Brain metastasis
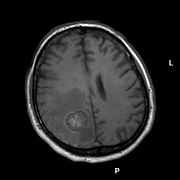
MRI with T2 flair weighting, the associated PET examination is shown below.
| Classification according to ICD-10 | |
|---|---|
| C79.3 | Secondary malignant neoplasm of the brain and meninges |
| ICD-10 online (WHO version 2019) | |
A brain metastasis is a settlement of cancer cells (metastasis) in the brain tissue that originates from malignant tumors outside the brain . Synonymous are the terms brain filia (from Latin filia "daughter") or cerebral metastasis (Latin cerebralis "belonging to the brain").
Common starting tumors are lung cancer , breast cancer , renal cell carcinoma and malignant melanoma . Brain metastases are the most common tumors of the malignant tumors that occur in the area of the brain and can manifest themselves as headaches, neurological deficits, seizures and changes in personality , among other things . Treatment and the chances of recovery depend on many factors, but brain metastases are usually a prognostically unfavorable condition.
Systematics
- A solitary brain metastasis is present if there is a single brain metastasis in addition to the original tumor (primary tumor) and there are no other metastases outside the central nervous system.
- In the case of a singular brain metastasis, on the other hand, there may be other metastases outside the central nervous system in addition to a single brain metastasis.
- Overall, multiple , i.e. multiple, brain metastases are more common .
The growth of tumor cells into the fluid spaces of the central nervous system in neoplastic meningiosis and the rare diffuse infiltration of the brain tissue by tumor cells of a non-brain tumor ( carcinosis ) must be distinguished from the solid brain metastases treated here .
frequency
Reliable epidemiological data on the frequency of brain metastases in German-speaking countries are not available. For the United States , the annual incidence has been estimated at about 8.3 per 100,000 population. There, brain metastases make up about half of all clinically diagnosed brain tumors . However, the number of brain metastases that remained undetected during their lifetime is probably higher: in a study from the 1960s, brain metastases were found autoptically in around 1.6% of all deceased and around 8% of all deceased with malignant tumors that were outside the central nervous system .
origin
The most common primary tumors in brain metastases are lung cancer (54–72%), breast cancer (20–34%), malignant melanoma, and renal cell carcinoma. In principle, however, any malignant tumor can metastasize to the brain. In children, colonization of rhabdomyosarcomas and germ cell tumors predominate . Brain metastases occur in approximately 20% of all lung cancer patients, 7% of all malignant melanoma patients, 7% of all renal cell carcinoma patients, 5% of all breast cancer patients, and 2% of colorectal cancer patients.
localization
Brain metastases are usually located in the area of the cerebrum , but can also occur in the cerebellum and brain stem . Most of the tumor cells reach the brain with the bloodstream (haematogenic metastasis). The extravasation, i.e. the leaving of the vessels, occurs on the arteriolar or capillary level, which is why the tumor colonization preferably occurs at the border between the cerebral cortex and the medullary bed . A special case is the metastasis of malignant tumors in pre-existing benign brain tumors.
Symptoms
Brain metastases can become noticeable before the primary tumor becomes clinically apparent. About one third of the patients are not known to have a tumor at the time of diagnosis. In individual cases, the primary tumor remains hidden despite an intensive search ( Cancer of Unknown Primary ). On the other hand, brain metastases can still occur years after the occurrence and treatment of a cancer disease (metachronically).
Overall, the symptoms of brain metastases correspond to those of malignant brain tumors such as glioblastoma . Since most brain metastases grow rapidly and tissue swelling in the area ( perifocal edema ) develops, life expectancy is only a few weeks to a few months if left untreated.
A common but unspecific symptom is headache . The reason for this is the space-occupying effect of metastasis and edema, which can lead to stretching of the pain-sensitive meninges .
Further neurological symptoms occur depending on the localization: if the brain metastasis is in the area of the cerebrum, epileptic seizures , paresis , sensory disorders , visual field defects or speech disorders can occur. Changes in personality and mood (for example in the case of frontal brain syndrome ) are not infrequently also noticeable to the bystanders. Sometimes an acute organic psychosyndrome develops with paranoid or aggressive features in the sense of delirium . If it is located in the area of the cerebellum or the brain stem, dizziness , ataxia or brain stem syndromes can occur.
An increase in intracranial pressure can lead to apathy , tiredness and clouding of consciousness. Insatiable vomiting or coma are late signs with a poor prognosis.
Diagnosis
Clinical examination
In the case of neurological symptoms or complaints that suggest the possible presence of brain metastases in view of a known cancer, the targeted neurological examination plays an important role. Among other things, we are looking for signs of intracranial pressure ( congestive papilla ), cranial nerve failure and central paralysis, which are noticeable through increased muscle tone and accentuated self-reflexes , sometimes also through signs of the pyramidal tract . Psychological changes, slowing down or disturbances of the experience are often already noticeable in the anamnesis discussion .
Imaging
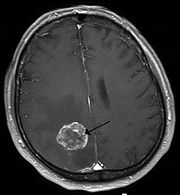
The core of the diagnostics are imaging processes , whereby magnetic resonance imaging (MRT) is superior to computed tomography (CT).
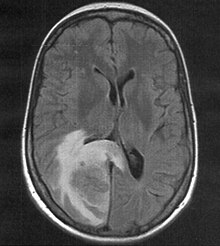
Computed tomography Computed
tomography, as a method that can be carried out quickly and is widely available, plays a role primarily in emergency medicine . Larger metastases distinguish themselves from the normal brain parenchyma as hypodense or rarely (malignant melanoma, chorionic carcinoma) hyperdense structure. Since metastases can also be isodense , it is possible that only the space- occupying effect as a mass displacement or the hypodense formation of the perifocal edema can be defined. Central hemorrhage, as it occurs in particular with metastases from malignant melanoma or renal cell carcinoma, is easily detectable on CT. Depending on the selected layer thickness, the detection limit is around one centimeter, so that smaller metastases can escape native computed tomography. Since computed tomography shows a relatively low soft tissue contrast , the administration of contrast medium is crucial: due to the disruption of the blood-brain barrier in the area of the metastasis, contrast medium accumulates (enhancement) , which is often ring-shaped or garland-shaped in the presence of central necrosis appears.
Magnetic resonance tomography Magnetic resonance
tomography has a significantly higher sensitivity with better soft tissue differentiation , especially after administration of gadolinium as a contrast medium, and is therefore more suitable for searching for brain metastases. Compared to a CT scan, the rate of patients with brain metastases detected by MRI is more than twice as high. This is especially true for very small findings and metastases in the area of the posterior fossa. Magnetic resonance imaging can be used for differentiation from brain abscesses and other potentially similar lesions imposing a nuclear magnetic resonance spectroscopy to be supplemented.

Positron emission tomography
The positron emission tomography (PET) as a functional imaging technique (they are, to put it simply, the metabolic activity figuratively again) allows the answers to specific questions. Such would be, for example, the distinction of a local recurrence of a Strahlennekrose under treatment, if this differentiation can not be derived from the MRI alone.
Angiography
Today angiography only plays a subordinate role in metastasis diagnosis, but it can be useful in individual cases for surgical planning.
CSF diagnostics
In the case of metastases on the brain surface, tumor cells can spread into the fluid spaces of the central nervous system, which is referred to as neoplastic meningiosis. In the nerve fluid ( liquor cerebrospinalis ) obtained by lumbar puncture , tumor cells can then be detected whose cytology and immunohistochemical expression profile often allow conclusions to be drawn about the primary tumor.

Diagnosis of an unknown primary tumor
If no underlying cancer is known when brain metastases are detected, the first thing to do is to find the primary tumor. The examination program includes a thorough examination of the skin, an X-ray of the chest , sonography and / or computed tomography of the thorax, abdomen and pelvis, in women a gynecological examination and a mammography and, if there is justified suspicion, a bronchoscopy with bronchoalveolar lavage , possibly also the positron emission -Tomography or skeletal scintigraphy . Laboratory tests for elevated tumor markers are rather unspecific and usually do not help.
If no primary tumor is found, a tissue sample can be surgically removed to confirm the diagnosis, which is usually done by means of a stereotactic biopsy . With a mortality of less than 1%, a histological diagnosis can be made in up to 96% of cases .
Differential diagnostics
The differential diagnosis to consider in addition to malignant primary brain tumors and lymphoma, inflammatory diseases of the brain, the clinic and imaging may resemble those of brain metastases. It is not uncommon for inflammatory foci in toxoplasmosis or solitary inflammatory foci of demyelinating to be operated on with clinical suspicion of brain metastasis. Septic-embolic brain abscesses , which can occur with haematogenous spread from an inflammatory focus (for example, an infected heart valve in endocarditis ), are sometimes difficult to differentiate from metastases. Benign brain tumors such as meningiomas , which are found by chance in the course of tumor staging, must also be distinguished.
If further imaging (magnetic resonance imaging, spectroscopy) and additional examinations (liquor removal) do not clarify the matter, a biopsy is also indicated here.
pathology

The neuropathological examination of the surgical material obtained by stereotactic biopsy or resection serves to confirm the diagnosis and to exclude other diseases whose clinical and radiological picture is similar to that of a brain metastasis. Since brain metastases can also primarily make themselves felt as a cerebral haemorrhage, material obtained during the neurosurgical clearing out of cerebral haemorrhages is always examined for the presence of tumor components.
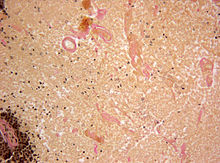
Histology
The histology of brain metastases often resembles that of the primary tumor and can thus provide initial clues as to their origin. A characteristic feature of brain metastases is the relatively clear delimitation of the tumor from the surrounding brain tissue, which is infiltrated by the tumor in the shape of a cone.
Immunohistochemistry
Especially when a brain metastasis is the only recognizable manifestation of cancer so far, immunohistochemical examinations can provide valuable information on the localization of the primary tumor. Here, expression patterns of proteins that are relatively typical for the various primary tumors are examined.

For example, a group of immunohistochemical markers is used for brain metastases from adenocarcinomas , including the cytokeratin subtypes CK7 and CK20, the thyroidal transcription factor 1 (TTF1) and the prolactin-induced protein (PIP, GCDFP-15).
In the case of metastases from malignant melanomas that have no melanin pigment , their melanosomal differentiation can be detected by staining for melanosomal antigens (melanA and HMB45).
| Primary tumor | Expression profile |
|---|---|
| Lung cancer | CK7 +, CK20–, TTF1 +, GCDFP15–, melanosomal antigens– |
| Breast cancer | CK7 +, CK20–, TTF1–, GCDFP15 +, melanosomal antigens– |
| Colon cancer | CK7–, CK20 +, TTF1–, GCDFP15–, melanosomal antigens– |
| Malignant melanoma | CK7-, CK20-, TTF1-, GCDFP15-, melanosomal antigens + |
Therapy and prognosis
Therapy and prognosis are closely linked, since on the one hand the prognostic factors determine which therapy options are possible, and on the other hand the choice of therapeutic method has a significant impact on life expectancy.
There are various therapeutic methods that are used for brain metastases. Which method is used depends, among other things, on the number, location and size of the brain metastases as well as the primary tumor. The general condition of the patient, which has a decisive influence on the prognosis and thus also the selection of the procedure, is also important. Patients in poor general condition tolerate invasive procedures such as surgical removal of the brain metastases less well than patients in good general condition. With the help of the Karnofsky index , the general condition can be objectified and compared. If possible, surgical, radio and chemotherapeutic procedures are combined.
Symptomatic therapy
Glucocorticoids lead to a regression of the edema to a reduction of the pressure on the surrounding brain tissue (mass effect) and thus to an alleviation of the symptoms; life expectancy is increased to an average of one to two months without further measures. Treatment is usually with dexamethasone , initially with relatively high doses of up to 24 milligrams per day. It will be reduced as soon as possible, as long-term use of glucocorticoids can lead to Cushing's syndrome . In the case of emergency treatment with glucocorticoids, its diagnosis is made more difficult if a lymphoma is also a possible differential diagnosis.
Epileptic seizures that are symptomatic of brain metastases are treated with anti-convulsive drugs ( anticonvulsants ). In contrast to occasional seizures, long-term treatment is started here after the first seizure event, as there is a high risk of recurrence. Symptomatic treatment also includes the administration of analgesics for headaches and anti-emetics when nausea and vomiting occur.

surgery
If the general condition of the patient is sufficiently good, solitary and singular brain metastases are completely surgically resected if possible . The general condition of the patient, the stage of the tumor disease and the surgical accessibility of the brain metastasis are essential for the decision to operate. If the above-mentioned conditions apply, surgery can also be performed in individual cases with two or three easily accessible metastases. Brain metastases from small cell lung cancer are generally not operated on because they respond well to radiation and chemotherapy.
If the CSF pathways ( hydrocephalus ) are blocked due to a shift in mass, the drainage of the CSF via an internal or external drainage may be considered.
Radiosurgery
Under radiosurgery refers to the application of a high radiation single dose percutaneously (through the skin) and stereotactically is applied. It can represent an alternative to conventional surgery up to a metastasis diameter of three centimeters and is also used in patients who are inoperable due to a poor general condition or the location of the metastasis (for example in the brain stem). Depending on the size of the metastasis treated, doses between 15 and 24 Gray are tolerated.
Whole brain radiation
The whole brain radiation therapy is an important treatment option as part of the treatment regimen of brain metastases. The irradiation is usually fractionated , i.e. in several individual doses with a total dose of 30 to 45 Gray, and covers the entire brain including the base of the skull and the first two cervical vertebrae. In individual cases a complete disappearance of the brain metastases could be achieved. Whole-brain irradiation can be used as an adjuvant therapy to supplement other forms of therapy that are the sole form of therapy or can also be used prophylactically .
In the case of solitary or singular brain metastases, whole-brain irradiation can be carried out adjuvantly after surgical removal of the brain metastases or stereotactic radiosurgery. Randomized studies are currently investigating whether additional whole-brain irradiation offers a survival advantage compared to surgery alone. In the presence of multiple metastases, whole-brain irradiation can be used in addition to surgery or as the sole form of therapy. Prophylactic whole-brain irradiation can reduce the incidence of symptomatic brain metastases in patients with small-cell lung cancer and increase survival time even in advanced disease.
Whole-brain irradiation can lead to various side effects and complications such as edema formation. Particularly in the case of larger metastases, there is a risk of serious neurological deficits due to the pressure of the edema on neighboring structures. The administration of glucocorticoids can reduce the extent of the edema and thus the side effects.
chemotherapy
Most tumors that metastasize to the brain are not very sensitive to chemotherapy , which therefore only plays a minor role in the treatment of brain metastases. Important exceptions to this are small cell bronchial carcinoma, breast carcinoma, chorionic carcinoma and germ cell tumors. The same cytostatics are usually used that are used for metastases outside the brain. In many patients, chemotherapy produces a temporary response, but overall life extension is small.
forecast
A general statement on the prognosis for brain metastases is not possible because it is influenced by various factors. The most important forecasting factors are
- the restriction in activities of daily living due to the tumor disease, measured in the Karnofsky index ,
- the age of the patient,
- control of the primary tumor,
- the time interval between the occurrence of the primary tumor and the brain metastasis,
- the histology of the primary tumor,
- the number, location and size of brain metastases as well
- the presence and extent of metastases outside the brain.
In general, metastatic cancers are considered incurable, with the exception of some germ cell tumors. The overall prognosis for metastases in the brain is poor. If left untreated, survival times range from a few weeks to a few months. Rapid deterioration with sudden death can result from massive bleeding into a metastasis or from acute cerebrospinal fluid build-up. Metastases of the posterior fossa (cerebellum and brain stem) lead to entrapment and thus death , even if the size increases . If the patient responds, the optimal therapy allows an improvement in the quality of life and an extension of survival, in individual cases by several months to several years.
Veterinary medicine
Brain metastases also occur in animals. Especially in small pets ( dogs and cats ) an increase in brain metastases has been observed in veterinary medicine since the mid-1980s , which is mainly attributed to more refined examination methods. A more recent study concludes that more than 60% of all tumors found in the brain are of metastatic origin. In percentage terms, dogs seem to be affected somewhat more often than cats. The most common primary tumors are sarcomas (fibro-, osteo-, chondro- and hemangiosarcomas). Brain metastases from carcinomas of the mammary gland , lungs , nose and kidneys as well as lymphatic tumors also occur.
Research history
The possibility of brain metastases forming has been known for several centuries. The importance of brain metastases was significantly underestimated, especially with regard to their frequency until the late 19th century. Their occurrence was rated as rare and unusual. The first significant publications go back to the British doctors William Richard Gowers and Byrom Bramwell in 1888. Gowers published a classification in which the causes of intracranial growth were divided into six categories and ordered according to frequency. Brain metastases were represented in third place as a subgroup of carcinomas. Bramwell recognized that brain metastases can in principle originate from any malignant tumor, a view that is still undisputed today. In addition, Bramwell underlined the importance of brain metastases by the potential growth in brain tissue with the growth of microorganisms on the 1882 environment of Robert Koch arisen agar - medium compared. The first clinical-pathological study was carried out by Globus and Selinsky in 1927. They described typical symptoms and pathological changes that occur with brain metastases. The knowledge about the properties of brain metastases is still partly based on these early publications and has been continuously expanded through numerous research projects.
literature
Textbooks
- Mitchel Berger , Michael Prados (Eds.): Textbook of neuro-oncology. 1st edition, Elsevier, Philadelphia 2005, ISBN 0-7216-8148-4 .
- Uwe Schlegel, Michael Weller and Manfred Westphal: Neuro-oncology. 2nd edition, Thieme, Stuttgart 2003, ISBN 978-3-13-109062-1 .
- Wolfgang Wick and Michael Weller: Brain Metastases. In: Thomas Brandt, Johannes Dichgans and Hans Christoph Diener (eds.): Therapy and course of neurological diseases. 5th edition, Kohlhammer, Stuttgart 2007, ISBN 978-3-17-019074-0 .
Guidelines
- S2k guidelines for brain metastases and meningiosis neoplastica of the German Society for Neurology (DGN). In: AWMF online (as of 2014)
Web links
- Guidelines for the Neuro-Oncological Working Group on Metastases and Meningeosis neoplastica (Status 2014; PDF; 245 kB)
Individual evidence
- ^ A b Uwe Schlegel, Michael Weller, Manfred Westphal: Neuroonkologie . Thieme, Stuttgart 2003, ISBN 978-3-13-109062-1
- ↑ Brain metastases: migration of cancer cells into the central nervous system , Cancer Information Service of the German Cancer Research Center (DKFZ), Heidelberg. Dated March 5, 2007. Last accessed September 4, 2014.
- ↑ Walker et al .: Epidemiology of brain tumors: the national survey of intracranial neoplasms. In: Neurology. Volume 35, Number 2, February 1985, pp. 219-226, ISSN 0028-3878 . PMID 3969210 .
- ↑ Jänisch et al .: About the frequency and origin of metastases in the central nervous system. In: German journal for neurology. Volume 189, Number 1, June 1966, pp. 79-86, ISSN 0367-004X . PMID 5982815 .
- ^ Paul: Brain metastases. In: Neuropathology, edited by Pfeiffer, Schröder and Paulus. Springer publishing house. 2nd Edition. Berlin 2002 ISBN 3-540-41333-2
- ↑ Barnholtz-Sloan et al .: Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. In: Journal of Clinical Oncology . Volume 22, Number 14, July 2004, pp. 2865-2872, ISSN 0732-183X . doi : 10.1200 / JCO.2004.12.149 . PMID 15254054 .
- ↑ Jarrell et al .: Metastases to hemangioblastomas in von Hippel-Lindau disease. In: Journal of Neurosurgery . Volume 105, Number 2, August 2006, pp. 256-263, ISSN 0022-3085 . doi : 10.3171 / jns.2006.105.2.256 . PMID 17219831 .
- ^ Seute et al .: Detection of brain metastases from small cell lung cancer: consequences of changing imaging techniques (CT versus MRI). In: Cancer . Volume 112, Number 8, April 2008, pp. 1827-1834, ISSN 0008-543X . doi : 10.1002 / cncr.23361 . PMID 18311784 .
- ↑ Poptani et al .: Characterization of intracranial mass lesions with in vivo proton MR spectroscopy. In: AJNR. American journal of neuroradiology. Volume 16, Number 8, September 1995, pp. 1593-1603, ISSN 0195-6108 . PMID 7502961 .
- ↑ Chen: Clinical applications of PET in brain tumors. In: Journal of nuclear medicine: official publication, Society of Nuclear Medicine. Volume 48, Number 9, September 2007, pp. 1468-1481, ISSN 0161-5505 . doi : 10.2967 / jnumed.106.037689 . PMID 17704239 .
- ↑ Kretzschmar et al .: The Value of Computed Tomography and Angiography for Diagnosing Supratentorial Brain Tumors. In: Neuroradiology. Volume 16, 1978, pp. 487-490, ISSN 0028-3940 . PMID 745745 .
- ^ WA Hall: The safety and efficacy of stereotactic biopsy for intracranial lesions. In: Cancer. Volume 82, Number 9, May 1998, pp. 1749-1755, ISSN 0008-543X . PMID 9576298 .
- ↑ Omuro et al .: Pitfalls in the diagnosis of brain tumors. In: The Lancet Neurology . Volume 5, Number 11, November 2006, pp. 937-948, ISSN 1474-4422 . doi : 10.1016 / S1474-4422 (06) 70597-X . PMID 17052661 .
- ↑ JJ Kepes: Large focal tumor-like demyelinating lesions of the brain: intermediate entity between multiple sclerosis and acute disseminated encephalomyelitis? A study of 31 patients. In: Annals of neurology. Volume 33, Number 1, January 1993, pp. 18-27, ISSN 0364-5134 . doi : 10.1002 / ana.410330105 . PMID 8494332 .
- ^ B. Licata, S. Turazzi: Bleeding cerebral neoplasms with symptomatic hematoma. In: Journal of neurosurgical sciences. Volume 47, Number 4, December 2003, pp. 201-210, ISSN 0390-5616 . PMID 14978474 .
- ↑ Park et al .: Panels of immunohistochemical markers help determine primary sites of metastatic adenocarcinoma. In: Archives of Pathology & Laboratory Medicine , Volume 131, Number 10, October 2007, pp. 1561-1567, ISSN 1543-2165 . doi : 10.1043 / 1543-2165 (2007) 131 [1561: POIMHD] 2.0.CO; 2 . PMID 17922593 .
- ↑ Drlicek et al .: Immunohistochemical panel of antibodies in the diagnosis of brain metastases of the unknown primary. In: Pathology, research and practice. Volume 200, Number 10, 2004, pp. 727-734, ISSN 0344-0338 . doi : 10.1016 / j.prp.2004.09.002 . PMID 15648611 .
- ↑ Mazoujian et al .: Immunohistochemistry of a gross cystic disease fluid protein (GCDFP-15) of the breast. A marker of apocrine epithelium and breast carcinomas with apocrine features. In: The American Journal of Pathology . Volume 110, Number 2, February 1983, pp. 105-112, ISSN 0002-9440 . PMID 6130702 . PMC 1916150 (free full text).
- ↑ Wen et al .: Treatment of brain metastases in favorable prognosis patients . UpToDate August 2007.
- ↑ a b c DGN guidelines: Solid brain metastases . Status: 2008 ( online version )
- ↑ Drappaz et al .: Management of vasogenic edema in patients with primary and metastatic brain tumors . UpToDate August 2007.
- ↑ J. Lokich, H. Levine, I. Nasser: malignancy-related hydrocephalus: clinical features and results of ventricular peritoneal shunt procedure in three patients. In: American Journal of Clinical Oncology . Volume 21, Number 4, August 1998, pp. 366-368, ISSN 0277-3732 . PMID 9708635 .
- ↑ Astner et al .: Radiotherapy of intracerebral metastases. The Oncologist 2008; 14: 246-254
- ↑ JG Cairncross, NL Chernik, JH Kim, JB Posner: Sterilization of cerebral metastases by radiation therapy. In: Neurology . Volume 29, Number 9 Pt 1, September 1979, pp. 1195-1202, ISSN 0028-3878 . PMID 225696 .
- ^ European Organization for Research and Treatment of Cancer: Adjuvant Radiation Therapy in Treating Patients With Brain Metastases. ClinicalTrials.gov Identifier: NCT 00002899
- ↑ Slot et al .: Prophylactic cranial irradiation in extensive small-cell lung cancer. In: The New England journal of medicine . Volume 357, Number 7, August 2007, pp. 664-672, ISSN 1533-4406 . doi : 10.1056 / NEJMoa071780 . PMID 17699816 .
- ^ Koestner & Higgins: Metastatic tumors of the central nervous system. In Pack DJ: Tumors in Domestic Animals. Blackwell, 2002: 737-738 ISBN 0-8138-2652-7
- ^ Raymond Sawaya: Intracranial Metastases: Current Management Strategies . Wiley-Blackwell 2004, ISBN 1-4051-1646-3