Eye muscles
In the eye muscles , a distinction according to their location and function of the inner of the outer muscles of the eye, including the further also the eyelid lifting muscle and that of the nictitating membrane of some vertebrates include.
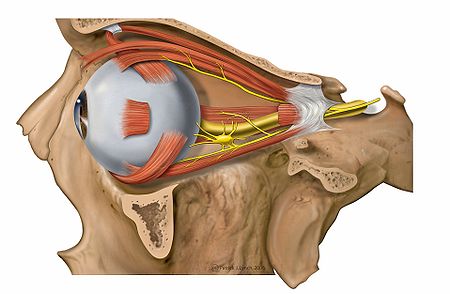
Outer eye muscles, including eyelid lifters and nictitating membrane muscles, belong to the skeletal muscles as striated muscles and belong to the appendix organs of the eye . The external eye muscles that attach directly to the eyeball have their origin in the rear area of the orbit on a common tendon ring , with the exception of the oblique lower muscle originating on the nasal wall of the eye socket. They are embedded in the body of an adipose tissue, which is stored in the eye with connective tissue and allows the shifts necessary for movements.
Inner eye muscles, on the other hand, are ring-shaped trains of smooth muscles of the iris and the ciliary body within the eyeball. The pupil width is adjusted with the iris muscles, while the ciliary muscle changes the curvature of the lens to adjust the distance .
The outer eye muscles perform eye movements of both eyeballs in the form of movements in the same direction ( conjugated ) or in opposite directions ( disjugated ) (as versions or vergences ). If one considers only the movements of one eye, one speaks of ductions if they occur in a horizontal, vertical or oblique meridian. Rolling movements, on the other hand, are called torsions .
External eye muscles
Development history
Originally, the external eye muscles were not used to target the gaze movements of the eyes, but to immobilize the images on the retina when the head or body moved. It was only with the formation of special retinal areas, such as the fovea centralis and consequently for the fixation of objects, that they were increasingly used for eye movements.
Embryonic development
The outer eye muscles, together with Tenon's capsule (part of the ligamentous apparatus ) and the fatty tissue of the eye socket (orbit), are descendants of the mesenchyme (embryonic connective tissue) surrounding the eye vesicle (early development stage of the eyeball ). From the third embryonic month , the further development is controlled from three growth centers, each of which is assigned a nerve. From this the later nerve supply ( innervation ) of the eye muscles is derived from three cranial nerves . The development of the external eye muscles depends on the normal development of the eye socket, while the development of the ligamentous apparatus is independent of this.
Anatomy and function
In most mammals , the eyeball is moved by seven external eye muscles: two oblique mm. obliqui , four straight mm. recti , as well as the retractor muscle , which is missing in humans. Together with nerves, vessels and connective tissue, they are embedded in a retrobulbar fat body ( corpus adiposum retrobulbare ), which enables the displacements that occur during eye movements . With the exception of the lower oblique eye muscle, which has its origin in the lower front of the eye socket wall on the side of the nose, all other muscles arise in the depths of the eye socket from a common tendon ring, the anulus tendineus communis , which surrounds the optic nerve before it enters the bony canalis opticus . Together with a connecting membrane, these form a cone-shaped muscle cone that widens forward from the tip of the orbit and attaches to the sclera of the eyeball.
The outer eye muscles consist of striated muscles , in which two types of fibers are distinguished, which have a different nerve supply (innervation) with regard to the relative number of nerve endings and their arrangement. Muscle fibers from Fibrillenstrukturtyp (A-fibers, thick muscle fibers) have large end plates and thick nerve and are simply innervated. They are primarily used for fast, phasic eye movements ( fast fibers ). The muscle fibers of the field structure type (B-fibers, thin muscle fibers) are innervated several times by thin nerve fibers and are responsible for the tonic movements ( slow fibers ). Recent ultrastructural investigations allow differentiations between five to six different fiber types, which can be assigned to two groups and which are referred to as the orbital and bulbar fiber layer. This muscle structure therefore distinguishes the eye muscles quite significantly from the other muscles.
In humans, the average width of the straight eye muscles in the middle third is 6-9 mm and the thickness is about 3 mm. The total lengths of the muscles are very different. The pure muscle length is between 30 mm (Mm. Obliqui) and 39 mm (M. Rectus inferior), while the lengths of the tendons differ significantly more. These are 0–2 mm for the M. obliquus inferior and 25–30 mm for the M. obliquus superior.
With a frequency of 1–3 microsaccades (quick glances) per second, the outer eye muscles are the most active muscles in the human body. Together with the ligament apparatus, a system of holding and inhibiting straps, as well as other connective tissue structures ( Lockwood ligament , Tenon's capsule ), they form a functional unit. If you consider the fixation of things and the related sequence of eye movements as a control loop , then they fulfill the function of actuators .
In a complex interplay, the outer eye muscles perform all the rotational movements of the eyes in all directions and ensure that the position of the eyes to one another is in a stable equilibrium. In addition, they align the line of sight , which starts from the fovea centralis as the motor zero point , exactly to the object to be fixed . The forces that act on the eye can be compared with the mechanical operating principle of lever and roller . Muscle origin and insertion , which together determine the direction of pull , together with the fulcrum of the eye, which is approximately 13.5 millimeters behind the vertex of the cornea in a person with normal vision, is the so-called muscle level . Since the pulling direction of a muscle can be different depending on the current viewing direction or position of the eye, the muscle level also changes. Each rotary movement takes place around an axis of rotation that runs perpendicular to the muscle plane through the pivot point of the eye.
The anatomical relationships of the eye sockets and the course of the eye muscles cause them to cling to the eyeball (Bulbus oculi) over a certain distance. This stretch is called the rolling stretch and is defined by the starting point of the muscle on the eye and the so-called tangential point at which the muscle contact with the eyeball ends. The point of tangency and pivot point of the eye form the lever arm through which the attacking forces take effect. When looking straight ahead (primary position), the rolling distances of the individual muscles vary in length and change depending on the direction in which you are looking.
Already in the primary position, the muscles are under tension of 0.05-0.1 N . Experimental muscle strength measurements have shown that the strength of an eye muscle can increase up to 1 N without subjective complaints or symptoms of fatigue occurring. The excursion distances of the human eye, i.e. the possible extent of its movements in all viewing directions with a calm head and body posture, is called the monocular field of vision . Its limits are expressed in degrees, sometimes in millimeters. It is about 45 ° when looking up, about 50 ° when looking to the right and left and up to 60 ° when looking out. However, these maximum values are hardly needed in daily life, since head and body movements that begin early in normal use make it easier to look at things and so the pronounced, pure turning of the eyes is not necessary.
Innervation
The external eye muscles are supplied by three cranial nerves : the III. ( Nervus oculomotorius ), the IV. ( Nervus trochlearis ) and the VI. Cranial nerve ( abducens nerve ). They are subject to constant innervation, which never completely paralyzes even during sleep. Each eye muscle is innervated by around 1000 so-called motor neurons. They branch out in the muscle and supply between 4 and 40 muscle fibers , which are known as the motor unit . The pulling force of a muscle is now increased by activating either motor units that were previously inactive or those that were active but not yet fully utilized. First, low-threshold motor units are switched on continuously, and the higher-threshold units as the eye turns in the direction of muscle pull. The frequency of the electrical discharges that the motor neurons conduct into the motor units reaches up to 300 discharges per second.
For each eye position, there is a certain innervation pattern on all six outer eye muscles, which the brain uses over and over again, regardless of how the eye got into this position. It doesn't matter what type of movement the eye turned there. Contrary to the earlier view that different motor neurons are responsible for versions and vergences, the same motor units are always activated, which, according to the principle of the common end section , always discharge at the same frequency.
| Cranial nerve | muscle |
|---|---|
| Oculomotor nerve ( N. III ) | Superior rectus muscle
Inferior rectus muscle Medial rectus muscle Inferior obliquus muscle Retractor bulbi muscle |
| Levator palpebrae superioris muscle | |
| Trochlear nerve ( IV nerve ) | Superior oblique muscle |
| Abducens nerve ( VI ) | Lateral rectus muscle
Retractor bulbi muscle |
The movements of the eyes are finally carried out by a reciprocal change in the innervation. For example, Sherrington's law states that the innervation of an antagonist decreases as that of the agonist increases. The fact that this also applies equally to the contralateral synergists and antagonists of the other eye, says Hering's law of the same side innervation .
Coordinated, binocular eye movements such as vergences or versions are controlled by a supranuclear system in the midbrain to which various neuronal structures belong.
Superior rectus muscle
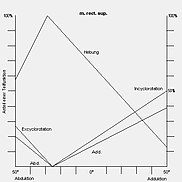
The rectus superior muscle ("upper straight muscle", referred to in animals as the rectus dorsalis muscle and formerly called the religiosus or admirator muscle - "the admirer") arises from the upper circumference of the anulus tendineus communis under the levator palpebrae muscle and lies the eyeball on top. It starts at the eyeball in an oblique line that is slightly curved towards the edge of the cornea ( limbus ), with the insertion about two thirds lateral (to the side) of the vertical meridian. The slightly outwardly curved (convex) approach means that its lateral edge is further away from the limbus than its medial edge . It is innervated by the oculomotor nerve. Its main function is to elevate the eye in the entire field of vision. With moderate movement to the side ( abduction ) of about 25 °, it is only a lifter. Its inward rolling (incyclorotatory) partial function is highest with maximum movement inwards towards the nose ( adduction ), but decreases more and more towards abduction and changes into an outward rolling (excyclorotatory) partial function with stronger abduction.
Inferior rectus muscle
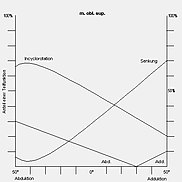
The rectus inferior muscle ("lower straight muscle", referred to in animals as the rectus ventralis muscle and formerly called the capucinorum muscle because it " humbles the eyes") arises from the lower circumference of the anulus tendineus communis and protrudes from the lower surface of the eyeball the equator. As with the superior rectus muscle, its insertion is shifted to the side in relation to the vertical meridian and laterally furthest away from the limbus. It is innervated by the oculomotor nerve. Its main function is to lower (depression) the eyeball in the entire field of vision. With moderate abduction of about 25 °, it is exclusively a sinker. Its outward rolling (excyclorotatory) partial function is greatest in maximum adduction, decreases in the direction of abduction and, with stronger abduction, changes into an inward rolling (incyclorotatory) partial function.
Medial rectus muscle
The musculus rectus medialis ("inner, nasal, straight muscle", formerly called M. bibitorius - "the drunkard") arises at the medial circumference of the annulus tendineus communis , immediately next to the nervus opticus, and runs straight forward near the nasal orbital wall and begins in the anterior half of the eyeball in an almost vertical, straight line to the limbus. This is the strongest eye muscle and moves the eye inwards towards the nose (adduction). It can have a slightly lifting effect (elevation) when looking strongly upwards, and a slightly lowering effect (depression) when looking down, and is innervated by the oculomotor nerve.
Lateral rectus muscle
The muscle rectus lateralis ("lateral straight muscle", formerly called M. indignatorius - "the curmudgeon") arises on the lateral part of the annulus tendineus communis , pulls forward directly next to the periorbita and lies on the side of the eyeball. It moves the eye outwards (abduction) and can have a slightly lifting effect (elevation) when the eye is raised and a lowering effect (depression) when the eye is lowered. It is innervated by the abducens nerve.
Superior oblique muscle
The superior oblique muscle ("upper oblique muscle", referred to in animals as the dorsal oblique muscle and previously called the patheticus muscle ) arises above the medial rectus muscle at the upper, medial edge of the common tendinous annulus . It runs forward in the upper, nasal wall of the eye socket, turns into a tendon after about 30 millimeters, which is then deflected backwards and outwards at an acute angle by a roll cartilage , the trochlea . It passes under the upper straight muscle and attaches to the top-side (dorsolateral) on the upper, outer, rear quadrant of the eyeball. A special feature of the wide-ranging attachment point (insertion) is its close proximity to the upper, outer vortex vein . Special attention should be paid to this fact during surgical interventions in this area, since it can easily lead to vascular injuries. The superior oblique muscle is innervated by the trochlear nerve. Its main function is lowering (depression) with rolling the eye inward (incycloduction) and slight abduction. In adduction, it is almost a pure sinker, while the inward rolling function increases as the eye turns to the outside.
The tendon of the M. obliquus superior must pull in adduction around the nasal attachment of the M. rectus superior as around a pivot point (hypomochlion). The resulting change in the direction of muscle pull leads to a relative increase in its abducting effect and a reduction in the other sub-functions.
Inferior obliquus muscle
The Musculus obliquus inferior ("lower oblique muscle", in animals called Musculus obliquus ventralis and formerly together with the M. obliquus superior also called Mm. Amatorii - "Muscles of lovers" -) originates at the tear bone (os lacrimale), in the lower nasal area of the orbit. It runs outwards under the inferior rectus muscle and attaches to the sclera in the lower, outer, posterior quadrant . It is also innervated by the oculomotor nerve. Since the outer, lower vortex vein leaves the sclera in the immediate vicinity of the muscle attachment, particular caution is required during surgical interventions, as there is an increased risk of injury to the vessel and thus the risk of bleeding. Its main function is to roll the eye outwards (excycloduction) and raise it (elevation) in adduction. Here it also has a low adducting partial function, while in abduction it has a low abducting effect. With a length of only 0 to 2 millimeters, the tendon of the M. obliquus inferior is the shortest of all external eye muscles.
Retractor bulbi muscle
The retractor bulbi muscle ("retraction of the eye") is absent in humans, but is developed in most other mammals. It lies like a cuff around the optic nerve and runs within the muscle cone to the posterior bulbus pole. It has four lobed functional parts that move the eyeball like the individual straight eye muscles and are accordingly innervated by the N. oculomotorius and N. abducens.
Functional schemes
The eye muscles have different, more or less pronounced main and sub-functions depending on the current direction of gaze. These can be represented graphically using so-called track lines. These are the movement components of lifting, lowering, adduction, abduction, inner roll and outer roll.
- Representation of the main and partial functions of the external eye muscles using track lines
|

|

|
|

|
| Superior rectus muscle | M. rectus inferior | M. rectus medialis and M. rectus lateralis |
M. obliquus superior | M. obliquus inferior |
Antagonists and synergists
There are two muscles in each eye that have a similar muscle level and move the eye around an almost identical axis of rotation, but each in an opposite direction of rotation. These muscles are called antagonists . In contrast, muscles that move the eye around a similar axis of rotation in the same direction are called synergists ( see also Innervation ). This terminology is also used when only partial functions of the respective muscles agree or counteract one another. It is only fully applicable for ductions, i.e. movements of one eye. If one extends the consideration to the opposite eye by the description of contralateral synergists and antagonists in the execution of binocular eye movements, then this definition for vergences, opposing eye movements, must be restricted.
Ipsilateral
Equilateral (ipsilateral) synergists and antagonists with regard to the respective muscle function
| Agonist | function | Synergists | Antagonists |
|---|---|---|---|
| M. rect. Medialis | Adduction | Rect. Superior, rect. Inferior | M. rect.lateralis, M. obl. Superior, M. obl. Inferior |
| Lateral rectus muscle | Abduction | M. obl. Superior, M. obl. Inferior | M. rect.medialis, M. rect. Superior, M. rect. Inferior |
| M. rect. Superior | Raising Innenrollung adduction |
M. obl. Inferior M. obl. Superior M. rect. Medialis , M. rect. Inferior |
M. rect. Inferior, M. obl. Superior M. rect. Inferior, M. obl. Inferior M. rect. Lateralis, M. obl. Superior, M. obl. Inferior |
| M. rect. Inferior | Reduction of external curl adduction |
M. obl. Superior M. obl. Inferior M. rect. Medialis , M. rect. Superior |
M. rect. Superior, M. obl. Inferior M. obl. Superior, M. rect. Superior M. rect. Lateralis, M. obl. Superior, M. obl. Inferior |
| M. obl. Superior | Lowering internal curl abduction |
M. rect.inferior M. rect. Superior M. rect. Lateralis, M. obl. Inferior |
M. rect. Superior, M. obl. Inferior M. rect. Inferior, M. obl. Inferior M. rect. Medialis , M. rect. Superior, M. rect. Inferior |
| M. obl. Inferior | Raising Außenrollung abduction |
M. rect. Superior M. rect. Inferior M. rect. Lateralis, M. obl. Superior |
M. rect. Inferior, M. obl. Superior M. obl. Superior, M. rect. Superior M. rect. Medialis, M. rect. Superior, M. rect. Inferior |
- Graphic representation of the involvement of individual muscles (synergists) in the respective rotational movements using the example of the right eye
|
Elevation: Mainly involved are the M. rectus superior and the M. obliquus inferior |
Depression: The main participants are the M. rectus inferior and M. obliquus superior |
Adduction: The main involved is the M. rectus medialis and the vertical Mm. recti |
Abduction: The main involved is the lateral rectus muscle and the Mm. obliqui |
Internal roll: The main participants are the superior obliquus and superior rectus muscles |
External curl: The main participants are the M. obliquus inferior and the M. rectus inferior |
Contralateral
With regard to both eyes movements as versions and vergences the muscles involved have also synergists and antagonists which mitvollführen the movement or antagonize each on opposite eye.
| Eye movement | Agonists | Synergists | Antagonists | |||
|---|---|---|---|---|---|---|
| right eye | left eye | right eye | left eye | right eye | left eye | |
| Dextroversion (right look) |
m. rect. lateralis | m. rect. medialis | m. obl. superior m. obl. inferior |
m. rect. superior m. rect. inferior |
m. rect. medialis | m. rect. lateralis |
| Load preview version (left view) |
m. rect. medialis | m. rect. lateralis | m. rect. superior m. rect. inferior |
m. obl. superior m. obl. inferior |
m. rect. lateralis | m. rect. medialis |
| Supra version (Aufblick) |
m. rect. superior | m. rect. superior | m. obl. inferior | m. obl. inferior | m. rect. inferior | m. rect. inferior |
| Infraversion (perspective) |
m. rect. inferior | m. rect. inferior | m. obl. superior | m. obl. superior | m. rect. superior | m. rect. superior |
| Dextrocycloversion (right roll with head tilted left) |
m. obl. inferior | m. obl. superior | m. rect. inferior | m. rect. superior | m. obl. superior m. rect. superior |
m. obl. inferior m. rect. Inferior |
| Laevozykloversion (left roll with head tilt ) |
m. obl. superior | m. obl. inferior | m. rect. superior | m. rect. inferior | m. obl. inferior m. rect. Inferior |
m. obl. superior m. rect. superior |
| Convergence (movement in the opposite direction with near fixation) |
m. rect. medialis | m. rect. medialis | m. rect. superior m. rect. inferior |
m. rect. superior m. rect. inferior |
m. rect. lateralis | m. rect. lateralis |
Muscle sheaths and intermuscular membrane
All eye muscles have connective tissue sheaths, which, however, are structured differently. In the posterior third, all of the straight eye muscles and the superior oblique muscle have a surrounding tissue made of collagenous, elastic fibers that only form a delicate epimysium (connective tissue sheath). Only in the middle third does a distinct muscular sheath develop ( fascia muscularis ). The M. obliquus inferior alone is wrapped in a dense muscle sheath over its entire length. From the anulus tendineus communis forward, the eye muscles are increasingly connected to one another with connective tissue fibers, the intermuscular membrane (membrana intermuscularis). This separates the retrobulbar fat body located in the muscle funnel (intra-conical) from its extra-conical part. In addition, it ensures that the distance between the eye muscles remains almost unchanged when the eye is moved and that they cannot slide unhindered over the globe.
Dimensions and distances in humans
Today's knowledge of the dimensions of eye muscles, tendons, attachment distances and their different shapes go back to investigations that were partly carried out in the middle of the 19th century. The values vary depending on age.
- Mm. recti: average distance of the tendon irradiation from the limbus in millimeters
| Insertion point |
eye | M. rect. Superior |
M. rect. Inferior |
location | eye | M. rect. Medialis |
Lateral rectus muscle |
|---|---|---|---|---|---|---|---|
| medial | right left |
7.48 ± 0.82 7.72 ± 0.83 |
7.29 ± 0.91 6.76 ± 0.61 |
above | right left |
7.38 ± 1.13 6.76 ± 0.83 |
8.59 ± 0.90 8.72 ± 0.76 |
| center | right left |
7.91 ± 0.88 7.44 ± 0.79 |
6.73 ± 0.63 6.85 ± 0.56 |
center | right left |
5.77 ± 0.69 5.69 ± 0.66 |
7.48 ± 0.78 7.25 ± 0.69 |
| lateral | right left |
10.13 ± 0.91 9.56 ± 0.86 |
8.89 ± 0.64 9.30 ± 0.84 |
below | right left |
6.96 ± 0.76 7.32 ± 1.02 |
8.70 ± 0.76 8.06 ± 0.74 |
- Mm. recti: average size values in millimeters
| eye | M. rect. Superior |
M. rect. Inferior |
M. rect. Medialis |
Lateral rectus muscle |
|
|---|---|---|---|---|---|
| Length * | right left |
37.31 ± 3.72 37.02 ± 3.41 |
36.95 ± 2.45 37.70 ± 3.33 |
37.68 ± 3.39 37.33 ± 2.56 |
36.36 ± 3.69 35.94 ± 4.00 |
| width | right left |
8.59 ± 1.40 7.83 ± 1.03 |
7.96 ± 1.37 7.46 ± 0.92 |
9.41 ± 1.43 9.73 ± 1.24 |
10.87 ± 1.81 10.32 ± 2.23 |
| thickness | right left |
2.23 ± 0.74 2.20 ± 0.89 |
3.87 ± 0.74 3.92 ± 0.52 |
3.80 ± 0.67 3.70 ± 0.65 |
2.87 ± 0.98 2.54 ± 0.76 |
* pure muscle length without tendon
- Mm. recti: average tendon length and width (tendon size) in millimeters
| eye | M. rect. Superior |
M. rect. Inferior |
M. rect. Medialis |
Lateral rectus muscle |
|
|---|---|---|---|---|---|
| length | right left |
4.29 ± 1.09 4.46 ± 1.16 |
4.70 ± 1.23 4.66 ± 1.39 |
3.04 ± 0.96 3.90 ± 1.30 |
7.19 ± 1.94 7.82 ± 1.37 |
| Attachment zone, width |
right left |
10.43 ± 1.39 9.84 ± 1.09 |
8.59 ± 1.26 8.68 ± 0.97 |
10.30 ± 1.35 9.92 ± 1.15 |
9.57 ± 1.32 9.22 ± 1.32 |
- Mm. obliqui: average distance between the tendon irradiation and the limbus in millimeters (radians)
| muscle | eye | front | back |
|---|---|---|---|
| M. obl. Inferior |
right left |
18.38 ± 1.85 18.50 ± 1.74 |
27.02 ± 1.43 27.02 ± 1.86 |
| M. obl. Superior |
right left |
16.33 ± 1.76 15.80 ± 1.53 |
23.21 ± 1.57 22.50 ± 2.18 |
- M. obliquus superior: average size values in millimeters
| Pars longi- tudinalis |
Area | eye | Dimensions | Pars obliqua |
Area | eye | Dimensions |
|---|---|---|---|---|---|---|---|
| Length * | right left |
37.59 ± 3.50 38.54 ± 4.04 |
Length * | right left |
22.12 ± 2.27 22.93 ± 3.11 |
||
| width | Trochlea- region |
right left |
3.38 ± 1.17 3.14 ± 0.80 |
width | Trochlea- region |
right left |
2.12 ± 0.65 2.00 ± 0.47 |
| Central district |
right left |
6.71 ± 0.93 6.50 ± 1.16 |
Tendon irradiation |
right left |
9.85 ± 2.11 9.55 ± 1.72 |
||
Area of origin |
right left |
4.78 ± 1.19 4.75 ± 1.35 |
|||||
| thickness | Central district |
right left |
2.30 ± 0.68 1.94 ± 0.78 |
thickness | Central district |
right left |
1.50 ± 0.49 1.50 ± 0.41 |
* including the tendon up to the trochlea (about 10 mm)
- M. obliquus inferior: average size values in millimeters
| Area | eye | Dimensions | |
|---|---|---|---|
| Length * | right left |
31.46 ± 4.12 30.92 ± 3.15 |
|
| width | Area of origin |
right left |
3.81 ± 1.10 3.65 ± 0.91 |
| Central district |
right left |
7.50 ± 0.86 7.13 ± 0.71 |
|
| Tendon irradiation |
right left |
7.14 ± 1.04 7.13 ± 0.80 |
|
| thickness | right left |
2.54 ± 0.36 2.50 ± 0.44 |
* including the tendon
- Roll-off sections: average length values in millimeters
| M. rect. Superior |
M. rect. Inferior |
M. rect. Medialis |
Lateral rectus muscle |
M. obl. Superior |
M. obl. Inferior |
|
|---|---|---|---|---|---|---|
| Roll-off distance * | 8.92 | 9.83 | 6.33 | 13.25 | 5.23 | 16.74 |
* in primary position
Blood supply
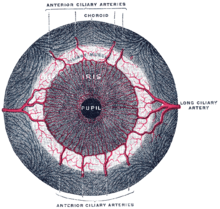
The outer muscles of the eye are mainly supplied by branches of the ophthalmic artery. This happens either directly via the rami musculares or, as with the M. rectus lateralis, indirectly via the arteria lacrimalis , one of the main branches of the A. ophthalmica. Branches of the infraorbital artery also supply the rectus inferior and inferior obliquus muscles. The so-called ciliary arteries (Arteriae ciliares anteriores) are considered to be the lower branches of these arteries . There are usually two supplying vessels on the superior rectus, medial rectus and inferior rectus muscles, and one on the lateral rectus muscle. The number and arrangement of these arteries can vary.
The venous outflow via the ophthalmic vein , as in the rear part of the eye socket ophthalmic vein inferior by the inferior orbital fissure and as superior ophthalmic vein through the superior orbital fissure runs, and then in the cavernous sinus lead to.
Functional disorders and pathophysiology
There are different causes for the loss of function of one or more eye muscles. As a rule, it is paralysis that is triggered by disorders of certain cranial nerves or their core areas . Paralysis of the external and / or internal eye muscles are generally referred to as ophthalmoplegia , which is divided into further sub-forms. In question in this case are a third nerve palsy , a fourth nerve palsy and sixth nerve palsy . These are always accompanied by a restriction of movement in the direction of pull of an affected muscle and the resulting restriction of the monocular field of vision . They are also expressed in a squint position , which varies in size depending on the direction of gaze ( incomitance ), as well as the perception of double images . Acquired paresis are much more common than congenital.
If, in general, the reduction in the ability to relax ( contracture ) of an antagonistic eye muscle on the same side is a secondary consequence of paretic motility disorders, there are clinical pictures in which this is the cause . An example of this is the Stilling-Türk-Duane syndrome , in which a pathological coinnervation of the medial rectus and lateral rectus muscles causes the eyeball to retract into the eye socket.
In principle, however, a strabismus does not have to be the result of reduced strength development and reduced function of a muscle. It is also a result of the total pulling power of agonists and equilateral antagonists, as well as mutual synergists and antagonists. The hyperfunction of a muscle also leads to a squint. This does not mean that it would therefore use more force than a "normal" muscle, but that it predominates in relation to its antagonist. A subfunction does not necessarily have to be of paretic origin either, but can express a relative inferiority to an antagonistic force. According to this, the pulling force of the eye muscles in non-paretic squint is the same, but the balance between agonist and antagonist does not maintain a so-called parallel position, but rather a squint position.
Damage to the superordinate gaze centers, so-called supranuclear paresis , does not lead to failure of individual muscles, but to disturbances of coordinated gaze target movements or vergences and to eye tremors ( nystagmus ). Uncontrolled activity of the trochlear nerve causes a rare microtremor called superior oblique myokymia .
Another cause of a loss of function can be disturbances in the transmission of stimuli from the nerve to the muscle fibers. The Myasthenia gravis is one of the most popular forms of disease of this kind. Likewise loss of function by inflammatory processes (ocular are myositis ), as well as damage possible even the muscle and the tissue. An example of this is the endocrine orbitopathy in Graves' disease . Mechanically conditioned restrictions also occur, for example, in the orbital floor fracture or Brown's syndrome .
Functional test and examination options
The functional test of eye muscles includes the assessment of eye position, eye mobility and the extent of the corresponding fields of vision. It is also important to consider constrained head postures as a compensation mechanism. Corresponding malfunctions almost always trigger sensory disturbances in binocular vision . Therefore, a strict separation between motor and sensory diagnostics is often not very useful in practice.
Orientation studies
Various tests allow a rough assessment of the eye position. This is already possible, for example, by examining the corneal reflex images with the Hirschberg test . Another method is the so-called Brückner test . The mobility and excursion ability of the eyes can be roughly determined using subsequent movements in the nine diagnostic viewing directions (primary, secondary and tertiary positions), in which the over- or under-functioning of one or more muscles can already be clearly identified. Tests of compensatory eye movements, such as the doll's head phenomenon , are also revealing, as is the assessment of command and target eye movements .
The so-called traction test (also: tweezer pull test ), a method to test the passive mobility of the eye, is used to differentiate between actual eye muscle paralysis and mechanical or fibrotic movement restrictions ( pseudoparesis ) .
Quantifying Procedures
To measure misalignments of the eyes, movement distances and fields of vision, there are a number of methods, some of which are apparatus-based, which enable the results to be quantified relatively precisely. One of the most important methods for assessing the position of the eyes is the so-called cover test in conjunction with prisms . Comprehensive motility analyzes, in which up to 180 measured values are determined and documented in various viewing directions, are possible with haploscopic devices such as the synoptometer . For examinations in free space, the so-called tangent table (according to Harms ) is usually used for this. The extent of constrained head postures to compensate for eye muscle disorders can also be quantified using simple methods. The measurement results obtained are usually the prerequisite and basis for further therapeutic measures.
Electrophysiological examination
In certain cases, for example with unclear symptoms of paralysis, it may be necessary to determine the activities of the eye muscles by deriving their electrical potentials . This is done using so-called electromyography using special, thin needles directly on the muscle. If the procedure is used to examine eye tremors (nystagmus), it is called electronystagmography , whereby the measurement is made using electrodes on the temple and forehead .
Imaging procedures
Imaging methods such as magnetic resonance tomography (MRT) or ultrasound examinations are used to assess muscle structures and their dimensions .
Therapeutic approaches
Treatment options for eye muscle imbalance can be found in the form of conservative and surgical measures. Some diseases of the eye muscles can make drug therapies necessary depending on the clinical picture, for example for inflammatory processes. Neurological disorders primarily require treatment of the underlying disease. Only after about 6–8 months should surgical therapy be considered for eye muscle paralysis.
Conservative treatments
Orthoptic exercise treatments in particular offer conservative options for training motor fusion skills . Prism glasses can be used to correct latent or manifest strabismus diseases, but without reducing or even eliminating them. In certain cases of paralysis strabismus, the highly effective neurotoxin botulinum toxin can be used for preoperative diagnostics or as an alternative to a strabismus operation. In addition, orthoptic rehabilitation measures are increasingly being used for cerebral eye muscle disorders.
Operative treatments
- → Main article: Eye muscle surgery
Surgical interventions on the eye muscles are used to correct strabismus, eye tremors (nystagmus) and ocular constrained head postures . Their application is based on the following principles:
- Change in muscle strength
- Change of the monocular field of vision (excursion ability)
- Change of the rolling distance
- Change in the position of the eyeball
- Change in the direction of muscle pull.
Levator palpebrae superioris muscle
- → Main article: Levator palpebrae superioris muscle
The levator palpebrae superioris muscle is the eyelid lifter . He also performs agonistic movements with the superior rectus muscle, so that the upper eyelid rises when looking up and lowers when looking down. It has its origin on the small wing of the sphenoid bone , runs forward over the superior rectus muscle and attaches its tendon as a fan-like structure ( levator aponeurosis ) to a cartilaginous connective tissue plate of the upper lid, the superior tarsus . It is innervated by the oculomotor nerve, namely by its smaller terminal branch, the superior branch ("upper branch").
Loss of muscle function leads to partial or complete drooping of the upper eyelid ( ptosis ) and, as a rule, also restricts the movement of the upper eyelid when looking vertically. A congenital ptosis is rarely the result of a paralysis of the oculomotor nerve rather than a malformation of the muscles of the levator palpebrae superioris itself. Another congenital disorder is the Marcus Gunn phenomenon , a paradoxical innervation between the lateral pterygoid muscle and the M levator palpebrae superioris.
A relative overactivity of the muscle may be at a paretic limiting the view elevation yield. In this case, an increased impulse to turn the gaze upwards is only implemented incompletely by the corresponding muscles, but it has a full effect on the agonistic movement of the levator palpebrae superioris muscle, which leads to an abnormal pulling up of the upper eyelid.
Internal eye muscles
The inner eye muscles consist of smooth muscles and are controlled by the autonomic nervous system. On the one hand, they serve to change the size of the pupil ( adaptation ) and, on the other hand, to regulate the refractive power of the eye.
Ciliary muscle
The ciliary muscle is part of the ciliary body and is used for dynamic adaptation ( accommodation ) of the eye to different object distances. The ciliary muscle consists of two differently extending parts, which are represented by the Müllerian muscle with its ring-shaped fibers and the Brückian muscle with meridional fibers. Müller's muscle is innervated by parasympathetic fibers of the oculomotor nerve and causes near accommodation, while the sympathetically supplied Brück's muscle makes a small contribution to the remote adjustment of the eye (double innervation).
Disturbances of the M. ciliaris lead to an accommodation paralysis ( cycloplegia ). Can, however very pronounced Akkommodationsleistungen (for example, long close work or at a high, but not corrected by glasses or contact lenses hyperopia ), possibly to a cramping of the ciliary muscle ( spasm of accommodation result).
The decline in accommodation performance in old age ( presbyopia ) is not due to a loss of function of the muscle, but to a decrease in the inherent elasticity of the eye lens .
Sphincter pupillae muscle
The sphincter pupillae muscle (also M. constrictor pupillae ) has the function of constricting the pupils ( miosis ). It lies with its grid-like fibers around the pupil in the rear part of the iris stroma. The muscle is controlled by parasympathetic fibers of the Edinger-Westphal nucleus ( Ncl. Accessorius n. Oculomotorii , nucleus of the III. Cranial nerve), which are connected in the ciliary ganglion from the pre- to the postganglionic neuron and called Nn. Pull ciliares breves through the white skin into the inside of the eye.
Paralysis of the sphincter pupillae muscle is an expression of a parasympathetic efferent disorder. The pupil is wide and reacts neither to the incidence of light nor to close focus (absolute pupil rigidity). One of the most common clinical pictures is pupillotonia .
Dilator pupillae muscle
The dilator pupillae muscle lies directly on the pigment sheet of the iris. It serves as an antagonist of the sphincter pupillae muscle of the pupil dilation ( mydriasis ). Its structures are related to those of the sphincter. It is innervated by sympathetic fibers from the superior cervical ganglion of the border cord, which also run through the ciliary ganglion , but without being connected there.
Weakening of the M. dilatator pupillae occurs with disturbances of the sympathetic innervation, with the symptoms of a reduced amplitude of the light reaction and a miosis; In Horner's syndrome , there is also ptosis and a slight elevation of the lower eyelid (as a loss of function of the sympathetically innervated tarsalis muscle ).
Blood supply
The arterial blood supply to the inner eye muscles occurs via the four anterior ciliary arteries, the arteriae ciliares anteriores . They are sub-branches of the ophthalmic artery. The venous outflow is directed through the anterior ciliary veins and the four vortex veins .
Eye muscles of other vertebrates
The musculoskeletal system consisting of the external eye muscles, like the accommodation apparatus consisting of the internal muscles, is a characteristic feature of the jaws (gnathostomata), to which all vertebrates belong, with the exception of the lampreys and hagfish .
External eye muscles
The extraocular muscles are mesodermal origin and originate as the branchial arch muscles the presomitic, paraxial mesoderm ( striated muscle ) before the otic placode . As in humans from the oculomotor nerve , the III. Cranial nerves, innervated eye muscles, rectus superior , rectus inferior , medial rectus and inferior obliquus muscles , together with the levator palpebrae superioris (eyelid lifter), originate from the head mesoderm of the foremost two thusomeres . The superior oblique muscle innervated by the trochlear nerve arises from the third and the lateral rectus muscle innervated by the abducens nerve , and the retractor bulbi muscle , which is no longer present in humans , from the fifth.
The eye muscles originally served primarily to immobilize the retinal image without shifting the image during locomotion and when turning the head . With the development of certain areas of the fundus , especially the fovea centralis , the function of the eye muscles also changed, and the eyes were used to change the direction of gaze with increasing mobility.
The outer eye muscles of birds behave similarly to those of mammals, the retractor bulbi muscle is missing. Birds can move both eyeballs independently of each other, but only to a very small extent overall (only about 2 ° in owls). This limitation is compensated for by the high mobility of the head and neck. Birds also have two muscles for moving the nictitating membrane : the quadratus membranae nicitantis muscle and the pyramidalis membranae nicitantis muscle .
Internal eye muscles
The accommodation (dynamic change in the refractive power) is sometimes fundamentally different in the different vertebrates. For example, at nine eye , the cornea and the other for adjustment to view distances lens by contraction of a Corneamuskels approximated the retina. In the case of fish ( cartilaginous fish and bony fish ), amphibians and snakes, however, the rigid lens located in a suspension device is displaced by different internal muscle structures. In cartilage and bony fish, the lens is pulled backwards by the retractor lentis muscle, and forwards in amphibians by the protractor lentis muscle . While the muscles in cartilaginous fish are only formed below the lens, in amphibians they form a wreath at the base of the suspension apparatus. Snakes do not have ligaments or muscles. With them, the lens is pushed forward by a muscle contraction at the base of the iris and the resulting higher pressure in the vitreous body .
In contrast to the inner, smooth eye muscles of mammals, these in birds and other reptiles ( lizards , turtles and crocodiles ) consist of striated muscles. The ciliary muscle is divided into two parts: Musculus ciliaris anterior and Musculus ciliaris posterior . The M. ciliaris anterior of birds and reptiles reduces the radius of curvature of the cornea when it contracts, the M. ciliaris posterior narrows the diameter of the ciliary body and compresses the soft lens of the eye. The share of the two muscles in accommodation varies within the bird world. In principle, diurnal birds tend to accommodate by changing the corneal curvature, and nocturnal birds with the help of the ciliary body and the elastic lens. The two pupillary muscles in the iris are also striated across and therefore do not react to the pharmacological agents commonly used in ophthalmology to dilate the pupil and eliminate accommodation, such as atropine .
literature
- Theodor Axenfeld (founder), Hans Pau (ed.): Textbook and atlas of ophthalmology. With the collaboration of Rudolf Sachsenweger a . a. 12th, completely revised edition. Gustav Fischer, Stuttgart a. a. 1980, ISBN 3-437-00255-4 .
- Herbert Kaufmann : Strabismus . 5th completely revised edition with Heimo Steffen. Georg Thieme Verlag, 2020, ISBN 978-3-13-241330-6 .
- Siegfried Priglinger , Michael Buchberger: Eye motility disorders. Computer-aided diagnosis and therapy. Springer, Vienna a. a. 2005, ISBN 3-211-20685-X .
- Rudolf Sachsenweger (Ed.): Neuroophthalmology. 3rd, revised edition. Thieme, Stuttgart a. a. 1983, ISBN 3-13-531003-5 .
- Paul Simoens: organ of vision , organum visus. In: Franz-Viktor Salomon, Hans Geyer, Uwe Gille (Ed.): Anatomy for veterinary medicine. 2nd, revised and expanded edition. Enke, Stuttgart 2008, ISBN 978-3-8304-1075-1 , pp. 579-612.
Individual evidence
- ↑ Wilfried Westheide, Reinhard Rieger (Ed.): Special Zoology. Part 2: vertebrates or skulls. Gustav Fischer Verlag, 2004, ISBN 3-8274-0900-4 , p. 86.
- ^ A b Herbert Kaufmann, Wilfried de Decker: Strabismus . Ed .: Herbert Kaufmann. 3. Edition. Georg Thieme Verlag, Stuttgart 2003, ISBN 3-13-129723-9 , p. 37 .
- ^ Herbert Kaufmann: Strabismus. With the collaboration of W. de Decker u. a.Enke, Stuttgart 1986, ISBN 3-432-95391-7 , p. 31.
- ↑ Herbert Kaufmann, Wilfried de Decker: Strabismus . Ed .: Herbert Kaufmann. 3. Edition. Georg Thieme Verlag, Stuttgart 2003, ISBN 3-13-129723-9 , p. 58 ff .
- ^ Herbert Kaufmann: Strabismus. With the collaboration of W. de Decker u. a.Enke, Stuttgart 1986, ISBN 3-432-95391-7 , p. 54.
- ^ Herbert Kaufmann: Strabismus. With the collaboration of W. de Decker u. a. Enke, Stuttgart 1986, ISBN 3-432-95391-7 , p. 61 ff.
- ^ Albert J. Augustin: Ophthalmology . Springer-Verlag, 2007, ISBN 978-3-540-30454-8 .
- ↑ Herbert Kaufmann, Wilfried de Decker: Strabismus . Ed .: Herbert Kaufmann. 3. Edition. Georg Thieme Verlag, Stuttgart 2003, ISBN 3-13-129723-9 , p. 511 .
- ↑ Paul Simoens: organ of sight, Organum visus. In: Franz-Viktor Salomon u. a. (Ed.): Anatomy for veterinary medicine . 2nd ext. Edition. Enke-Verlag, Stuttgart 2008, ISBN 978-3-8304-1075-1 , pp. 579-612.
- ^ Herbert Kaufmann: Strabismus. With the collaboration of W. de Decker u. a.Enke, Stuttgart 1986, ISBN 3-432-95391-7 , p. 38.
- ^ Herbert Kaufmann: Strabismus. With the collaboration of W. de Decker u. a.Enke, Stuttgart 1986, ISBN 3-432-95391-7 , p. 32 ff.
- ↑ Example of the Duisburg Clinic - Special Medical Treatment Procedures ( Memento of the original from July 18, 2014 in the Internet Archive ) Info: The archive link was automatically inserted and not yet checked. Please check the original and archive link according to the instructions and then remove this notice.
- ↑ Guidelines for Diagnostics and Therapy in Neurology. 3rd revised edition. Georg Thieme Verlag, Stuttgart 2005, ISBN 3-13-132413-9 . (Keyword: peripheral eye muscle and nerve paresis; AWMF guidelines register: No. 030/033)
- ↑ T. Krzizok: Botulinum toxin injections for the treatment of strabismus. Springer Verlag, Berlin / Heidelberg, ISSN 0941-293X .
- ↑ Axenfeld / Pau: Textbook and Atlas of Ophthalmology. With the collaboration of R. Sachsenweger u. a. Gustav Fischer Verlag, Stuttgart 1980, ISBN 3-437-00255-4 , p. 464.
- ↑ after Hans-Peter Schultze: Gnathostomata, Kiefermünder. In: W. Westheide, R. Rieger (Ed.): Special Zoology. Part 1: Protozoa and invertebrates. Gustav Fischer, Stuttgart / Jena 1997, 2004, ISBN 3-8274-1482-2 , p. 196.
- ↑ after Wolfgang Maier: head. In: W. Westheide, R. Rieger (Ed.): Special Zoology. Part 1: Protozoa and invertebrates. Gustav Fischer, Stuttgart / Jena 1997, 2004, ISBN 3-8274-1482-2 , p. 32.
- ↑ a b c d after Michael Hoffmann, Steven F. Perry: Kopf. In: W. Westheide, R. Rieger (Ed.): Special Zoology. Part 1: Protozoa and invertebrates. Gustav Fischer, Stuttgart / Jena 1997, 2004, ISBN 3-8274-1482-2 , pp. 85-86.
- ^ A b Franz-Viktor Salomon, Maria-Elisabeth Krautwald-Junghans: Sehorgan. In: Salomon / Geyer / Gille (Hrsg.): Anatomy for veterinary medicine . 2nd ext. Edition. Enke, Stuttgart 2008, ISBN 978-3-8304-1075-1 , pp. 804-806.
- ↑ Winnie Achilles and Franz-Viktor Salomon: Anatomie der Reptilien In: Salomon / Geyer / Gille (Hrsg.): Anatomie für die Tiermedizin . 2nd ext. Edition. Enke, Stuttgart 2008, ISBN 978-3-8304-1075-1 , pp. 815-844.