weakness, upset stomach and physical exhaustion. Exhaustion, sleep disturbances and shortness of breath were mentioned as frequently occurring symptoms, which can occur up to a month before the actual heart attack event. Chest pain may be less predictive in women than in men.
Some heart attacks cause no, few or atypical symptoms and are sometimes diagnosed at a later point in time, e. B. on the occasion of an EKG examination. For example, some of the infarcts diagnosed in the 30 years of the Framingham study were only detected on the basis of the routinely prepared ECG; almost half of them were without symptoms (“silent” or “silent” infarcts). The proportion of unnoticed heart attacks was higher in women (35%) than in men (28%).
Of the more than 430,000 patients enrolled in the National Registry of Myocardial Infarction 2 in U.S. hospitals through 1998 , 33% had no chest pain at hospital admission. Among the patients without chest pain, there were more women, more elderly and more diabetics. Numerous silent infarcts are also not detected in the ECG examination, but they can be detected in the SPECT , especially in diabetics.
Clinical signs
The findings of the physical examination are variable, they range from normal findings in an unimpaired patient to an unconscious patient with cardiovascular arrest. There are no clear clinical signs of myocardial infarction, but typical is the overall impression of a patient suffering from pain with paleness, anxious facial expression, vomiting and a tendency to perspire.
Other findings already indicate complications that have occurred:
- Pulse irregularities on the extrasystoles common in infarction ,
- Pulse acceleration, when listening ( auscultation ) in addition to the two normal heart sounds and rattling noises over the lungs and jugular vein congestion on a pumping weakness of the heart ( heart failure ),
- Heart murmurs indicate mitral regurgitation , inflammation of the pericardium (pericarditis) or a rupture of the ventricle (rupture of the heart chamber) and
- Collapse, loss of consciousness and cardiovascular arrest to serious arrhythmias such as ventricular fibrillation , ventricular tachycardias or asystoles .
Technical findings
electrocardiogram
The most important examination method for suspected infarction is the EKG . In the acute stage, there are occasional increases in the T waves (see ECG nomenclature ) and frequent changes in the ST segment, with ST segment elevations indicating the complete occlusion of a coronary artery. In the further course, after about a day, there is often a "negativity" (rash below the so-called zero line) of T waves. Changes in the QRS complex in this phase indicate transmural infarction , a tissue destruction that affects all wall layers of the heart muscle. These QRS changes usually remain visible for life and are often referred to as "infarct scar".
The ECG is also of decisive importance for the detection and assessment of cardiac arrhythmias as frequent complications of a heart attack. In order to be able to recognize extrasystoles , ventricular fibrillation and AV blockages as quickly as possible in the acute phase and, if necessary, treat them, continuous ECG monitoring is carried out in the acute phase .
Following the acute phase, a stress ECG is used to assess the resilience and detection of persistent circulatory disorders of the heart muscle, and a long-term ECG to detect otherwise unnoticed cardiac arrhythmias.
Laboratory tests
So-called biomarkers are enzymes and other proteins that are released by dying heart muscle cells. They can be measured in increased concentrations in the blood after a heart attack.
The classic biomarkers, and until the early 1990s the only ones, are creatine kinase (CK), its isoenzyme CK-MB, aspartate aminotransferase (AST, mostly still abbreviated as GOT) and lactate dehydrogenase (LDH). Since then, myoglobin and troponin (troponin T and troponin I, often abbreviated as "trop") have been added. The newest biomarker is glycogen phosphorylase BB (GPBB). This biomarker is heart-specific and an early marker, but is currently (2013) not used clinically.
The measurement of the blood concentrations of these biomarkers is usually repeated at regular intervals, since the increase, the highest value and the decrease in the concentration allow conclusions to be drawn about the time of the start of the infarction, the size of the heart attack and the success of the therapy.
Imaging procedures
The ultrasound examination of the heart ( echocardiography ) shows a wall movement disorder in the affected heart muscle area during a heart attack. Since the extent of this wall movement disorder is very important for the prognosis of the patient, the examination is carried out in almost all infarct patients. In the acute phase, echocardiography provides important additional information in the event of diagnostic uncertainties and complications, because it helps to reliably assess the pump function and possible tears (ruptures) of the heart muscle, incompetence of the mitral valve ( mitral valve insufficiency ) and fluid accumulations in the pericardium ( pericardial effusion ).
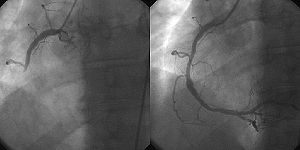
Vascular imaging ( angiography ) of the coronary arteries as part of a cardiac catheter examination allows the direct detection of occlusions and constrictions. It is either carried out as early as possible as an emergency examination in preparation for a PTCA (see reperfusion therapy ) or in the further course if there are indications of persistent circulatory disorders of the heart muscle. The high radiation exposure of up to 14.52 mSv can be a disadvantage. That is as much as 725 chest x-rays. Every year, billions of images are made worldwide using radiation technology - around a third of these images in patients with acute myocardial infarction. Between 1980 and 2006 the annual dose increased by an estimated 700%.
Diagnosis
Common and newer diagnostic methods
The diagnosis of myocardial infarction is made when one of the so-called "biomarkers" (preferably cardiac troponin , alternatively CK-MB ) in the blood is increased and at least one of the following criteria is met:
- typical EKG changes or
- typical chest pain or
- recent coronary artery intervention ( e.g. PTCA ).
The blood concentration of the biomarkers troponin and CK-MB does not rise until after three to six hours, so that a reliable diagnosis has previously only been possible after four to six hours.
According to the latest studies, a faster and more specific diagnosis can now be made promptly using the newly discovered heart marker glycogen phosphorylase BB (GPBB). GPBB can diagnose a heart attack from the first hour, so that the risk of irreversible damage to the heart tissue can be contained.
In this acute phase, the most important examination procedure is an EKG that is produced as quickly as possible . If there is evidence of ST segment elevation, an infarct is assumed with a diagnostic certainty of over 95% and the corresponding treatment is initiated as soon as possible.
If, on the other hand, the ECG shows lowering of the ST segment or no changes, an infarction can only be ruled out or confirmed with certainty based on the biomarker six hours after the onset of symptoms. If there is diagnostic uncertainty in this phase, the detection of a wall movement disorder in the echocardiography can help to better estimate the probability and the extent of a heart attack.
Differential diagnosis
Because of the potentially far-reaching consequences, the suspected diagnosis of myocardial infarction was often made earlier, in the acute situation the differential diagnoses pneumothorax , pulmonary embolism , aortic dissection , pulmonary edema of other causes, herpes zoster , stress cardiomyopathy , Roemheld syndrome , heart neurosis or biliary colic had to be considered. A heart attack was actually found in only about 32% of patients with suspected infarction. Today, the term infarct is mostly avoided until it is definitively proven and instead spoken of as acute coronary syndrome in order to express the frequent diagnostic uncertainty in the first few hours.
Infarct diagnostics are also subject to possible errors: in some patients (0.8% in one study), especially in older patients and those with diabetes mellitus , the infarct is not correctly recognized even in hospitals.
An unusual mix-up of symptoms was observed in a (rather rare) case of consumption of honey from the Turkish Black Sea coast (see honey # Toxins in honey and poisonous honeys ).
therapy
First aid
The first minutes and hours of a heart attack are crucial for the patient.
Within the first hour (the so-called golden hour or golden hour ) are good prospects, the vascular occlusion by thrombolytic therapy or cardiac catheter treatment to make almost completely reversed. Therefore, the immediate alerting of the rescue service is the top priority for laypersons. The German Heart Foundation recommends for this situation:
- Do not wait.
- Alert the ambulance service by calling 112 (in Europe) or another local emergency number and expressing suspicion of a heart attack.
- Never drive to the clinic yourself because of the risk of collapsing while driving.
The risk of cardiac arrest due to ventricular fibrillation is greatest in the first hour. In this case, death or severe damage due to insufficient oxygen supply to the brain can only be prevented by rapid cardiopulmonary resuscitation by first aiders and rescue services . By a defibrillation by medical personnel or by means of a publicly available automated external defibrillator , which can be operated by laymen, there is a possibility that the fibrillation is stopped and again adjusts a stable intrinsic rhythm.
Medical first aid
The rescue personnel of the rescue service will initially focus on the earliest possible detection of acute hazards and complications. This includes a quick clinical examination with blood pressure measurement and auscultation (listening) to the heart and lungs. Only a quickly produced twelve-channel ECG can identify the ST elevation myocardial infarction and allow the urgent lysis therapy or catheter treatment to be initiated. In order to be able to recognize cardiac arrhythmias immediately, continuous ECG monitoring (rhythm monitoring) is started and a peripheral indwelling cannula is placed to administer medication .
In acute situations, drug therapy aims at the best possible oxygen supply to the heart, pain relief and avoidance of further blood clots. As a rule, nitroglycerin spray or capsules are administered sublingually and morphine preparations , acetylsalicylic acid and clopidogrel as well as heparin are administered intravenously . According to the current guidelines of the ERC, oxygen (O 2 ) is only administered if the blood oxygen saturation is low . The general administration of oxygen is no longer recommended because of its potentially harmful effects.
In special situations and in the event of complications, additional medication may be necessary, for example benzodiazepines such as diazepam or midazolam for calming down ( sedation ), atropine for vagal reactions , antiemetics ( e.g. metoclopramide ) for nausea or vomiting , beta blockers for tachycardia despite freedom from pain and lack of signs of left heart failure ( for example, metoprolol ) and cardiogenic shock, the administration of catecholamines .
Reperfusion therapy
The primary goal of therapy in ST elevation myocardial infarction is the opening of the coronary artery affected and, in this situation, usually closed as quickly as possible . This restoration of blood flow in the infarct area is called reperfusion therapy. The earlier this occurs, the better the infarct can be prevented from spreading (“time is muscle”). If reperfusion therapy can be used in the first hour after the onset of the infarction, many of these infarcts can even be prevented.
Two treatment methods are established as reperfusion therapy:
- Primary percutaneous coronary intervention (also direct PTCA or primary PTCA): mechanical opening ( recanalization ) of the vessel with subsequent balloon dilatation and stent implantation using a cardiac catheter. If a finding that cannot be approached by PTCA is found, acute operative myocardial revascularization may be indicated in individual cases .
- Lysis therapy or thrombolysis : intravenous administration of a clot-dissolving drug. This thrombolytic agent can be administered by the emergency physician on site ( pre-inpatient lysis ) and leads to better results by starting treatment early than initiating therapy in the hospital.
With simultaneous availability, primary PCI in an experienced center is the preferred strategy. However, since less than 20% of German hospitals have the option of primary PCI, the decision on the optimal therapy must be made on a case-by-case basis. Many emergency doctors are equipped with twelve-channel ECG devices and medication for lysis therapy, so that today they can select the best possible reperfusion therapy immediately after diagnosis, depending on the duration of the infarction, the patient's condition, the availability of an experienced cardiac catheter team and the transport distance.
In the case of non-ST elevation myocardial infarction (NSTEMI), the benefit of immediate reperfusion therapy has not been proven; lysis therapy is contraindicated . Whether and when a cardiac catheter examination is necessary is a matter of dispute despite many studies on this topic. The predominant recommendation, which is also anchored in the guidelines of the cardiological specialist societies, provides for an "early intervention" within 48 hours. New discussions arose from another study published in autumn 2005, which found no higher risk in 1200 patients with NSTEMI if the intervention was only carried out in patients with persistent symptoms.
Further treatment
In the hospital, heart attack patients are treated because of possible cardiac arrhythmias in the acute phase in an intensive care or monitoring ward , where continuous ECG monitoring is possible. If the course is uncomplicated, they can often be mobilized step by step the following day and discharged after five to eight days. Patients with large infarcts that have led to a pumping weakness ( heart failure ) of the heart muscle sometimes need up to three weeks to be able to resume normal everyday activities.
After a heart attack, lifelong drug therapy makes sense for most patients, which prevents complications such as cardiac arrhythmias and cardiac insufficiency as well as new heart attacks. This includes therapy with beta blockers , ASA , statins , ACE inhibitors and, in some patients, clopidogrel or prasugrel . In reality, however, it has been shown that drug therapy is often not implemented in accordance with the guidelines and that the affected patients are clearly under-supplied.
If the heart's pumping function is severely restricted, the prophylactic installation of an implantable defibrillator is recommended to protect against sudden cardiac death .
After the occurrence of large front wall infarcts, thrombi can form in the left ventricle (<50%) , which can lead to the risk of a cerebral infarction. If thrombi can be detected by echocardiography, anticoagulant therapy with phenprocoumon is usually carried out for several months .
Particular attention needs to be paid to the risk factors that can significantly affect the life expectancy of the heart attack patient. Strict abstinence from nicotine and an optimal setting of blood pressure, blood sugar and blood fat values are advantageous. In addition to the normalization of lifestyle, stress reduction and weight normalization, a healthy diet and regular physical endurance training as recommended by a doctor play an essential role.
Following hospital treatment, outpatient or inpatient follow-up treatment is often recommended in Germany . This usually lasting three-week measure aims of physiotherapy ( physical therapy ) allow, dosed physical training, training and psychosocial care as good as possible and complete reintegration into everyday life. Attending a heart school can be useful for a permanent lifestyle change .
Further therapy for coronary heart disease with coronary artery bypass or PTCA
In order to prevent further infarctions, the (often several) critical stenoses must be definitively treated by means of stent implantation or coronary artery bypass . The current guidelines of the European Cardiological Society on revascularization recommend that patients with a high surgical risk and one or two affected coronary arteries without involvement of the main left coronary trunk (or an equivalent proximal stenosis of the anterior interventricular branch) should be treated with PTCA. For all other patients, a higher-grade recommendation for surgical treatment with coronary artery bypasses applies. A procedure tailored to the individual patient is advocated, especially with regard to the accompanying diseases (such as hemodynamically relevant aneurysm, thoracic reoperation). Therapy planning and patient advice should be carried out by a "heart team", an interdisciplinary meeting of cardiologists and heart surgeons. Experience has shown that this is rather the exception in daily practice in Germany.
Experimental approaches
Since the 1990s, attempts have been made to use stem cells to positively influence the pumping function of the heart muscle after a heart attack . Various techniques are used, including the injection of stem cells obtained from blood or bone marrow into the affected coronary artery ( intracoronary , using a cardiac catheter). The subcutaneous injection of granulocyte-colony stimulating factor ( G-CSF ), which promotes stem cell production, is also being investigated. Several studies published between 2004 and 2006 indicate that the intracoronary use of bone marrow stem cells can actually improve the pump function, whereas the administration of G-CSF alone does not bring any benefit. However, a study from 2012 found no positive effect. Another therapeutic approach that has recently been pursued in preclinical studies is the use of growth factors such as fibroblast-like growth factors ( FGF- 1), insuline-like growth factors ( IGFs ) and vascular endothelial growth factors ( VEGF ), which stimulate the formation of new blood vessels ( angiogenesis) ) stimulate.
Course of the disease and prognosis
The first two hours after the onset of a heart attack are of decisive importance for the further course and the patient's chance of survival, at least in the case of an ST elevation myocardial infarction (STEMI), because
- The majority of deaths, usually caused by ventricular fibrillation , occur in this short period of time and
- a reperfusion therapy initiated during this time significantly influences the prognosis .
According to various studies, the acute mortality rate of those patients who are admitted to the hospital is between less than ten and almost twelve percent today. Furthermore, almost a third of all patients die before they are admitted to a clinic, so that the one-year mortality rate of all heart attack patients has remained almost unchanged at around 50% over the past 30 years.
The death rate associated with a heart attack is strongly influenced by the age of the patient. The Berlin myocardial infarction registry determined a hospital mortality rate of 23.9% for those over 75 years of age for the years 1999 to 2003, and 7.3% for younger patients. Overall, however, the rate of deaths after heart attacks has fallen sharply, as an epidemiological study with data from the WHO showed. Heart attack deaths have halved in Europe since 1980. In Germany it was 15–17% in 2009, in Austria 19–20% and in France 6–8%.
Complications
Cardiac arrhythmias are very common , even with small infarcts, especially in the early phase. Ventricular tachycardias through to ventricular fibrillation are the most common cause of death in heart attacks, which is why constant monitoring and defibrillation readiness is ensured in an intensive care unit in the acute phase . In individual cases, treatment with an antiarrhythmic is necessary. In particular, posterior wall infarcts can lead to AV block via ischemia of the AV node and to sick sinus syndrome with ischemia of the sinus node , which temporarily (or permanently) requires the use of a pacemaker .
If the infarct affects large areas of the heart (more than 30% of the muscles), cardiogenic shock can develop , in which the heart is no longer able to maintain adequate circulatory function due to the damage to the heart muscle. These patients have a significantly poorer prognosis; cardiogenic shock is the second most common cause of death in the context of an acute heart attack. An intra-aortic balloon pump (IABP) can temporarily support the heart.
A heart wall aneurysm can develop due to the weakness of the wall after a heart attack. A bulge develops in the damaged heart wall. Chronically, there is a deteriorated heart function, the formation of a thrombus due to impaired blood flow with the possibility of arterial embolism . In the direct phase after an infarction, the bulge may rupture (burst) with subsequent pericardial tamponade , which must be relieved immediately and generally treated surgically.
By necrosis in cardiac septal region may also be a septal come. Subsequently, blood passes from the left to the right part of the heart.
In the case of posterior wall infarcts, in particular, acute insufficiency of the mitral valve can occur due to necrosis of the papillary muscles with subsequent tearing of a tendon thread. The backflow of blood into the left atrium can lead to acute heart failure and require rapid heart surgery. A newly occurring systolic heart murmur can lead to this suspected diagnosis, therefore patients should be monitored ( auscultated ) regularly after a heart attack .
In the further course (a few days to approx. Eight weeks) an inflammation of the pericardium , the so-called Dressler's syndrome , can develop as part of an autoimmune reaction .
Infarcts in the elderly
| ≤ 75 years | > 75 years | |
|---|---|---|
| Heart failure | 3.5% | 14.4% |
| Renal failure | 3.9% | 11.5% |
| Diabetes mellitus | 24.3% | 37.3% |
| Pulmonary congestion | 19.7% | 45.4% |
| Left bundle branch block | 3.6% | 12.7% |
In European countries, around a third (24 to 42%) of all heart attacks affect people over the age of 74. This proportion will increase over time due to demographic developments. According to estimates, the proportion of people over the age of 75 will already be two thirds by 2050.
Older heart attack patients suffer more often from significant concomitant diseases such as heart failure , kidney failure and diabetes mellitus (diabetes). They are more likely to see signs of a severe infarction such as pulmonary congestion and left bundle branch block. The time between the onset of symptoms and admission to hospital is longer for them and, measured by the use of reperfusion therapy and the use of beta blockers and statins , a guideline-based therapy is used less often.
In addition, cardiac diseases such as heart attack also increase the risk of cognitive problems. In particular, women with heart disease suffer from mild, non-amnesic cognitive impairment in old age ( difficulty finding words , attention problems , disorientation, etc.).
history
From the beginning to 1950
It has been known since the beginning of the 19th century that a thrombosis in the coronary artery can lead to death. Animal experiments with ligation of a coronary vessel and dissection findings suggested that the coronary thrombosis was a fatal event. In May 1876 Adam Hammer in Vienna was the first to diagnose a heart attack in a living person. In 1901 the German Ludolf von Krehl proved that it was not always fatal; the first detailed description of non-fatal heart attacks comes from the Russians VP Obraztsov and ND Strazhesko in 1910.
In 1912 the American James B. Herrick referred to this publication and introduced physical rest as a therapy principle for heart attack patients. It remained the only treatment option until the early 1950s and was practiced consistently: The patients were not allowed to move for two weeks and should therefore be fed. It was also Herrick who introduced electrocardiography, developed in 1903 by the Dutchman Einthoven , for diagnosing myocardial infarction.
In 1923, Wearn published a description of the course of the disease in 19 patients with myocardial infarction who were prescribed absolute bed rest and restricted fluid intake. They received digitalis preparations against pulmonary congestion as well as caffeine and camphor to prevent and treat low blood pressure, syncope and cardiac arrhythmias. In 1928, Parkinson and Bedford described their experience of treating pain with morphine in 100 heart attack patients; they considered nitrates to be contraindicated because of their antihypertensive effect.
In 1929, Samuel A. Levine published the first specialist book devoted exclusively to the treatment of infarcts, in which, among other things, the importance of cardiac arrhythmias was discussed and quinidine was recommended for ventricular tachycardias and adrenaline for blockages .
In the 1950s, heart attacks were already seen as a major cause of death in industrialized countries. Because of the high risk of thrombosis and pulmonary embolism due to long bed rest, the concept of earlier mobilization ( arm chair treatment ) propagated by Bernard Lown gained in importance. Generous hydration and regular oxygenation were recommended.
The "Thrombolysis Era"
As early as 1948, it was recommended to take coumarins as an anticoagulant as a preventive measure after a heart attack . Mainly Fletcher and Verstraete demonstrated experimentally in the 1950s and 1960s that fresh coronary thromboses can be resolved with drugs. In 1959, the German Behring-Werke brought streptokinase onto the market, which, among other things, made lysis therapy possible for acute myocardial infarction. In the 1970s, it was two working groups headed by Yevgeny Tschasow and Klaus Peter Rentrop who provided evidence of successful lysis therapy using intracoronary infusion of streptokinase. Their results were supported by findings from De Wood , who found occluding coronary thrombi (occluding the vascular lumen) in 90% of patients with ST segment elevation. In the early 1980s it became clear that intravenous infusion was equivalent to intracoronary infusion, which greatly encouraged the spread of the method.
In 1986 the first randomized clinical study on lysis therapy, known as the GISSI study , was published. It was carried out on 11,806 patients and demonstrated a reduction in 21-day mortality from 13 to 10.7%, which corresponds to one human life saved per 43 treatments.
Further development of therapy
In 1960, the American Heart Association published the Framingham Study , which showed the link between smoking and the occurrence of heart attacks. In the mid-1990s, the balloon dilatation of the coronary arteries, introduced by Andreas Grüntzig in 1977, was also used on a larger scale as a therapy option for acute myocardial infarction. Today this is the treatment of choice and is used in more than 200,000 patients annually in Germany.
Myocardial infarction in animals
In contrast to humans, myocardial infarction is rarely observed in animals. In addition, in domestic animals, in contrast to the usually non-infectious etiology in humans, especially infectious -related endocarditis of the mitral valve with runoff of thrombi in the coronary arteries triggers of myocardial infarction.
In animals that reach old age even in human care, such as domestic dogs and parrots and zoo animals (e.g. Pacific walrus ), there are also isolated myocardial infarctions as a result of atherosclerotic changes as described in humans. A decreased oxygen supply to the heart muscle due to amyloidosis of the small heart arteries has also been observed in dogs . These - usually small - infarcts remain clinically mostly unnoticed and are found relatively often as local scarring of the myocardium as incidental findings in pathological examinations. In cats , infarcts seem to occur primarily as a complication of already existing heart muscle diseases ( hypertrophic cardiomyopathy ).
The increased susceptibility of the heart muscle of pigs to stress, on the other hand, is not due to insufficient blood flow, but is based on a massive and uncontrolled release of calcium within the muscle cell with muscle destruction ( porcine stress syndrome ).
literature
- German Society for Cardiology - Heart and Circulatory Research : AWMF Guideline 2019-2024: Heart attack-related cardiogenic shock - diagnosis, monitoring and therapy .
- European Society of Cardiology : ESC Clinical Practice Guidelines 2018: Fourth Universal Definition of Myocardial Infarction Guidelines .
- Douglas P. Zipes, Peter Libby, Robert O. Bonow, Douglas L. Mann, Gordon F. Tomaselli: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine , 11th Edition, Elsevier Health Sciences, Philadelphia 2019, ISBN 9780323555937 , preview Google Books .
- Herbert Reindell , Helmut Klepzig: diseases of the heart and blood vessels. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition, ibid. 1961, pp. 450-598, here: pp. 555-559 ( Der Herzinfarkt ).
Web links
- Heart attack - information at Gesundheitsinformation.de (online offer of the Institute for Quality and Efficiency in Healthcare )
- Test heart attack risk online - German Heart Foundation
Individual evidence
- ↑ Total deaths in 2011 according to the ten most common causes of death on the ICD-10 . Federal Office of Statistics. Retrieved January 17, 2013.
- ↑ Deaths (absolute, death rate, ranks, proportions) for the 10/20/50/100 most common causes of death (from 1998) Federal health reporting . Retrieved August 3, 2020.
- ^ German Heart Report 2010, Ernst Bruckenberger, ISBN 978-3-00-032101-6 , October 2010.
- ^ Hil: Bremen: More heart attacks in poorer parts of the city. In: aerzteblatt.de . September 4, 2013, accessed December 26, 2014 .
- ↑ a b F. van de Werf, D. Ardissino u. a .: Management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. In: European heart journal. Volume 24, Number 1, January 2003, pp. 28-66, PMID 12559937 .
- ↑ CW Hamm: Guidelines: Acute Coronary Syndrome (ACS) - Part 1: ACS without persistent ST elevation. In: Z Kardiol , 2004, 93, pp. 72–90, leitlinien.dgk.org (PDF)
- ↑ a b c Elliott M. Antman u. a .: ACC / AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology / American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction) . In: Journal of the American College of Cardiology . 44, August 4, 2004, pp. E1-E211. doi : 10.1016 / j.jacc.2004.07.014 . PMID 15358047 .
- ^ Gerd Herold and colleagues: Internal medicine. A lecture-oriented presentation. 2011, p. 247.
- ↑ Werner Böcker (Ed.): Pathology. 4th edition. Urban and Fischer, 2008, p. 479.
- ↑ C. Clair, NA Rigotti et al. a .: Association of smoking cessation and weight change with cardiovascular disease among adults with and without diabetes. In: JAMA. Volume 309, Number 10, March 2013, pp. 1014-1021, doi: 10.1001 / jama.2013.1644 . PMID 23483176 . PMC 3791107 (free full text).
- ↑ The studies in which emotional predictors could be demonstrated include e.g. For example, the following: Stephen Manuck, Frederick N. Garland: Coronary-Prone Behavior Pattern, Task Incentive, and Cardiovascular Response , Psychophysiology, Volume 16, Issue 2, March 1979, pp 136-142, doi: 10.1111 / j.1469 -8986.1979.tb01458.x .
- ^ A. Rozanski, JA Blumenthal, J. Kaplan: Impact of Psychological Factors on the Pathogenesis of Cardiovascular Disease and Implications for Therapy . In: circulation . 1999, pp. 2192-2217. PMID 10217662 .
- ↑ U. Wilbert-Lampen, D. Leistner, S. Greven, T. Pohl, S. Sper, C. Völker, D. Güthlin, A. Plasse, A. Knez, H. Küchenhoff, G. Steinbeck: Cardiovascular Events during World Cup Soccer . In: The New England Journal of Medicine . 358, No. 5, 2008, pp. 475-483. doi : 10.1056 / NEJMoa0707427 .
- ↑ D. Niederseer, CW Thaler a. a .: Watching soccer is not associated with an increase in cardiac events. In: International journal of cardiology. Volume 170, number 2, December 2013, pp. 189–194, doi: 10.1016 / j.ijcard.2013.10.066 . PMID 24182671 .
- ↑ G. Ironson, CB Taylor et al. a .: Effects of anger on left ventricular ejection fraction in coronary artery disease. In: The American journal of cardiology. Volume 70, Number 3, August 1992, pp. 281-285, PMID 1632389 .
- ^ Redford Williams: The Trusting Heart , New York: Times Books / Random House, 1989.
- ↑ Lyndra H. Powell: Emotional Arousal as a Predictor of Long-Term Mortality and Morbidity in Post MI Men , Circulation, Volume 82, Issue 4, Supplement III, October 1990
- ↑ MA Mittleman, M. Maclure u. a .: Triggering of acute myocardial infarction onset by episodes of anger. Determinants of Myocardial Infarction Onset Study Investigators. In: Circulation. Volume 92, Number 7, October 1995, pp. 1720-1725, PMID 7671353 .
- ↑ KJ Mukamal, CM Chen, SR Rao and RA Breslow: Alcohol consumption and cardiovascular mortality among US adults, 1987 to 2002 . In: Am Coll Cardiol . No. 55, 2010, pp. 1328-1335. doi : 10.1016 / j.jacc.2009.10.056 .
- ↑ SD Collins: Excess mortality from causes other than influenza and pneumonia during influenza epidemics. In: Public Health Rep (1896-1970) . tape 47 , 1932, p. 2159-2179 .
- ↑ Jeffrey C. Kwong, Kevin L. Schwartz, Michael A. Campitelli, Hannah Chung, Natasha S. Crowcroft: Acute Myocardial Infarction after Laboratory-Confirmed Influenza Infection . In: The New England Journal of Medicine . tape 378 , no. 4 , January 25, 2018, ISSN 1533-4406 , p. 345-353 , doi : 10.1056 / NEJMoa1702090 , PMID 29365305 .
- ↑ Julio Ramirez, Stefano Aliberti, Mehdi Mirsaeidi, Paula Peyrani, Giovanni Filardo: Acute myocardial infarction in hospitalized patients with community-acquired pneumonia . In: Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America . tape 47 , no. 2 , July 15, 2008, ISSN 1537-6591 , p. 182-187 , doi : 10.1086 / 589246 , PMID 18533841 .
- ↑ Liam Smeeth, Sara L Thomas, Andrew J Hall, Richard Hubbard, Paddy Farrington: Risk of myocardial infarction and stroke after acute infection or vaccination . In: The New England Journal of Medicine . tape 351 , no. 25 , December 16, 2004, ISSN 1533-4406 , p. 2611-2618 , doi : 10.1056 / NEJMoa041747 , PMID 15602021 .
- ^ Daniel M Musher, Michael S Abers, Vicente F Corrales-Medina: Acute Infection and Myocardial Infarction . In: New England Journal of Medicine . tape 380 , no. 2 , January 10, 2019, ISSN 0028-4793 , p. 171-176 , doi : 10.1056 / NEJMra1808137 .
- ↑ Cited, slightly modified, from E. Giovannuchi et al .: 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study . Arch Intern Med (2008) 168, 11: pp. 1174-1180, PMID 18541825 .
- ↑ Quoted after Poor compliance is fatal. MMW update Med. No. 5/2007 (Vol. 149), p. 22 and cited from JN Rasmussen et al .: JAMA, 297 (2007), pp. 177-186.
- ↑ Blood group influences the risk of myocardial infarction. In: welt.de . August 15, 2012, accessed December 26, 2014 .
- ↑ Meian He u. a .: ABO Blood Group and Risk of Coronary Heart Disease in Two Prospective Cohort Studies . In: Arteriosclerosis, Thrombosis, and Vascular Biology . August 14, 2012. doi : 10.1161 / ATVBAHA.112.248757 . PMID 22895671 . Retrieved June 8, 2013.
- ↑ rme: Migraines with aura as a risk of heart attack and thrombosis. In: aerzteblatt.de . January 16, 2013, accessed December 26, 2014 .
- ↑ Heart attack rates rise with plunging GDP in Greece's financial crisis
- ↑ Higher heart attack rates continue 6 years after Katrina
- ↑ Changes in heart attack timing continue years after hurricane
- ↑ PTSD linked to insulin resistance and metabolic syndrome, early markers of heart disease
- ↑ G. Cesaroni, F. Forastiere et al. a .: Long term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. In: BMJ. Volume 348, 2014, p. F7412, PMID 24452269 . PMC 3898420 (free full text).
- ↑ JG Canto, RJ Goldberg, MM Hand et al .: Symptom presentation of women with acute coronary syndromes: myth vs reality . In: Arch. Intern. Med. . 167, No. 22, December 2007, pp. 2405-2413. doi : 10.1001 / archinte.167.22.2405 . PMID 18071161 .
- ↑ M. Kosuge, K. Kimura, T. Ishikawa et al .: Differences between men and women in terms of clinical features of ST-segment elevation acute myocardial infarction . In: Circulation Journal . 70, No. 3, March 2006, pp. 222-226. doi : 10.1253 / circj.70.222 . PMID 16501283 .
- ↑ JC McSweeney, M. Cody, P. O'Sullivan, K. Elberson, DK Moser, BJ Garvin: Women's early warning symptoms of acute myocardial infarction . In: Circulation . 108, No. 21, 2003, pp. 2619-2623. doi : 10.1161 / 01.CIR.0000097116.29625.7C . PMID 14597589 .
- ^ WB Kannel : Silent myocardial ischemia and infarction: insights from the Framingham Study. In: Cardiology clinics. Volume 4, Number 4, November 1986, pp. 583-591, PMID 3779719 .
- ↑ JG Canto, MG Shlipak et al. a .: Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. In: JAMA. Volume 283, Number 24, June 2000, pp. 3223-3229, PMID 10866870 .
- ↑ N. Arenja, C. Mueller et al. a .: Prevalence, extent, and independent predictors of silent myocardial infarction. In: The American journal of medicine. Volume 126, Number 6, June 2013, pp. 515-522, doi: 10.1016 / j.amjmed.2012.11.028 . PMID 23597799 .
- ↑ a b D. Peetz, F. Post u. a .: Glycogen phosphorylase BB in acute coronary syndromes. In: Clinical chemistry and laboratory medicine: CCLM / FESCC. Volume 43, number 12, 2005, pp. 1351-1358, doi: 10.1515 / CCLM.2005.231 . PMID 16309372 .
- ↑ Prashant Kaul, Department of Cardiovascular Medicine, Duke University Medical Center, Durham and colleagues: Report at the 2009 AHA meeting.
- ↑ Quoted from Medical Tribune, November 27, 2009, p. 3.
- ↑ HR Arntz et al .: Guidelines for the diagnosis and treatment of acute myocardial infarction in the prehospital phase. Zeitschrift für Kardiologie (2000) 89: pp. 364-372, doi: 10.1007 / s100490070009 .
- ↑ Typical chest pain, but: heart attack was honey poisoning! cme.springer.de ( Memento from December 26, 2014 in the Internet Archive ) (PDF; 1.4 MB)
- ↑ German Heart Foundation: Heart attack - every minute counts! . online , accessed October 24, 2006.
- ↑ Guidelines of the European Resuscitation Council on cardiopulmonary resuscitation ( Memento of December 17, 2007 in the Internet Archive ) (PDF, English)
- ↑ H.-R. Arntz et al .: Initial Management of Patients with Acute Coronary Syndrome. Section 5 of the guidelines for resuscitation 2010 of the European Resuscitation Council, doi : 10.1007 / s10049-006-0794-2 .
- ^ The preclinical administration of oxygen part 1: The acute coronary syndrome (ACS). January 18, 2012, accessed February 16, 2012 .
- ^ RJ de Winter, F. Windhausen u. a .: Early invasive versus selectively invasive management for acute coronary syndromes. In: The New England Journal of Medicine . Volume 353, Number 11, September 2005, pp. 1095-1104, doi: 10.1056 / NEJMoa044259 . PMID 16162880 .
- ^ SC Smith, EJ Benjamin et al. a .: AHA / ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. In: Circulation. Volume 124, Number 22, November 2011, pp. 2458-2473, doi: 10.1161 / CIR.0b013e318235eb4d . PMID 22052934 .
- ↑ Sandra Mangiapane, Reinhard Busse: Prescription prevalence of secondary drug prevention and therapy persistence after myocardial infarction: A routine data analysis of the reality of care . In: Deutsches Ärzteblatt Int . tape 108 , no. 50 , December 16, 2011, p. 856–862 , doi : 10.3238 / arztebl.2011.0856 .
- ↑ Pocket guideline for acute coronary syndrome with persistent ST segment elevation (STEMI) . (PDF)
- ↑ W. Wijns et al. a .: Guidelines on myocardial revascularization. In: European heart journal. Volume 31, number 20, October 2010, pp. 2501-2555, doi: 10.1093 / eurheartj / ehq277 . PMID 20802248 .
- ↑ S. Janssens, C. Dubois et al. a .: Autologous bone marrow-derived stem-cell transfer in patients with ST-segment elevation myocardial infarction: double-blind, randomized controlled trial. In: Lancet. Volume 367, Number 9505, January 2006, pp. 113-121, doi: 10.1016 / S0140-6736 (05) 67861-0 . PMID 16413875 .
- ↑ D. Zohlnhöfer, I. Ott u. a .: Stem cell mobilization by granulocyte colony-stimulating factor in patients with acute myocardial infarction: a randomized controlled trial. In: JAMA. Volume 295, Number 9, March 2006, pp. 1003-1010, doi: 10.1001 / jama.295.9.1003 . PMID 16507801 .
- ↑ RS Ripa, E. Jørgensen et al. a .: Stem cell mobilization induced by subcutaneous granulocyte-colony stimulating factor to improve cardiac regeneration after acute ST-elevation myocardial infarction: result of the double-blind, randomized, placebo-controlled stem cells in myocardial infarction (STEMMI) trial. In: Circulation. Volume 113, Number 16, April 2006, pp. 1983-1992, doi: 10.1161 / CIRCULATIONAHA.105.610469 . PMID 16531621 .
- ^ J. Wöhrle, F. von Scheidt u. a .: Impact of cell number and microvascular obstruction in patients with bone-marrow derived cell therapy: final results from the randomized, double-blind, placebo controlled intracoronary stem cell therapy in patients with Acute Myocardial Infarction (SCAMI) trial. In: Clinical research in cardiology. Volume 102, Number 10, October 2013, pp. 765-770, doi: 10.1007 / s00392-013-0595-9 . PMID 23896972 .
- ↑ a b c J. Schuler, B. Maier u. a .: Present treatment of acute myocardial infarction in patients over 75 years - data from the Berlin Myocardial Infarction Registry (BHIR). In: Clinical research in cardiology. Volume 95, Number 7, July 2006, pp. 360-367, doi: 10.1007 / s00392-006-0393-8 . PMID 16741630 .
- ↑ M. Nichols, N. Townsend et al. a .: Trends in age-specific coronary heart disease mortality in the European Union over three decades: 1980-2009. In: European heart journal. Volume 34, number 39, October 2013, pp. 3017–3027, doi: 10.1093 / eurheartj / eht159 . PMID 23801825 . PMC 3796269 (free full text).
- ↑ RO Roberts, YE Geda et al. a .: Cardiac disease associated with increased risk of nonamnestic cognitive impairment: stronger effect on women. In: JAMA neurology. Volume 70, number 3, March 2013, pp. 374-382, doi: 10.1001 / jamaneurol.2013.607 . PMID 23358884 . PMC 3734560 (free full text).
- ^ JE Muller: Diagnosis of myocardial infarction: historical notes from the Soviet Union and the United States. In: The American journal of cardiology. Volume 40, Number 2, August 1977, pp. 269-271, PMID 327787 .
- ^ R. Sarmento-Leite, AM Krepsky, CA Gottschall: Acute myocardial infarction. One century of history. In: Arquivos brasileiros de cardiologia. Volume 77, Number 6, December 2001, pp. 593-610, PMID 11799435 .
- ↑ Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico (GISSI): Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. In: Lancet. Volume 1, Number 8478, February 1986, pp. 397-402, PMID 2868337 .
- ^ AD Gruber, M. Peters u. a .: Atherosclerosis with multifocal myocardial infarction in a Pacific walrus (Odobenus rosmarus divergens Illiger). In: Journal of zoo and wildlife medicine: official publication of the American Association of Zoo Veterinarians. Volume 33, Number 2, June 2002, pp. 139-144, PMID 12398303 .
- ↑ S. Driehuys, TJ Van Winkle, CD Sammarco, KJ Drobatz .: Myocardial infarction in dogs and cats: 37 cases (1985-1994). In: J. Am. Vet. Med. Assoc. , 1998, 213 (10), pp. 1444-1448, PMID 9828941 .