connective tissue
Connective tissue describes different types of tissue that occur in all areas of the body and perform a variety of supporting tasks there. Connective tissue contains comparatively few cells . But it is rich in intercellular mass . Connective tissue is indispensable for the body because it maintains organ shapes and protects against damage, serves as a water reservoir and plays a central role as a place of defense reactions against pathogens. The soft tissue components of the connective tissue, which penetrate the whole body as an enveloping and connecting tension network, are also known as fascia .
The various tissues, which are summarized under the generic term connective tissue, appear very different both when viewed with the naked eye and when magnified under the microscope. In the specialist literature there is no complete agreement as to which tissues are to be assigned to connective tissue. There is far-reaching consensus that loose, tight, reticular, gelatinous and spinocellular tissue belong to the connective tissue type in the narrower sense; in a somewhat broader sense, cartilage and bone tissue as supporting tissue also belong to the connective tissue. Usually the fatty tissue is also considered as a special form of connective tissue, more rarely also the blood and the various types of muscle tissue .
All these types of connective tissue develop from the mesenchyme , which, together with the gelatinous connective tissue, is also known as "embryonic connective tissue".
development
During human embryonic development, 34 to 35 somites develop from the middle germ layer ( mesoderm ) . The ventral and medial parts of the somites develop as sclerotomes and become part of the mesenchyme. The neuroectoderm also plays a role in the formation of the mesenchyme . The mesenchyme consists of pluripotent stem cells , the numerous processes of which are connected to one another by contact surfaces known as gap junctions . The cells divide easily and are amoeboid . The individual types of connective tissue develop from the mesenchyme in the course of further embryonic development.
Common features
Connective tissue consists of comparatively few cells and a lot of intercellular substance . Different types of fibers are embedded in the intercellular substance. The fibers, made up of fibrillar proteins - the main part are collagens - form a dense meshwork. The space between the fibers is largely filled by highly swelling proteoglycans . The function of the fibers is to withstand tensile forces , while the proteoglycans have a compression damping effect. The interaction of fiber meshwork and proteoglycan buffer preserves the shape of organs.
The intercellular substance, which also serves to store extracellular growth factors , is produced by fibroblasts . In order to build up new connective tissue, fibroblasts can change their location, in which they differ from the localized fibrocytes. In addition to the predominantly local fibroblasts and fibrocytes, there are also permanently mobile cells in the connective tissue that are part of the immune system.
Connective tissue fibers
Collagen fibers
The high tensile strength, but hardly stretchable, collagen fibers are 1 to 10 micrometers thick , rarely up to 20 micrometers thick. In the electron microscope you can see a horizontal stripe, which is caused by the overlapping arrangement of the collagen molecules during the synthesis of collagen fibrils . The hydroxylation of proline residues necessary to stabilize the fibrils can only take place completely if sufficient vitamin C is available. A lack of vitamin C therefore leads to a disruption of collagen synthesis, which in severe cases leads to scurvy .
A large number of different types of collagen are found in the connective tissues; the most important are the collagen types I to IV:
| Collagen type | shape | Occurrence |
|---|---|---|
| Type I. | fibril-forming | in most forms of connective tissue (e.g. in the skin , in the bones and in the organ stromata ) |
| Type II | fibril-forming | in the cartilage |
| Type III | fibril-forming | in the reticular connective tissue , in the reticular-fibrous connective tissue, in the lamina fibroreticularis |
| Type IV | networking | in the basal laminae |
A special subgroup of the collagen fibers are the reticular fibers . These fibers, consisting of type III collagen, form strikingly highly branched networks. With a diameter of 20 to 40 nanometers, they are significantly thinner than all other types of collagenous fibers. Reticular fibers are mainly found in the reticular connective tissue described below , but also in other tissues , for example in the dissesal space of the liver .
Elastic fibers
Elastic fibers consist of the glycoprotein fibrillin and the protein elastin stored in it . They can be - in any direction - many times their original length stretch and then return back to their original length. This is made possible by the tangled arrangement of the elastin in the fibers. The extensibility of the elastic fibers is spatially limited by collagen fibers that are adjacent in different proportions and that are significantly less elastic . Elastic fibers can be found in almost every type of connective tissue, but above all in lung tissue , in elastic arteries and elastic ligaments (e.g. in the ligamenta flava ).
Elastic fibers can be made visible with a light microscope using special elastic dyeing .
Connective tissue cells
The cells that characterize connective tissue are fibroblasts and fibrocytes. Both cell types are oval in shape and connected to one another via widely branched cell extensions. The main distinguishing feature between the two cell types is the cell nucleus , which appears significantly larger in the more active fibroblasts than in the more passive fibrocytes.
Between the fibers and the local cells there are also amoeboid, mobile, free cells that are primarily in the service of the immune system . These cells come from the bone marrow and migrate into the connective tissue via the blood vessels . In part, it is also typically in the blood occurring cells there to the white blood cell count. The most common free cells are:
In acute inflammatory processes , granulocytes in particular increasingly migrate into the connective tissue, which can be seen in the tissue section under the microscope by the high density of granulocytes between the few fibroblasts and fibrocytes.
Special types of connective tissue
Loose connective tissue
Loose connective tissue is used as filling material in various spaces in the body and forms the stroma , i.e. the framework of many organs. The basic substance usually predominates in loose connective tissue. Functionally, it serves, among other things, as a water reservoir, shifting layer and lounge for numerous free cells.
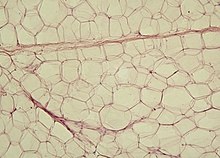
A special form of loose connective tissue is fatty tissue . In contrast to other types of connective tissue, there is hardly any intercellular substance in adipose tissue. The specialized cells are called adipocytes and store large amounts of fat in their cytoplasm .
Tight connective tissue
The tight connective tissue is characterized by a high proportion of collagen fibers - significantly more than in loose connective tissue. The proportion of basic substance is correspondingly lower. In addition, the tight connective tissue contains far fewer cells. According to the direction of the collagen fibers, it can be divided into tight, braid-like and tight, parallel-fiber connective tissue.
In the taut, braided connective tissue , the collagen fiber bundles cross over and over, which results in tensile strength in different directions. This type forms, for example, organ capsules , the dermis of the eye and skin, and the hard meninges .
The tight, parallel-fibrous connective tissue forms tendons and ligaments . The collagen fibers are arranged in parallel, which results in high tensile strength in one direction. The fibrocytes of the tendon tissue are also known as tendinocytes or "wing cells". They have flat and flat, three-dimensional wing-like extensions, between which and along which the collagen fiber bundles align.
Reticular connective tissue
The reticular connective tissue occurs only in the secondary lymphatic organs ( lymph nodes , spleen , mucous membrane-associated lymphatic tissue ) and in the bone marrow. The task of this tissue is to provide a meeting place for free cells, especially cells of the immune system.
The fibroblasts of the reticular connective tissue are called fibroblastic reticular cells . They form a large three-dimensional network of reticular fibers . However, these are always surrounded by extensions of the reticular cells and have no contact with the intercellular space. This is in contrast to other types of tissue, in which reticular fibers also occur, but which are released into the intercellular space by the fibrocytes there.
Gelatinous (collagenous) connective tissue
Gelatinous connective tissue, also known as collagenous connective tissue, consists of flat, branched fibrocytes that form a wide-meshed network with one another. Gelatinous connective tissue is mainly found in the umbilical cord area, where it is also called Wharton's jelly . It also occurs in the pulp of young teeth. The extracellular matrix of the gelatinous connective tissue contains fine collagenous and reticular fibers as well as hyaluronic acid . The latter can bind a large amount of water, creating the gelatinous consistency that gave this type of connective tissue its name. The strong water retention ensures the protective function of the gelatinous connective tissue for the vessels in the umbilical cord , which must be secured against constriction without impairing their flexibility.
Spinocellular connective tissue
The spinocellular connective tissue is found in the cortex of the ovary . The fibrocytes are close to one another and are often arranged like a fish train. A few reticular fibers are found in the sparse intercellular substance. The theca cells, which form the theca folliculi , arise from the fibrocytes of the spinocellular connective tissue during the maturation of the egg cells in the ovary .
In some cases, the lining of the uterus, the endometrium , is also viewed as a form of spinocellular connective tissue.
Support fabric
Supporting tissue can in turn be divided into cartilage tissue and bone tissue .
Cartilage tissue
Cartilage tissue is a special form of connective tissue: it is firm, but elastic, can be deformed and cut. The cartilage-forming cells are called chondrocytes and form the cartilage matrix. This mainly contains type II collagen, but also other, rarer types of collagen. Furthermore, Aggrecan and, among other things, the hyaluronic acid bound to it ensure water storage, which is responsible for the consistency of the cartilage. Here, too, consistency plays an important role in function: cartilage has a shaping role, keeps the airways open and, in the form of joint cartilage, ensures reduced friction. In addition, most bones are initially created as cartilage models during development and only ossified later. With the exception of the fetal cartilage, cartilage is not supplied by nerves or blood vessels, but is nourished by diffusion from the cartilage skin ( perichondrium ).
There are three or four different types of cartilage:
- hyaline cartilage
- fetal cartilage (can also be viewed as hyaline cartilage with blood vessels )
- elastic cartilage
- Fiber cartilage
Bone tissue
Bone tissue consists of a calcified matrix (intercellular substance) that is formed by osteoblasts and broken down by osteoclasts. Osteoprogenitor cells (precursors of osteoblasts) and osteocytes also occur. Around one third of the bone matrix consists of organic matter (mainly collagen type I). Two thirds of the matrix consist of hydroxyapatite , a crystalline calcium salt that is responsible for the hardness of the bone tissue.
Bone tissue differs according to the internal order of cells and fibers in braided bones and lamellar bones. The osteocytes are irregularly distributed in the woven bone and the collagen fibers of the bone matrix are apparently disordered in coarse bundles. It is usually rebuilt into lamellar bone that appears to be ordered and consists of a compact outer layer and a spongy interior.
Illnesses and injuries
The wound healing proceeds from the connective tissue and also many immune responses play out, at least partially, in the connective tissue from. Typical connective tissue diseases are collagenoses in which the immune system directs itself unspecifically against the body's own cells. There are also a number of other diseases that specifically affect the connective tissue.
Acquired diseases
As already mentioned, a pronounced vitamin C deficiency leads to the clinical picture of scurvy .
The breakdown of collagen occurs in periods of hunger , immobilization or weightlessness , as well as in rheumatoid arthritis and prolonged, high-dose administration of cortisone .
In fibrosis and sclerosis , there is an increased collagen (type I) synthesis, which leads to functional restrictions or loss of the affected tissue.
Benign and malignant tumors also occur in connective tissue. Benign tumors are, for example, the fibroma or the lipoma , malignant tumors are summarized under the term sarcomas . In detail these are z. B. fibrosarcoma , liposarcoma or rhabdomyosarcoma .
Hereditary diseases
In the so-called glass bone disease ( osteogenesis imperfecta ) there is a gene mutation that leads to a disrupted formation of a collagen subunit or prevents it entirely. The result is a greatly increased tendency to break bones.
The group of diseases described with Ehlers-Danlos syndrome are also hereditary diseases. Due to an enzyme defect, collagen fibrils cannot be assembled correctly, which manifests itself in a tendency to injury and increased elasticity of the skin as well as overstretchability of joints.
The Marfan syndrome is a more or less pronounced instability all connective tissues of the body.
Web links
Individual evidence
- ↑ a b c Ulrich Welsch: Textbook Histology . 2nd Edition. Urban & Fischer at Elsevier, Munich 2006, ISBN 3-437-44430-1 , p. 108 .
- ^ A b Herbert Lippert: Textbook Anatomy . 7th edition. Urban & Fischer at Elsevier, Munich 2006, ISBN 3-437-42362-2 , p. 25 ff .
- ↑ Norbert Ulfig: Short textbook histology . 2nd Edition. Thieme, Stuttgart 2005, ISBN 3-13-135572-7 , p. 44 .
- ↑ Ulrike Bommas-Ebert, Philipp Teubner, Rainer Voß: Short textbook anatomy and embryology . 2nd Edition. Thieme, Stuttgart 2005, ISBN 3-13-135532-8 , p. 46 .
- ↑ J. Myllyharju, KI Kivirikko: Collagens, modifying enzymes and their mutations in humans, flies and worms . In: Trends Genet. . 20, No. 1, 2004, pp. 33-43. PMID 14698617 .
- ↑ Eble, JA: Antimetastatic Integrin Inhibitors . In: BIOspectrum . 6, 2009, pp. 621-623.
- ↑ Ulrich Welsch : Textbook Histology . 2nd Edition. Elsevier / Urban & Fischer , Munich 2006, ISBN 3-437-44430-1 , pp. 118 .
- ↑ a b c Werner Müller-Esterl : Biochemistry . 1st edition. Elsevier / Spektrum Akademischer Verlag , Munich 2004, ISBN 3-8274-0534-3 , pp. 126 ff .
- ↑ a b Ulrich Welsch: Textbook Histology . 2nd Edition. Elsevier / Urban & Fischer, Munich 2006, ISBN 3-437-44430-1 , pp. 121 .
- ↑ Norbert Ulfig: Short textbook histology . 2nd Edition. Thieme, Stuttgart 2005, ISBN 3-13-135572-7 , p. 41 .
- ↑ Ulrich Welsch: Textbook Histology . 2nd Edition. Urban & Fischer at Elsevier, Munich 2006, ISBN 3-437-44430-1 , p. 125 .
- ↑ Ulrich Welsch: Textbook Histology . 2nd Edition. Urban & Fischer at Elsevier, Munich 2006, ISBN 3-437-44430-1 , p. 126 .
- ↑ Norbert Ulfig: Short textbook histology . 2nd Edition. Thieme, Stuttgart 2005, ISBN 3-13-135572-7 , p. 47 .
- ↑ Ulrich Welsch: Textbook Histology . 2nd Edition. Urban & Fischer at Elsevier, Munich 2006, ISBN 3-437-44430-1 , p. 135 .
- ↑ Werner Böcker, Helmut Denk, Phillip U. Heitz (eds.): Pathology . 3. Edition. Urban & Fischer at Elsevier, Munich 2004, ISBN 3-437-44470-0 , p. 205 f .