Local anesthetic
As a local anesthetic (plural local anesthetics ) are anesthetics for local anesthesia ( local anesthesia called). A distinction is made between injectable local anesthetics and external (external, “ topical ”) local anesthetics (“contact anesthetics”, surface anesthetics) that are applied directly to the skin or mucous membrane. There are active ingredients that are available in both forms. Although their origin can be traced back to cocaine , the modern active ingredients do not have any euphoric or addictive effects. You are not allowed to use narcotics as defined inNarcotics Act , such as morphine or heroin , can be confused.
history
Although the Incas already used coca leaves for local anesthesia, it was not until the middle of the 19th century that a scientifically based use became established. In 1859 the Goslar chemist Alfred Niemann isolated cocaine for the first time at the chemistry faculty in Göttingen and described its local anesthetic effect. In 1884 the Viennese ophthalmologist Carl Koller performed painless eye surgery with cocaine for the first time. The surgeon William Halsted undertook the first conduction anesthesia in 1884 by numbing the inferior alveolar nerve on the mandibular foramen with cocaine. Infiltration anesthesia was introduced by Carl Ludwig Schleich in 1892. In 1899 August Bier injected cocaine into the vertebral canal, inventing spinal anesthesia or even (accidentally) epidural anesthesia . In 1905 Bier also developed the method of intravenous regional anesthesia . The epidural anesthesia was established in 1920 by Fidel Pagés .
At first, cocaine was mainly used. In 1903 (proposed in 1897) the Leipzig surgeon Heinrich Braun extended the duration of cocaine in anesthesia by adding adrenaline . The first synthetic local anesthetics to replace cocaine to gain acceptance in medical practice (surgery) were Stovain by Ernest Fourneau in 1903, tested in clinical practice by the French surgeon Paul Reclus , and Novocaine by Alfred Einhorn in 1904, in clinical practice tested by Heinrich Braun in 1906. Other precursors such as benzocaine , nirvanin (1898, Einhorn), and eukain (Georg Merling 1897) did not succeed. In 1948, with lidocaine , which had been synthesized by the Swedish chemists Nils Löfgren and Bengt Lundqvist in 1943, a local anesthetic of the amide type came onto the market for the first time. Since then, other local anesthetics have been developed again and again, for example chlorprocaine was introduced in 1955.
Chemical structure
The chemical structure of many local anesthetics is similar. They consist of a lipophilic aromatic ring structure, an intermediate chain and a hydrophilic amino group. According to the intermediate chain, a distinction is made between amino esters (local anesthetics of the “ ester type”) and amino amides (local anesthetics of the “ amide type”). The amino esters are metabolized in the tissue by a cholinesterase . The aminoamides are broken down in the liver by N-dealkylation or hydrolysis .
Mechanism of action
Local anesthetics work on the cell membrane of nerve cells . Here they block sodium channels and thereby prevent the influx of sodium ions into the cell and thus the formation of action potentials . In higher concentrations, the potassium channel is also blocked and potassium ions prevented from escaping from the inside of the cell. In this way, the formation and transmission of sensations such as temperature, pressure or pain and the transmission of motor impulses at this point are weakened or completely interrupted.
Most local anesthetics are weakly basic amines and are charged and uncharged at a physiological pH value . The site of action is on the inside of the sodium channels in the cell membrane, so diffusion of the substances into the cell plasma is necessary. Only the uncharged base can get through the cell membrane inside, is protonated here to the charged ammonium form, which is also the active form of the local anesthetic, reaches the binding site of the sodium channel and develops its effect there.
The local anesthetics have a pK S value 7 to 9 in water, they are (protonated) only in the ionized form, that is, at pH values below the respective pK S value. Therefore, they are administered in injection solutions with a pH of 4-6. In the tissue having a pH value of 7.4, the injection solution is buffered and, depending on the pK S value of the local anesthetic 2-30% of the local anesthetic in the nonionized, lipid-soluble form. However, the anesthetic is only effective in the ionized form, so that from a pH value of 9, all local anesthetics become ineffective. Conversely, a low pH value, such as that found in inflamed tissue (pH ≤ 6), can mean that the local anesthetic cannot penetrate the nerve fibers and also remains ineffective.
application
Preparations of this type are used almost exclusively to eliminate pain in medical procedures such as B. Operations and used for pain therapy . In surgery and above all in anesthesia , various methods of local anesthesia have developed over time . These range from simple infiltration anesthesia to the installation of pain catheters near the spinal cord ( epidural anesthesia ).
Various techniques of local anesthesia in dentistry have been developed to eliminate pain in the mouth, jaw and face area.
Some preparations contain adrenaline , noradrenaline or phenylephrine . These so-called vasoconstrictors (also known as blocking bodies in veterinary parlance ) constrict the blood vessels in the effective area and thus reduce the blood flow. This slows down the removal of the local anesthetic and extends the duration of the effect of the local anesthetic. In addition, they lead to an emptiness in the operating theater area and thus a better overview for the surgeon.
The addition of vasoconstrictors applies to surgical use on the acres ( hands , fingers , feet and toes ), nose , ear and penis as so-called off-label use , as an off-label use that may involve liability risks, as there is the risk of end artery occlusion and the resulting tissue necrosis (death of tissues) due to reduced blood flow. However, the addition of vasoconstrictors is still common practice. It was as WALANT anesthesia, (acronym of English wide awake local anesthesia no tourniquet ) entered the surgery. Epinephrine was wrongly accused of causing acral necrosis, because this complication was based - as we know today - on the effects of procaine and its improper storage.
In addition, these substances can cause complications of the cardiovascular system in patients with heart disease .
In spinal anesthesia , the local anesthetic is injected into the subarachnoid space of the spinal canal ; This is where the spinal cord (up to about the 12th thoracic vertebrae, including nerve cords that pull further down) lies in a fluid, the cerebrospinal fluid . For this type of anesthesia there are special preparations to which a glucose solution has been added. These so-called hyperbaric local anesthetics sink after injection into the subarachnoid space, obeying the force of gravity, as they have a higher specific weight than the cerebrospinal fluid due to the admixture . In this way, depending on the patient's position, a targeted expansion of the anesthetized area can be achieved.
External local anesthetics are used to treat painful lesions of the skin and mucous membranes and to combat itching. They are also used for anesthesia of the cornea and conjunctiva during diagnostic and surgical interventions on the eye. They are offered as an ointment , cream , gel , lotio , solution , spray or plaster, depending on the area of application .
unwanted effects
In the case of the undesirable effects, a distinction must be made between what they are due to, and accordingly
- on the anesthetic substance
- an added vasoconstrictor
- an added preservative
- on the concentration and dosage
- on interactions with other drugs
- on the present disease
- a concomitant illness
- an allergy
- if you are pregnant / breastfeeding
- on the application technology.
Local anesthetics can not only block the formation of action potentials in peripheral nerves, but also in other areas such as the brain or heart . Since they are generally (with the exception of intravenous regional anesthesia) applied in the vicinity of peripheral nerves or spinal cord , there are no such systemic effects. However, if too large an amount of the substance used gets into the circulatory system, for example in the case of an intravenous injection unnoticed, this can lead to undesirable effects.
Mode of action
The cause of the undesirable effects is, in addition to the blockage of the sodium channels in the nervous system and in the heart, the disruption of calcium channels and a decoupling of the respiratory chain in the mitochondria . The breathing, which is disturbed by the symptoms, leads to acidosis of the blood, which increases the amount of free local anesthetic due to reduced plasma protein binding and promotes penetration into the nerves and heart cells. To make matters worse, the acidosis increases the blood flow to the brain and thus more local anesthetic reaches it. Finally, intracellular acidosis also develops, which protonates the local anesthetic and prevents it from diffusing out of the cell. This mechanism is called ion trapping ( ion trap called).
The intoxication can be divided into four stages:
- Prodromal stage (perioral numbness, metallic taste)
- Preconvulsive stage (tremor, tinnitus, nystagmus, somnolence)
- Convulsive stage (generalized tonic-clonic seizures)
- Stage of CNS depression (coma, apnea, circulatory collapse)
CNS side effects
If the plasma levels of local anesthetics are too high, it primarily leads to functional disorders of the central nervous system (CNS). These can range from restlessness, dizziness, oral tingling, a metallic taste in the mouth or numbness to generalized seizures and coma. Since the central nervous symptoms are mostly reversible, efforts are made to administer drugs whose CNS side effects occur long before the cardiac ones (high CC / CNS ratio, e.g. ropivacaine).
Cardiotoxicity
At the heart of it, in a high plasma levels be side effects of a local anesthetic. It can lead to a decrease in the strength of the heart (inotropy), a slowdown in the transmission of impulses in the heart and even life-threatening cardiac arrhythmias .
Allergies
Allergies occur primarily with local anesthetics of the ester type ( procaine ), as the breakdown of these substances produces paraaminobenzoic acid , which is held responsible for the allergic reaction ( cross allergy ). In Germany, local anesthetics of the ester type are mostly used topically and only very rarely as an injection. In the case of local anesthetics of the amide type, allergic reactions in particular to certain stabilizers added to the preparations were observed. Especially methyl paraben , which serves as a preservative. Newer local anesthetics of the amide type are made paraben-free. In addition, sodium thiosulphate, which is also used as a preservative, can lead to allergic reactions.
Therapy of intoxication
The therapy focuses on securing the vital functions. Oxygen is administered at 15 l / min through a mask. The transitions between the stages are fluid and not in strict order. In the case of convulsive equivalents, the airways should be secured immediately by intubation. Above all with bupivacaine , but also with ropivacaine , blockages of the conduction system of the myocardium are to be expected due to the high lipophilicity of the substances . This lipophilicity is also the basis for emergency therapy with endovenous lipids (lipid sink).
According to the recommendations of the German Society for Anesthesiology and Intensive Care Medicine (DGAI), intravenous fat infusion (lipid emulsion, lipid rescue ) should also be used at an early stage in the event of local anesthetic toxicity, in addition to safeguarding vital functions according to the current resuscitation guidelines . Animal experiments and clinical case studies in humans have shown a higher survival rate when treatment with fat infusion is used. It is assumed that the administered fat partially binds the (lipophilic) local anesthetic in the blood and / or reduces the harmful effect of the local anesthetic on the heart. Usual 20% fat emulsions are used, as they are also used in intensive care units for intravenous nutrition. However, the use of these fat infusions for local anesthetic toxicity is a so-called off-label use outside of the intended uses approved by the manufacturer. The therapy recommended by the DGAI can be found in the table:
| Procedure for local anesthetic intoxication. |
|---|
| 1. Stop the supply of local anesthetic |
| 2. Adequate oxygenation, if necessary ventilation |
| 3. Cardiopulmonary resuscitation in the event of cardiac arrest |
| 4. IV administration of lipid emulsion (bolus 1.5 ml / kg; infusion 0.1 ml / kg / min over 30 minutes or 0.5 ml / kg / min over 10 minutes) |
| 5. Anticonvulsants for seizures |
The experience of treatment with fat emulsion can be reported on CIRS.
Adverse effects when used externally
In principle, most of the side effects that occur when local anesthetics are injected are also conceivable with local application, but they are much less common, as less active ingredient gets into the bloodstream. Problems can arise with larger or deeper lesions as well as with extensive or frequent use (topical local anesthetics must not be applied to open wounds). Local allergic (seldom systemic) reactions partly against the active ingredient itself, partly against the carrier substance are likely to be the most common.
Active ingredients
| substance | structure | Application type | Onset of action | PK s | Duration of action | Protein binding | introduction |
|---|---|---|---|---|---|---|---|
| Aminoamides | |||||||
| Lidocaine | 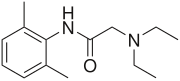 |
Injection, topical |
fast | 7.9 | 60-120 min | 65% | 1943 |
| Mepivacaine |  |
injection | fast | 7.6 | 90-180 min | 75% | 1957 |
| Prilocaine | 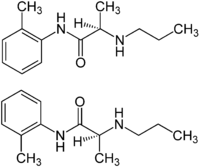 |
Injection, topical |
fast | 7.7 | 60-120 min | 55% | 1960 |
|
Articain (until 1984 Carticain) |
 |
injection | fast | 7.8 | 0.5-5 h | 95% | 1970 |
| Bupivacaine |  |
injection | slowly | 8.1 | 4-5 h | 95% | 1963 |
| Ropivacaine |  |
injection | slowly | 8.1 | 4-6 h | 94% | 1996 |
| Cinchocaine (= dibucaine ) |
 |
topical | slowly | 1.5-2 h | 1930 | ||
| Etidocaine # |  |
injection | fast | 7.7 | 4-6 h | 95% | 1972 |
| Amino ester | |||||||
| Procaine |  |
injection | slowly | 8.9 | 45-60 min | 5% | 1905 |
| Benzocaine | 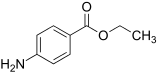 |
topical | fast | 3.5 | 30-60 min | 6% | 1900 |
| Chloroprocaine or chloroprocaine |  |
injection | fast | 9.1 | 30-45 min | 1952 | |
| Oxybuprocaine |  |
topical | |||||
| Tetracaine |  |
topical | slowly | 8.6 | 60-180 min | 80% | 1931 |
| Proxymethacaine |  |
topical | |||||
| Fomocaine | |||||||
| Fomocaine # |  |
topical | |||||
| other | |||||||
| Quinisocaine |  |
topical | 1952 | ||||
| Dyclonin # |  |
topical | |||||
| Lauromacrogol 400 (Polidocanol) |
Structure example |
topical | |||||
|
# No preparations approved in Germany (Rote Liste Online, October 2018). Credentials: |
|||||||
literature
- Christoph Klaus Müller, Local Anesthesia. What are the risks from a general medical perspective? , Zahnärzteblatt Baden-Württemberg, 03/2011 edition. Retrieved March 9, 2015.
- Leonard S. Jacob: Intensive Course: Pharmacology . Urban & Schwarzenberg, Munich / Vienna / Baltimore 1995, ISBN 3-541-12831-3 .
- HA McLure, AP Rubin: Review of local anesthetic agents. In: Minerva Anestesiol. 2005 Mar; 71 (3), pp. 59-74. Review. PMID 15714182 ( PDF, 113 kB )
- W. Zink, BM Graf: Toxicology of local anesthetics. Pathomechanisms - Clinic - Therapy. In: Anaesthesiologist. 2003 Dec; 52 (12), pp. 1102-1123. Review. PMID 14691623 ( PDF, 462 kB )
Web links
Individual evidence
- ↑ a b Hans-Anton Adams: Colloids and resorption of local anesthesia solutions: “In vitro” and animal experimental findings as well as clinical results in test subjects and patients . Volume 213 of Anaesthesiology and Intensive Care Medicine Anesthesiology and Intensive Care Medicine . Springer-Verlag, 2013, ISBN 9783642754807 , p. 1.
- ↑ Ulf Glade: History of anesthesia. ( Memento from May 25, 2012 in the Internet Archive ) at: www-user.uni-bremen.de
- ↑ Raymond S. Sinatra, Jonathan S. Jahr, J. Michael Watkins-Pitchford: The Essence of Analgesia and Analgesics - Sinatra / year / Watkins-Pitc . ISBN 1-139-49198-9 , pp. 280 .
- ↑ Michael Heck, Michael Fresenius: Repetitorium Anaesthesiologie. Preparation for the anesthesiological specialist examination and the European diploma in anesthesiology. 3rd, completely revised edition. Springer, Berlin / Heidelberg / New York et al. 2001, ISBN 3-540-67331-8 , p. 803.
- ↑ Adrenalin for acra, nose, ear and penis , Deutsches Ärzteblatt, vol. 114, issue 47, November 24, 2017. Accessed on July 14, 2019.
- ↑ Frank Mattes, Adrenaline in Digital Blocks Leads to Necrosis. Myth or Truth? , Society for Foot Surgery, 2003. Retrieved July 14, 2019.
- ↑ Engelhardt P., Anesthesia in foot surgery . In: Orthopedic foot surgery. Steinkopff, Heidelberg, 2001, ISBN 978-3-642-47745-4 , pp. 9-12
- ↑ Andreas Gohritz, Is hand surgery under local anesthesia with adrenaline additive ("wide awake") reliable and safe? - Systematic literature review and own experiences with 163 patients , German Society for Hand Surgery. 57th Congress of the German Society for Hand Surgery, September 20, 201. Accessed July 14, 2019.
- ↑ Pharmaceutical Course Book 2007/09. Arzneimittel-Verlags-GmbH Berlin 2007.
- ^ Pharmaceutical course book, p. 728.
- ^ PH Tonner: Pharmacotherapy in anesthesia and intensive care medicine . Springer, Berlin 2011, ISBN 978-3-540-79155-3 .
- ↑ DGAInfo: T. Volk, BM Graf, W. Gogarten, P. Kessler, H. Wulf: Recommendations for the treatment of lipids in intoxication with local anesthetics, Recommendations for the treatment of local anesthetic toxicity with lipids. ( Memento of the original from April 2, 2015 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. In: Anästh Intensivmed. 2009; 50, pp. 698-702.
- ↑ cirs-ains.de CIRS
- ↑ lipid rescue .
- ↑ S. Schulz-Stübner: Local anesthetics. In: Rolf Rossaint, Christian Werner, Bernhard Zwißler (eds.): The anesthesiology. General and special anesthesiology, pain therapy and intensive care medicine. 2nd Edition. Springer, Berlin 2008, ISBN 978-3-540-76301-7 .
- ↑ H. Niesel, H. Van Aken: local anesthesia, regional anesthesia, regional pain therapy. Georg Thieme Verlag, 2006, ISBN 3-13-143412-0 .
- ↑ A. Dullenkopf, A. Borgeat: Local anesthetics. In: Anaesthesiologist. 2003 Apr; 52 (4), pp. 329-340. PMID 12715136
- ↑ Red List Online (October 2018), Wikipedia (for substances not listed there)
