Examination of the thyroid
The examination of the thyroid gland in humans includes various medical examination methods of the thyroid gland depending on the occasion and the question as well as the specialist discipline ( general practitioner , general internist , endocrinologist , radiologist or nuclear medicine specialist ) .
In the specific anamnesis , typical complaints are recorded and previous illnesses related to the thyroid gland and medication intake are queried. In the physical examination, on the one hand, the neck is palpated ( palpation ), on the other hand, general physical signs of thyroid diseases are to be recognized. The most important and usually the first imaging procedure is thyroid sonography . With it many structural changes of the organ can be recorded. It is possible that completes thyroid scintigraphy imaging with its pictorial representation of regional thyroid function. The most important laboratory parameter for determining thyroid dysfunction is thyrotropin (TSH). A normal TSH level largely rules out significant thyroid dysfunction. The thyroid hormones fT 3 and fT 4 must be determined in order to diagnose an overactive thyroid ( hyperthyroidism ) or underactive thyroid ( hypothyroidism ). The determination of thyroid autoantibodies and tumor markers is only necessary for certain diseases. Some further examinations can contribute to the diagnosis in special cases .
anamnese
At the beginning of the thyroid examination there is a specific anamnesis .
On the one hand, the complaints that are in the foreground for the patient are recorded. However, specific questions are also asked about complaints that speak for an enlarged thyroid gland ( goiter ) (feeling of pressure in the neck area, feeling of lump and foreign body ( globus syndrome ), swallowing disorders, aversion to tight collars, shortness of breath ). Typical symptoms of over- or under-function are queried: for example, nervousness, palpitations , unwanted weight loss, heat intolerance, increased sweating and diarrhea speak in favor of over-function ; Dry skin, tiredness, reduced performance, cold intolerance, unwanted weight gain, constipation , a rough and hoarse voice and depression all speak of hypofunction . Sudden swelling associated with physical activity may indicate a bleeding cyst of the thyroid gland. Unilateral thyroid pain radiating to the ear on the same side occurs in de Quervain's subacute thyroiditis . Nodules with a tendency to grow can be an indication of thyroid cancer . Patients with Graves' disease are asked about symptoms of endocrine orbitopathy : feeling of pressure behind the eyes and headache , sensitivity to light, sensation of foreign bodies, tears in the eyes, double vision.
You are usually asked about previous thyroid diseases and treatments ( anti- thyroid drugs , thyroid surgery, radioiodine therapy ). Any previous radiation therapy of the neck region should be inquired about, as it is associated with an increased risk of a malignancy of the thyroid gland on the one hand and the development of hypothyroidism on the other . Information on thyroid diseases that occur in families (goiter, autoimmune thyroiditis , medullary thyroid carcinoma) can give the doctor important information about the patient's current disease.
The use of certain medications is important for further diagnosis. Medicines containing iodine ( e.g. amiodarone ) and contrast media reduce the absorption of tracers in the scintigram. Oral contraceptives and other estrogen preparations change the plasma protein binding of the thyroid hormones triiodothyronine and thyroxine . The same applies to an existing pregnancy . In addition, thyroid scintigraphy with radioactive tracers is prohibited during pregnancy . The use of anticoagulants can speak against performing a puncture.
Physical examination
Thyroid diseases can often be identified with a physical examination . A pronounced goiter or an upper accumulation of influence are usually visible ( inspection ). Scars in the neck area can be the reason to supplement the anamnesis regarding previous operations. In Graves' disease , look out for signs of endocrine orbitopathy : exophthalmos , redness and swelling of the eyelids and conjunctiva.
The thyroid can be examined by palpation . For this purpose, the patient's neck is scanned from the front or the back with both hands, usually while sitting. In addition to the size of both thyroid lobes and the isthmus (the tissue bridge between the two lobes), their respective properties are also of interest. A hard thyroid is found in Riedel's goiter and in malignantly changed organs. Tenderness suggests subacute granulomatous thyroiditis or an abscess . The size and position of thyroid nodules should be recorded. The lack of mobility of the thyroid gland or thyroid nodules when swallowing indicates malignant changes. On palpation of the remaining cervical soft tissues, enlarged cervical lymph nodes can again be an indication of a malignancy or an inflammation of the thyroid gland.
The World Health Organization (WHO) differentiates the following goiter grades according to size, each of which is cited with minimal differences:
| Classifications of the degrees of goiter | |||
| according to Hotze and Schumm-Dräger | according to AWMF guidelines | ||
| Grade 0a | No goiter | Stage 0 | No goiter |
| Grade 0b | Palpable but invisible goiter | Stage 1a | Palpatory but invisible enlargement |
| Grade I. | Palpable goiter, just visible when the head is bent back | Stage 1b | Visible enlargement at maximum neck reclination |
| Grade II | Visible goiter | Stage 2 | Thyroid visible with normal head position |
| Grade III | Large visible goiter | Stage 3 | Heavily enlarged thyroid |
The classification of a patient in this grade depends on the one hand on subjective factors of the examiner, on the other hand on the nutritional status of the patient and the development of the neck muscles. It can therefore only be used as an orientation description of the finding, not to give the exact size of the thyroid gland.
The rest of the general physical exam may indicate an over- or underactive thyroid. The following speak in favor of hyperthyroidism: high pulse ( tachycardia ), increased difference between systolic and diastolic blood pressure , warm and moist skin, subtle tremors and accelerated muscle reflexes . Symptoms of hypothyroidism are general slowing of the patient, dry, rough and pale skin, hoarse voice and lumpy speech, swelling of the eyelids and hands, low pulse ( bradycardia ), slow muscle reflexes and signs of myopathy .
Imaging procedures

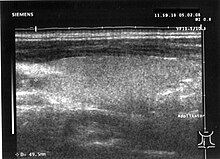
1 right common carotid artery , 2 right thyroid lobes, 3 trachea , 4 left thyroid lobes, 5 left common carotid artery , 6 left internal jugular vein , 7 isthmus (tissue bridge between right and left thyroid lobes)
Imaging methods are part of in vivo diagnostics because they take place in the living organism .
Sonography
In the diagnostic imaging which is first ultrasound used. The use of real-time devices is recommended for the thyroid . The transmission frequency of the transducer should not fall below a center frequency of 7.5 MHz ; Sound heads with a higher transmission frequency of up to 13.5 MHz offer better detail resolution, especially in structures near the surface. New devices sometimes offer higher transmission frequencies of up to 17 MHz (as of 2010). In the majority of cases of enlarged thyroid glands, an image width of about 6 cm allows the total diameter to be determined; Linear transducers with a larger image width can complicate the examination in patients with short necks.
Lateral to the thyroid gland, the common carotid artery (round, pulsating and hardly compressible) and the internal jugular vein (sickle-shaped, easily compressible) can be seen. The esophagus can be demarcated to the left behind the thyroid . Further orientation structures are the sternocleidomastoid muscle on the right and left and the leading edge of the vertebral bodies of the cervical spine.
With sonography, the expansion of the thyroid gland can be measured in the three spatial axes and the volume calculated from this ( ellipsoid : length times height times width times 4/3 times pi divided by 8; the volume (in ml) is approximately length times height times width (each in cm) divided by 2). The thyroid gland has a normal volume of around 6 to 18 ml in women and around 9 to 25 ml in men. An enlarged thyroid is known as a goiter . In Graves' disease , the organ is usually enlarged, in Hashimoto's thyroiditis in the hypertrophic form it is normal or enlarged, in the atrophic form (Ord thyroiditis) it is reduced in size. A basal goiter of the tongue as well as a median cervical cyst , which may contain scattered thyroid tissue, can often be shown. A (retrosternal) goiter located partially behind the breastbone can often be at least partially assessed in terms of its size. The measurement deviation of the thyroid volume is between 10 and 30%. The larger the thyroid, the less precisely the measurement result can be reproduced .
Deviations in the basic sonographic pattern can be found in autoimmune diseases of the thyroid gland; the organ often appears inhomogeneous or hypoechoic . Focal findings (lumps, cysts ) are described in terms of their size, position and type of border. Autonomic adenomas often have a hypoechoic rim. An inhomogeneously hypoechoic and indistinctly demarcated node is suspicious of the presence of thyroid carcinoma ; additional calcifications in this node can be an indication of medullary thyroid carcinoma. Cysts are anechoic and show an (apparent) amplification of sound on the side facing away from the transducer.
Color-coded Doppler sonography provides additional information about the type of thyroid disease. Diffuse increased blood flow can be found in Graves' disease, often also in Hashimoto's thyroiditis. The hypoechoic rim of the autonomic adenoma corresponds to increased blood flow at the edge in the Doppler sonogram. A differentiation between benign and malignant nodes cannot be made with certainty even with this method; the same applies to scintigraphy.
A new, promising method is elastography , with which the compressibility of thyroid nodules can be assessed. A more solid structure comes with an increased risk of malignancy. The significance of this method has not yet been conclusively assessed.
The 3D ultrasound does not play a role in thyroid diagnostics .
Scintigraphy

The thyroid scintigraphy allows the assessment of regional and global function of the thyroid gland.
Scintigraphy with technetium
The most commonly used tracer is 99m Tc (sodium pertechnetate, Na 99m TcO 4 ). It is available in all nuclear medicine practices and has favorable physical properties in terms of radiation type (pure gamma emitter ), radiation energy (140 keV ) and half-life (6 hours). The tracer is absorbed into the thyroid ("iodination") in the same way as iodine , but not incorporated into thyroid hormones ("iodination"). The uptake of technetium in the thyroid gland ( uptake ) is proportional to the uptake of iodide . The radiation dose for the thyroid in the thyroid scintigram is about 0.12 cGy , the effective equivalent dose for the whole body with an activity of 75 MBq is about 0.9 mSv . Technetium is also absorbed into the salivary glands and stomach lining.
The 99m Tc uptake is normally about 0.5 to 2% of the intravenously administered technetium. A globally increased uptake can be found in iodine deficiency , under therapy with anti-thyroid drugs and in Graves' disease ; a regionally increased uptake in autonomic adenomas . A globally reduced uptake can be demonstrated after exposure to iodine (for example contrast media or amiodarone ), with the intake of sodium perchlorate or thyroid hormones, as well as with autoimmune thyroiditis , thyroiditis de Quervain and with secondary hypothyroidism . A regionally reduced uptake is found in de Quervain's thyroiditis and in cold nodules .
Suppression scintigraphy Scintigraphy under suppression can be used
to demonstrate thyroid autonomy , which can not be detected by scintigraphy in a normal metabolic situation. For this purpose, the patient temporarily takes thyroid hormones according to a prescribed scheme , which lead to a reduction in the TSH value ("suppression") via the thyrotropic control circuit . In the scintigram under suppression conditions, non-autonomous thyroid tissue does not absorb any tracer , so that autonomous areas are better demarcated. A total Tc uptake of more than 3% in the thyroid under suppressive conditions indicates a high risk of developing hyperthyroidism after exposure to iodine.
- Scintigraphy with iodine
Scintigraphy with 131 I is reserved for follow-up care for differentiated thyroid carcinoma and the preliminary examination before radioiodine therapy ( radioiodine test ) due to unfavorable physical properties in terms of radiation type (predominantly beta emitters ), radiation energy (364 keV) and half-life (around 8 days) . 123 I (pure gamma emitter, radiation energy 159 keV, half-life 13 hours) would be the ideal nuclide for thyroid scintigraphy, since, in contrast to technetium, it is also subject to iodization. However, it has to be manufactured in a cyclotron in a more complex manner than with technetium generators and is too expensive for routine diagnostics. It is used primarily in the diagnosis of dystopic goiter (base of the tongue, mediastinal goiter, ovarian goiter ) and the missing thyroid gland ( athyroidism ).
Scintigraphy with MIBI
If the thyroid gland is cold, a thyroid scintigram can also be made with methoxy-isobutyl-isonitrile (MIBI). If the lump shows increased accumulation, there is an urgent suspicion of thyroid carcinoma. If thyroid cancer is known, a whole-body scintigram with MIBI can find metastases that have lost the ability to store iodine.
Other imaging tests
In the chest X-ray an enlarged thyroid can be noticed. The X-ray target image of the trachea and esophagus (possibly with contrast agent ) are largely displaced by the ultrasound. For certain questions - especially intra- thoracic goiter and follow-up care for thyroid cancer - other imaging methods are also used: computed tomography (CT) and magnetic resonance imaging (MRT), for thyroid cancer skeletal scintigraphy and positron emission tomography (PET) . If a malignancy of the thyroid gland is suspected, iodine-containing contrast media must not be used.
In endocrine orbitopathy , the structures of the orbit can be assessed using ultrasound or computed tomography; However, the method of first choice is magnetic resonance imaging .
Laboratory values
The laboratory tests are also known as in vitro diagnostics , as they take place outside of a living organism . On the other hand, the laboratory tests allow the thyroid function to be determined in addition to the scintigraphy .
TSH
The most important parameter for assessing thyroid function is thyrotropin (or thyroid-stimulating hormone, TSH). A normal TSH value (normal range, depending on the laboratory, mostly between 0.4 and 4.0 mU / l) largely rules out a major functional disorder of the thyroid. The upper value of the TSH normal range increases steadily with age in adults, namely - according to an analysis of an extensive data collection in the USA - between the age groups 20–29 and 80+ from 3.5 to 7.5 mU / l.
The TSH test plays a special role in the early detection of congenital hypothyroidism in the context of newborn screening . Modern TSH tests have a lower limit of detection in the range from 0.005 to 0.01 mU / l. The TRH test for the detection of latent functional disorders has thus become obsolete in the majority of cases, the test is only used occasionally in the case of borderline low or high TSH values and the clinical situation is unclear; it can also be used in non-thyroidal illness , a change the thyroid hormone values without their own disease value can be used for severe general illnesses and for certain disorders of the pituitary gland and hypothalamus .
The IGeL monitor of the MDS ( Medical Service of the Central Association of Health Insurance Funds ) rated the test to determine TSH for people without complaints in 2017 as "generally negative". The most important source is a review article from 2015. The scientists did not find any studies on the question of the benefits and harms of a thyroid check for non-pregnant adults without symptoms. Studies on the question of whether treatment for people without symptoms, but with TSH levels outside the norm, shows no benefit from early treatment, for example on quality of life, blood pressure, body mass index, bone density, mental fitness or blood lipid levels. On the other hand, damage is possible, since the drugs have side effects and only a fraction of people with abnormal TSH levels experience symptoms later. Of three high-quality international guidelines, only one recommends screening for people (60 and over) without symptoms.
fT 3 and fT 4 , rT 3
The normal values for thyroid hormones are age-dependent: the levels are higher in children and lower in older people.
In the case of reduced or increased TSH, the determination of the thyroid hormone parameters triiodothyronine (T 3 ) and thyroxine (T 4 ) is necessary in order to detect manifest thyroid dysfunction. Determining T 4 on its own is not sufficient, as isolated T 3 hyperthyroidism could be overlooked. Since the thyroid hormones in the serum are largely bound to proteins , but only the non-bound portion is biologically effective, the free hormones fT 3 and fT 4 are usually determined. If a test for fT 4 is not available, it is recommended that thyroxine-binding globulin (TBG) also be determined in order to be able to assess protein binding.
In the case of non-thyroidal illness, the fT 3 level is reduced , while the structurally isomeric , but biologically inactive rT 3 (reverse T 3 ) is increased. This parameter is not part of routine diagnostics.
| Functional situation / illness | TSH | T 3 | T 4 | annotation |
|---|---|---|---|---|
| manifest hyperthyroidism | mostly <0.1 mU / l | n or ↑ | n or ↑ | T 3 and / or T 4 ↑ |
| latent hyperthyroidism | ↓ | n | n | |
| Euthyroidism | n | n | n | |
| latent hypothyroidism | ↑ | n | n | |
| manifest hypothyroidism | mostly> 10 mU / l | n or ↓ | n or ↓ | T 3 and / or T 4 ↓ |
| secondary hypothyroidism mostly pituitary insufficiency |
n or ↓ | ↓ | ↓ | Rare |
| secondary hyperthyroidism mostly TSH-producing pituitary adenoma |
n or ↑ | ↑ | ↑ | Rare |
| peripheral thyroid hormone resistance | different constellations | Rare | ||
| pronounced iodine deficiency | n | ↑ | ↓ | no thyrostatic treatment |
| n: normal - ↑: increased - ↓: decreased | ||||
Additional thyroid function tests may be required for specific questions .
Autoantibodies
For certain autoimmune diseases of the thyroid gland, the determination of the thyroid autoantibodies can be useful: elevated antibodies against the TSH receptor ( TRAK ) are evidence of Graves disease, but negative antibodies do not rule it out with certainty. High TRAK values in patients with Graves' disease in remission indicate that there is a high probability of a relapse . Antibodies against thyroid peroxidase ( TPO-AK ) are found in around 90% of patients with Hashimoto's thyroiditis and still in around 70% of patients with Graves' disease, but also in around 20% of patients with non-immunogenic thyroid diseases. Every year around 5% of TPO-AK positive people with initially normal thyroid function develop hypothyroidism. The detection of antibodies against thyroglobulin ( Tg-AK ) can confirm the diagnosis of autoimmune thyroiditis in those patients who are TPO-AK negative.
Tumor markers
Thyroglobulin
Thyroglobulin (Tg) serves as a tumor marker in the follow-up of differentiated thyroid carcinoma (more precisely: papillary or follicular thyroid carcinoma) after thyroidectomy and, if necessary, radioiodine therapy . Modern tests achieve a sensitivity of 0.2 ng / ml. If the thyroid gland is still present, high Tg levels can be detected without a tumor being present. In the presence of thyroglobulin antibodies (Tg-AK) the measured value can be determined as false-low; In order to detect such interfering influences, it is customary to also carry out a so-called recovery test: a defined amount of Tg is added to the sample after the measurement; if the new measurement corresponds to the first result plus the addition, a recovery of 100% ("correct recovery": 70 - 130%) is available. In the absence of a thyroid gland (athyroidism), Tg cannot be detected, in hyperthyroidism it is usually at least reduced. The sensitivity of the Tg is improved with increased TSH . In order to achieve a sufficiently high TSH, the patient has to pause his medication with thyroid hormones for a few weeks, which, however, creates a deep hypothyroidism with all negative effects for the patient. Alternatively, recombinant TSH (rTSH) is given intramuscularly , which in turn is associated with considerable costs.
Calcitonin and pentagastrin test
Calcitonin is used as a tumor marker in follow-up care and follow-up monitoring of medullary thyroid carcinoma. Slightly elevated values are rarely found in small cell lung cancer , carcinoid , breast or stomach cancer . However, only medullary thyroid carcinoma shows an increase in calcitonin in the pentagastrin test . The determination of calcitonin and pentagastrin tests are of particular importance in family examinations of relatives of patients with multiple endocrine neoplasia type MEN 2.
CEA
The carcinoembryonic antigen (CEA) is positive in three quarters of patients with medullary thyroid cancer. In advanced disease or very aggressive tumor growth, the calcitonin level does not rise sufficiently. Here the increase in CEA can indicate a progression of the tumor disease.
Genetic test
A genetic test is available for the familial form of medullary thyroid carcinoma , with which mutations in the RET proto-oncogene can be detected. Detection of mutations is associated with an almost one hundred percent probability of developing medullary thyroid cancer in the course of life.
The test is indicated in patients with proven medullary thyroid carcinoma, bilateral pheochromocytoma and in the presence of multiple endocrine neoplasia of type IIa and IIb. The genetic test is also indicated as a screening method for all family members of patients with a proven mutation in the RET proto-oncogene. These people can have a preventive thyroidectomy.
Determination of iodine in urine
In hyperthyroid patients whose disease is particularly severe (e.g. thyrotoxic crisis ) or can not be brought under control with normal doses of thyrostatic treatment , a determination of the iodine content in the urine can provide information about whether an exposure was possibly the cause with iodine - for example through iodine-containing contrast media or amiodarone - is present (iodine contamination). In children with congenital hypofunction, the cause could be severe iodine deficiency . Patients with thyroid carcinoma in particular, but also those with benign thyroid disease, should avoid iodine before therapy or diagnosis with radioiodine (iodine abstinence ).
In iodine-deficient areas, the iodine content in the urine is mostly below 100 µg / l or below 100 µg / g creatinine . With values above 300 µg / l or above 300 µg / g creatinine, there is a suspicion of iodine contamination.
Other investigations
- Fine needle puncture
- A mostly ultrasound-controlled fine needle puncture of the thyroid gland is used to obtain samples for a cytopathological examination . The most important indication is a lump with suspected malignancy, rarely diagnostic problems when classifying an inflammation of the thyroid gland . Thyroid cysts with mechanical complications are therapeutically relieved by a puncture. The puncture is contraindicated in the case of a known hemorrhagic diathesis or the use of anticoagulants .
- ENT medical examination
- If an operation is planned, you will usually see an ear, nose and throat doctor in order to rule out existing disorders of vocal cord mobility or paralysis of the vocal cord nerves ( recurrent palsy ).
- Perchlorate Depletion Test
- The perchlorate depletion test is a method for detecting Pendred syndrome , a rare sensorineural hearing loss, and other disorders of iodine utilization.
literature
- FA Verburg, T. Krohn: Thyroid diagnosis in good clinical practice . In: The nuclear medicine. Volume 35, 2012, pp. 12-21 doi: 10.1055 / s-0031-1301349 .
- Lothar-Andreas Hotze, Petra-Maria Schumm-Draeger: Thyroid diseases. Diagnosis and therapy. Berlin 2003, ISBN 3-88040-002-4 .
- Torsten Kuwert: Thyroid. In: Torsten Kuwert, Frank Grünwald , Uwe Haberkorn, Thomas Krause: Nuclear Medicine. Stuttgart / New York 2008, ISBN 978-3-13-118504-4 .
- Thyroid. In: Gerd Herold : Internal Medicine. Cologne 2005.
Web links
- Thyroid diagnostics at laborlexikon.de
- Thyroid diagnostics. ( Memento from June 6, 2008 in the Internet Archive ) Guideline of the German Society for Nuclear Medicine
- Practice Guideline for the Performance of a Thyroid and Parathyroid Ultrasound Examinations. (PDF; 351 kB) Guidelines of the American College of Radiology (English, status 2007)
Individual evidence
- ^ Klaus Holldack, Klaus Gahl: Auscultation and percussion. Inspection and palpation. Thieme, Stuttgart 1955; 10th, revised edition ibid 1986, ISBN 3-13-352410-0 , p. 47 f.
- ^ Lothar-Andreas Hotze, Petra-Maria Schumm-Draeger. Thyroid diseases. Diagnosis and therapy. Berlin 2003 ISBN 3-88040-002-4 , p. 152
- ↑ Outdated guidelines of the German Society for Pediatric Surgery: Struma ( Memento from March 31, 2008 in the Internet Archive )
- ↑ Chr. Reiners, J. Rendl. Thyroid. in: U. Büll et al. (Ed.) Nuclear Medicine. Stuttgart, New York 2001, ISBN 3-13-128123-5 , p. 149
- ^ Thyroid Function Tests . British Thyroid Foundation; accessed on May 20, 2019.
- ↑ MI Surks, JG Hollowell: Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: implications for the prevalence of subclinical hypothyroidism. In: The Journal of clinical endocrinology and metabolism. Volume 92, number 12, December 2007, pp. 4575-4582, doi: 10.1210 / jc.2007-1499 , PMID 17911171 (free full text).
- ↑ N. Aggarwal, S. Razvi: Thyroid and aging or the aging thyroid? An evidence-based analysis of the literature. In: Journal of thyroid research. Volume 2013, 2013, p. 481287, doi: 10.1155 / 2013/481287 , PMID 24106641 , PMC 3782841 (free full text) (review).
- ↑ JV Hennessey, R. Espaillat: Diagnosis and Management of Subclinical Hypothyroidism in Elderly Adults: A Review of the Literature. In: Journal of the American Geriatrics Society. Volume 63, number 8, August 2015, pp. 1663–1673, doi: 10.1111 / jgs.13532 , PMID 26200184 (review) ( free full text: PDF ).
- ↑ TSH determination for the thyroid check . IGeL monitor; accessed on March 15, 2019. More on the assessment: Evidence in detail . (PDF) accessed on March 15, 2019.
- ↑ JB Rugge, C. Bougatsos, R. Chou: screening and treatment of thyroid dysfunction: an evidence review for the US Preventive Services Task Force. In: Annals of internal medicine. Volume 162, Number 1, January 2015, pp. 35-45, doi: 10.7326 / M14-1456 , PMID 25347444 (review).
- ↑ Doctors newspaper online: Thyroid function. MDK leaves no good hair on the TSH test . May 5, 2017, as well as Deutsches Ärzteblatt: Thyroid test: IGeL-Monitor evaluates self-pay performance as “generally negative” . May 8, 2017.
- ^ ML Lefevre: Screening for thyroid dysfunction: US Preventive Services Task Force recommendation statement . In: Ann Intern Med , 2015; 162 (9), pp. 641-650, PMID 25798805 . JR Garber et al .: Clinical practice guidelines for hypothyroidism in adults . (PDF): cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. In: Thyroid , 2012; 22 (12), pp. 1200-1235. G. Brenta et al .: Clinical practice guidelines for the management of hypothyroidism . In: Arq Bras Endocrinol Metabol , 2013; 57 (4), pp. 265-291, PMID 23828433 .
- ↑ Gerd Herold . Internal Medicine. Cologne 2005, p. 640
- ^ Karl Jürgen Schmidt. Thyroid tumors. In: Wieland Meng. Thyroid disease. Gustav Fischer Verlag Jena, Stuttgart 1992, ISBN 3-334-60392-X , p. 307
- ^ R. Hörmann: Thyroid diseases . ABW-Wissenschaftsverlag, 4th edition 2005, page 128ff. ISBN 3-936072-27-2
- ↑ K. Hahn, S. Fischer. The 123 iodine depletion test for diagnosing Pendred syndrome in children. Nuclear Medicine 2009; 32: 17-18. doi: 10.1055 / s-0028-1119389