Prostate enlargement
| Classification according to ICD-10 | |
|---|---|
| N40 | Prostatic hyperplasia |
| ICD-10 online (WHO version 2019) | |
A benign enlargement of the prostate (prostate gland) - also known as benign prostatic hyperplasia ( BPH ) - results from the proliferation of otherwise normal cells . Earlier names are also prostate adenoma ( PA ) or falsely benign prostate hypertrophy .
BPH usually occurs in middle to elderly men. It is an enlargement of the prostate gland and parts of the intermediate tissue , which mostly starts from the so-called transition zone. A pathological significance does this benign gland enlargement only when accompanied by symptoms to (such. As nocturnal urination , urinary retention or weakened urine at the same time massively increased urination sdruck). The disease can be treated well using modern methods. If left untreated, however, the prostate can grow until it completely closes the bladder outlet. As a result of the occlusion, the kidney can no longer excrete (postrenal kidney failure), which leads to death from internal poisoning in uremia .
Although prostate cancer is also associated with enlargement of the prostate, BPH does not in itself represent an increased risk of prostate cancer.
Terminology
The term benign prostatic hyperplasia only describes the increase in volume of the prostate as such and not clinical findings or symptoms caused by it. The Anglicism Benign Prostatic Enlargement ( BPE ) is synonymous in the literature . If BPH leads to an increase in bladder outlet resistance, this is known as benign prostate obstruction ( BPO) or also with the English term bladder outlet obstruction (BOO) . If, for example, BPH is the cause of corresponding complaints when emptying the urinary bladder ( micturition ), the so-called symptoms of the lower urinary tract ( Lower Urinary Tract Symptoms , LUTS) , we speak of a benign prostate syndrome (BPS) . The outdated terms prostate adenoma carrier for symptom-free patients with BPH and prostate adenoma patients for patients with BPH can still be found in the literature today .
distribution
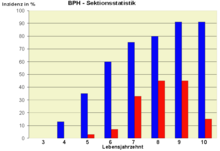
BPH is the most common benign tumor in men. It is very rare in the first few decades of man's life, but from the 6th decade onwards, 50% of all men have an enlarged prostate. The incidence of the disease increases to over 90% in the 9th decade of life. The risk of developing it is 10–20% in the 50 to 59 age group and 25–35% in the 60 to 69 age group. Due to its high incidence of disease, BPH is a widespread disease .
The occurrence of BPH is not limited to humans; it can also occur in (non-neutered) males . However, it does not play a role in other pets.
Cause and origin
→ For the anatomical structure, see main article: Prostate .
The urethra runs a little way through the prostate gland below the bladder. This consists of a left and right lobe as well as a part located behind the urethra, which is called the prostate isthmus or the middle lobe. BPH occurs when cells multiply in the so-called transition zone and the (periurethral) glands around the urethra. However, it is not only the gland cells that multiply, but also connective tissue and muscle cells - which is why the term prostate adenoma , which was used earlier, is technically incorrect. With a correspondingly pronounced enlargement, the peripheral zone of the prostate - it normally makes up three quarters of the organ mass - is pushed outward and stretched so far that it only surrounds the organ as a thin layer, the so-called surgical capsule, in the sectional view . The isthmus prostatee (lobe medius, middle lobe) can also bulge far into the interior of the bladder.
The weight of the prostate is usually around 20 to 25 grams. When BPH is present, the prostate weighs 30 to 150 grams. All in all, BPH represents an obstacle to the outflow of urine from the bladder (subvesical obstruction, i.e. below the urinary bladder). With normal micturition pressure (pressure that the bladder wall builds up to expel urine) the urine flow rate is reduced. A compensatory increased urination pressure can lead to a bladder bladder or autonomic detrusor contractions (Overactive Bladder, OAB). The enlarged central lobe that protrudes into the interior of the urinary bladder (hence also referred to as intravesically located in clinical parlance) is of additional importance and can obstruct the bladder outlet. This effect can occur regardless of the narrowing of the urethra below the bladder.
It has been known since the first half of the 20th century that the male sex hormone testosterone is essential for the development of BPH . Men who don't make testosterone won't develop BPH either. However, the exact cause is still the subject of scientific research. For example, the testosterone levels in the blood serum do not correlate with the development of BPH, especially since it is not testosterone but dihydrotestosterone that is the essential steroid of the prostate. This is also of particular importance as a growth factor for the prostate gland. It is formed in the gland through conversion from testosterone using 5-alpha reductase .
Clinical manifestations
The decisive factor for the disease value are symptoms , which initially mostly only affect the quality of life, and objectifiable pathological findings. In the further course, untreated BPH can lead to urinary retention and congestion of the urine drainage and associated damage to the kidneys and ultimately to death from uremia in the end stage .
Typical for BPH are irritation symptoms and voiding disorders when urinating ( micturition ). Typical irritation symptoms are pain when urinating, frequent, nocturnal and sudden urge to urinate - symptoms similar to cystitis . Emptying disorders are characterized by difficult, long-lasting urination supported by abdominal pressure. Symptoms include delayed start of micturition, a weak, often interrupted urine stream, prolonged micturition time, dribbling up to residual urine formation in the bladder.
According to Alken, BPH is divided into three stages:
- In stage I, also known as irritable stage is called, there are clinical symptoms such as a weak urine stream, dribbling after urination, frequent striking ( urinary frequency ), and nocturnal urination ( nocturia ). However, there is no residual urine formation. Even at this stage, urination problems can be a nuisance at work and in private life, and mental well-being and sexuality can also be considerably restricted. The symptoms can be so stressful that the men affected limit social contact as much as possible (social withdrawal behavior). A study by scientists from the University of Witten / Herdecke on 469 patients documented a clear connection between BPH-specific symptoms and health-related quality of life; Among other things, there was a significantly deteriorated general quality of life and a strong impairment of social activities, including sex life.
- In stage II (stage of compensated urinary retention ) the clinical symptoms increase and the residual urine volume is 50–100 ml, with a simultaneous decrease in functional bladder capacity .
- For stage III (stage of decompensated urinary retention ) urinary retention and overflow bladder (ischuria paradoxa) are typical. In addition, an increasingly can decreased renal function (up to uremia ) Stauungsnieren , bar bubble and bubbles pseudodiverticula occur.
examination
An enlargement of the prostate is felt during the digital rectal examination and, if necessary, can be measured by means of a rectal ultrasound examination. Symptoms can be objectified by means of a urodynamic examination , with a reduced urinary stream volume and relevant residual urine formation being typical. An obstruction of the urinary tract can, if necessary, be shown by means of ultrasound or urogram . The aim of the investigation is to find out to what extent the patient's symptoms are related to BPH. Furthermore, it is clarified whether there is a need for treatment and, if so , which form of therapy is the most suitable. If abnormal findings independent of BPH come to light ( screening ), such as an abnormal palpation finding, a PSA value above 4 or an unclear sonographic inhomogeneity of the gland, further examinations to rule out prostate cancer are indicated.
Medical history and physical examination
With appropriate complaints one is history with particular attention to voiding , hematuria (blood in the urine), previous surgery, urinary tract infection , diabetes mellitus , congestive heart failure , and pre-existing neurological diseases and medication (with respect to potentially miktionsbeeinflussender substances such as anticholinergics , psychotropics or antidepressants performed).
The psychological strain is usually classified using the international prostate symptom score (IPSS) . Zero to five points are awarded for seven symptoms: residual urine sensation, repeated urge to urinate two hours after the last visit to the toilet, stuttering urine, inability to delay urination, weak stream, pressure when urinating and frequency of nocturnal urination. Some questionnaires also ask a question about quality of life. According to this point system, patients are divided into those with mild (IPSS <8), moderate (8 ≤ IPSS ≤ 19) and severe (20 ≤ IPSS ≤ 35) symptoms. Therapy is usually started from a value greater than 7 and existing psychological stress.
The physical examination consists in particular of the rectal-digital palpation examination , in which not only the prostate is assessed, but also the anal sphincter tone (tension of the sphincter muscle of the anus) and the bulbo-cavernous reflex . In addition, an orienting motor and sensory status of the perineum, the genitals and the lower extremities is assessed.
Laboratory tests
The urine will be checked for blood and signs of a urinary tract infection . The PSA level in the blood is determined in particular with a view to largely excluding prostate cancer (below 4.0 ng / ml). In addition, the progression of BPH can also be estimated from this. A determination of the serum creatinine indicates a congestion-related renal failure and is obligatory before a urogram .
Apparative investigation
With the help of the urine stream measurement (determination of the urine stream volume per unit of time - uroflowmetry ), if the micturition volume is more than 150 ml, indications of bladder emptying disorders can be detected in screening examinations . The maximum urine flow rate should generally not be below 10 ml / s. The use of the method to detect a BPH-related obstruction is uncertain.
Residual urine and prostate volume in particular areassessed sonographically . Sonography also enables the detection of an enlarged middle lobe (mostly urodynamically particularly relevant). The ultrasound examination is usually carried out transrectally , but also enables a good determination of the residual urine volume transabdominally and, if the bladder is full, also of the prostate volume and the endovesical middle lobe. The findings are used to assess the risk of progression and the need for treatment. A pathologically increased amount of residual urine alone is not evidence of BPH that hinders the flow of urine. Relevant urinary congestion can be excluded by means of sonography of the upper urinary tract.
A urogram is indicated if a kidney disease is suspected.
Optional investigations
These examinations are carried out in cases in which further differential diagnostic clarification is required after the diagnosis described above has been completed . The amount consumed as well as the frequency and volume of micturition are recorded in a micturition log. As a result, for example, urinary frequency from a polyuria be distinguished. With the help of urodynamics , the urine flow rate can be compared with the temporal course of the micturition pressure built up in the bladder. This examination makes it possible, for example, to differentiate between a subvesical obstruction (BPH) and a weakness of the bladder muscles when the urine stream is weakened. The obstructive effect of BPH can be estimated using sonographic measurement of the detrusor thickness . For special questions, other procedures such as urethrocystoscopy are also used.
- Histological sections
Histological examination
The fine tissue examination of prostate tissue is carried out either from a surgical specimen or from a tissue sample obtained to rule out prostate cancer . In BPH there are no malignant cells, but compared to the healthy prostate, the tissue shows a nodular remodeling due to the proliferation of the stroma and glandular epithelium. Vertebral muscle nodes and focal ducts lined with a single layer of epithelium are typical . These nodular changes are usually relatively large and therefore not recognizable in small-volume tissue samples. The changes vary widely, but BPH always has a single-layer epithelium, whereas cell atypia are absent .
Treatment and healing prospects
Without treatment, BPH tends to progress slowly. The aim of therapy can therefore be to prevent the disease from progressing, to reduce existing symptoms that impair quality of life, or to strive to reduce BPH. In the absence of symptoms, treatment can primarily be dispensed with (controlled waiting) . In this case, however, progress is assumed. The benign enlargement of the prostate gland and its consequences can basically be treated with lasting success. However, relapses ( recurrences ) do occur.
Medical therapy
Drug treatment is indicated in stage I and in some cases in early stage II of the disease. It is individually coordinated by the doctor, whereby accompanying illnesses are also taken into account. It is not indicated if there are complications such as recurrent urinary retention or urinary tract infections, urinary bladder concrements , recurrent macrohematuria that cannot be managed conservatively or congestion-related expansion of the upper urinary tract with impaired kidney function or renal insufficiency.
Drug therapy can pursue various therapy goals. This includes reducing disturbing symptoms, preventing the progression of prostate growth or symptoms and the complications associated with them. The treatment must be permanent if it is to prevent the disease from progressing. In general, phytopharmaceuticals (herbal medicines), α1-adrenoceptor antagonists , 5α-reductase inhibitors, muscarinic receptor antagonists and combination preparations are available for the drug therapy of BPH . The PDE-5 inhibitor tadalafil is also used to treat symptoms of BPH.
Phytopharmaceuticals and biogenic drugs
For milder complaints (stage I or stage II according to Alken), plant extracts are also used, for example from saw palmetto fruits ( Serenoa repens , Sabal serrulata ), the African plum tree ( Prunus africana ), nettle roots ( Urtica dioica ), rye pollen ( Secale cereale ) and pumpkin seeds ( Cucurbita) pepo ) is used. They are used either alone (monopreparations) or combined (combination preparations). The reasons for a herbal therapy are usually the patient's tolerance and compliance. Extracts from the same plant may have different compositions and dosage regulations due to the manufacturers' different extraction processes.
Β-sitosterol is an essential and effective component of many herbal medicines . The substance is also used therapeutically in isolated form. There is evidence that β-sitosterol has an antiandrogenic effect and inhibits prostaglandin and leukotriene synthesis. The preparations do not remedy the enlargement of the prostate, but are intended to alleviate discomfort when urinating by influencing relevant measurement parameters (increase in micturition volume and the maximum urine flow, decrease in the amount of residual urine). Due to the lower drug risks (side effects, interactions, contraindications), phytopharmaceuticals used to treat BPH are not subject to prescription requirements . The therapeutic efficacy is considered insufficiently proven, as the evidence for a long-term, clinically relevant efficacy has not yet been produced. There is a lack of sufficient data on an influence on the risk of the progression of benign prostate syndrome and on the prevention of complications. In the USA, the sale of non-prescription phytopharmaceuticals was banned in 1990 in order not to give the patient a false sense of security or to delay further investigation. In Germany, the products contain a corresponding note in the instructions for use.
According to the AWMF guideline, there are indications of effectiveness from randomized, controlled studies for four phytotherapeutic preparations. However, further studies based on international criteria are required. According to an analysis by the Cochrane Collaboration , saw palmetto fruit extract improves slightly to moderate urinary flow and urination problems. The relief of symptoms through the extract is comparable to that of finasteride, a prescription drug. However, more research on the long-term effects of saw palmetto fruit extract is needed. The use of an extract combination of saw palmetto fruits and nettle roots had proven in a study to be just as symptomatically effective as the prescription-only alpha-receptor blocker tamsulosin . Rye pollen extract also seems to improve the symptoms of urination somewhat. Preparations made from pumpkin seeds and nettle root are based on a bibliographical proof of effectiveness, i.e. H. without submission of preparation-specific clinical studies, approved ("general medical use").
α1-adrenoceptor antagonists
The effect of the α1-adrenoceptor antagonists ( α-blockers ) is based on the relaxation of the smooth muscles of the prostate and urethra, which improves the flow of urine and alleviates the associated symptoms. However, they have only a minor influence on the mechanical obstruction of the discharge from the bladder caused by the enlargement of the prostate, but are recommended to reduce and delay the progression of symptoms. For example, alfuzosin , doxazosin , tamsulosin and terazosin are used . With a suitable dosage, all α-blockers are equally effective. They have a relatively prompt onset of action and appear to be superior to 5α-reductase inhibitors in the treatment of disturbing symptoms. In the long term, α-blockers have no influence on the growth of the prostate and the risk of acute urinary retention.
Alpha-blockers were originally introduced in 1969 for the treatment of high blood pressure ( Minipress ). It is therefore easy to understand that they can lead to considerable side effects in the cardiovascular system, especially if the accompanying medication is chosen accordingly. In addition, fatigue, dizziness , headache , diarrhea , swelling of the nasal mucosa and flu-like symptoms are typical undesirable effects. In principle, however, they are reversible after discontinuation of the drug. Abnormal ejaculations can also occur, especially with tamsulosin . Due to the drug risks, α-blockers require a prescription.
5α-reductase inhibitors
By blocking the enzyme 5α-reductase, 5α-reductase inhibitors inhibit the conversion of testosterone into dihydrotestosterone . The latter acts selectively on the prostate and is essentially responsible for its growth. Be used dutasteride and finasteride , which differ pharmacologically easily. The aim of treatment using these preparations is to shrink the prostate gland. Finasteride has been shown to be effective in terms of symptoms and progression of benign prostatic hyperplasia. Side effects such as decreased libido and impotence as well as decreased growth of hormone-dependent body hair were found.
Muscarinic receptor antagonists
Muscarinic receptor antagonists ( anticholinergics ) cause a decrease in the tone of the smooth bladder wall muscles ( detrusor vesicae muscles ). Their use is therefore limited to micturition problems caused by overactivity of this muscle, as can occur with BPH (urgency to urinate, urge incontinence , pollakiuria ; corresponds to the symptoms of an overactive bladder ). However, the use of these drugs must be weighed up critically, as they can lead to urinary retention due to the weakening of the bladder muscles in relevant obstructions caused by BPH . Muscarinic receptor antagonists are contraindicated for urinary retention . Typical side effects of the muscarinic receptor antagonists are sleep and memory disorders as well as confusion and an increased tendency to fall.
Tadalafil
The only PDE-5 inhibitor approved for the treatment of BPH syndrome is tadalafil , which has been approved in the USA, the EU and other countries such as Canada and Japan for this indication. By increasing cGMP , tadalafil causes muscle relaxation in the urinary tract (smooth muscles of the prostate, the bladder and the supplying blood vessels), which leads to an improvement in the symptoms, assessed using the International Prostate Symptom Score (IPSS). The approval is based on four clinical studies that were carried out on more than 1500 patients over a period of 12 weeks. Tadalafil was tested against placebo and against tamsulosin ; Among them, one of the studies looked at the improvement in benign prostate syndrome and erectile dysfunction in patients with both diseases.
Evidence analyzes between 2007 and 2012 that were carried out by the guideline group of the “Academy of German Urologists ” in the course of drawing up guidelines for the AWMF guideline, which is no longer valid due to the passage of time , and including the systematic review with meta-analysis by Gacci et al. had not found any reliable evidence of a relevant benefit with regard to the examined endpoints for various of the PDE-5 inhibitors ( vardenafil , sildenafil and tadalafil). A review article from 2019 confirmed an improvement in lower urinary tract symptoms (LUTS) with tadalafil, but the evidence is low and insufficient to assess the long-term effectiveness and prevention of the progression of symptoms. An overview, also from 2019, came to the result that, on the basis of the examined preclinical and clinical data, relaxation in the bladder and prostate induced by tadalafil could be determined and that the active ingredient was used both in monotherapy and in additional therapy in patients with urinary tract symptoms (LUTS ) is effective as a result of BPH. Unlike the 5α-reductase inhibitors, which are also used in BPH and which can lead to sexual dysfunction as a side effect, tadalafil improves sexual function.
surgery
According to the guidelines of the German Society for Urology from 2014, surgical treatment is indicated if the prostate forms an obstacle (obstruction) to the outflow of urine that is significant to health - and cannot be treated in any other way - or if there are complications such as recurrent urinary retention , recurrent urinary tract infections , conservative uncontrollable, recurrent gross hematuria , urinary bladder concrements , dilation of the upper urinary tract, impaired renal function or renal insufficiency . A basic distinction is made between two types of intervention. Either part of the prostate tissue is removed directly (primarily ablative) , or it is damaged in one way or another in such a way that the volume of the gland is reduced after the procedure (secondary ablative) .
Chances of success
The success of an operation - measured on the basis of a clear reduction in stressful symptoms - depends to a large extent on whether the enlarged prostate actually caused a noticeable restriction in the flow of urine (obstruction), and not just other complaints, such as frequent urination with or without Incontinence. There are non-invasive , reliable tests to answer this question , such as the penile cuff test (PCT) , which has been known since 1997 , in which a computer-controlled air pressure cuff (similar to a blood pressure measurement ) around the penis measures the pressure of the urine flow. Using this method, a 2013 study showed that 94% of patients classified as “obstruction” had a successful operation. In contrast, 70% of the patients with the classification “no obstruction” had an unsuccessful result of the operation.
If an enlargement of the prostate (BPH) with obstruction occurs together with a frequent urge to urinate ( overactive bladder ), which occurs in approx. 50% of cases, this component of the disturbance persists in approx. 20% of the patients even after the operation. However, this rate only applies to follow-up examinations within a few years. After 10–15 years, in a study of 55 patients with obstruction and overactive bladder before the operation, 48 (= 87%) had retained the decrease in obstruction, but with regard to the overactive bladder, they had returned to the state they had before the operation.
Transurethral resection of the prostate
The transurethral resection of the prostate (TURP) is still today the so-called gold standard in the operative therapy of BPS. There is no other surgical procedure whose long-term success in terms of subjective and objective parameters (urodynamics) has been so well documented. As with any surgical procedure, complications can also arise with TURP. Bleeding and flushing of irrigation fluid (TUR syndrome) during the operation and secondary bleeding play a decisive role here. Depending on the study, the frequency is given as up to almost nine percent. Mortality, which 40 years ago was still quite high at 2.5%, is now below 0.1 to 0.25 percent. With regard to the complication rate, TURP has been technically modified many times in the past. These include changes to the high-frequency generator (coagulating intermittent cutting), the current flow (bipolar resection), the electrodes (sling, vaporization) and the resection technique. For individual modifications it is documented that the perioperative risk of bleeding can be reduced. The postoperative incidence of permanent urinary incontinence is around 0.5% (0.1–1.8). The loss of ejaculation ( retrograde ejaculation ) occurs in approx. 65% of the operated on.
Transurethral incision of the prostate
The transurethral incision of the prostate (TUIP) is also a form of transurethral treatment, in which the aim is not to shrink the prostate gland, but only to incise it in order to reduce the outlet resistance of the bladder. It is suitable for younger men with a relatively small prostate (<30 grams). The effectiveness seems to be comparable to that of TURP, the rate of side effects is lower, but at 15.9% after ten years, more patients have to be operated on than after TURP (8–15%).
Open prostate surgery
Open prostate surgery is also known as prostate enucleation or adenoma enucleation; it is the oldest method for the surgical treatment of BPH. After opening the bladder, the prostate is manually detached from the surrounding tissue intravesically and removed. The continued effectiveness of the method is well documented. Typical complications are bladder neck sclerosis, urethral stricture and meatus tightness. There are different figures for the postoperative risk of permanent urinary incontinence . These range from less than for TURP to 9.5%.
Laser process
Interstitial laser coagulation (ILC), holmium laser enucleation (HoLEP) and laser vaporization of the prostate have so far achieved clinical relevance among laser procedures .
The volume of the prostate can be reduced to a relevant extent using ILC , but its effectiveness is inferior to that of TURP. Another major disadvantage of the method is the coagulation-related initial increase in the bubble outlet resistance. It has not yet found widespread use.
The HoLEP ( Holmium laser enucleation of the prostate) (lat. Ex nucelus, literally "from the core" for peeling, peeling) has been increasingly offered as an alternative to the classic abdominal incision procedure since 2007. The inner tissue of the prostate is lifted off with little bleeding by means of a laser beam, shredded and then suctioned off. This procedure is on a par with TURP in terms of its effect; postoperatively, it has a lower frequency of complications (e.g. bleeding, catheter length of stay and hospital stay). According to a study, HoLEP is superior to TURP and should become the new gold standard. However, it is difficult to learn and therefore not widely used yet. At some clinics, the HoLEP procedure has completely replaced the standard therapy using incision surgery through the abdominal wall and bladder for larger glands. The HoLEP process even allows patients to continue to take blood thinners (e.g. ASS100 ). The hospital can often be left three days after the operation. Even with this form of prostate reduction, a follow-up operation may have to be expected after 15 to 20 years, as the tissue will grow back again.
The laser vaporization is also a hard-to-learn techniques. Your results depend on the surgeon. Long-term data on this are still lacking. For KTP laser vaporization (evaporation) of the excess, constricting prostate tissue, an Nd: YAG laser that is frequency- doubled by means of a KTP crystal and generates light with a wavelength of 532 nm is used . This wavelength is in the green , visible range of the color spectrum (greenlight process) . The light pulses are able to remove prostate tissue with almost no bleeding. Their use therefore seems to be possible in high-risk patients (for example coagulation disorders or anticoagulation ).
Transurethral microwave thermotherapy
In transurethral microwave thermotherapy (TUMT), the tissue of the prostate is heated. A distinction is made between low-energy (≤ 55 ° C) and high-energy technology (> 55 ° C). The relief of symptoms is comparable for both procedures. In comparison to the procedures mentioned above, the TUMT treatment can be carried out on an outpatient basis and under local anesthesia.
The low energy technology (NE-TUMT) does not have an ablative effect due to the lower temperature development, i.e. H. the prostate tissue is not destroyed. This procedure was therefore not able to establish itself and is now only used very rarely.
In contrast to this, the effectiveness of high-energy technology (HE-TUMT) is only slightly worse than that of classic TURP, whereas the morbidity rate is lower. The further development of high-energy technology is the so-called HE-TUMT with integrated temperature feedback. This method works with several temperature probes, which enable improved control and more targeted energy input. Results comparable to those of the TURP can be achieved here.
Typically, heat edema of the treated tissue occurs after the procedure, which can make a temporary urinary drainage (catheter) necessary. The HE-TUMT can be used as an alternative to the TURP, especially for high-risk patients with urinary retention.
The guidelines of the American Urological Association (AUA) 2018 on this topic expressed the view that the treatment could be offered by TUMT, provided that the patient would be noted that in this case the rate of repeat operations was higher than TURP.
In the 2019 update of the guidelines of the European Association of Urology (EAU) on this topic, the TUMT treatment form was removed from the guidelines.
Transurethral needle ablation
In transurethral needle ablation (TUNA), the prostate tissue is heated using radio frequency waves . It can be done without anesthesia. There is no risk of bleeding, other complications are rare, erection and ejaculation remain unaffected, cases of persistent urinary incontinence have not yet been described. The success rate is comparable to that of TURP, but 13.8–23.3% of patients have to undergo renewed therapy within five years. "The TUNA is particularly suitable for patients with moderate to pronounced symptoms and low-grade obstruction." (Quoted from) .
The 2018 American Urological Association (AUA) guidelines on this subject indicated that TUNA treatment was not recommended.
In the 2019 update of the guideline of the European Association of Urology (EAU) on this topic, the TUNA treatment form was removed from the guidelines.
Prostatic stents
Stents are inserted temporarily or permanently into the prostatic part of the urethra without anesthesia. The purpose of the temporary implants is to replace a transurethral or suprapubic urinary catheter. They need regular changes. Permanent stents epithelialize and can be left permanently. The complication rate is relatively high, typical are primary maladjustment, secondary displacement , incrustation, persistent urge incontinence as well as secondary worsening of micturition and symptoms. 20% of permanent stents must be removed within the first year and 50% within the first ten years. Stents are suitable for polymorbid patients and those with a limited life expectancy if there is a strict indication (e.g. no large prostate middle lobe ) .
Prostate lifting
The symptoms of BPH can be improved with the so-called Urolift . This implant is inserted transurethrally into the prostate and helps to gather the prostate tissue and thus expand the diameter of the urethra. Two studies by the manufacturer show the effectiveness of these implants and led to the implants being approved by the FDA . Urine flow is increased by an average of 30%, and patients report an improvement in symptoms and an increase in quality of life. Within the studies, only minor complications such as pain during micturition or blood in the urine could be observed, serious complications did not occur. The European BPH-6 study tries to compare the Urolift with the TURP.
Removal by water jet
A more recent method - still known as experimental ("under investigation") - is tissue ablation using a water jet ( aquablation or aquabeam ) as part of a largely automated operation.
Review articles from 2018 and 2019 rated aquablation as probably as effective as TURP, with shorter surgery times and fewer undesirable side effects in the area of sexual functions.
Preliminary results suggest that aquablation has a good chance of success even with a large prostate (80–150 mL) and with a middle lobe reaching into the bladder.
Removal by steam injection
Another new method - still known as experimental ("under investigation") - is tissue ablation by means of micro-injections of water vapor ( Rezum system). The minimally invasive operation is performed on an outpatient basis and the time required for the core treatment, the steam injections, is only about 10 minutes. The body's own removal of the cells that have been switched off by the steam takes place gradually over a period of approx. 3 months, with the first relief often already being noticeable after 3 weeks.
The Rezum procedure works from within the organ without injuring the part of the urethra that is in the prostate. This happens because the micro-injection needle of the device penetrates the urethra in this area, but does not injure it.
Although it is a relatively new procedure, one study has already shown positive results in follow-up tests after four years. The procedure also proved to be suitable for large prostates (> 80 mL) and for those in which the middle lobe protrudes into the bladder. Previous studies have shown that sexual functions were not impaired by the procedure.
Other procedures
Other methods such as water-induced thermotherapy (WIT) , high-intensity focused ultrasound (HIFU) , which heats the tissue, and injections of ethanol or botulinum toxin into the prostate have so far not been widely used. For this reason, there is a lack of sufficiently valid empirical values with regard to side effects and studies for proof of effectiveness. In the WIT, water heated to 60 degrees is fed into the prostatic part of the urethra via a special transurethral catheter . There it heats the prostate tissue. Recently, u. a. Prostate artery embolization (PAE) was also offered at various German clinics .
Prevention and prognosis
Although BPH is primarily related to the aging process , its severity can also be influenced by accompanying factors such as obesity . As a preventive measure , it is recommended to eat a balanced, high-fiber diet and drink enough water. Such a diet prevents obesity, an important factor in preventing this prostate disease. Heavy smoking is seen as a further risk factor . Sufficient exercise and regular physical activity are important positive influencing factors. Even in the case of a clinically manifest disease caused by BPH, the prognosis is very favorable with appropriate treatment; the fatal outcome of the disease known from centuries ago is no longer an issue today.
Historical aspects
In earlier centuries, chronic prostate swelling after the age of 50 was considered a result of inflammation. Fundamental knowledge in this area in the sense of modern medicine was first published in 1761 by Giovanni Battista Morgagni . This work was resumed and continued in the following years by John Hunter and his brother-in-law Everard Home .
The beginnings of prostate surgery in the 19th century were closely based on the experience of stone incisions (surgical bladder stone removal) that was already available at that time . At the end of the 19th and beginning of the 20th century, there was competition between perineal , retro- pubic and transvesical procedures, i.e. access through the perineum, above the pubic bone or through the bladder. The latter were so refined in the first half of the 20th century that a procedure (transvesical prostate enucleation) is still used regularly today. In 1926 the first instrument set for electroresection, a forerunner of the transurethral prostate resection (TURP), which is now the gold standard , was presented in the USA.

Veterinary medicine
BPH plays an important role in dogs . Here the disease occurs regularly in older males. Since the enlargement of the prostate takes place symmetrically and evenly distributed over the entire organ, the most common symptom observed is defecation discomfort due to an obstruction of the pelvic outlet. In addition, multiple prostate cysts can appear, which can result in the spontaneous discharge of serous, bloody secretions from the urethra. The enlarged prostate is also considered a risk factor for the development of a perineal hernia . Therapeutic options are castration as well as drug deactivation of testicular function. Osaterone and delmadinone are approved for this application ; In addition, there have been positive experiences with cyproterone and finasteride , but these are not approved for veterinary use.
literature
- Ulrike Zwergel, Jürgen Sökeland: Benign prostatic hyperplasia: Basics and therapy . Springer Verlag, 1999, ISBN 3-540-65269-8 .
- D. Jocham, C. Doehn: Benign prostatic hyperplasia. In: M. Böhm, F. Jockenhövel, W. Weidner: Men’s consultation hour: the practical handbook on counseling, prevention and therapy . Springer Verlag, 2004, ISBN 3-540-00915-9 .
- Klaus Höfner, CG Stief, Udo Jonas: Benign Prostatic Hyperplasia: Practical Guide . Springer Verlag, 2000, ISBN 3-540-62968-8 .
Web links
- Benign prostate syndrome (BPD)
- Rezum - How It Works , video, 1:04 min, by Potomac Urology.
Individual evidence
- ↑ RT Chang, R. Kirby, BJ Challacombe: Is there a link between BPH and prostate cancer? In: The Practitioner. Volume 256, Number 1750, April 2012, pp. 13-6, 2, PMID 22792684 .
- ^ JM Hollingsworth, TJ Wilt: Lower urinary tract symptoms in men. In: BMJ. Volume 349, August 2014, p. G4474, doi : 10.1136 / bmj.g4474 , PMID 25125424 , PMC 4688452 (free full text) (review).
- ↑ a b c d e S2-AWMF guideline : Diagnostics and differential diagnostics of the benign prostate syndrome (BPS) , register number 043/034
- ↑ Examples for the use of the outdated terms: Hartmut Link u. a .: Supportive therapy for malignant diseases: prevention and treatment of disease symptoms and therapy-related side effects . Deutscher Ärzteverlag, 2006, ISBN 3-7691-0466-8 , p. 435; Peter Dosch (Ed.): Textbook of neural therapy according to Huneke. (Regulation therapy with local anesthetics) . Georg Thieme Verlag, 1995, ISBN 3-7760-1451-2 , p. 315 ( limited preview in Google book search); Hans-Joachim Schmoll, Klaus Höffken, Kurt Possinger (eds.): Compendium of internal oncology . Springer, 2005, ISBN 3-540-20657-4 , p. 1418.
- ↑ J. Altwein: Urology . Enke-Verlag, 1979, ISBN 3-432-89931-9 , p. 279.
- ↑ a b Y. Gat, M. Gornish, M. Heiblum, S. Joshua: Reversal of benign prostate hyperplasia by selective occlusion of impaired venous drainage in the male reproductive system: novel mechanism, new treatment. In: Andrologia. Volume 40, Number 5, October 2008, pp. 273-281, doi: 10.1111 / j.1439-0272.2008.00883.x . PMID 18811916 .
- ↑ R. Mischke: Cytological internship for veterinary medicine . Schlütersche, 2005, ISBN 3-89993-013-4 , p. 162 ( limited preview in the Google book search).
- ↑ E. Dahme et al.: Outline of the special pathological anatomy of domestic animals . Georg Thieme Verlag, 2007, ISBN 978-3-8304-1048-5 , p. 208 ( limited preview in the Google book search).
- ↑ U. Zwergel: Urology specialist examination: In cases, questions and answers . Urban & Fischer Verlag, 2008, ISBN 978-3-437-24510-7 , p. 246 ( limited preview in Google book search).
- ^ MY Kang, JH Ku, SJ Oh: Non-invasive parameters predicting bladder outlet obstruction in Korean men with lower urinary tract symptoms. In: Journal of Korean medical science. Volume 25, number 2, February 2010, pp. 272-275, doi: 10.3346 / jkms.2010.25.2.272 . PMID 20119582 . PMC 2811296 (free full text).
- ↑ D. Pfeiffer et al.: HIFU technology for the primary interventional treatment of prostate cancer - early results. Hamburger Ärzteblatt, 5/2006, p. 277 pdf ( Memento from December 12, 2010 in the Internet Archive )
- ^ C. Huggins et al: The effect of castration on benign prostatic hypertrophy in men . In: Urologist, 1940, 43, pp. 705-711; quoted from: U. Zwergel et al.: Benign prostatic hyperplasia: Basics and therapy. Springer, 1999, ISBN 3-540-65269-8 .
- ↑ D. Ganten et al.: Molecular medical principles of age-specific diseases. Springer, 2004, ISBN 3-540-00858-6 , p. 306 ( limited preview in Google book search).
- ↑ C. Dadak: Sexuality, Reproduction, Pregnancy, Birth . Facultas Verlag, 2009, ISBN 978-3-7089-0535-8 , p. 30 ( limited preview in Google book search).
- ↑ J. Grüger, L. Pientka: Symptoms and quality of life in patients with benign prostatic hyperplasia in the outpatient area in Germany. In: Current Urology. 27, No. 5, 1996, pp. 260-266, doi: 10.1055 / s-2008-1055604 .
- ↑ S3 guideline for prostate cancer: early detection, diagnosis and therapy of the various stages of the German Society for Urology (DGU). In: AWMF online (as of 2018).
- ↑ L. Bubendorf et al.: Pathology: Zytopathologie. Springer, 2010, ISBN 978-3-642-04561-5 , p. 212 ( limited preview in Google book search).
- ↑ U. Zwergel: Benign prostatic hyperplasia: Basics and therapy. Springer, 1999, ISBN 3-540-65269-8 , p. 4 ( limited preview in Google book search).
- ↑ S. Madersbacher, M. Marszalek: Benign prostatic hyperplasia: successes and limits of pharmacotherapy. In: The internist. 2007, doi: 10.1007 / s00108-007-1843-8
- ↑ M. Oelke et al.: Drug therapy of benign prostatic hyperplasia. In: The Urologist. 2009, doi: 10.1007 / s00120-009-2141-y
- ↑ a b c d e f g h i j k l m n o p q r s t u S2-AWMF guideline : Therapy of Benign Prostate Syndrome (BPS) from 2014
- ↑ T. Dingermann, K. Hiller, G. Schneider, I. Zündorf: Schneider drug drugs. 5th edition. Elsevier, 2004, ISBN 3-8274-1481-4 , p. 14 ff.
- ↑ U. Zwergel et al.: Benign prostatic hyperplasia: Basics and therapy. Springer, 1999, ISBN 3-540-65269-8 , pp. 60 ff. ( Limited preview in the Google book search).
- ↑ Ernst Mutschler, Gerd Geisslinger, Heyo K. Kroemer, Peter Ruth, Monika Schäfer-Korting: drug effects. Textbook of pharmacology and toxicology. 9th edition. Wissenschaftliche Verlagsgesellschaft mbH, Stuttgart 2008, ISBN 978-3-8047-1952-1 , p. 710.
- ↑ Drug treatment of benign prostatic hyperplasia. In: arznei-telegram. November 1991, Retrieved November 26, 2010 .
- ↑ J. Tacklind, R. MacDonald, I. Rutks, TJ Wilt: Serenoa repens for benign prostatic hyperplasia. In: Cochrane database of systematic reviews (online). Number 2, 2009, S. CD001423, doi: 10.1002 / 14651858.CD001423.pub2 . PMID 19370565 . PMC 3090655 (free full text). (Meta-analysis).
- ↑ U. Engelmann u. a .: Efficacy and safety of a combination of sabal and urtica extract in lower urinary tract symptoms. A randomized, double-blind study versus tamsulosin. Drug research 2006; 56 (3) pp. 222-229.
- ^ T. Wilt, R. Mac Donald, A. Ishani, I. Rutks, G. Stark: Cernilton for benign prostatic hyperplasia. In: Cochrane database of systematic reviews (online). Number 2, 2000, S. CD001042, doi: 10.1002 / 14651858.CD001042 . PMID 10796739 (meta-analysis).
- ↑ a b J. Tacklind, HA Fink, R. Macdonald, I. Rutks, TJ Wilt: Finasteride for benign prostatic hyperplasia. In: Cochrane database of systematic reviews (online). Number 10, 2010, p. CD006015, doi: 10.1002 / 14651858.CD006015.pub3 . PMID 20927745 . (Meta-analysis).
- ↑ a b F. Perabo and others: Incontinence: Questions and Answers. Deutscher Ärzteverlag, 2009, ISBN 978-3-7691-1252-8 , p. 148 ff. ( Limited preview in the Google book search).
- ↑ AM Arisco, EK Brantly, SR Kraus: oxybutynin extended release for the management of overactive bladder: a clinical review. In: Drug Design, Development and Therapy . Volume 3, 2009, pp. 151-161, PMID 19920931 . PMC 2769230 (free full text).
- ↑ a b G. Geisslinger et al .: Mutschler drug effects . 11th edition. WVG, Stuttgart 2019, pp. 626‒627.
- ^ ABDA database - International Medicines . Accessed July 31, 2020.
- ↑ Sven Siebenand: PDE-5 inhibitor Tadalafil: More than a sexual enhancer , Pharmazeutische Zeitung of December 11, 2012, accessed on July 28, 2020.
- ^ Pharmaceuticals and Medical Devices Agency , accessed July 31, 2020.
- ↑ Assessment Report Cialis , Committee for Medicinal Products for Human Use (CHMP), October 18, 2012 ( PDF ).
- ↑ Mauro Gacci, Giovanni Corona, Matteo Salvi, Linda Vignozzi, Kevin T. McVary, Steven A. Kaplan, Claus G. Roehrborn, Sergio Serni, Vincenzo Mirone, Marco Carini, Mario Maggi: A systematic review and meta-analysis on the use of phosphodiesterase 5 inhibitors alone or in combination with α-blockers for lower urinary tract symptoms due to benign prostatic hyperplasia . In: European Urology . tape 61 , 2012, doi : 10.1016 / j.eururo.2012.02.033 .
- ↑ Evidence analysis 2012 on the therapy of benign prostate syndrome (BPS) - research of randomized controlled studies as well as systematic reviews and meta-analyzes from 2007 to August 2012 - validity expired - guideline is being reviewed. Ed .: Medical Center for Quality in Medicine (2013). Accessed July 31, 2020.
- ↑ Roderick MacDonald, Michelle Brasure, Philipp Dahm, Carin M. Olson, Victoria A. Nelson, Howard A. Fink, Michael C. Risk, Bruce Rwabasonga, Timothy J. Wilt: Efficacy of newer medications for lower urinary tract symptoms attributed to benign prostatic hyperplasia: a systematic review . In: The Aging Male . tape 1 , 2019, doi : 10.1080 / 13685538.2018.1434503 .
- ↑ Fabiola Zakia Mónica, Gilberto De Nucci: Tadalafil for the treatment of benign prostatic hyperplasia . In: Expert Opinion on Pharmacotherapy . tape 8 , 2019, doi : 10.1080 / 14656566.2019.1589452 .
- ^ A b Y. H. Jiang, HC Kuo: Recent research on the role of urodynamic study in the diagnosis and treatment of male lower urinary tract symptoms and urinary incontinence. In: Ci ji yi xue za zhi = Tzu-chi medical journal. Volume 29, number 2, 2017 Apr-Jun, pp. 72-78, doi : 10.4103 / tcmj.tcmj_19_17 , PMID 28757770 , PMC 5509199 (free full text) (review).
- ↑ S. Malde, AK Nambiar, R. Umbach, TB Lam, T. Bach, A. Bachmann, MJ Drake, M. Gacci, C. Gratzke, S. Madersbacher, C. Mamoulakis, KA Tikkinen, S. Gravas: Systematic Review of the Performance of Noninvasive Tests in Diagnosing Bladder Outlet Obstruction in Men with Lower Urinary Tract Symptoms. In: European urology. Volume 71, number 3, 03 2017, pp. 391-402, doi : 10.1016 / j.eururo.2016.09.026 , PMID 27687821 (review), PDF .
- ↑ G. Losco, L. Keedle, Q. King: Non-invasive urodynamics predicts outcome prior to surgery for prostatic obstruction. In: BJU international. Volume 112 Suppl 2, November 2013, pp. 61-64, doi : 10.1111 / bju.12382 , PMID 24127677 , PDF .
- ↑ RS Eapen, SB Radomski: Review of the epidemiology of overactive bladder. In: Research and reports in urology. Volume 8, 2016, pp. 71-76, doi : 10.2147 / RRU.S102441 , PMID 27350947 , PMC 4902138 (free full text) (review).
- ^ AW Thomas, P. Abrams: Lower urinary tract symptoms, benign prostatic obstruction and the overactive bladder. In: BJU international. Volume 85 Suppl 3, May 2000, pp. 57-68, PMID 11954200 (review), PDF
- ^ O. Reich: Benign prostate syndrome. In: Der Urologe A. Volume 49, No. 1, 2010, pp. 113–126, doi: 10.1007 / s00120-009-2183-1 .
- ↑ a b K.-H. Bichler: The urological report. Springer, 2004, ISBN 3-540-42757-0 , p. 338 ( limited preview in the Google book search)
- ↑ JN Cornu, S. Ahyai, A. Bachmann, J. de la Rosette, P. Gilling, C. Gratzke, K. McVary, G. Novara, H. Woo, S. Madersbacher: A Systematic Review and Meta-analysis of Functional Outcomes and Complications Following Transurethral Procedures for Lower Urinary Tract Symptoms Resulting from Benign Prostatic Obstruction: An Update. In: European urology. Volume 67, number 6, June 2015, pp. 1066-1096, doi : 10.1016 / j.eururo.2014.06.017 , PMID 24972732 (review), PDF .
- ↑ J. Michalak, D. Tzou, J. Funk:: HoLEP: the gold standard for the surgical management of BPH in the 21 (st) Century . In: American journal of clinical and experimental urology . 3, No. 1, 2015, pp. 36–42. PMID 26069886 .
- ↑ Karin Lehrich: Comparison of transurethral holmium laser enucleation of the prostate (HoLEp) and transvesical adenoma enucleation of the prostate: a prospective study. Dissertation, Free University of Berlin, 2002, http://d-nb.info/966392221
- ↑ TF Aho: Holmium laser enucleation of the prostate: a paradigm shift in benign prostatic hyperplasia surgery. In: Ther Adv Urol. 2013 Oct; 5 (5), pp. 245-253. PMID 24082919 .
- ↑ University of Munich Hospital: Holmium Laser Enucleation of the Prostate (HoLEP)
- ↑ a b Foster HE, Barry MJ, Dahm P, Gandhi MC, Kaplan SA, Kohler TS et al .: Surgical Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA Guideline. . In: J Urol . 200, No. 3, 2018, pp. 612-619. doi : 10.1016 / y.juro.2018.05.048 . PMID 29775639 .
- ↑ EAU: Management of Non-neurogenic Male LUTS - Summary of Changes 2019 .
- ↑ EAU: Management of Non-neurogenic Male LUTS - Summary of Changes 2019 .
- ↑ New medical device treats urinary symptoms related to enlarged prostate . English. US Food and Drug Administration press release dated September 13, 2013. Online at fda.gov, accessed September 20, 2013.
- ^ BPH-6: Comparison of the UroLift System to TURP for Benign Prostatic Hyperplasia . English. Online at clinicaltrials.gov on May 6, 2013. Accessed September 20, 2013.
- ↑ EAU: Management of Non-neurogenic Male LUTS - Summary of Changes 2019 .
- ↑ a b Pham H, Sharma P: Emerging, newly-approved treatments for lower urinary tract symptoms secondary to benign prostatic hypertrophy . In: Can J Urol . 25, No. 2, 2018, pp. 9228-9237. PMID 29679999 .
- ↑ Blessing Dhliwayo, Saheel Mukhtar: Novel Surgical Treatments for Benign Prostatic Hyperplasia . In: Dougmar Publishing Group, Inc. (Ed.): Journal of Endoluminal Endourology . 2, No. 1, January 31, 2019, ISSN 2561-9187 , pp. E17 – e23. doi : 10.22374 / jeleu.v2i1.29 . , PDF .
- ↑ Hwang EC, Jung JH, Borofsky M, Kim MH, Dahm P: Aquablation of the prostate for the treatment of lower urinary tract symptoms in men with benign prostatic hyperplasia. . In: Cochrane Database Syst Rev . 2, 2019, p. CD013143. doi : 10.1002 / 14651858.CD013143.pub2 . PMID 30759311 . PMC 6373984 (free full text).
- ^ Saadat H, Elterman DS: The Role of Aquablation for the Surgical Treatment of LUTS / BPH. . In: Curr Urol Rep . 20, No. 8, 2019, p. 46. doi : 10.1007 / s11934-019-0905-5 . PMID 31227924 .
- ↑ Zorn KC, Goldenberg SL, Paterson R, So A, Elterman D, Bhojani N: Aquablation among novice users in Canada: A WATER II subpopulation analysis. . In: Can Urol Assoc J . 13, No. 5, 2019, pp. E113-E118. doi : 10.5489 / cuaj.5501 . PMID 30332589 . PMC 6520060 (free full text).
- ↑ EAU: Management of Non-neurogenic Male LUTS - Summary of Changes 2019 .
- ↑ JC Ulchaker, MS Martinson: Cost-effectiveness analysis of six therapies for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. In: ClinicoEconomics and outcomes research: CEOR. Volume 10, 2018, pp. 29-43, doi : 10.2147 / CEOR.S148195 , PMID 29343977 , PMC 5749396 (free full text).
- Jump up ↑ KT McVary, T. Rogers, CG Roehrborn: Rezūm Water Vapor Thermal Therapy for Lower Urinary Tract Symptoms Associated With Benign Prostatic Hyperplasia: 4-Year Results From Randomized Controlled Study. In: Urology. Volume 126, 04 2019, pp. 171–179, doi : 10.1016 / j.urology.2018.12.041 , PMID 30677455 (free full text).
- ↑ JY Leong, AS Patel, R. Ramasamy: Minimizing Sexual Dysfunction in BPH Surgery. In: Current sexual health reports. Volume 11, number 3, September 2019, pp. 190-200, doi : 10.1007 / s11930-019-00210-1 , PMID 31467497 , PMC 6714584 (free full text) (review).
- ↑ H. Pham, P. Sharma: Emerging, newly-approved treatments for lower urinary tract symptoms secondary to benign prostatic hypertrophy. In: The Canadian journal of urology. Volume 25, number 2, 04 2018, pp. 9228-9237, PMID 29679999 (review), PDF .
- ↑ KT McVary, T. Rogers, J. Mahon, NK Gupta: Is Sexual Function Better Preserved After Water Vapor Thermal Therapy or Medical Therapy for Lower Urinary Tract Symptoms due to Benign Prostatic Hyperplasia? In: The journal of sexual medicine. Volume 15, number 12, December 2018, pp. 1728–1738, doi : 10.1016 / j.jsxm.2018.10.006 , PMID 30446471 .
- ↑ J. Westwood, R. Geraghty, P. Jones, BP Rai, BK Somani: Rezum: a new transurethral water vapor therapy for benign prostatic hyperplasia. In: Therapeutic advances in urology. Volume 10, number 11, November 2018, pp. 327-333, doi : 10.1177 / 1756287218793084 , PMID 30344644 , PMC 6180381 (free full text) (review).
- ↑ JK Parsons, AV Sarma, K. McVary, JT Wei: Obesity and benign prostatic hyperplasia: clinical connections, emerging etiological paradigms and future directions. In: The Journal of Urology 182, 2009, pp. S2 7 – S3 1, doi: 10.1016 / j.juro.2009.07.086 , PMID 19846130 . (Review).
- ^ EA Platz, EB Rimm, I. Kawachi, GA Colditz, MJ Stampfer, WC Willett, E. Giovannucci: Alcohol consumption, cigarette smoking, and risk of benign prostatic hyperplasia. In: American journal of epidemiology. Volume 149, Number 2, January 1999, pp. 106-115, PMID 9921955 .
- ↑ J. Sea, KS Poon, KT McVary: Review of exercise and the risk of benign prostatic hyperplasia. In: The Physician and sportsmedicine, Volume 37, Number 4, December 2009, pp. 75-83. PMID 20048544 .
- ↑ Vidal Auguste-Théodore: Textbook of surgery and operation theory. Verlag Reimer, 1859, p. 129 ff. ( Limited preview in the Google book search).
- ↑ U. Zwergel et al.: Benign prostatic hyperplasia: Basics and therapy. Springer, 1999, ISBN 3-540-65269-8 , p. 130.
- ↑ HG Dietrich: Illustrated history of urology. Springer, 2004, ISBN 3-540-08771-0 , p. 122 ff. ( Limited preview in the Google book search).
- ↑ E.-G. Grünbaum, E. Schimke (ed.): Clinic of dog diseases. Enke, 2007, p. 775.




