Dental implant
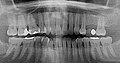
A dental implant (from Latin implantare 'to plant' ) is an "alloplastic prefabricated part" ( implant ) inserted into the jawbone . The branch of dentistry that deals with the insertion (insertion) of dental implants into the jawbone is called implantology (from the Greek λόγος lógos , word , teaching '). Because they can be used as a carrier for dentures , dental implants take on the function of artificial tooth roots . To do this, they are either screwed into the jawbone (endosseous implants) using screw threads or inserted. They combine with the surrounding bone within 3 to 6 months to form a solid, extremely resilient carrier unit ( osseointegration ).
The surgical insertion technique depends on the shape of the implant. The design of the abutment , the part of the implant protruding from the jawbone, results in the production of the superstructure , the dentures to be incorporated on the implants. Dental implants have usually been made of titanium since the 1980s , but also of ceramic materials or plastic (PEEK) .
Implant systems and shapes
There are around 80 major manufacturers and 200 to 300 different types of implants worldwide.
Titanium implants
After many decades with various, now sometimes naive-looking, implant shapes from the pre-war period, rotationally symmetrical implants (mostly screw implants) have established themselves . In these implants, the implant body is circular in cross section, so that the implant cavity, the cavity that is intended to receive the implant, can be prepared in the jawbone with rotating instruments , for example a cannon drill. The screw implants differ mainly in their conicity and the type of thread .
This surgical approach puts less stress on the patient than previous implantation techniques and very rarely leads to complications in wound healing. In addition, screw implants have the advantage that, thanks to their thread , they “fix” themselves immediately in the bone (primary stability). This shortens the healing time because only a small amount of bone has to "grow back". In some of the implants, the cylindrical basic shape tapers apically towards the end, so that a conical shape is created overall .
In contrast to orthopedics , in which titanium alloys are primarily used, dental implants are made from pure titanium . Titanium has a high level of biocompatibility , which does not trigger any allergic or foreign body reactions . In contrast to other materials, titanium forms a direct molecular bond with the bone. The rough, morphological surface design with an average micro-pore depth of 5 to 100 µm plays a key role here. At the beginning, this was achieved by spraying on ("additive process") titanium powder under argon and high temperature (titanium plasma spray "TPS"). This process is relatively expensive, so that many manufacturers have been using the cheaper acid etching process ("acid etching" or combinations thereof, called "SLA") using a mixture of hydrochloric acid and sulfuric acid ("subtractive process") since the year 2000. ), which is equivalent or even superior to the additive method.
The property of titanium to form a protective oxide layer on the surface with oxygen is the reason for its particularly good compatibility. Both methods have a high success rate (over 95% with a five-year stay). Implants must be certified by the health authorities as safe medical devices ( CE or FDA approval). Exceptions exist in accordance with the Medical Devices Act (MPG) for individual implants that are made for a single patient on the prescription of the dentist.
Compound dental implants have prevailed mainly because they can be best adapted to the given conditions due to the possibility of combining the root and crown portion, and because the two-stage procedure ensures that the osseointegration of the implant is not impaired by too early loading. Multi-part implants consist of the implant body anchored in the bone , more rarely a separate neck part located in the area of the oral mucosa and the head part , the abutment, which accommodates the superstructure. The two or three parts are usually screwed together. The superstructures (crowns, bridge or prosthesis anchors) attached to it are screwed, cemented or glued.
With one-piece dental implants , the implant head protrudes from the mucous membrane, which means that premature loading during the healing phase can often not be avoided.
Hollow cylindrical implants
The hollow cylinder implants (also known as cup implants) developed in the 1980s were intended to enlarge the osseointegrating surface, but they have not proven successful, as the bone portion in the cylinder had led to complications due to insufficient blood flow. In modified form as short implants with a wide diameter and with new surgical technology, they are currently experiencing a renaissance.
Leaf implants
In addition to these cylindrical implants with or without screw thread, there are also flat, leaf-shaped implants (extension implants) that are sunk along the course of the bones of the jaw into an approx. 1 mm wide slit of 4 to 14 mm length prepared there and grow into it. These implants also have perforations through which the bone can also grow horizontally.
Narrow jaw implants
Narrow jaw implants, also known as mini implants, are 1.8 to 3.1 mm in diameter. Individually, they are only suitable for small tooth gaps and are subject to indication restrictions, e.g. B. in the posterior region. Because of the rapid dimension-related fatigue during mastication they are usually constructed in one piece. An improved bionic design as well as high quality titanium gradations or titanium alloys lead to a renewed increased use z. B. in geriatric prosthetics. After diagnostic work-up, they are used for minimally invasive and one-step surgical procedures. The technique, which is still controversial today, is prosthetically mostly provided with primary interlocking (bar) or secondary interlocking with various anchor systems. The target group for such procedures are patients who, after taking a detailed anamnesis, cannot undergo a more complex conventional implant treatment from an anatomical, psychological or financial point of view. The therapeutic value of narrow jaw implants is undisputed. B. for temporary use in orthodontics , for intraoral fixation of drilling templates or as auxiliary implants for extensive provisional implant restorations.
Disc implants
Disk implants belong to the group of BASAL implants. They have the shape of a skeleton cylinder and are inserted into the side of the jaw. The hold takes place in the hard and well-perfused outer wall of the bone. Disc implants can be loaded immediately under certain circumstances. Due to their special shape, they should ensure stable healing even with low bone height or advanced jaw resection.
Subperiosteal implants
The subperiosteal implants lie as large as possible under the mucous membrane directly on the bone . They were mainly used in cases of severe bone loss, when the jawbone was too flat or too narrow for cylinder or extension implants . The mere placement of the flat subperiosteal implant under the periosteum ( periosteum ) often led to extensive inflammation with e.g. In some cases, considerable extensive bone meltdowns, because there is naturally no effective protection against infection through a bacteria-proof seal at the point of passage of the head part.
Although there have been great successes with subperiosteal implants in the USA (over 95% after five years in the case of unilateral mandibular implants), their scientific development has not been advanced in Germany. The reason is essentially that the findings of bone biology with regard to the reliable regeneration of bone tissue open up the possibility of inserting cylinder implants through suitable surgical jaw augmentation procedures even in cases of scarce bone supply. There is no manufacturer of subperiosteal framework implants in Germany.
Ceramic implants
The pure ceramic implants used previously were characterized by excellent ingrowth. However, fractures occurred very often because the ceramic is brittle (higher modulus of elasticity ) and is subject to aging processes. As a biological tissue, bone enables more or less pronounced bends that ceramics cannot. Therefore this group of materials has largely been abandoned.
Zirconium (IV) oxide
Because of cosmetic problems with regression of the gums and bones, zirconium (IV) oxide (ZrO 2 ) (also known as zirconium dioxide or with the common name zirconium oxide, colloquially incorrectly referred to as " zircon ") is used as an implant material. Zirconium (IV) oxide is said to be characterized by tissue compatibility comparable to titanium. There are still no scientific studies on the amount of the removal torque, a parameter that provides information about the degree of osseointegration of the implant body. More recent experience reports, however, show extensive bone-dissolving inflammation and a loss rate of over 50% in the 2-year period. In comparison to the use of titanium implants, these numbers are completely unacceptable and were the reason for the end of the so-called Tübingen or Munich implants years ago . These, too, were made of ceramic and had a failure rate of over 30%, because the mechanism inherent in the titanium crystal, namely the reversible ionic binding of bone calcium, is missing in zirconium (IV) oxide and other ceramics. This integration with titanium is bacteria-proof.
Ceramic compatibility during bone healing is said to be improved by coating the implants with bone-related materials (artificial bone mineral, i.e. hydroxyapatite ) or calcium phosphate (TCP). The previous attempts have so far shown no advantage in terms of accelerated osseointegration. On the contrary, the hydroxyapatite led to meltings in the bone bed with subsequent loss of the implant. Even tricalcium phosphate coatings have so far not brought any advantages over the pure titanium surface with regard to faster “healing”.
Cytokines
More recent approaches coat the implant surface with proteins that are intended to stimulate and promote bone formation on the implant. It remains to be seen whether these attempts will ultimately prevail and whether they will accelerate osseointegration. The as yet unexplained overall effect of these special proteins ( cytokines ) on other areas of the organism's biology puts a clear question mark behind these experiments, because there are initial indications of fatal liver damage. The cytokines used here, especially BMP 2, by no means only have a special bone-promoting effect, but act elsewhere as a trigger for controlled cell death ( apoptosis ). Their effect is increased significantly (20-fold) above all by the influence of the blood coagulation inhibition by heparin .
Ultimately, however, with the success rate of consistently over 95% of the most common types of implants without artificial mineral or protein deposits, there is hardly anything that can be improved. The causes of the remaining 3–4% loss cannot be scientifically traced back to the surface design or the shape of the implant.
Distribution of indications for dental implants
In partially edentulous patients (> 90%), implants are the most common indication, with single tooth gaps being the most common indication for implant treatment with over 50%. Augmentation techniques were also used in around 40% of the cases, in the form of membrane techniques or sinus floor elevation. The frequent use of both augmentation techniques means that 53% more implants were placed in the upper jaw than in the lower jaw.
A Swiss study by the University of Bern shows the following distribution:
- Single tooth gaps 51.6%
- Free-end situations 23.5%
- Gaps 16.9%
- Edentulous jaws 8%
Consensus conference on implantology
The consensus conference on implantology , a cooperation between two professional associations ( Federal Association of Dental Implantologists, BDIZ, Professional Association of German Oral Surgeons, BDO), two scientific specialist societies ( German Society for Implantology , DGI, German Society for Dental Implantology , DGZI) and an association that is both professional association as well as a scientific society ( German Society for Oral and Maxillofacial Surgery , DGMKG), has defined the indication classes for implants (as of October 7, 2014).
The optimal therapy for tooth loss is the replacement of each individual tooth with an implant. As a rule, the 8th tooth of a quadrant does not need to be replaced and the necessity of replacing the 7th tooth must be critically assessed on an individual basis. Since this optimum cannot always be achieved for a variety of reasons (especially anatomical, economic), the following standard cases are set up.
Indication classes
Standard care provides for the following classes of indications:
- Class I: single tooth replacement
- Class II: Reduced remaining teeth
- Class II a: free-end situation
- Class III: Toothless jaw
Definition of the standard care
Front teeth
- Class I a:
- If up to four teeth are missing from the maxillary anterior, the neighboring teeth are clinically intact: 1 implant per missing tooth.
- If up to four teeth in the lower anterior are missing and the neighboring teeth are clinically intact: 2 implants are intended to replace the missing teeth.
Posterior dentures
- Class I b:
- If teeth from the closed row of teeth are missing in the posterior area, each missing tooth should be replaced by an implant in neighboring teeth that do not require treatment.
- Class II:
Reduced residual dentition Principle: In the case of implantological restoration of the reduced residual dentition, the dentition of the opposing jaw must be taken into account in the planning. In addition, the rules of conventional prosthetics apply
Free-end situation
- Class II a:
- Teeth 7 and 8 are missing: no indication for implantation
- Teeth 6–8 missing: 1–2 implants
- Teeth 5–8 missing: 2–3 implants
- Teeth 4–8 missing: 3 implants
Toothless jaw
- Class III:
- For the anchoring of a fixed denture: 8 implants in the toothless upper jaw, 6 implants in the toothless lower jaw.
- For anchoring a removable denture: 6 implants in the upper jaw, 4 implants in the lower jaw.
The definitive number of implants always depends on the respective situation and position of the natural teeth, so that the final decision is made by the practitioner in consultation with his patient.
With the help of computed tomography (CT) or digital volume tomography ( DVT), the position of the implant can be determined before the procedure. Planning takes place three-dimensionally on the computer and is implemented using an individually manufactured drilling template. The radiation exposure and the additional costs for the patient are disadvantageous here.
Possible complications
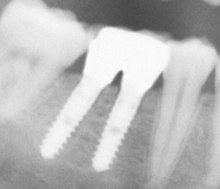
The main complications are all factors that promote infection in the implantation area. Dental implants are at risk of peri-implantitis , an inflammation of the bone tissue around the dental implant. The cause can be traced back to either surgical errors or poor oral hygiene on the part of the patient. Peri-implantitis leads to bone loss that ultimately causes the implant to fail. Tooth implantation is considered a failure if the implant is mobile or has peri-implant tissue shrinkage of more than 1 mm in the first year. Peri-implantitis can be treated with prophylactic measures together with antibiotic therapy. Peri-implantitis can be seen on an X-ray.
With assembled implants there are gaps and cavities between the actual implant and the abutment, into which germs from the oral cavity can penetrate. These germs later find their way back into the adjacent tissue and can thus cause peri-implantitis. As a prophylaxis, these implant interiors should be sealed.
Diabetics must be well adjusted so that the risk of inflammation in the teeth is reduced to a manageable level.
In patients who have to undergo chemotherapy , not only is the immune defense restricted, but also the ability of the tissue to regenerate during the healing phase after the implantation. Therefore, in these patients, the end of the chemotherapy should be awaited and implanted a few months later.
Bedridden patients can possibly be provided with implants if the procedure is performed in an inpatient setting.
Treatable periodontitis is not an exclusion criterion.
The risk of failure is increased for smokers. However, failure can also occur if the implant has not been correctly positioned.
Removal of the implant
Contraindications
There are numerous contraindications to implant restoration.
General medical contraindications
- Cachexia
- severe obesity
- medication
- Haematological diseases
- Cardiovascular disease
- Collagenoses
- Osteogenesis imperfecta
- Condition after radiation
- Unsanitary dentition
- osteoporosis
Bisphosphonates
An uncontrollable complication has been known about since 1999 in patients who have been treated for osteoporosis or cancer with an active ingredient from the bisphosphonate group . After dental surgery, atrophy (regression) of the bone tissue occurs in the surgical area, selectively in the area of the jawbone . The cause has not yet been clarified. It is still unknown whether it is the combination of chemotherapy and bisphosphonates that causes this phenomenon. At present, all types of oral surgery, including tooth extractions , when taking bisphosphonates at the same time, are contraindicated . It is not known how long it takes bisphosphonates to lose their destructive effects in the bone after they are discontinued. Like tetracyclines, they are stored in the bones. It can take up to 10 years since hydrolysis via phosphatases does not take place due to the molecular structure. The intake of bisphosphonates requires a strict indication because of this serious undesirable side effect.
Jaw augmentation
Ridge build-up or jaw augmentation is understood to mean surgical procedures that serve in particular to rebuild degraded alveolar bones in toothless parts of the upper or lower jaw. For this purpose, bone substitute material is applied to the resorbed remaining alveolar ridge. For a height of more than 3 mm, the body's own bone grafts are fixed to the jawbone and then have to heal for months. The bone loss of the jawbone can occur through tooth loss, periodontitis or through the pressure applied by dentures.
Bone quality
Bone quality is of crucial importance for osseointegration. It results from the relationship between the dense compacta and the less dense cancellous bone . The latter is interspersed with numerous cavities. The spongiosa lies inside the bone and is enveloped on the outside by the cortex (substantia compacta). The bone marrow is located in the cavities of the “sponge” formed by the cancellous bone , so that there is less mechanical contact with the implant than with the dense bone of the outer bone layer (compacta). The cancellous bone is an important place for new bone formation and above all for blood formation .
The bone quality is divided into classes, whereby in addition to the classification according to Carl E. Misch, the following classification has prevailed:
| class 1 | Almost exclusively compacts | |
| 2nd grade | Wide compact | close-meshed cancellous bone |
| Class 3 | Thin compacts | close-meshed cancellous bone |
| Grade 4 | Thin compacts | wide-meshed cancellous bone |
In addition, the bone quality can be classified in Hounsfield units [HU], from which the resulting implant healing times follow.
| Bone quality | Bone density [HE] | Implant healing time [months] |
|---|---|---|
| D1 | 1500 | 3-4 |
| D2 | 500 | 4-5 |
| D3 | 250 | 4-6 |
| D4 | 100 | 6-9 |
Bone compaction
With the process of bone compression ( engl .: Bone condensing) the stability of the dental implant can be increased in the jaw bone, for example in the presence of a very wide-meshed bone of class 4, the use of bone compaction method can contribute to significantly improved primary stability of the dental implant. Since the upper jaw often falls into this category, bone condensation is almost exclusively used there. This method is also often used in connection with the sinus lift operation.
Special features of bone biology in the anterior region
The tissue is essentially fed by the blood supply. In the upper jaw, this is mainly done by two large arteries ( arteria palatina ), which pull forward on both sides from the rear edge in the lateral notch of the upper jaw. Thus, the palate is well supplied with blood, while the vestibular side of the bone has to be nourished through the teeth and through the mucous membrane on the cheek side. This relative malnutrition of the bone on the cheek side leads, even under natural circumstances, to the fact that the contour of the tooth roots is reflected in the bony base of the gums there, especially clearly visible in the canine area. For this reason, after an implantation, the thin alveolar wall in the anterior region may recede, and with it the gums. This has unpleasant cosmetic effects, so that you can see the metallic-dark implant body, especially when you laugh.
In order to remedy this situation, they returned to the white ceramics that were used earlier. At that time these materials were abandoned because they were not elastic enough and often broke in the depths under the bending of the bone. For some time now there has been an extremely hard material, zirconium, which can withstand these loads and, because of its white color, is not so cosmetically troublesome if the bone and gums recede. Unfortunately, this ceramic does not form a bond with the bone that is comparable to titanium. Experience with this material is not yet sufficient to really be considered an alternative to titanium. Here we still have to wait.
However, since the regression of the bone in the front is related to the nutrition of the bone, this problem can be solved by using a narrower or differently shaped implant. In addition to leaf implants, there is also a cylindrically shaped implant type, which is characterized by the fact that it looks like a column of coins with large gaps between them. The core is very thin. This construction has the advantage that the nutrition of the bone is guaranteed especially in the horizontal direction. In addition, its upper edge is beveled in a conical shape and therefore corresponds more closely to the tapered alveolar ridge. As a result, the bone layer at the upper edge remains much thicker and can better nourish the gums. The regression of the bone and the gingiva in the aesthetically particularly important area of the front is therefore less likely.
The nutrition of the bone in the sensitive anterior tooth areas is also reduced if too many implants are used there, for example one implant for each missing tooth. In contrast to the natural tooth, in which there is a nutritional interaction between the tooth and the bone surrounding it ( Tarnow, New York University ), this nutrition is absent in the implant body. Above all, the thin bone gap between the implants often means that this “residual bone” does not feed itself and then perishes. So it depends on the correct ratio of living substance to dead foreign substance. If the jawbone is replaced by too much metallic foreign substance, as in the case of thick implant cylinders, which are also very narrow, it withdraws due to malnutrition. How this quotient between bone substance and metal must look has not yet been defined and is therefore the subject of future studies. For the minimum distance between the implant body and its pillars supporting the future tooth crown , an empirical value of 1.5 to 2 mm applies in the upper area at the point of passage through the gums, namely all around, i.e. also on the lip side. This value must be undercut relatively often in the front, especially since the natural tooth socket (alveolus) often has an edge thickness of less than 1 mm there. Very often, even in natural teeth, the gums retract exactly where they can be seen most (apparently long teeth). The implant adds to the problem.
This could be remedied by an oval instead of a circular implant shape, as is the case with natural anterior teeth. This oval shape would widen the bone layer between the implants if they were each rotated so that the narrow edges are oriented outward and inward. However, this would still not solve the problem of the too thin bony outer layer (on the lip side) of the implant site. The introduction of this oval implant would also be more difficult for the practitioner than with a circular implant.
Without a doubt, despite the enormous successes with implants in the oral area, there are still numerous opportunities for improvement.
Time of treatment
A distinction between immediate implants immediately after tooth loss, delayed immediate implants 2-8 weeks after tooth loss and late implants after complete bony healing of the tooth socket . Immediate implants should only be used if the alveolus is free of inflammation immediately after extraction of the tooth. Delayed immediate and late implantations reduce the risk of infection. In the case of single-root teeth in regions with thin vestibular bone lamellae (for example in the anterior region), however, immediate implantation or delayed immediate implantation (within 2 weeks) has the advantage that bone loss and thus the risk of aesthetic failure is minimized.
Immediate implantation comes closest to the patient's needs, but also carries a greater risk of failure.
The navigated implant is a prosthetic and surgical assistance process, to facilitate the correct placement of dental implants in the jawbone. The indications and restrictions on use for a navigated implantation are set out in the guidelines of the European Association of Osseointegration (EAO) and, for the German-speaking area, in the S2-K guideline of the German Society for Dentistry, Oral and Maxillofacial Medicine (DGZMK). Most of the indications relate to an expansion of the diagnostic possibilities for three-dimensional representation of the jawbones and their neighboring structures, in order to enable an improved assessment of the surgical area, especially when there is little bone supply or its unclear representation in conventional imaging techniques.
Surgical technique of an implantation
A dental implantation is usually carried out on an outpatient basis under local anesthesia . After a mucoperiosteal incision has been made, the mucous membrane is unfolded at the planned location and the implant bore is gradually prepared according to an individually determined length and diameter. To avoid overheating of the bone, the preparation is carried out with a low speed of the rotating instrument, low pressure and permanent cooling with physiological saline solution .
The implant is inserted using a torque wrench. Depending on the bone quality , up to 55 N · cm should be used in order to achieve the necessary primary stability . After the insertion, the gums are sutured again. With appropriate follow-up care (cool compresses, medication) complications (swelling, etc.) can largely be avoided. After ten days, the external wound healing is usually complete. An unloaded healing phase, depending on the bone quality, follows.
In a minimally invasive procedure, the implant bed is prepared for the mini-implant without forming a mucoperiosteal flap . The simplified and shorter operation can reduce any postoperative discomfort. A drilling template provides guidance .
Temporary dentures
If necessary, a temporary denture is used for the healing time of the implant.
In the case of a multi-part implant, the internal thread of the implant body is exposed after the healing phase, the abutment, the part of the crown on the implant, is screwed in and the superstructure is manufactured and integrated. After the healing phase, the superstructure can be fabricated and incorporated on a one-piece implant immediately.
Aftercare
Immediately after an implantological restoration, the surgical site should not be stressed. Too intensive cleaning measures (for example with a hard toothbrush) directly at the seam should be avoided, whereas the rest of the dentition must be cleaned very carefully. Antiseptic mouthwashes (e.g. with chlorhexidine ) are available as an additional aid . Infection prophylaxis plays a key role in the first 48 hours after the operation. It is also important not to use any prostheses in the surgical area or at least to “place them hollow”, because otherwise they could transfer uncontrolled loads to the implant. The duration of the healing phase up to the direct loading of the implant is currently still being scientifically discussed - with a tendency towards decreasing duration (see also loading time) up to immediate loading.
Dental implants must be checked regularly because of the risk of infection. Infections detected in good time can be treated much more successfully than advanced infections, which have already led to the breakdown of bone material. Therefore, dental implants should be checked every 6 months by the treating dentist or implantologist. Clinical experience has shown that it can make sense, especially in the case of major orthodontic implantological measures in both jaws, to provide brief inpatient care after the operation, for example in the case of large-volume bone structures with bone transplants from the hip or with bone substitute material. The key point of this post-operative follow-up care is the feeding of the patient via a venous catheter in order to avoid a bacterial risk to the fresh surgical wounds in the mouth through normal oral food intake.
Time of loading
In addition to the time of operation after tooth extraction, the time of loading of the implant is also important. One distinguishes the immediate loading of the delayed loading . Immediate loading requires primary stability (high strength of the implant already during the operation) and means immediate restoration of the implant with the loading superstructure (crown, bridge , removable prosthesis). On the other hand, the primary stability is not decisive for late loading because the bone encloses the implant more and more tightly during the healing period (several weeks to months). The lower the primary stability of the implant during the operation, the more time must be allowed for the formation of sufficient bone substance. Standards for primary stability measured (in Ncm screw-in torque) have only been in existence since 2006.
Immediate implants
An immediate implant is the insertion of an implant into the fresh (extraction) wound (alveolus) immediately after the removal or loss of a tooth. Implant shapes with a tapered lower end (conical screw implants) come closest to the natural root shape and seem to be particularly useful for immediate implantations in order to protect the existing bony structures. The cylindrical, parallel-walled implants ensure better primary stabilization, because higher friction is achieved in the area of the tip of the empty tooth socket . There is controversy as to whether a healing phase is necessary. There must be sufficient bone density for immediate loading .
Technically, conical, root-shaped implants have the disadvantage that the depth of insertion cannot be varied due to the shape of the implant and thus cannot always be adequately adapted to the given anatomical conditions. Due to the increasing number of different diameters and lengths of the implants, a satisfactory primary stability can also be achieved with conical implants.
With regard to primary stability, implants should be used angled for immediate implantation in order to achieve optimal positioning. A bone structure can thus be partially avoided. A prerequisite is good health.
The roots of natural teeth are on the outer radius of the jawbone. In old age, the jaw is degraded from the outside to the inside, which is why the direction of insertion of the implant should be determined by individually preparing the implant bed towards the inner radius of the jaw.
- Immediate implantation procedure on an upper incisor with a long-term temporary bridge restoration.
Immediate implant b1.jpg Tooth 11 (with crown) before extraction due to a root fracture and immediate implantation.
Immediate implant b2.jpg Situation after removal of the tooth crown 11 with a root post .
Immediate implant b3.jpg Removed tooth root and crown with a view of the root fracture.
Immediate implant b4.jpg Alveolus after extraction of the fractured tooth root.
Immediate implant b5.jpg Situation after drilling the implant bed in the extraction socket .
Immediate implant b6.jpg Axis control and length measurement of the implant bore before placing the planned implant.
Immediate implant b7.jpg Law implant in pre-drilled extraction socket (with insertion post ).
Immediate implant b8.jpg Incisal view of the inserted implant after screwing in the healing screw.
Immediate implant b9.jpg Bone build-up with the patient's own bone (collected drilling chips). Insertion into remaining cavities and crevices.
Immediate implant b10.jpg Bonded temporary bridge in region 11 after checking the occlusion with occusion paper (view from the palatal).
Immediate implant b11.jpg Bonded temporary bridge in region 11 immediately after extraction and immediate implantation.
A custom-made implant is intended to replace one or more roots of a single tooth immediately after extraction. Since an individually manufactured implant has to fit into the fresh socket, it can only be inserted immediately after a tooth extraction. With the new generation of printers, the extracted tooth can be scanned and soon printed from zirconium dioxide. The accuracy for “printed” definitive tooth restorations is currently not sufficient for reliable clinical use. Therefore, experimentally milled CAD / CAM solutions are currently preferred. A review from August 2018 shows that so far only a few studies on the mechanical and biological benefits and no long-term studies are available.
Length of stay
The length of time the implants remain in the jaw, ie the “durability”, depends on the preservation of the surrounding bone. The connection between implant and bone can almost exclusively be destroyed by bacterial influences (dissolution of the bone matrix by matrix metalloproteases , MMPs). Genetic aspects of evolutionary biology relatively young diet with cereals explain the increased susceptibility to infection of the gums (gingiva) and the periodontal apparatus in focus oriented bread diet in Germany. Therefore, infection prevention before, during and after the insertion of the dental implant plays a decisive role. With decreasing sensitivity to bacterial influences with a simultaneous increase in the intensive implant-bone contact (BIC: bone to implant contact ) under functional- physiological chewing load, the risk of implant loss decreases because the mechanical load, depending on time and intensity, leads to an increased mineralization of the surrounding bone that can be x-rayed leads. This means that much more attention must be paid to teeth cleaning and oral hygiene in the initial period after the operation than, for example, after about 2 years of uneventful wear. The length of stay also depends on the size of the surface due to the implant geometry, the micromorphological design and the external shape.
According to international statistics, the certainty of success of cylindrically oriented implants is 85–90% in the 5-year interval. It is essentially dependent on the occurrence of an infection. With suitable measures that focus on consistent infection prophylaxis immediately postoperatively through inpatient follow-up care, it is therefore possible to increase the success rate to almost 100% every 10 years. This only applies to non-smokers, as the chances of success for smokers are highly dependent on their nicotine consumption. There are known to be times of more than 40 years when the implant can be worn in the dentition without further measures.
With these numbers, dental implantology is one of the most successful medical interventions. The success rates in the field of orthopedic implants are significantly lower at 75 to 85%. The reasons lie in the increased electivity of dental implants. Even the endogenous infectious factors dental implantology is dedicated to intense. In the case of orthopedic implants, various changes to the micro- and macromorphological aspects could also increase the success rate.
History of implantology
Early implants
The first implantations to replace teeth are documented in the 7th to 8th centuries among the Mayans by the Italian professor of implantology at the University of Santos (Brazil), Amedeo Bobbio . In a fragment of the lower jaw bone of a young woman there are three implants made from a milled mussel shell. Due to the radiologically proven osseointegration, these mussel implants were inserted during lifetime and not post mortem . Another fragment from the time of the Mayans, which was found and described by the archaeologist RR Andrews, in which a "black stone" should have been implanted as a lower jaw anterior tooth, can no longer be found. Until it was proven by Bobbio in 1970, the mussel implants were considered to be inserted post mortem, in the sense of a funeral ritual.
Other attempts to replace missing teeth are not to be called implants, such as the transplantation or reimplantation of teeth and teeth made of organic or inorganic materials such as ivory or walrus teeth and their attachment to the existing teeth by means of gold threads or gold bands. This also included transplantation of the teeth of the dead, as mentioned in the Middle Ages by Abulcasis , in the early modern period by Pierre Fauchard and Ambroise Paré and many others, as well as during the Battle of Waterloo (1815) and other wars.
The invention of the artificial ceramic tooth by Giuseppangelo Fonzi in 1806 was of great importance for the further development of implantology. His artificial teeth, which were implanted directly into the socket with platinum hooks, fulfilled both aesthetic and functional requirements. A first metal implant made of gold was designed by the Italian J. Maggiolo in 1809 and inserted into a fresh human extraction wound. Maggiolo practiced in Paris and published his findings in his book Le Manuel de l'Art du Dentiste in Nancy.
Around 1840, Chapin Aaron Harris and Horace Henry Hayden , founders of the Baltimore College of Dental Surgery , tried endosseous implants with teeth made of iron and later of lead. Several similar case reports followed by Rogers (1845), Younger (1885), Edmunds (1886), Edwards (1889), and Payne (1898). In 1895 William Gibson reported to Arlington Bonwill about gold and iridium abutments that he implanted in alveoli to replace individual teeth and restore entire dental arches.
The development in the 20th century
Alvin Strock installed the first Vitallium screw implant as a tooth root replacement in the USA in 1937 . Vitallium was the first biocompatible metal, developed a year earlier by Charles Venable , an orthopedic surgeon. The beginning of endosseous implantology is attributed to Manlio Formigini , who recommended a helicoid screw ( Greek : ἑλικοειδής helikoeidēs , as if twisted) made of tantalum . He is known as the father of modern implantology. This was followed by the Raphaël Cherchève screw or the tantalum screws and needle implants by Jacques Scialom and Ernst-Helmut Pruin . The complication-prone subperiosteal framework implants located under the periosteum, which were developed by Müller in 1937 and were widely used in the 1950s and 1960s, formed a side route.
In the 1960s, the blade implant was designed by Leonard I. Linkow ( Linkow Blade ), as was the stabilized blade implant in 1975 by Benedict Heinrich .
At the beginning of dental implantology in Germany around 1969, initially a few dentists, mainly established in their own practice, used dental implants against the resistance of many university clinics and oral surgeons that had been declared for years. On the other hand, the demand for dental implants from patients was very high right from the start.
The modern development of implantology began with the discovery of the biocompatibility of the titanium surface by the Swedish orthopedic surgeon Per-Ingvar Brånemark in 1967. In 1978 the first Dental Implant Consensus Conference took place, which was jointly sponsored by the National Institutes of Health and Harvard University . It was a historic event at which retrospective data on dental implants were collected and analyzed and criteria and standards for modern implantology were established.
In 1982 Brånemark presented its work in Toronto, which had started 15 years earlier in Gothenburg. His discovery and application of osseointegration or the biological fusion of bone with a foreign body was unique. The scientific documentation of implantology has never been so comprehensive. The Toronto Conference resulted in widespread recognition of Brånemark implant methods and materials. It is one of the most significant scientific breakthroughs in dentistry since the late 1970s.
Then in 1982 the scientific recognition of dental implantology took place in Germany. In 1988, the dental services associated with implantology were included in the fee schedule for dentists (GOZ) with a small item catalog of 10 fee numbers (GOZ no. 900-909), described there individually and assessed with a fee.
Titanium has prevailed among all implant materials since the 1970s. The connection between the titanium surface and the bone has proven to be reliable. Fractures of the implant body rarely occur because the elastic moduli of bone and titanium are similar.
At the end of the 1980s around 1,500 dentists (approx. 2.5%), and in 2006 around 5,000–7,000 dentists (approx. 8–12% of the approx. 60,000 German dentists) implanted more or less regularly. Numerous dentists work closely on an interdisciplinary basis with an oral surgeon or specialist in oral and maxillofacial surgery who does the surgical part and inserts the implants and the dentist then integrates the superstructure (the dentures on the implants). In some federal states, the superstructures may not be made and incorporated by the oral surgeon if the specialist area is restricted.
Implantology is not a separate subject at universities, so dentists acquire the relevant knowledge as part of postgraduate training.
3D implantology
3D implantology is a method for precise virtual diagnostics, planning and positioning of implants. Due to the exact representation of the anatomical jaw structures, this method offers the possibility of maximum tissue protection even with a tooth implantation. For this purpose, an image of the jaw is first created using 3D x-rays (digital volume tomography), which shows the finest bone and soft tissue structures in three dimensions. With the help of special planning software, the implants can be placed virtually on the screen, with the optimal size, position and axis being determined. The planned position of the implants can then be transferred to the mouth using a navigation template. Using this drilling template, the implants can be placed in the jaw with millimeter precision. This helps to avoid mistakes and injuries (e.g. of nerves, blood vessels and maxillary sinuses).
Advantages of 3D implantology:
- Minimally invasive implantation - keyhole surgery
- Shortened operation time
- Minimal risk of damage to neighboring structures
- Avoidance of bone formation through optimal use of the jawbone
- Backward planning
Backward planning
With backward planning, the planning of the implantation is not based on the jaw and bone situation, but on the dentures. The position of the implants is, so to speak, backwards based on the position of the new implant-supported teeth. On the basis of impressions and three-dimensional image data, the dental laboratory develops a model of the subsequent tooth replacement. The implantologist uses this model to determine the appropriate number, position, length, alignment and drilling depth for the implants with computer-aided 3D implant planning. The individual bone and soft tissue situation is also taken into account here.
The digital simulation is transferred to the mouth using a drilling template for precise placement.
- Optimal aesthetic appearance
- Patients can assess their results in advance and make wishes
- Hygienic positioning of the implants
- Screw-in implant crowns
Superstructures
Superstructures are the actual dentures that are placed on top of the tooth root replacement, the implant.
Dental implants and fixed dentures
Here, single crowns or bridge abutments are screwed or cemented onto the (usually unscrewable) pillars of the implants to close a tooth gap with a bridge .
Indications:
- Single tooth replacement or small gap (1–2 missing teeth in the otherwise closed row of teeth)
- Large gap (more than 2 missing teeth in the otherwise closed row of teeth)
- Free-end situation (shortened row of teeth) (fixed dentures only possible to a limited extent)
Single tooth replacement or closing a small tooth gap
Reasons for tooth loss can be tooth decay, pulpitis, periodontitis, general illnesses or an accident.
If teeth are not created, intensive consultation with an orthodontist must take place.
When replacing individual teeth or closing a small gap, the neighboring teeth do not have to be ground compared to the conventional restoration using a bridge . A crown can be placed directly on the implant. The gums lies down at a favorable initial situation harmoniously with the crown and nothing indicates more attention to the loss of teeth. In less favorable cases, soft tissue management must be carried out by means of periodontal surgery in order to achieve an aesthetically satisfactory transition from the tooth to the gingival margin, which is particularly important in the visible area.
Problems with individual tooth replacement can arise if the tooth gap is not sufficiently large, which is the case if the interdental distance is too small. Until 2003, efforts were made to use implant diameters that filled the gaps as much as possible in order to achieve an aesthetic result. After failures were recorded as a result, this procedure was replaced by the knowledge that a sufficiently large minimum distance of around 1.5 to 2 mm to the neighboring natural roots must be maintained.
Large gaps
Of large switching gaps occurs when missing up to four teeth in a sextant and the gap is in each case delimited by a tooth.
In order to close such a gap with a fixed denture, the following options are available (if a "normal" bridge is no longer possible):
- For each tooth to be replaced, an implant is inserted and each is provided with a crown (very complex and costly).
- At least two implants are used as bridge abutments, and more than two in the case of very large gaps. A bridge is then attached to these implants (implant-supported bridge).
- Implants and natural teeth together serve as bridge abutments (hybrid bridge). This is only recommended in exceptional cases, because an implant does not allow any movement, but natural teeth can move within certain tolerance limits (see tooth support apparatus ).
Free-end situation
A free-end situation exists when there is no longer any natural bridge abutment in the distal area that could support a bridge. In these cases, fixed dentures ( bridges ) are possible with appropriately placed implants .
Example of a cemented implant bridge on two implants in the lower jaw
Example of a screwed implant bridge on two implants in the lower jaw
- Example of a cantilever bridge on two implants
Removable dentures
Implant pillars can also be used to anchor removable partial dentures, which can be attached to the implants using double crowns , bars, attachments, spherical heads similar to push buttons or magnets and thus become so-called combined dentures .
Indications:
- Anchoring combined dentures
- Anchoring of deck or cover denture prostheses ( hybrid prostheses ) in the edentulous jaw
Greatly reduced dentition
One speaks of a strong reduction in dentition in a jaw when there are only 5–6 of one's own teeth. The assessment of when a dentition should be classified as severely reduced depends on the distribution of the remaining dentition, whether only anterior teeth are present or whether it is unilateral or bilateral residual dentition.
In such a set of teeth, implants are used to increase the number of pillars in order to ensure better support and a more secure fit of a prosthesis or removable bridge. Fastening with telescopic crowns is a possible solution in these cases.
Total replacement - edentulous jaw
Some prosthesis wearers complain about a poor fit of their prosthesis or painful pressure points. Adhesives or mechanical aids often do not solve these problems satisfactorily. In these cases, implants can be the method of choice. The wearing comfort of a prosthesis can thus be improved.
Fastening full dentures to implants is more common in the edentulous lower jaw than in the edentulous upper jaw, because lower jaw prostheses also cause problems more often. This is due to the low suction effect and the smaller contact surface of a lower jaw prosthesis. Two implants may be sufficient in the lower jaw, whereby the distribution of force over four implants is advantageous. In the upper jaw, at least four implants should be used due to the softer bone structure.
The implants can be connected to one another via bar connections (possibly with friction aids). This serves both to stabilize the implants and to better anchor the prosthesis. With good primary stability, immediate loading is possible in certain cases.
If there are around 6 to 8 implants, a full denture can be supported on these alone. Loading of the ridges is then omitted so that no bone loss is to be feared. With this number of implants, a fixed dental prosthesis is an alternative. Originally intended as a social indication, screwed bridges are now possible on four implants each in the upper or lower jaw. This can reduce costs and treatment time. The length of stay with this type of care is comparable to the conventional procedure.
Studies mainly from Canada and Germany have shown that a single implant in an edentulous jaw can significantly improve the comfort of a full denture if more implants are no longer possible for economic reasons.
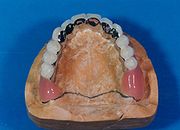
- An example of a partial upper denture (combined denture) (here with 7 double crowns and a bar on 7 implants)
Fixed part of the maxillary hybrid prosthesis seen from the occlusal .
Upper hybrid prosthesis on the working model seen from the occlusal . Note: The hard palate is not covered with a plastic sheet.
Upper hybrid prosthesis seen from the vestibular on the working model .
- An example of a cover denture prosthesis in the lower jaw (here on 4 implants and 2 bars)
Fixed part of a mandibular hybrid prosthesis seen from the vestibular direction: 4 implants and 2 bars
Fixed part of the mandibular hybrid prosthesis seen from the occlusal
The hybrid mandibular prosthesis seen from the crestal point . When the image is enlarged, one can clearly see the retention pins, which are used for the friction of the prosthesis.
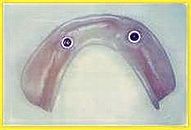
- An example of a cover denture prosthesis in the lower jaw (here on 2 implants with spherical heads)
2 implants in the lower jaw with patrixes to fix a cover denture prosthesis
the matching lower jaw prosthesis with the incorporated matrices
Advantages and disadvantages of dental implants
Advantages:
- reduced bone loss in the edentulous alveolar ridge area,
- reduced pressure on the mucous membrane with partial dentures,
- Grinding of the neighboring teeth can be avoided,
- improved hold of a prosthesis,
- Fastening of full dentures as cover denture dentures .
Disadvantages or possible risks:
- surgical intervention required,
- possible nerve injury (especially the inferior alveolar nerve in the mandibular canal of the lower jaw, Vincent symptom ),
- possible opening of the maxillary sinus with possible sinusitis with maxillary implants
- Since dental implants grow rigidly into the bone, the chewing pressure is not cushioned by the Sharpey fibers as is the case with natural teeth and can thus lead to overloading of the temporomandibular joint,
- expensive,
- higher demands on oral hygiene,
- Long treatment time,
- Risk of peri-implantitis,
- Risk of implant loosening and loss.
- If there is not enough bone available, bone replacement may be necessary
literature
- Ugo Pasqualini, Marco E Pasqualini. Treatise of Implant Dentistry - The Italian Tribute to Modern Implantology , Carimate, Ariesdue, 2009, ISBN 88-903821-1-2 , ( digitized English full version). Retrieved April 22, 2017.
See also
Web links
- Implant supply for oral rehabilitation in connection with head and neck radiation . (PDF) S3 guideline , AWMF register number 007/089, status 05/2015.
- Implant prosthetic restoration of the edentulous upper jaw . (PDF) S3 guideline, Working Group of the Scientific Medical Societies in Germany, AWMF register number: 083-010, status: November 2014, valid until: November 2019. Accessed on April 10, 2017.
- Patient information. (PDF; 140 kB) German Dental Association and German Society for Dentistry, Oral and Maxillofacial Medicine
- Risks in implantology on implantat-wissen.de
- Limits of dental implantology: heart and circulatory diseases, blood coagulation, diabetes mellitus - Initiative proDente e. V. on prodente.de
- Scientific updates in implantology on implantate.com
- https://dentalimplantat.de/implantation/3d-implantologie
Individual evidence
- ↑ enossal in the Wiktionary .
- ↑ A. Nedjat, The PEEK implant as an alternative to titanium. ( Memento of March 2, 2014 in the Internet Archive ) In: Implantologie Journal. Journal of the German Society for Dental Implantology. No. 06, 2014, p. 8ff.
- ^ André Schröder, 1976, Bern
- ↑ a b N. Schwenzer, M. Ehrenfeld: Tooth-mouth-jaw medicine. 5 volumes, volume 3: Dental surgery. Thieme Verlag, Stuttgart 2000, ISBN 3-13-116963-X .
- ↑ CM ten Bruggenkate, K. Müller, HS Oosterbeek: Clinical evaluation of the ITI (F-Type) Hollow cylinder implant. In: ITI Hollow cylinder implant. Chapter 6, ISBN 90-90-03708-X , pp. 75-83. PMID 2263324
- ↑ K. Müller: Narrow jaw implants - innovation increases quality of life. In: Implantologie Journal. 10th year, 8/2006, pp. 26-30, ISSN 1435-6139 http://www.drklausmueller.de/plugins/files/922680/narrow_jaw_implants.pdf
- ↑ Carl E. Misch (Ed.): Contemporary implant dentistry.
- ↑ B. Zhao. In: J Biol Chem . 2006, ISSN 0021-9258 .
- ^ Thomas Sulzer, Michael M. Bornstein, Daniel Buser: Current range of indications in oral implantology at a referral clinic . (PDF). In: Switzerland Monthly Dental Medicine. 2004, Volume 114, pp. 444-450.
- ↑ Indication classes of the consensus conference on implantology , as of October 7, 2014. Accessed on November 27, 2014.
- ↑ CU Fritze Meier, W. Schmüdderich: Periimplantitisprophylaxe by sealing the implant interiors, Implantology 15 (1), 2007, pp 71-80.
- ↑ Regina Schindjalova: Fast & Fixed therapy concept - also for periodontitis profunda . In: Implantologie Journal . No. 8/2012 , 2012, ISSN 1435-6139 , p. 28-32 ( oemus.com [PDF]).
- ↑ G. Hexdecke: Orale Implantologie. ( Memento from August 13, 2011 in the Internet Archive ) (PDF; 1.7 MB) uke.de (University of Hamburg).
- ↑ Prof. Dr. Dr. Norbert Kübler: Implantology of the oral and maxillofacial surgery of the UKD. Uniklinik Düsseldorf, April 12, 2016, accessed on February 14, 2019 .
- ^ Carl E. Misch: Density of bone effect on treatment plans, surgical approach, healing and progressive loading. In: Int J Oral Implantol. 1990, 6 (2), pp. 23-31.
- ↑ U. Lekholm, GA Zarb: patient selection and preparation. In: PI Brånemark, GA Zarb, T. Albrektsson: Tissue-integrated prostheses-Osseointegration in Clinical Dentistry. Quintessence Publishing, Chicago 1985, pp. 199-209.
- ↑ HB Engels: Failures in oral implantology. A little breviary to avoid failure. In: HB Engels: Manual for the BDIZ / EDI implant register. Basic.Dent-Verlag, 2003, pp. 273-293.
- ↑ U. Lekholm U., GA Zarb: patient selection and preparation. In: PI Brånemark, GA Zarb, T. Albrektsson: Tissue-integrated prostheses-Osseointegration in Clinical Dentistry. Quintessence Publishing. Chicago 1985, pp. 199-209.
- ↑ A. Markovi ?, D. Calasan include: Implant stability in posterior maxilla: bone-condensing versus bone-drilling: a clinical study. In: Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. Volume 112, Number 5, November 2011, pp. 557-563, ISSN 1528-395X . doi: 10.1016 / j.tripleo.2010.11.010 . PMID 21330161 .
- ^ D. Harris, K. Horner et al .: EAO guidelines for the use of diagnostic imaging in implant dentistry 2011. A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. In: Clinical oral implants research. Volume 23, Number 11, November 2012, pp. 1243-1253, ISSN 1600-0501 . doi: 10.1111 / j.1600-0501.2012.02441.x . PMID 22432473 .
- ↑ S2k guideline: Indications for implantological 3D X-ray diagnostics and navigation-assisted implantology ( Memento of the original from September 23, 2015 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. (PDF) German Society for Dentistry, Oral and Maxillofacial Medicine (DGZMK). Retrieved on October 19, 2014.
- ↑ Heather J. Conrad: Accuracy of two impression techniques with angulated implants . In: The journal of prosthetic dentistry . tape 97 , no. 6 , 2007, ISSN 0022-3913 , p. 349-356 , PMID 17618917 .
- ↑ Ashok Sethi: Evolution of the concept of angulated abutments in implant dentistry: 14-year clinical data . In: Implant Dentistry . tape 11 , no. 1 , 2002, ISSN 1056-6163 , p. 41-51 , PMID 11915544 .
- ↑ White and Screwed , Dental Magazin, June 14, 2018. Accessed February 9, 2019.
- ↑ Miguel Pessanha-Andrade, Mariane B. Sordi, Bruno Henriques, Filipe S. Silva, Review Article: Custom-made root-analogue zirconia implants: A scoping review on mechanical and biological benefits, August 2, 2018. Journal of Biomedical Materials Research Part B: Applied Biomaterials, Volume 106, Issue 8, pp. 2888-2900, doi: 10.1002 / jbm.b.34147
- ↑ Amedeo Bobbio, Maya, the first authentic alloplastic, endosseous dental implant. A refinement of a priority. Rev Assoc Paul Cir Dent. 27 (1), Jan-Feb 1973, pp. 27-36. PMID 4620759
- ↑ Abū al-Qāsim Khalaf ibn ʻAbbās al-Zahrāwī: مقالة في العمل باليد . University of California Press, 1973, ISBN 978-0-520-01532-6 , pp. 276 ff . ( google.com ).
- ↑ P. Fauchard, Le Chirurgien Dentiste Urschrift, Gallica .
- ↑ La méthode curative of Playes, & Fractures de la Teste humaine, 1561st
- ^ HD Pape, R. Heiss: [History of tooth transplantation]. In: Advances in Maxillofacial Surgery. Volume 20, 1976, pp. 121-125, ISSN 0071-7916 . PMID 770274 .
- ↑ Stephanie Pain: The great tooth robbery. In: New Scientist . 2295, June 16, 2001, historyhome.co.uk.Retrieved April 22, 2017.
- ↑ J. Maggiolo, Le manuel de l'art du dentiste, ou, L'État actuel des découvertes modern sur la dentition: les moyens de conserver les dents en bon état: les mécaniques nouvelles inventées par M. Maggiolo: et tous les details pratiques et moyens d'exécution des dents artificielles, etc. (French), 1807, Wellcome, archive.org. Retrieved April 22, 2017.
- ↑ Paolo Zampetti, L'evoluzione dei materiali utilizzati in implantologia. Considerazioni storico-cliniche. Odontoiatria. Rivista degli Amici di Brugg. 22 (1), 2003, pp. 65-72.
- ^ Robert J. Rudy, Paul A. Levi, Jr. et al, Intraosseous Anchorage of Dental Prostheses - An Early 20th Century Contribution , Compendium of Continuing Education in Dentistry. May 2008, Volume 29, Issue 4. Retrieved April 22, 2017.
- ^ History of Dentistry ( Memento of July 14, 2016 in the Internet Archive ), Complete Dental Guide. Retrieved April 22, 2017.
- ↑ K. Müller: Kleines Handbuch der Oralen Implantologie, 1978, ISBN 3-9800176-2-1 .
- ↑ Norbert Schwenzer: Dental surgery: 35 tables . Georg Thieme Verlag, 2000, ISBN 978-3-13-116963-1 , p. 127 ( google.com ).
- ↑ David L. Hoexter, A tribute to Dr Leonard I. Linkow: A guiding light , Dental Tribune, December 22, 2010. Retrieved September 23, 2014.
- ↑ Bruno E. Gysi, Peter Schärer: Focus on oral implantology and reconstruction . Quintessenz, 1983, ISBN 978-3-87652-288-3 , pp. 143 ( books.google.com ).
- ↑ Anke K. Brinkmann, Egon LW Brinkmann: The history of dental implantology in Germany. Anke-Verlag, Oldenburg 1995, ISBN 3-00-000527-7 . (Dissertation, University of Munich 1993).
- ↑ LB Shulman, TD Driskell: Dental Implants: A Historical Perspective. In: M. Block, J. Kent, L. Guerra: Implants in Dentistry. WB Saunders, Philadelphia 1997, ISBN 0-7216-2174-0 , p. 2.
- ↑ A. Salti: The 2000 year history of implantation. (PDF; 408 kB) on zwp-online.info, ZWP, Implantologie Journal , 2003/1, pp. 6–8.
- ↑ Ingrid Grunert: The patient is toothless - what to do? (PDF; 114 kB) BZB , 6/2012, pp. 52–57.
- ↑ P. Maló, B. Rangert, M. Nobre: "All-on-Four" immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. In: Clinical implant dentistry and related research. Volume 5 Suppl 1, 2003, pp. 2-9, ISSN 1523-0899 . PMID 12691645 .
- ↑ C. Mehl, S. Harder, "Fixed Third Teeth" in One Day. In: ZMK aktuell. Volume 03, 2015.
- ↑ P. Malo, M. de Araújo Nobre et al .: A longitudinal study of the survival of All-on-4 implants in the mandible with up to 10 years of follow-up. In: Journal of the American Dental Association (1939). Volume 142, Number 3, March 2011, ISSN 1943-4723 , pp. 310-320. PMID 21357865 .
- ^ Joanne N. Walton, Michael Glick, Michael I. MacEntee: A Randomized Clinical Trial Comparing Patient Satisfaction and Prosthetic Outcomes with Mandibular Overdentures Retained by One or Two Implants. In: Int J Prosthodont. Volume 22, 2009, pp. 331-339.
- ↑ S. Harder, S. Wolfart et al .: Three-year clinical outcome of single implant-retained mandibular overdentures - results of preliminary prospective study. In: Journal of Dentistry. Volume 39, Number 10, October 2011, pp. 656-661, ISSN 1879-176X . doi: 10.1016 / j.jdent.2011.07.007 . PMID 21821093 .
- ↑ Matthias Kern u. a .: Survival and Complications of Single Dental Implants in the Edentulous Mandible following Immediate or Delayed Loading: A Randomized Controlled Clinical Trial. In: Journal of Dental Research. Volume 97, number 2, February 2018, pp. 163–170, ISSN 0022-0345 , PMC 6029143 (free full text), doi: 10.1177 / 0022034517736063 . PMID 29045800 .