anemia
| Classification according to ICD-10 | |
|---|---|
| D50-D53 | Alimentary anemia |
| D55-D59 | Hemolytic anemia |
| D60-D64 | Aplastic and other anemias |
| ICD-10 online (WHO version 2019) | |
A anemia (German anemia , colloquially anemia , formerly chlorosis ) is a reduction in the hemoglobin concentration in the blood (or, alternatively, the hematocrit ) falls below the standard age and gender.
Hemoglobin is an oxygen-carrying protein that is predominantly found in the red blood cells ( erythrocytes ) of the blood . Anemia is therefore usually associated with a lack of erythrocytes (erythrocytopenia) . In anemia, the oxygen transport capacity of the blood is reduced. In order to continue to ensure the oxygen supply to the organs, the organism typically reacts by increasing the heart rate so that the blood is pumped through the circulation faster. However, this makes it easier for the body to reach its limits. Typical symptoms of anemia are therefore easy fatigue, shortness of breath, especially during physical exertion, and often headaches.
Anemia is either acquired or congenital. Acquired anemia can be caused by blood loss, increased blood breakdown, diseases of the blood-forming system , deficiency diseases, kidney diseases, hormonal disorders, pregnancy or “ consuming diseases ” such as tumor diseases or chronic inflammatory diseases. Congenital anemias occur e.g. B. in hemoglobinopathies (genetic disorders of hemoglobin formation).
etymology
The term anemia, Latin for anemia in 1843 by the French physician Gabriel Andral , comes from the ancient Greek ἄναιμος ánaimos "bloodless" and is made up of the prefix αν- an- “un-”, “without”, “not” and that Word αἷμα haíma "blood".
Symptoms
The symptoms of anemia are either a direct result of the oxygen deficiency or the body's compensatory mechanisms. Patients notice due to the lack of oxygen supply to the whole body as the first symptoms often have a body weakness , a dyspnea , a drop in performance and rapid fatigue .
Skin and mucous membranes are characterized by paleness, although at least the paleness of the skin is not always easily recognizable, depending on the skin color. In some cases a whitish color with a bluish undertone can be seen in the sclera , due to anemia in the smallest conjunctival vessels. An insufficient supply of oxygen to the brain can cause headaches, ringing in the ears ( tinnitus ), nausea, fainting ( syncope ), insomnia, difficulty concentrating and visual disturbances. An insufficient supply of oxygen to the heart muscle leads to angina pectoris . As a result of an insufficient supply of oxygen, the kidneys may excrete a small amount of blood in the urine (microscopic hematuria ), a slight amount of protein ( proteinuria ) and a retention of salt and water ( renal insufficiency ). In addition, brittle fingernails and toenails , hair loss and split ends can be observed with long-term anemia .
Since the body tries to meet the oxygen demand of the tissues despite the reduced oxygen transport capacity of the blood, accelerated breathing ( tachypnea ) and an increased heartbeat ( tachycardia ) can occur.
Due to the increased frequency of the blood circulation and thus also the increased flow rate of the blood, characteristic noises can occur in the jugular veins on the neck, the so-called whimsy , as well as anemic flow noises on the heart valves, which can be perceived with the stethoscope without a structural heart valve defect consists.
In addition to these general symptoms, depending on the form of anemia, other clinical pictures can occur. However, anemia is always a symptom of an underlying disease or malnutrition; it can never be a complete diagnosis. Nevertheless, even small signs of anemia should be taken seriously, as they can lead to increased mortality in the long term, especially from cardiovascular diseases .
Diagnosis
| designation | Women | Men |
|---|---|---|
| hemoglobin | 12 to 16 g / dl | 14 to 18 g / dl |
| Erythrocytes | 4.3 to 5.2 million / μl | 4.8 to 5.9 million / μl |
| MCH | 28-34 pg | |
| MCHC | 30-36 g / dl | |
| MCV | 78-94 fl | |
| Reticulocytes | 1 % | |
| Hematocrit | 37-47% | 40-54% |
| Ferritin | 22-112 µg / l | 34-310 µg / l |
| Transferrin | 212-360 mg / dl | |
| Vitamin B12 | > 300 ng / l | |
| Folic acid | > 2.5 ng / ml | |
A suspected diagnosis can already result from the medical history ( anamnesis ) and the general physical findings. In the context of further clarification of the cause, the search for bleeding sources (especially bleeding from the stomach and intestines as well as genital bleeding in women) as well as signs of hemolysis and a graded system of laboratory tests are available.
It is important to distinguish whether anemia is caused by increased blood loss / breakdown or anemia caused by a blood formation disorder. Mixed forms can also occur. The most important technical tool for diagnosing anemia is the blood count .
The first piece of information a blood count provides is whether there is any anemia at all. By determining the hematocrit and erythrocyte count, it can indicate a reduction in the number of cells in the blood. The values for the mean volume (mean individual erythrocyte volume , MCV from mean corpuscular volume ) of the erythrocytes and the width of the erythrocyte distribution provide information about the size of the cells (and thus an indication of the cause, see section Classification ). The hemoglobin concentration in the blood as well as the hemoglobin content (mean corpuscular hemoglobin, MCH) and the hemoglobin concentration (mean corpuscular hemoglobin concentration, MCHC) of the erythrocytes offer possible indications of disturbances in the formation of the red blood pigment.
Anemia is often a sign of a systemic disease (e.g. infection or tumors) or the main symptom of a disorder of erythropoiesis (formation of red blood cells).
Examples from diagnostics:
- The number of reticulocytes (immature red blood cells) can be used to determine whether there is a haematopoietic disorder, as these are normally released in increased numbers from the bone marrow when there is a loss of red blood cells.
- The concentration of the proteins involved in iron metabolism, such as ferritin , transferrin and transferrin receptor, provides information about the presence of iron deficiency anemia or a deficiency in vitamin B12 and folic acid in megaloblastic or pernicious anemia.
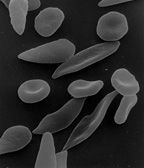
- Deviations in the shape of the red blood cells can also provide information about certain anemias (for example sickle cell anemia ).
- A bone marrow smear can show whether the cause is in the blood-forming tissue in the bone marrow itself.
Hemoglobin content
The criteria for the diagnosis of anemia, which are still widely recognized today, are based on a report by a WHO expert group from 1968. According to this, anemia is present if the hemoglobin content falls below the following values:
| Person category | Hb lower limit (g / dl) |
|---|---|
| Children from 6 months to 6 years | 11 |
| Children from 6 to 14 years | 12 |
| Adult men | 13 |
| Adult women, not pregnant | 12 |
| Adult women, pregnant | 11 |
These values have been adjusted based on more recent knowledge and larger reference samples. Recent studies in the US observe differences between physiological hemoglobin levels in white and black populations.
| source | Men lower Hb limit (g / dl) |
Women lower limit of Hb (g / dl) |
|---|---|---|
| WHO 1968 | 13 | 12 |
| Jandl 1996 | 14.3 | 12.3 |
| Williams (Beutler et al.) 2001 | 14.0 | 12.3 |
| Wintrobe (Lee et al.) 1998 | 13.2 | 11.6 |
| Rapaport 1987 | 14th | 12 |
| Goyette 1997 | 13.2 | 11.7 |
| Tietz 1995 | 13.2 | 11.7 |
| Hoffman et al. a. 2004 | 13.5 | 12.0 |
Classification
Anemia can be classified as follows:
- according to the morphology in micro-, macro- or normocytic anemia ( MCV )
- according to the hemoglobin content in normo-, hypo- or hyperchromic anemia ( MCH )
- after erythropoiesis in hypo-, normo- or hyperregenerative anemia
- in acute or chronic anemia
- in congenital or acquired anemia
Aregenerative anemia
Depending on the appearance of the remaining erythrocytes, anemias are divided into three groups in the clinic. The size of the cells and the hemoglobin content are considered. When cells appear normal, one speaks of normochromic, normocytic anemia , if the hemoglobin content is decreased, of hypochromic, microcytic anemia , if it is increased, of hyperchromic, macrocytic anemia .
Normochromic, normocytic anemia
While the number of red blood cells and thus the oxygen transport capacity of the blood are reduced, the cells appear morphologically normal. In hypoproliferative anemia , insufficient new erythrocytes are produced to meet the demand due to a deficiency or inadequate response to the hormone erythropoietin and to cytokines with a comparable effect (especially interleukin-6 and interleukin-8 ). The cause is either kidney disease, as erythropoietin is synthesized there ( renal anemia ), or diseases that cause the patient to be hypometabolic (low metabolic state). This applies in particular to hypothyroidism , pituitary insufficiency or a lack of protein .
If the number of precursor cells of the red blood cells is reduced, not enough new cells can be released into the circulation. In these diseases, the concentration of erythropoietin in the blood is mostly normal. Aplastic anemia results from a loss of stem cells. The reason for this is often unknown. Aplastic anemia is very rare, with 0.2 cases per 100,000 population per year in Europe, with an increase in adolescence , pregnancy and old age. Sometimes chromosomal changes are found to be the cause ( Fanconi anemia ). Radiation, chemicals, infections, some drugs, and hypersplenism also damage the bone marrow and indirectly cause anemia. However, this damage is unspecific and also affects the precursor cells of the other blood components. In the case of tumor diseases, normochromic, normocytic anemia often occurs, the extent of which can be exacerbated by chemotherapy. One also speaks of chemotherapy-associated anemia. Depending on the initial findings and chemotherapy regimen, the anemia is normocytic or slightly macrocytic, typically with reticulopenia as a result of the erythropoic damage. If only the precursors of the erythrocytes are affected, one speaks of erythroblastopenia or PRCA ( Pure Red Cell Aplasia ). Chronic PRCAs are caused by viral infections; chronic PRCAs can be congenital or acquired (due to diseases of hemolysis , thymomas , immune reactions or in the case of chronic lymphocytic leukemia ). After all, in myelodysplastic syndrome, blood formation does not come from healthy, but from genetically modified cells of origin. This also leads to anemia.
In osteomyelofibrosis , the blood-forming tissue in the bone marrow is gradually replaced by connective tissue so that normal erythropoiesis cannot occur. Other causes of bone marrow degeneration are certain malignancies , metastasis infiltration , malignant lymphomas, or leukemia .
Hyperchromic macrocytic anemia
This is also known as megaloblastic anemia . Red blood cell production is restricted as a result of vitamin B12 , thiamine or folic acid deficiency . This occurs most frequently, with an annual incidence of 9 cases per 100,000 population, as a result of vitamin B12 deficiency.
Vitamin B12 (cobalamin) is needed in the body for DNA synthesis . Since there is not enough DNA available for cell division , it remains with cells that are larger than mature erythrocytes ( megaloblasts ). The lack of vitamin B12 can have various causes:
- Insufficient intake with food (especially in the case of a vegan diet, i.e. complete avoidance of food of animal origin)
-
Malabsorption :
- For the absorption of vitamin B12 in the intestinal mucosa, it must be bound with the so-called intrinsic factor (IF). If this is not available or is insufficient, vitamin B12 cannot be absorbed. The cause for this can either be genetic or acquired. Acquired causes are either gastrectomies (surgical removal of the stomach) or autoimmune diseases (this condition is known as pernicious anemia ). Another possible cause of malabsorption is the inhibition of the binding of IF to cobalamin or the binding of the complex of the two to receptors in the ileum (ileum). This is also due to autoimmune diseases.
- Illnesses of the ileum can also inhibit cobalamin uptake. These include celiac disease , enteritis , intestinal tuberculosis and resections of the ileum, but also chronic inflammatory bowel diseases such as Crohn's disease and ulcerative colitis .
- Tapeworm infestation can also cause a vitamin B12 deficiency, as the tapeworms need larger amounts of vitamin B12.
- Enteral overgrowth, d. H. an incorrect composition of the intestinal flora
- Deficiency of transcobalamin II, the transport protein for vitamin B12 in the blood
- During pregnancy, in childhood, with malignant tumor diseases and with increased hematopoiesis, the need for vitamin B12 is increased. If this increased need is not met with a correspondingly increased intake through food, deficiency symptoms can also occur.
- Cadmium poisoning
Folic acid (more precisely tetrahydrofolic acid ) acts as a coenzyme in the synthesis of purines , thymine and methionine . If there is a deficiency, DNA synthesis is also disrupted. Possible causes:
- Insufficient intake
- Malabsorption due to celiac disease, drugs ( barbiturates , phenytoin ), alcohol
- Metabolism disorders due to a lack or inhibition of dihydrofolate reductase
- Cytotoxic drugs that inhibit DNA synthesis
- Increased need during pregnancy, in childhood, with malignant tumor diseases and with increased haematopoiesis.
Hypochromic, microcytic anemia
Microcytic anemia usually occurs as a result of iron deficiency or problems with the use of iron in the body.
The iron-deficiency anemia is in a proportion of 80% by far the most common type of anemia. In Europe around 10% and in developing countries more than 50% of women of childbearing age suffer from it. Generally 80% of the patients are female. The cause is usually an increased loss of iron due to recognized (e.g. in an accident or during menstruation ) or undetected bleeding, e.g. in the digestive tract, or due to increased intravascular hemolysis (see also section on hemolytic anemia ). Other possible causes are inadequate absorption as a result of diarrhea , a gastric acid deficiency or after a gastrectomy , insufficient intake with food or an increased requirement in developmental age, during pregnancy or during menstruation. The number of immature normoblasts (precursor cells of erythrocytes) is increased in the bone marrow .
If iron cannot get from its storage locations to the places where blood is formed in the bone marrow, anemia can also result. Causes are either genetic deficits or defects in the iron transport protein transferrin or protein loss in the kidneys in nephrotic syndrome . Inadequate use of iron also occurs either with hemoglobinopathies such as B. in thalassemia or sickle cell anemia , or in structural disorders of the heme group such as porphyrias .
In the case of an acquired, congenital or idiopathic impairment of iron utilization, iron is stored in erythroblasts (so-called sideroblasts , sideroblastic or sideroachrestic anemia), in the monocyte-macrophage system and in parenchymatous organs such as the liver with usually increased serum iron. At the same time, the number of platelets and white blood cells is often also reduced.
Chronic diseases such as cancer , autoimmune diseases ( systemic lupus erythematosus or rheumatoid arthritis ) as well as acute and chronic infections can also cause anemia. The release of cytokines by activated T lymphocytes and macrophages (phagocytes) stimulates the increased storage of iron in cells of the reticuloendothelial system ; the iron is then no longer available elsewhere. In addition, cytokines directly inhibit erythropoiesis. In the case of malignant tumor diseases, one speaks of tumor anemia .
Regenerative anemia
Regenerative anemias can be divided into those that occur after acute or chronic bleeding (bleeding anemia) and are associated with high blood loss, and those that result from an abnormally high level of destruction of the erythrocytes (hemolytic anemia).
Bleeding anemia
The natural restoration of normal red blood cell counts in anemia following sudden, profuse (acute) bleeding can be divided into three phases. The number of red blood cells is normal immediately after the bleeding, as the release of catecholamines ( adrenaline and noradrenaline ) mobilizes red blood cells from reservoirs (mainly from the spleen ) (hemodynamic compensation) . In the second phase, the plasmatic compensation , a few hours later, in order to maintain the blood pressure, the renin-angiotensin-aldosterone system is activated and vasopressin is released. The subsequent retention of water and the influx of tissue fluid lead to the thinning of the blood and thus to a reduction in hematocrit and the relative number of red blood cells, and ultimately to normochromic, normocytic anemia ( acute bleeding anemia ). The cellular compensation begins with the release of erythropoietin as a result of tissue hypoxia. This stimulates the formation of new erythrocytes and also causes an increased number of reticulocytes in the blood as these are increased and released prematurely from the bone marrow. It can take six to eight weeks to get a completely normal blood count, depending on the amount of blood lost and the amount of iron stored in the body.
Chronic bleeding (in the digestive tract, gynecological bleeding, hemorrhagic diathesis ) usually leads to iron deficiency anemia .
Hemolytic anemia
Anemia as a result of increased erythrocyte destruction is called hemolytic anemia . A distinction is made between corpuscular hemolytic anemias , in which the cause lies in the erythrocytes, and extracorpuscular hemolytic anemias , in which the erythrocytes are destroyed from the outside. By destroying the erythrocytes, the substances inside the cells are released. Therefore, the plasma levels of potassium , lactate dehydrogenase , free (unbound) hemoglobin, unconjugated bilirubin and iron increase . The saturation of transferrin with iron also increases, which leads to a reduction in the body's ability to bind iron. In addition, the plasma levels of haptoglobin and hemopexin decrease. The increased bilirubin content leads to pleiochromic (dark) stool and possibly jaundice (jaundice). The urobilinogen content of the urine is increased, hemoglobinuria and possibly also proteinuria can be observed.
treatment
Treatment of anemia is primarily aimed at eliminating the causes.
In patients who do not menstruate, iron deficiency anemia due to inadequate dietary iron intake is rare. Bleeding in the digestive tract must therefore be excluded as a possible cause of the anemia in these patients. The iron required is usually administered orally, in rare cases (inflammatory gastrointestinal diseases, malabsorption, poor tolerability of oral administration) also parenterally as an injection .
Megaloblastic anemia is treated by eliminating the cause (such as treating tapeworm disease) and administering vitamin B12 or vitamin B6 parenterally .
If the cause is insufficient blood formation due to genetic defects, a bone marrow donation can promise healing or relief.
In general, anemia that develops slowly (over months) is better tolerated by the patient than one that occurs as a result of massive bleeding within hours, as the body adapts to the long-lasting hemoglobin deficiency. Acute bleeding are transfusion of red cell concentrates treated. Exact guideline values from which a transfusion is necessary do not exist. Instead, in addition to blood counts, the duration, severity, and cause of the anemia, as well as the patient's history, age, and clinical condition must be taken into account. As a guideline for the need for a blood transfusion, the blood donation service of the DRK specifies a drop in hematocrit as a result of acute blood loss to values below 30% in seriously ill patients with cardiovascular diseases and to values below 20% in organically healthy, resilient patients. If the drop is less pronounced, volume substitution with infusions is sufficient . Long-term disadvantages of regular transfusions are the potential risk of infection, immunization and iron overload.
Furthermore, anti-anemics , which have an effect similar to erythropoietin , are available to stimulate blood formation . Erythropoietin is a glycoprotein hormone that is important as a growth factor for the formation of red blood cells (erythrocytes) during blood formation ( hematopoiesis ). Biotechnologically produced erythropoietin, such as epoetin alpha, is used as a therapeutic agent, primarily in the treatment of anemia in dialysis patients in whom blood formation is impaired as a result of kidney failure, and after aggressive chemotherapy cycles.
See also
literature
- Tinsley R. Harrison et al. a .: Harrison's Principles of Internal Medicine . Mcgraw-Hill Professional, 2005, ISBN 0-07-007272-8 .
- M. Wick et al. a .: iron metabolism, anemia. Diagnostics and therapy. New concepts in renal anemia and rheumatoid arthritis . Springer Verlag, Vienna 2002, ISBN 3-211-83802-3 .
- G. Bags u. a .: Anemia at a glance . Thieme Verlag, Stuttgart 2003, ISBN 3-13-137881-6 .
- Bruno de Benoist, Erin McLean, Ines Egli, Mary Cogswell (eds.): Worldwide prevalence of anemia 1993-2005: WHO global database on anemia. (PDF, 51S, 687 kB) World Health Organization, 2008, ISBN 978-92-4-159665-7 .
- Irmgard Müller: Anemia. In: Werner E. Gerabek u. a. (Ed.): Encyclopedia of medical history. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 53.
- Ludwig Heilmeyer , Herbert Begemann: blood and blood diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition, ibid. 1961, pp. 376-449, here: pp. 395-416 ( anemia ).
Web links
- Anemia chart. University of Heidelberg
- Anemia diagnostics in childhood. Guidelines for diagnosis and therapy in pediatric oncology and hematology
- Aplastic anemia. (PDF) Guidelines for Diagnostics and Therapy in Pediatric Oncology and Hematology
- Guidelines for diagnosis and therapy in pediatric oncology and hematology: sickle cell disease
- Thalassemia. Guidelines for diagnosis and therapy in pediatric oncology and hematology
- Sideroblastic anemia. OrphaNet
Individual evidence
- ↑ Irmgard Müller: Anemia . In: Werner E. Gerabek, Bernhard D. Haage, Gundolf Keil, Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte . De Gruyter, Berlin / New York 2005, p. 53 .
- ↑ hil: anemia-independent risk factor for cardiovascular mortality. In: aerzteblatt.de . September 5, 2013, accessed January 21, 2015 .
- ↑ Labor Lexicon: blood picture, small. In: laborlexikon.de. January 25, 2011, accessed January 21, 2015 . ISSN 1860-966X
- ↑ Labor dictionary on ferritin
- ↑ Labor Lexicon on Transferrin
- ↑ Laboratory dictionary on vitamin B12
- ↑ Labor dictionary on folic acid
- ↑ Nutritional anaemias. Report of a WHO scientific group. In: World Health Organ Tech Rep Ser. 1968; 405, pp. 5-37. who.int (PDF; 1.5 MB)
- ↑ a b Ernest Beutler, Jill Waalen: The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? In: Blood. 2006; 107, pp. 1747-1750.
- ↑ G. Halwachs-Baumann (ed.): Labormedizin. Clinic - practice - case studies. Springer, Vienna / New York 2006.
- ↑ a b c G. Herold u. a .: internal medicine. 2007.
- ↑ Heinz Lüllmannand, Lutz Hein, Klaus Mohr: Pharmacology and Toxicology. 17th edition. Thieme Verlag, 2010, ISBN 978-3-13-368517-7 .
- ^ Roche Lexicon Medicine. [Electronic resource] 5th edition. Elsevier, Urban & Fischer Verlag, Munich / Jena 2003, ISBN 3-437-15072-3 ; Online version Keywords: anemia, sideroachrestic and sideroblast
- ↑ P. Kühnl u. a .: Transfusion of blood components and plasma derivatives . ( Memento from August 19, 2007 in the Internet Archive ; PDF)
- ↑ Guidelines for therapy with blood components and plasma derivatives . 3rd revised and expanded edition. issued by the German Medical Association, OCLC 249422362 .