Human papillomavirus
| Human papillomavirus | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
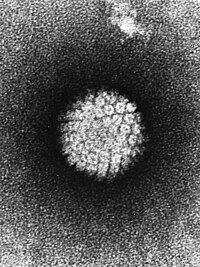
HPV in the electron microscope |
||||||||||||||
| Systematics | ||||||||||||||
|
||||||||||||||
| Taxonomic characteristics | ||||||||||||||
|
||||||||||||||
| Left | ||||||||||||||
|
| Classification according to ICD-10 | |
|---|---|
| B97.7 | Papillomaviruses as the cause of diseases that are classified in other chapters |
| B07 | Viral warts |
| Z22.8 | Carriers of other infectious diseases |
| ICD-10 online (WHO version 2019) | |
Human papillomaviruses ( HPV , also human papillomaviruses , English human papillomaviruses ) form a group of DNA viruses that are now divided into more than 100 different types. The HPV are non-enveloped , double-stranded DNA viruses (dsDNA) and belong to the family of the Papillomaviridae and the genera Alphapapillomavirus , Betapapillomavirus and Gammapapillomavirus . They infect epithelial cells of the skin and various mucous membranes and can cause uncontrolled tumor-like growth in the infected cells. These tumors are usually benign and lead to the formation of warts on the affected skin or mucous membrane (the site of the infection). If the infection develops in the genital or anal area (usually through sexual intercourse), genital warts (e.g. genital warts ) develop .
However, some types of HPV can cause malignant changes, particularly cervical cancer in women. A significant proportion of vaginal, penile and anal cancers are probably also the result of such an HPV infection. HPV infection also seems to be involved in the development of basal cell cancer ("white skin cancer"). HPV can also be transmitted to the oral mucosa through oral sex and cause oral tumors there.
The gene products of these viruses, especially those of the E6 and E7 genes, prevent programmed cell death ( apoptosis ) and make it impossible to repair the DNA double strand. The skin changes caused by papilloma viruses are often not visible to the naked eye. The degeneration caused by the virus in the event of uncontrolled growth pose particular problems, for example when the body's defenses are weakened by another disease.
Human papillomaviruses were examined in particular in the laboratories of Harald zur Hausen (who received the Nobel Prize for discovering the connection with cervical cancer) and Gérard Orth from the Pasteur Institute .
Virus groups
A distinction must be made between the classification (based on the clinical picture and course) and the taxonomy (based on the genetic relationship).
classification
So far, 124 HPV types have been fully described. About 30 of them almost exclusively infect skin and mucous membranes in the anogenital area ( anus and genitals ). The genital HPV types can generally be divided into two groups, the low risk and the high risk types. The classification is based on the type of risk: A few pathogens occur extremely frequently in connection with carcinomas.
- The high-risk types have been identified in 99.7% of all cases of cervical cancer (cancerous tumors of the cervix). The majority of cervical cancers (around 70%) are caused by high-risk types 16 and 18, followed by genotypes 31 and 33.
- The low-risk types are almost never directly involved in the development of cervical cancer. In the case of multiple infections (infections with more than one HPV genotype), however, they can also be detected in cervical carcinomas, but then together with a clinically relevant high-risk type.
The types are:
- " Low-risk " viruses
- This group HPV 6 and 11 are counted because it is the main cause of warts (in genital condyloma acuminata no potentially lethal pathogens are called also "warts"). Other low-risk types are 40, 42, 43, 44, 54, 61, 70, 72, 81 and CP6108.
- " High-risk " viruses
- The second group includes v. a. HPV 16, 18, 31 and 33, but also 35, 39, 45, 51, 52, 56, 58, 59, 68, 73 and 82. In almost every occurrence of cervical carcinoma (cancer of the epithelial tissue of the cervix ) at least one is the High-risk HPV groups detectable in an HPV screening. Some cancers of the anus and mouth are also considered to be HPV-associated.
-
possibly high-risk viruses
- HPV 26, 53 and 66 are counted for this purpose.
- Viruses without a clear risk allocation (HPV genotypes of undetermined risk)
In 2005 the IARC officially classified genotypes 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 66 as carcinogenic. The dangerous virus subgroups have been shown not only to be involved in the development of cervical cancer, but are also found in cancers of the penis , the vulva (external female genitalia), the anus and the throat.
Systematics
The decision about different taxa (taxonomic, i.e. kinship groups) is advised and made by an international body, the International Committee on Taxonomy of Viruses (ICTV). The taxonomy of the Papillomaviridae as of November 2018 is as follows (for genera with only a single species, this has the number 1 and is not specifically listed):
-
- Family Papillomaviridae
-
- Subfamily Firstpapillomavirinae
- Genus Alphapapillomavirus (with species Alphapapillomavirus 1 to 14 )
- Genus Betapapillomavirus (with Species Betapapillomavirus 1 to 6 )
- Genus Gammapapillomavirus (with Species Gammapapillomavirus 1 to 27 )
- Genus Deltapapillomavirus (with species Deltapapillomavirus 1 to 7 )
- Genus Epsilonpapillomavirus (with Species Epsilonpapillomavirus 1 and 2 )
- Genus Zetapapillomavirus
- Genus etapapillomavirus
- Genus thetapapillomavirus
- Genus Iotapapillomavirus (with species Iotapapillomavirus 1 and 2 )
- Genus Kappapapillomavirus (with species Kappapapillomavirus 1 and 2 )
- Genus lambda papilloma virus (with species lambda papilloma virus 1 to 5 )
- Genus Mupapillomavirus (with species Mupapillomavirus 1 to 3 )
- Genus Nupapillomavirus
- Genus Xipapillomavirus (with species Xipapillomavirus 1 to 5 )
- Genus omicron papillomavirus
- Genus Chipapillomavirus (with Species Chipapillomavirus 1 to 3 )
- Genus Pipapillomavirus (with Species Pipapillomavirus 1 and 2 )
- Genus Rhopapillomavirus (with species Rhopapillomavirus 1 and 2 )
- Genus sigmapapillomavirus
- Genus Taupapillomavirus (with species Taupapillomavirus 1 to 3 )
- Genus Upsilonpapillomavirus (with Species Upsilonpapillomavirus 1 to 3 )
- Genus Phipapillomavirus
- Genus Psipapillomavirus (with species Psipapillomavirus 1 to 3 )
- Genus omegapapillomavirus
- Genus Dyodeltapapillomavirus
- Genus Dyoepsilonpapillomavirus
- Genus Dyozetapapillomavirus
- Genus dyoetapapillomavirus
- Genus Dyothetapapillomavirus
- Genus Dyoiotapapillomavirus (with species Dyoiotapapillomavirus 1 and 2 )
- Genus Dyokappapapillomavirus (with species Dyokappapapillomavirus 1 to 5 )
- Genus Dyolambdapapillomavirus
- Genus Dyomupapillomavirus
- Genus Dyonupapillomavirus
- Genus Dyoxipapillomavirus (with species Dyoxipapillomavirus 1 and 2 )
- Genus dyoomicron papillomavirus
- Genus dyopipapillomavirus
- Genus dyorhopapillomavirus
- Genus Dyosigmapapillomavirus
- Genus Dyotaupapillomavirus
- Genus Dyophipapillomavirus
- Genus Dyoupsilonpapillomavirus
- Genus dyopsipapillomavirus
- Genus Dyoomegapillomavirus
- Genus Treisdeltapillomavirus
- Genus Treisepsilonpapillomavirus
- Genus Treiszetapapillomavirus
- Genus Treisetapapillomavirus
- Genus Treisthetapapillomavirus
- Genus Treisiotapapillomavirus
- Genus Treiskappapillomavirus
-
- Subfamily Secondpapillomavirinae
- Genus alefpapillomavirus
-
transmission
The infection runs mainly through skin contact, with certain virus types primarily through unprotected sexual intercourse ( genital , anal or oral intercourse ). HPV infection is therefore one of the most common sexually transmitted infections , but the infection often goes unnoticed. Condoms can cut the risk of infection in half. The viruses are also rarely transmitted through shared towels, drinking glasses or toothbrushes. In the context of an existing infection, pubic hair removal by shaving can lead to an infection of previously unaffected areas of the body.
frequency
In women under 30 years of age, the infection rate is up to 25%. For those over 30, it is still up to 8%. HPV infection often heals within months to a year and a half. The general immunity of women also plays an important role here, so smokers have a higher risk.
There are no general figures on infection rates in men. The reason for the lack of figures is the lack of regular medical check-ups in this area for men. It is known that if one partner has lesions , there is a high probability that the other is also infected with HPV. Up to 70% of the male partners of a woman who tested positive in HPV screening also have an infection, but this often only causes the smallest lesions on the penis. Men are therefore often not even aware of the infection with the HP virus and do not even notice it. Yet they are carriers.
A study of 838 American women between the ages of 14 and 19 presented by the US Center for Disease Control and Prevention (CDC) in March 2008 showed that 18.3% of them were papilloma virus carriers.
Consequences of illness
After infection, papillomaviruses can often remain inactive for years . This applies to both low-risk and high-risk viruses. This means that even weeks to months or up to a year after sexual contact, both heterosexual and homosexual couples can develop genital warts, making the search for the infectious sexual partner very difficult. The most common sequelae are warts, especially genital warts ( condylomata acuminata ), and in women cervical cancer (cancer of the cervix).
HPV belongs together with the hepatitis B virus (HBV), the hepatitis C virus (HCV), the Epstein-Barr virus (EBV), the human T-lymphotropic virus 1 (HTLV-1) and the human herpes virus 8 (HHV-8, also Kaposi's sarcoma herpesvirus, KSHV) to a group of human carcinogenic viruses ( oncoviruses ), which are responsible for 10 to 15 percent of all cancers worldwide .
If an infection with papillomavirus occurs in combination with a certain genetic defect, a chronic, generalized HPV infection known as epidermodysplasia verruciformis can develop.
Overview
| HPV types | Consequences of illness |
|---|---|
| HPV types 6 and 11 ("low risk") | Condylomata acuminata ("genital warts", virus warts of the mucous membrane) and Buschke-Löwenstein tumor |
| HPV types 6 and 11 ("low risk") as well as 16, 18 and 31 ("high risk") | Condylomata plana (referred to as CIN, VIN, VAIN, AIN and PIN depending on the location) |
| HPV types 16, 18, 45 and 31 ("high risk") | Cervical intraepithelial neoplasia (CIN): can lead to cervical cancer ( cervical cancer ) |
| HPV types 16 and 18 ("high risk") | Oropharyngeal cancer |
| HPV type 16 ("high risk") - (almost exclusively this type) | Bowenoid papulosis , most intraepithelial neoplasia in men than Penile (PIN, viral warts of the penis ) can Erythroplasia and penis cancer cause |
| HPV types 16, 18, 45 and 31 ("high risk") | Vulvar intraepithelial neoplasia (VIN, viral warts of the vulva ) |
| HPV types 16, 18, 45 and 31 ("high risk") | Vaginal intraepithelial neoplasia (VAIN, viral warts of the vaginal mucosa ) |
| HPV types 16, 18, 45 and 31 ("high risk") | Anal intraepithelial neoplasia (AIN, viral warts of the anus ) |
| HPV types 13 and 32 ("low risk") | Heck's disease (viral warts of the oral mucosa ) |
| HPV types 1, 2, 3 and 4 | Verruca vulgaris (common skin wart) |
| HPV types 1, 2, and 4 | Verruca plantaris (plantar wart) |
| HPV types 3 and 10 | Verruca plana juvenilis (juvenile flat warts) |
| HPV type 7 | "Butcher's wart" |
| HPV types 5 and 8 (“intermediate risk”), as well as occasionally the other types of the EV group: 5, 8, 9, 12, 14, 15, 17, 19, 20, 21 and 47 | Epidermodysplasia verruciformis (EV) |
partly from:
Men and HPV
Several studies show that around 64 to 70% of male partners of women who suffer from HPV disease of the cervix themselves have HPV-associated lesions on the penis. HPV can often remain undetected for a long time in the skin of the penis. In rare cases, malignant changes, including carcinomas, can occur in the penis. Because the penile cancer in circumcised is extremely rare men who retained (retiniertes) are Smegma , and repeated infections of the foreskin and the glans (chronic balanitis ) in uncircumcised men as decisive factors of the gradual in time as well as causal respects development of cancer ( carcinogenesis viewed). However, infection with the human papillomavirus alone and the cytomegalovirus are also considered to be the cause.
Several studies suggest that HPV infections can cause oral cancer. Among other things, a French study diagnosed a high number of oral cancer patients with human papilloma viruses. Oral intercourse is the mode of transmission . There is no reliable protection. However, the strict use of condoms presumably reduces the risk of transmission, see also safer sex .
In men who have passive anal intercourse with other men, genital warts can also appear in the area of the anus . The symptoms (itching, burning) of an anal infection with HPV are initially difficult to assign, especially since the condylomata in that area are even more difficult to recognize. If they can already be seen with the naked eye or can be clearly felt, the stage is usually so advanced that surgical removal is necessary. Since this is associated with a painful healing phase and sometimes has to be carried out several times due to the limited chance of success, men with suspected anal genital warts should opt for a proctological examination at an early stage .
Anal HPV infections occur v. a. in homosexual men and women. In gay men, anal HPV infections are more common than penile infections.
In Germany, vaccination for 9 to 14-year-old boys has been recommended by the Standing Vaccination Commission (STIKO) since 2018 , the costs are covered by the health insurance until their 18th birthday.
diagnosis
The fact that high-risk types occur in 99.7% of cervical carcinomas (HPV 16: 50%, HPV 18: 20%), compared to an otherwise low rate, underlines the importance of HPV infection in this carcinoma, which is worldwide is the second most common cancer (and third leading cause of cancer death) in women. The DNA of the HP viruses can be detected by means of the polymerase chain reaction (PCR) and further differentiated between the different types by sequencing or hybridization . At low virus concentrations (as with any PCR), false negative results also occur. The detection of HP viruses without further signs of a change in the mucous membrane on the cervix does not allow any statement to be made about a possible risk of carcinoma, since the infection heals without consequences in over 98% of cases.
therapy
- Article on Symptom Treatment of HPV Warts: Condylomata acuminata # Treatment
There is currently no specific papilloma virus therapy. If the lesions are present, surgical interventions or local burns are the main options. As a rule, the healing process begins with the removal of the lesion, although relapses (recurrences) are common. Systemic or local therapies, for example with interferons and other cytokines , have so far not led to any resounding success.
Photodynamic therapy was tested in a study in Mexico . All patients without lesions were free of HPV at the end of treatment; in patients with lesions the figure was 57%.
Preventive vaccination
The HPV vaccine Gardasil from the US pharmaceutical company MSD Sharp & Dohme (sold in Austria and Germany by the joint venture between Merck (USA) MSD and Sanofi-Aventis Sanofi Pasteur MSD ) for the preventive vaccination against some cervical cancer causing HPV has been in Europe since the end Approved in September 2006, available in Germany since October and approved in the USA in June 2006. A second vaccine, Cervarix , from GlaxoSmithKline was approved in Germany in autumn 2007.
The Standing Vaccination Commission first recommended in the Epidemiological Bulletin of March 23, 2007 that 12 to 17 year old girls should be vaccinated against HPV. In 2009 some scientists called for a reassessment of HPV vaccination. The question that was still open at the time as to whether an HPV vaccination could actually reduce the incidence of cervical cancer and its precursors has now been answered: In Australia, a 75% decrease in cancer precursors was observed in young girls after vaccination was introduced. Another Australian study confirms a positive effect even for young men who have not been vaccinated and who now develop genital warts less often. The German Society for Gynecology and Obstetrics , the Professional Association of Gynecologists , the Federal Center for Health Education and many other institutions therefore recommend vaccination for the prevention of cervical cancer without reservation. Gardasil immunizes against the high-risk HPV genotypes 16 and 18 as well as the low-risk types 6 and 11 and is approved for both sexes from 9 years of age. Cervarix immunizes against the two high-risk genotypes 16 and 18. The statutory health insurance companies have so far paid for the HPV vaccination in Germany for girls and young women between 12 and 17 years of age. However, the STIKO lowered the recommended vaccination age for vaccination against HPV in August 2014. The Federal Joint Committee (GBA) has adopted the revised vaccination recommendations. This means that the financing of HPV vaccinations for girls between the ages of 9 and 14 is enshrined in law. However, up to the age of 18, the health insurances must also offer vaccination for women. At the age of 9 to 13, only 2 vaccine doses are required instead of the previous 3. From an older age or a shorter vaccination interval than 6 months between the 1st and 2nd vaccination, 3 doses are still required.
Both vaccines have a preventive effect; an already existing HPV infection cannot be treated or eliminated with it. Nor can the consequences of such an infection, such as cervical cancer or its precursors, be treated with a vaccination. Preventive examinations for early detection of cervical cancer ( Pap test ) are still necessary despite vaccinations.
According to a Canadian study published on May 28, 2018, of 291,000 girls aged 12 to 17 years, they were not exposed to an increased risk of autoimmune diseases as a result of the vaccination . A meta-analysis by the Cochrane Collaboration of over 70,000 subjects in 2018 concluded that prophylactic vaccination is safe and effective against cervical cancer. Scientists from Scotland also shared this view. The analysis of more than 100,000 health records showed that routine HPV vaccinations in girls aged 12-13 years significantly reduced the likelihood of abnormal cells and cervical intraepithelial neoplasia . The earlier an HPV vaccination took place, the more effective the HPV vaccination was.
The Standing Vaccination Commission (STIKO) has recommended vaccination for 9 to 14-year-old boys since 2018 ; the costs are covered by health insurance until their 18th birthday.
Other prevention options
An effective measure to prevent infection is safer sex , which significantly reduces the risk of HPV infection, but cannot completely prevent it. This is particularly due to the fact that HPV infection is not a classic sexually transmitted disease. B. the gonorrhea is transmitted via the sperm or other body fluids, but a contact infection, whereby body parts outside the area protected by the condom can serve as a source of infection.
One study found a lower risk of cervical cancer in the partners of high-risk men who had unprotected sex with prostitutes who had been circumcised : monogamous partners are statistically less likely to develop cervical cancer if the man is circumcised and none has unprotected sex with prostitutes. In the present study, the probability found is moderate, but not significantly lower (“ moderate, but nonsignificant, decrease in the risk of cervical cancer ”) and is therefore not adequately confirmed scientifically.
Web links
- Human papillomavirus (HPV) - information from the Robert Koch Institute
- Mobilization against Cancer Report on research to develop a vaccine against HPV-16
- Ulf Schleth: HPV and vaccination: infected below. In: taz.de . October 7, 2018, accessed November 23, 2019 .
- How much protection does the HPV vaccination offer against cervical cancer?
- Questions about the clinical trial and the approval of the Paul Ehrlich Institute to criticize the approval of the HPV vaccine ( Memento from February 3, 2009 in the Internet Archive )
Individual evidence
- ↑ a b c d e ICTV: ICTV Taxonomy history: Alphapapillomavirus 1 , EC 51, Berlin, Germany, July 2019; Email ratification March 2020 (MSL # 35)
- ↑ a b c Alphabetical directory for the ICD-10-WHO Version 2019, Volume 3. German Institute for Medical Documentation and Information (DIMDI), Cologne, 2019, p. 674.
- ↑ UV radiation alone does not cause skin cancer. In: welt.de . July 20, 2011, accessed May 22, 2015 .
- ↑ Koh: Viruses promote UV-induced skin cancer. In: dkfz.de. November 23, 2010, accessed May 22, 2015 .
- ↑ D. Viarisio, K. Mueller-Decker et al .: E6 and E7 from beta HPV38 cooperate with ultraviolet light in the development of actinic keratosis-like lesions and squamous cell carcinoma in mice. In: PLoS pathogens. Volume 7, number 7, July 2011, ISSN 1553-7374 , p. E1002125, doi: 10.1371 / journal.ppat.1002125 , PMID 21779166 , PMC 3136451 (free full text).
- ↑ Doctors newspaper: Does oral sex lead to oral tumors? In: aerztezeitung.de. May 16, 2012, accessed May 22, 2015 .
- ↑ N. Muñoz et al .: Epidemiologic classification of human papillomavirus types associated with cervical cancer. In: The New England Journal of Medicine . Volume 348, Number 6, February 2003, pp. 518-527, ISSN 1533-4406 . doi: 10.1056 / NEJMoa021641 . PMID 12571259 .
- ^ V. Cogliano et al .: Carcinogenicity of combined oestrogen-progestagen contraceptives and menopausal treatment. In: The Lancet Oncology . Volume 6, Number 8, August 2005, pp. 552-553, ISSN 1470-2045 . PMID 16094770 .
- ↑ SIB: Deltapapillomavirus , on: ViralZone
- ↑ SIB: Mupapillomavirus , on: ViralZone
- ↑ SIB: Nupapillomavirus , on: ViralZone
- ↑ Human papilloma viruses (HPV) ( Memento from March 8, 2017 in the Internet Archive ), Doctors in the Net GmbH
- ↑ RL Winer u. a .: Condom use and the risk of genital human papillomavirus infection in young women. . In: The New England Journal of Medicine . 354, No. 25, 2006, pp. 2645-2654. PMID 16790697 .
- ↑ D. Martin, JS Gutkind: Human tumor-associated viruses and new insights into the molecular mechanisms of cancer. In: Oncogene. Volume 27 Suppl 2, December 2008, ISSN 1476-5594 , pp. S31-S42, doi: 10.1038 / onc.2009.351 , PMID 19956178 (review).
- ↑ T. Patel et al .: Epidermodysplasia verruciformis and susceptibility to HPV. In: Disease markers. Volume 29, number 3-4, 2010, ISSN 1875-8630 , pp. 199-206, doi: 10.3233 / DMA-2010-0733 , PMID 21178278 , PMC 3835378 (free full text) (review).
- ↑ Peter Fritsch: Dermatology and Venereology. 2nd Edition. Springer Verlag, 2004, ISBN 3-540-00332-0 .
- ↑ Wolfgang F. Caspary, Manfred Kist, Jürgen Stein (eds.): Infectiology of the gastrointestinal tract . Springer, 2006, ISBN 978-3-540-41359-2 , pp. 315 ( limited preview in Google Book search).
- ↑ N. Kiviat et al .: Anal human papillomavirus infection among human immunodeficiency virus-seropositive and -seronegative men. In: The Journal of Infectious Diseases. Volume 162, Number 2, August 1990, pp. 358-361, ISSN 0022-1899 . PMID 1973695 .
- ↑ a b RKI - STIKO recommendations - preliminary information: STIKO recommends HPV vaccination for boys. Retrieved June 11, 2018 .
- ↑ a b spiegel.de
- ↑ Alexis Ortiz: Mexican scientist cures Human Papilloma Virus. February 6, 2019, accessed February 9, 2019 .
- ↑ FDA Licenses Quadrivalent Human Papillomavirus (Types 6, 11, 16, 18) Recombinant Vaccine (Gardasil) for the Prevention of Cervical Cancer and Other Diseases in Females Caused by Human Papillomavirus ( Memento of May 22, 2009 in the Internet Archive )
- ↑ ( page no longer available , search in web archives )
- ↑ rme: Deutsches Ärzteblatt: Early regression of cervical lesions due to HPV vaccination. In: aerzteblatt.de . June 20, 2011, accessed May 22, 2015 .
- ↑ H. Ali et al .: Genital warts in young Australians five years into national human papillomavirus vaccination program: national surveillance data. In: BMJ (Clinical research ed.). Volume 346, 2013, p. F2032, ISSN 1756-1833 . PMID 23599298 .
- ↑ Erin Y. Liu et al .: Canadian Medical Association Journal: Quadrivalent human papillomavirus vaccination in girls and the risk of autoimmune disorders: the Ontario Grade 8 HPV Vaccine Cohort Study. May 28, 2018, accessed June 3, 2018 .
- ↑ Marc Arbyn et al .: Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursor . In: The Cochrane Library . John Wiley & Sons, Ltd, May 9, 2018 ( cochranelibrary-wiley.com [accessed June 11, 2018]).
- ^ Deutscher Ärzteverlag GmbH, editorial office of the Deutsches Ärzteblatt: The HPV vaccination works. April 11, 2019, accessed May 27, 2019 .
- ↑ Tim Palmer et al .: Prevalence of cervical disease at age 20 after immunization with bivalent HPV vaccine at age 12-13 in Scotland: retrospective population study . In: BMJ . tape 365 , April 3, 2019, p. l1161 , doi : 10.1136 / bmj.l1161 , PMID 30944092 .
- ^ A. Bhimji, D. Harrison, Male circumcision, penile human papillomavirus infection, and cervical cancer. (PDF) In: The New England Journal of Medicine . Volume 347, Number 18, October 2002, pp. 1452-1453, ISSN 1533-4406 . PMID 12418039 .


