lung infection
When pneumonia or pneumonia , latin Pneumonia (from ancient Greek πνεύμων Pneumon , German , lungs' ; at Hippocrates πεεριπνευμονία peripneumonia ), there is an acute or chronic inflammation of the lung tissue which is either unilateral (one-sided, that is in only one lung) or occurs bilaterally (on both sides, i.e. in both lungs at the same time). It is mostly caused by an infection with bacteria , virusesor fungi , more rarely also chemically, e.g. B. by inhalation of toxic substances or aspiration of acidic gastric juice, or by immunological (such as allergic) processes. If the pleura (pleura) is clearly involved in the form of pleurisy , it is referred to as pleuropneumonia in clinical usage . The inflammation after radiation therapy is usually referred to as radiation pneumonitis.
| Classification according to ICD-10 | |
|---|---|
| J18.- | Pneumonia, pathogen unspecified |
| J17 .- * | Pneumonia in Diseases Classified Elsewhere |
| P23.9 | Congenital pneumonia, unspecified |
| J84.9 | Interstitial lung disease, unspecified |
| Further: | Classification under the specific pathogens or other causes |
| ICD-10 online (WHO version 2019) | |
Classification and causes
Since a division of pneumonia after the pathogen (bacteria obligate, intracellular bacteria such as Rickettsia and Chlamydia , viruses, mycoplasma , fungi , protozoa , worms ) often fails because of the lack of detection of pathogens, themselves following classifications have prevailed that for further diagnostics and therapy of Meaning are.
Primary and secondary pneumonia
A distinction is made between primary and secondary pneumonia: If a healthy person suffers from pneumonia without showing any particular risk factors, one speaks of primary pneumonia. In contrast, secondary pneumonia has a predisposing factor or a triggering event for the disease (see risk groups ).
Primary pneumonia pathogens are mostly pneumococci , staphylococci , Haemophilus influenzae , mycoplasmas , chlamydia , legionella and, in the case of viral pneumonia, viruses such as the flu virus , adenovirus and parainfluenza viruses. In secondary pneumonia, the spectrum of pathogens shifts to herpes viruses ( CMV , HSV ), fungi, Pneumocystis jirovecii , protozoa (toxoplasmosis) and anaerobic bacteria.
Clinical classification
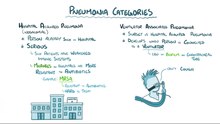
For the assessment of the pathogen spectrum, diagnostic considerations, the further therapy and the course, the pneumonias are classified according to the situation in which they were acquired:
- Ambulatory , that is one in everyday life outside of a hospital -acquired pneumonia (abbreviated as AEP for, community-acquired pneumonia 'or English community-acquired pneumonia, CAP ). This includes pneumonia acquired in old people's or nursing homes. A distinction is made between community-acquired pneumonia that can be treated on an outpatient basis ( called aCAP ) and those that require inpatient admission and are referred to as hCAP . Common pathogens are Streptococcus pneumoniae , Haemophilus influenzae , Mycoplasma pneumoniae , Chlamydophila pneumoniae and, rarely, Legionella pneumophila .
- If there is severe community-acquired pneumonia , it is referred to as sCAP ( severe community-acquired pneumonia ). An sCAP is present when the inflammation localized in the lungs spreads generalized to the body and leads to sepsis-associated complications such as sepsis , septic shock or organ failure . An sCAP has a high lethality and requires intensive antibiotic therapy - often also ventilation therapy in an intensive care unit. The presence of sCAP can be differentiated from normal CAP on the basis of various clinical criteria.
- Nosocomial pneumonia , that is in hospital-acquired pneumonia ( English hospital-acquired pneumonia, HAP ) is the only more developed than two days after admission and up to 14 days after discharge. A special form is the ventilator associated pneumonia ( ventilator-associated pneumonia, VAP ). In frequent pathogens are Pseudomonas aeruginosa , Enterobacter , E. coli , Proteus , Serratia , Klebsiella pneumoniae (Friedlander pneumonia).
- Pneumonia acquired from immunocompromised , i.e. immune-compromised patients. The immunosuppression can be caused by diseases such as AIDS, or it can be brought about and desired by drugs, e.g. B. after organ transplants.
Community-acquired pneumonia usually has a good prognosis. Nosocomial pneumonia requires more aggressive treatment right from the start. Special pathogens such as mycobacteria , which can cause tuberculosis , can occur more frequently in immune-weakened patients .
Epidemiology
Community-acquired pneumonia is the second most frequently registered infectious disease worldwide after diarrheal diseases and is therefore of great socio-medical and economic importance. Around 90% are of bacterial origin.
In the United States alone, two to three million cases are diagnosed each year, resulting in ten million GP contacts and around 500,000 hospital admissions.
There is no comparable data for Germany, especially about how many AEP cases are treated exclusively in the outpatient setting. The incidence (= number of new cases of illness) in the general population is estimated at one to eleven cases per 1000 inhabitants and year, and at 68 to 114 cases per 1000 people for retirement home residents. This corresponds to around 400,000–600,000 cases per year in Germany. Over 30% of the sick have to be treated in the hospital, 10% of them in the intensive care unit (i.e. approx. 3% of all patients with community-acquired pneumonia). Community-acquired pneumonia thus led to inpatient admission more often than myocardial infarction (132,000 admissions) or apoplexy (= stroke, 162,000 admissions). Around 20,000 people die of pneumonia in Germany every year. The costs caused by the disease are likely to be more than 500 million euros per year. Among the pathogens, pneumococci are leading with around 25 to 45% of AEPs, followed by Haemophilus influenzae (5 to 20%). Mycoplasma pneumoniae (5 to 15%) is particularly important in younger people. However, these numbers come mainly from examinations of inpatients, so that, due to the selected patient population, they probably do not reflect the distribution in the outpatient area. Viruses are also detected in 5 to 25% of cases , often involving bacteria. Influenza viruses are particularly common, with a superinfection by pneumococci often occurring .
Pneumonia contributes significantly to child mortality worldwide : According to Save the Children, almost one million children die from pneumonia every year.
Typical and atypical pneumonias
Traditionally, a distinction is made between typical pneumonia caused by bacteria such as pneumococci or staphylococci, and atypical pneumonia caused by viruses, fungi or obligate intracellular bacteria. This distinction is associated with a characteristic distribution of the findings in the X-ray image:
- The typical lobar pneumonia starts (acute pneumonia acuta , also called acute pneumonia ), is on one or more lung lobes limited, comes with fever , chills , cough , purulent mucus, poor general condition and typical Auskultationszeichen associated. There are signs of inflammation in the blood : increased sedimentation rate , leukocytosis , increased acute phase proteins . Pleural effusions are frequent and pronounced. The pathogens are mostly pneumococci ( Streptococcus pneumoniae ), which were first detected as pathogens by Albert Fraenkel in 1886 , but also staphylococci and Klebsiella , Pseudomonas or Proteus . In older patients, the signs of inflammation (fever, typical blood values) may be absent from lobar pneumonia. The typical phases of lobar pneumonia , which establish a connection between histological structural changes and pathophysiology , are: coupling> red hepatization > gray hepatization> yellow hepatization> lysis.
- Atypical pneumonia or interstitial pneumonia often begin less acutely, are accompanied by only moderate fever and are usually accompanied by headache and body aches . In this type of pneumonia, the pathogens (chlamydia, rickettsiae, mycoplasma , legionella , Pneumocystis jirovecii , Coxiella burnetii , also viruses) are absorbed by alveolar macrophages and thus enter the interstitium (tissue between the alveoli), which distinguishes them from alveolar pneumonia. The inflammatory process therefore takes place in the “framework” of the lungs . An unproductive cough (no pus formation) and structures tracing the interstitium in the X-ray are characteristic signs.
- Between them is bronchopneumonia (also called focal pneumonia , lobular pneumonia ), which develops as a secondary pneumonia from a descending bronchitis and is noticeable by a focal, bronchial distribution in the lung tissue.

It must be said, however, that the X-ray findings do not allow any reliable conclusions to be drawn about the spectrum of pathogens in question.
With the introduction of antibiotics , chemotherapeutics and immunosuppressants , but also with the general increase in life expectancy, the spectrum of pneumonia has changed significantly in the last 70 years. Whereas in the past pneumococci were primarily responsible for pneumonia, today viruses and obligate intracellular bacteria have become more common.
risk groups
Classical risk groups usually develop secondary pneumonia. People with the following predisposing factors are at increased risk:
- Age
- general immune deficiency, e.g. B. HIV infection, chemotherapy , immunosuppression , cancer , leukemia , diabetes mellitus , liver cirrhosis and alcoholism
- small children
- chronic heart failure (heart failure)
- Underlying diseases of the lungs, e.g. B. severe chronic bronchitis , COPD , cystic fibrosis , pulmonary fibrosis , bronchiectasis, and emphysema
- Kidney disease (e.g. pyelonephritis )
- Scleroderma
- Allergies
In addition, certain events can increase the risk of pneumonia:
- Tobacco smoking
- Poisoning (e.g. alcohol, drugs)
- acute heart failure with consecutive backlog of blood ("congestion pneumonia")
- Bed rest (due to shallow, obstructed breathing)
- Aspiration of stomach acid , food residues, oil, water, foreign bodies ( aspiration pneumonia )
- Relocation of a bronchus , e.g. B. from a bronchial carcinoma (" cancer pneumonia ")
- Intubation or tracheotomy , because here the natural defense mechanisms are undermined (especially the mucociliary clearance )
- Radiation pneumonitis after exposure to radiation
- Pulmonary embolism (infarct pneumonia)
- Legionella in (elderly) immunocompromised people, if they could settle in poorly maintained air conditioning systems . Also hot tubs can become contaminated, even at too low temperature hot water pipes and hot water tank . A Legionnaire's disease is a notifiable disease for 2,001th
Symptoms
The typical pneumonia runs of sudden onset, cough, shortness of breath and strenuous breathing (increase of breathing frequency, u. U. use of accessory respiratory muscles ), purulent (sometimes bloody) sputum, fever, chills , increased pulse , chest pain and an exudate caused pleural effusion .
The atypical pneumonia is characterized by insidious onset, cough, shortness of breath less, little and mostly clear sputum, headache and body aches, low fever.
The following symptoms are in the foreground in children : shortness of breath with labored breathing (increased breathing frequency, nostril breathing, possibly use of auxiliary respiratory muscles ), excruciating cough that does not improve with symptomatic therapy, paleness, in severe cases also cyanosis and poor circulation.
Examinations and diagnostics
The selection of examination methods (diagnostics) depends on the type of pneumonia. In the case of nosocomial, severe and secondary pneumonia, a pathogen detection for targeted therapy is usually sought. In contrast to this, uncomplicated, primary and community-acquired pneumonia are only treated according to the clinical picture; more aggressive diagnostics and therapy are only started if the therapy fails.

Signs of inflammation
Patients with pneumonia usually have a fever and elevated levels of CRP and leukocytes in the blood ( leukocytosis of over 12,000 / mm 3 ). In addition, the lowering of blood cells is greatly accelerated.
Auscultation and palpation
By listening ( auscultation ) of the lungs with a stethoscope , typical breathing noises such as fine-bubble rattling noises can be determined when the air-conducting parts are affected. This fine crackling that occurs in the infiltration stage is called crepitatio (indux) . The inflamed air bubbles crackle when you inhale and exhale. In contrast, interstitial pneumonia, which first affects the lungs, does not cause any altered breathing sounds. The fremitus may like the bronchophony be reinforced. The physical examination of the patient using auscultation and percussion is only of limited informative value (sensitivity and specificity around 60%).
roentgen
If pneumonia is suspected, two x-rays of the lungs are usually taken . In the X-ray image , poorly ventilated areas appear bright. B. indicate pneumonia. This change ( infiltrate ) is caused by the immigration of leukocytes (infiltration) and the inflammation-related swelling. If the air-conducting parts of the lungs and the alveoli are not affected - as in interstitial pneumonia (inflammation of the connective tissue between the alveoli) - they are shown in the X-ray image (positive bronchopneumogram). If, on the other hand, the alveoli can no longer be seen in the inflamed area, this indicates that there is liquid there and the inflammation is taking place in the alveoli, e.g. B. in lobar pneumonia.
The differentiation of severe tracheobronchitis from bronchopneumonia is difficult and sometimes only possible during the course.
Further diagnostics
The following examinations can be added for special questions and difficult processes:
- Ultrasound of the pleural space to detect a pleural effusion and an infiltrate close to the pleural space
- Computed tomography of the lungs
- Detection of pathogens in the blood ( blood culture ), sputum , tracheal secretions , bronchial secretions , bronchoalveolar lavage or pleural effusion, in special cases also in gastric juice
- in rare cases, lung biopsy
- Antibody search and pathogen DNA in the blood if viral diseases are suspected
- Urine test if pneumococci and legionella are suspected (antigen test)
Differential diagnoses
The following diseases can have symptoms and test results similar to those of pneumonia:
- Bronchial carcinoma
- Pulmonary tuberculosis
- Pulmonary embolism with infarction
- Pulmonary fibrosis
therapy
General principles of pneumonia therapy are:
- Antibiotic administration depending on the pathogens to be expected, the severity of the disease or special risk factors such as older age, concomitant diseases, previous therapy with antibiotics and previous treatment in the hospital,
- fever-lowering measures, only if necessary, especially if you have a high fever; z. B. calf wraps or the administration of antipyretic drugs such as paracetamol or acetylsalicylic acid (ASA),
- adequate fluid intake of at least 1.5 l per day,
- bed rest and thromboembolism prophylaxis for high fever ,
- early mobilization , respiratory therapy,
- if necessary oxygen via nasogastric tube, if necessary ventilation,
- expectorant measures such as inhalations and expectorant drugs, e.g. B. Acetylcysteine (ACC) or Ambroxol ,
- cough suppressants ( antitussives ) for excruciating, unproductive, dry cough, e.g. B. with codeine .
If certain risk factors are present (e.g. CRB65 or CURB above 0) or according to the doctor’s individual assessment, the patient should be admitted to the hospital; if the disease is severe, it may also be admitted to the intensive care unit (a modified ATS score).
As antibiotics usually come aminopenicillins such as ampicillin or cephalosporins (eg. B. ceftriaxone optionally in combination with β-lactamase inhibitors such as sultamicillin and macrolides such as clarithromycin alternative) is used, a fluoroquinolone of the fourth generation as monotherapy. In milder cases, doxycycline or clarithromycin can also be used. An improvement usually occurs within two days.
In children with community- acquired pneumonia, the use of specific antibiotics is recommended. These work just as well as broad spectrum antibiotics , but are more specific for the most common causative germs.
Secondary and nosocomial pneumonia
The treatment of secondary pneumonia is much more difficult and usually requires hospital admission. The focus is on the pathogen detection in order to be able to carry out a causal and specific therapy with antibiotics, antimycotics or virostatics . In the case of nosocomial pneumonia in particular, treatment is made more difficult by resistance to antibiotics. In addition to general measures, the underlying disease is always treated - as far as possible - in the case of secondary pneumonia. In severe cases, mechanical ventilation can save lives, but there is a risk of further lung damage from ventilation.
Specific therapy
- Pneumonia with viruses of the herpes group ( cytomegalovirus , varicella-zoster virus , herpes virus ): administration of antivirals ("acyclovir", "ganciclovir")
- Pneumocystis pneumonia (PCP), atypical pneumonia in immunosuppressed and AIDS patients, as well as premature infants: early administration of cotrimoxazole , early indication of ventilation
- Fungal pneumonia, also in immunosuppressed people and with long-term antibiotic administration: Amphotericin B administration
- Aspiration pneumonia: sucking off the aspirate, removing foreign bodies
- Legionella pneumonia, especially in the elderly: administration of macrolides
maintenance
Professional care must be focused on three tasks:
- Patient observation for early detection of possible complications such as lack of oxygen, poor circulation
- Respiratory support, e.g. B. by suitable storage
- Fever control
Possible complications
- Pleurisy ( pleurisy )
- Acute progressive lung failure (ARDS)
- Lung abscess , pulmonary gangrene
- Pulmonary fibrosis
- Pleural empyema (accumulation of pus in the area of the pleura and pleura outside the lungs)
- Pleural effusion (accumulation of fluid in the pleura and pleura outside of the lungs)
- Sepsis ("blood poisoning")
- The body's own inflammatory defense reactions of the whole organism (SIRS)
- Pneumatocele (encapsulated or enclosed air pockets connected to the bronchial system)
forecast
The prognosis is highly dependent on the disposition. Primary, community-acquired pneumonia has a good prognosis; the mortality rate is below 0.5% on average, provided there are no additional risk factors . Secondary and nosocomial pneumonia, on the other hand, have an extremely poor prognosis, which worsens when the risk factors are added up. Since the introduction of antibiotics, the average death rate due to age-related, more severe complications in an aging society has not improved.
For the prognosis assessment, the prognosis scores CRB-65 and CURB-65 have proven themselves . With the CRB-65 one point is given for:
- C onfusion , confusion ',
- R espiratory rate , respiratory rate '> 30 / min,
- B lutdruck below 90 mm Hg systolic or diastolic below 60 mmHg and
- Age 65 or older.
The CRB-65 is mainly used in outpatient practice because it is based on parameters that are easy to collect. In particular, it helps to decide whether inpatient therapy is necessary. Patients with a CRB-65 value of one point already have a significantly increased mortality risk and should be treated as an inpatient depending on the overall circumstances; inpatient therapy is indicated from two points.
The following estimated mortality values result:
| 0 points | 1-2% |
| 1-2 points | 13% |
| 3–4 points | 31.2% |
prevention
- Vaccination against pneumococci , recommended for patients with a weakened immune system, see also risk groups
- Annual flu vaccination, recommended for people over 60 years of age or who have work-related contact with many people (nursing staff, kindergarten staff, salespeople)
- Haemophilus influenza vaccination
- optimal treatment of high-risk diseases
- Quit smoking
- Consistent wearing of breathing masks in jobs with dust exposure
literature
Guidelines
- German Society for Pneumology and Respiratory Medicine, Paul Ehrlich Society for Chemotherapy, German Society for Infectious Diseases, Competence Network CAPNETZ, Austrian Society for Pneumology, Austrian Society for Infectious Diseases and Tropical Medicine, Swiss Society for Pneumology (publisher):
- S3 guideline: Treatment of adult patients with community-acquired pneumonia and prevention - Update 2016 (pdf, 1 MB)
- S1- Guideline Nosocomial Pneumonia - Epidemiology, Diagnosis and Therapy of Adult Patients of the German Society for Pneumology and Respiratory Medicine (DGP). In: AWMF online (as of 2012)
- Recommendations for the therapy of acute respiratory infections and community-acquired pneumonia (pdf, 40 pages, 3rd edition. 2013). In: Drug Ordinance in Practice (Volume 40, Special Issue 1), published by the Drugs Commission of the German Medical Association (AKdÄ)
- Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 3rd, expanded edition. Verlag Peter Wiehl 2010, ISBN 978-3-927-21920-5 , pp. 82-96.
Textbooks
- Kasper, Braunwald, Fauci , Hauser, Logo, Jameson: Harrison's Principles of Internal Medicine. 16th edition. Part 9 Disorders of the respiratory system. McGraw-Hill Medical Publishing Division, ISBN 0-07-140235-7 , pp. 1528 ff.
- Hilmar Burchardi: Etiology and pathophysiology of acute respiratory failure (ARI). In: J. Kilian, H. Benzer, FW Ahnefeld (ed.): Basic principles of ventilation. Springer, Berlin a. a. 1991, ISBN 3-540-53078-9 , 2nd, unchanged edition, ibid. 1994, ISBN 3-540-57904-4 , pp. 47-91; here: pp. 76–80.
- Reinhard Marre, Manuel Battegay: Clinical Infectiology. Recognize and treat infectious diseases. Elsevier, Urban & Fischer, Munich 2008, ISBN 978-3-437-21741-8 .
- Gerd Herold: Internal Medicine. Taking into account the subject catalog for the medical examination; with ICD 10 key in the text and index; a lecture-oriented presentation. Herold Verlag, Cologne 2006. Edition 2019: ISBN 978-3-981-46608-9 .
- F. Konrad, A. Deller: Clinical examination and surveillance, bacteriological monitoring. In: J. Kilian, H. Benzer, FW Ahnefeld (ed.): Basic principles of ventilation. Springer, Berlin a. a. 1991, ISBN 3-540-53078-9 , 2nd unaltered edition, ibid 1994, ISBN 3-540-57904-4 , pp. 121-133; here: pp. 124–131.
- Joachim Frey : Diseases of the respiratory organs. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 599–746, here: pp. 669–699, especially pp. 669–686 ( inflammation of the lungs ) and 686–693 ( consequences of pneumonia )
Web links
- Pulmonary Information Service: Pneumonia
- Capnetz: patient information pneumonia
- www.pneumonie-aktuell.de - website with pathogen overview , diagnostics, therapy and case reports
- Entry on pneumonia in Flexikon , a Wiki of the DocCheck company
Remarks
- ↑ Cf. Georg Sticker : Hippokrates: Der Volkskrankheiten first and third book (around the year 434-430 BC). Translated, introduced and explained from the Greek. Johann Ambrosius Barth, Leipzig 1923 (= Classics of Medicine. Volume 29); Unchanged reprint: Central antiquariat of the German Democratic Republic, Leipzig 1968, p. 100 f.
- ^ Pneumonia acuta .
- ↑ Pneumonia chronica and Pneumonia recidiva .
- ↑ a b c d e Alphabetical directory for the ICD-10-WHO Version 2019, Volume 3. German Institute for Medical Documentation and Information (DIMDI), Cologne, 2019, pp. 706–708.
- ↑ Not to be confused with HCAP , Health Care-Associated Pneumonia .
- ^ Gert Höffken: Severe, community-acquired pneumonia. In: Intensive Care Medicine. Volume 46, 2009, pp. 474-479.
- ^ BM Schlosser, G. Rohde, E. Marchel, M. Orth, TT Bauer: Outpatient acquired pneumonia. In: pulmonologist. Volume 2, 2005, pp. 28-33.
- ^ Institute for Quality and Patient Safety: Community Acquired Pneumonia. ( Memento of January 13, 2014 in the Internet Archive ) Retrieved October 13, 2011.
- ↑ Revised Global Burden of Disease (GBD) 2002 estimates: Incidence. ( MS Excel ; 167 kB) WHO , 2004, accessed on March 5, 2013 .
- ↑ a b c M. W. Pletz, G. Rohde, H. Schütte, R. Bals, H. von Baum, T. Welte: Epidemiology and pathogens in community-acquired pneumonia (CAP). In: German Medical Weekly (1946). Volume 136, Number 15, April 2011, pp. 775-780, ISSN 1439-4413 . doi: 10.1055 / s-0031-1275806 . PMID 21469047 . (Review).
- ↑ G. Höffken, J. Lorenz, W. Kern, T. Welte, T. Bauer, K. Dalhoff, E. Dietrich, S. Ewig, P. Gastmeier, B. Grabein, E. Halle, M. Kolditz, R Marre, H. Sitter: Epidemiology, diagnostics, antimicrobial therapy and management of adult patients with community-acquired lower respiratory tract infections and community-acquired pneumonia - Update 2009. S3 guidelines of the Paul Ehrlich Society for Chemotherapy, the German Society for Pneumology and Respiratory Medicine , the German Society for Infectious Diseases and the CAPNETZ competence network. In: Pneumology. Volume 63, Number 10, October 2009, pp. E1-68, ISSN 1438-8790 . doi: 10.1055 / s-0029-1215037 . PMID 19821215 .
- ↑ Almost a million children die of pneumonia each year. In: Spiegel Online. November 11, 2017. Retrieved November 13, 2017 .
- ↑ Joachim Frey : Diseases of the respiratory organs. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 599-746, here: pp. 669-677 ( acute pneumonia ).
- ↑ Joachim Frey : Diseases of the respiratory organs. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 599-746, here: pp. 677-680 ( focal pneumonia ).
- ↑ Legionella hysteria costs tenants millions welt.de, on April 17, 2015
- ↑ Noah Lechzin: High coughing of blood. In: MSD Manual. 2018 (online).
- ^ Klaus Holldack, Klaus Gahl: Auscultation and percussion. Inspection and palpation. Thieme, Stuttgart 1955; 10th, revised edition, ibid 1986, ISBN 3-13-352410-0 , pp. 87 f.
- ^ Jörg Braun: Lungs. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 285-310, here: pp. 291-296 ( pneumonia ).
- ^ Jörg Braun: Lungs. 2016, p. 294 ( Calculated antibiotic therapy for pneumonia ).
- ^ MA Queen, AL Myers, M. .. Hall, SS Shah, DJ Williams, KA Auger, KE Jerardi, AM Statile, JS Tieder: Comparative Effectiveness of Empiric Antibiotics for Community-Acquired Pneumonia. In: PEDIATRICS. S., doi: 10.1542 / peds.2013-1773 .
- ^ Jörg Braun: Lungs. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 285-310, here: pp. 291-296 ( pneumonia ).
- ^ S. Ewig, N. Birkner, R. Strauss, E. Schaefer, J. Pauletzk, H. Bischoff, P. Schraeder, T. Welte, G. Hoeffken: New perspectives on community-acquired pneumonia in 388 406 patients. Results from a nationwide mandatory performance measurement program in healthcare quality. In: Thorax. 2009 Dec; 64 (12), pp. 1062-1069, electronic publication on May 18, 2009.
- ↑ capnetz.de (with numerous links)
- ↑ also published in Pneumology. Volume 70, 2016, pp. 151-200.
- ↑ see also 20th edition 2018 and en: Harrison's Principles of Internal Medicine