Spinal cord
The spinal cord ( Latin medulla spinalis or medulla dorsalis , ancient Greek ῥαχίτης μύελος rhachítes mýelos or νωτιαῖος μύελος nōtiaios mýelos ) is that part of the central nervous system of the vertebrates that is surrounded by the meningeal brain within the vertebral canal . Substantial parts of the peripheral nervous system are connected to the spinal cord via the spinal nerves .

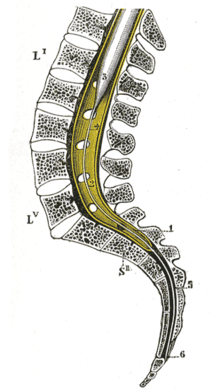
Color legend:
Positional relationships
The spinal cord develops from the posterior neural tube and lies as a cylindrical strand of connective tissue membranes ( meninges ), surrounded by cerebrospinal fluid ( liquor cerebrospinalis ) and enclosed by the spine in the vertebrate back area . In humans, it passes cranially into the elongated medulla of the brain stem at about the level of the large occipital opening without a sharp border ; at the caudal end it tapers conically to the conus medullaris (medullary cone), the tip of which ends in a thread-like manner with the filum terminale (end thread).
While the spinal cord still fills the entire length of the spinal canal before the 3rd human embryonic month, the end of the conus regularly shifts cranially during fetal development due to the relatively greater length growth of the spine, which is also referred to as ascent or ascent. In the newborn, the tip of the conus is usually approximately at the level of the third lumbar vertebra (L3); in adults, 95% of the spinal cord ends at L2 or higher.
As a result, the roots of the spinal nerves emerging from the spinal cord on both sides cover an increasingly longer path within the spinal canal before they leave it through their intervertebral hole. Below the tip of the conus, in addition to the filum terminale, only the root fibers of the paired spinal nerves run as a cauda equina (horse's tail). In adults, a lumbar puncture , usually after a puncture between the spinous processes of the 3rd and 4th lumbar vertebrae, can be used to remove CSF or inject a drug without the risk of immediately injuring the spinal cord.
An ascensus also occurs in other mammals - and ends here at the level of the posterior lumbar vertebrae - but not in other vertebrates . In humans, disorders of the ascensus can not only lead to a depression in the cone, but also to the clinical picture of a tethered cord if there is abnormally increased tension on the spinal cord and nerve fibers .
Spinal membranes

(1) Conus medullaris ,
(2) Filum terminale ,
(3) Cauda equina .
The membranes of the spinal cord ( Meninges medullae spinalis ) merge with the meninges and, like these, are differentiated into the outer dura mater , the middle arachnoid (spider tissue) and the pia mater directly adjacent to the spinal cord . Compared to the membranous covering in the area of the brain, some structural peculiarities stand out. The dura mater is not fused with the periosteum of the bony elements of the vertebral canal. An epidural space or peridural space is therefore formed between the bone and the dura mater . In addition to a dense venous plexus, it also contains connective and fatty tissue . Local anesthetics , for example, can be introduced into the epidural space in order to break the conduction of excitation from nerve fibers ( epidural anesthesia ).
Furthermore, there are segmental bridges between the membranes of the spinal cord, which form the so-called denticulate ligament as a “toothed ligament”. These structures, which are triangular when viewed from above, serve to stabilize the suspension of the spinal cord in the subarachnoid space between the arachnoid and pia mater, which is filled with cerebrospinal fluid .
Outer shape
The spinal cord is a whitish, round cord cylinder that is thickened in the intumescentia cervicalis or the intumescentia lumbosacralis , since these areas innervate the upper and lower extremities as well as the trunk . In the caudal direction, the spinal cord otherwise becomes somewhat narrower because of the fewer ascending and descending connections with brain regions and tapers at the lower end as a conus medullaris (medullary cone). Its tip continues the approximately 1 mm thick filum terminale (end thread), which, in addition to the connective tissue of the pia mater, also contains glial cells and fat. It connects the tip of the conus with the lower end of the dural sac or, in humans, with the posterior surface of the coccyx .

On the front of the spinal cord, a fine furrow runs from top to bottom, which divides the ventral side (ventral) as the fissura mediana ventralis left from the right side. On the back there is a deeper trench between the two sides, the sulcus medianus posterior . In the lateral circumference, three strands (Latin funiculi ) can be separated from each other: paramedian of the median fissure, the anterior strand ( funiculus anterior ), behind the posterior strand ( funiculus posterior ) and between the two the lateral strand ( funiculus lateralis ).
In the groove on one side between the posterior and lateral cord , the posterior lateral sulcus , the posterior roots of the spinal nerves enter , and between the lateral and anterior cord , in the anterior lateral sulcus , their anterior roots emerge from the spinal cord. As Fila radicularia the front and the rear roots roots form two continuous rows on each side and unite only the height of the intervertebral foramina ( intervertebral foramina ), during passage through the spine to the individual spinal this page.
Birds are the only recent vertebrates in which the so-called glycogen body (also called corpus gelatinosum ) is embedded in the area of the intumescentia lumbosacralis between the posterior cords on both sides . It is a gelatinous, egg-shaped formation with glycogen-rich glial cells, the functional significance of which has not yet been clarified. In the domestic chicken it is about 1 cm long and 4 mm wide.
structure
Externally, the spinal cord can be divided into segmental sections depending on the common roots of a pair of spinal nerves, which are assigned to five consecutive areas:
- Neck or cervical medulla ( pars cervicalis ), in mammals with 8 segments (C1-C8)
- Breast or thoracic cord ( pars thoracica ), in humans with 12 segments (Th1-Th12)
- Lumbar or lumbar cord ( pars lumbalis ), in humans with 5 segments (L1-L5)
- Cross or sacral medulla ( pars sacralis ), in humans with 5 segments (S1 – S5)
- Tail or coccygeal medulla ( pars coccygis ), usually 1 segment (Co1) in humans
One of the mostly 31 segments in humans corresponds to a section of the spinal cord to which the root fibers for one left and one right spinal nerve belong. The associated pair of spinal nerves leaves the spinal canal above or below a vertebra and exits through intervertebral holes on both sides, which are usually no longer exactly at the level of its spinal cord segment. It is assigned and named to a spinal column area after these exit points.
In the thoracic area and further caudally, a spinal nerve and its segment is called after the vertebra above it, and the number of back carcass segments corresponds to the number of vertebrae. In contrast, with seven cervical vertebrae, eight segments of the cervical medulla are assigned to the cervical region, since the first spinal nerve (C1) does not emerge below, but above the first cervical vertebra, the atlas ; the pair of spinal nerves exiting below the seventh cervical vertebra (C8) is still assigned to the cervical area. What superficially resembles a fence post problem has its deeper reason in the fact that parts of the occipital bone (Os occipitale) can be considered as fused vertebrae in evolutionary terms.
Feinbau
The spinal cord is made up of gray matter and white matter . The gray matter consists mainly of nerve cell bodies ( perikaryen ), the white matter of axons .
Gray matter
The gray matter has the shape of a butterfly in the cross-section of the spinal cord . The front, wider wing part is called the front horn ( Cornu anterius , in animals Cornu ventrale ), the rear, narrower part is called the rear horn ( Cornu posterius or dorsale ). The smaller lateral horn ( cornu laterale ) is located between the anterior and posterior horns in the thoracic and lumbar cord area .
The two butterfly-wing-like sides of gray matter are connected with each other by cross connections ( Commissura grisea ). They run as gray commissures in the central region in front of and behind the central canal ( Canalis centralis ). This tubular cavity is filled with liquor and represents the inner liquor space of the spinal cord.
The gray matter can be divided into ten layers ( laminae ), some of which are also known by other names. Lamina II is also known as the substantia gelatinosa Rolandi (after Luigi Rolando ). The laminae I – VII are in the posterior horn, the laminae VIII and IX in the anterior horn. The lamina X contains the commissura grisea ( anterior or posterior ). Functionally, individual nerve nuclei or core columns ( Columnae ) can be differentiated (see figure).
Nerve cell types
Different cell types can be highlighted in the cytoarchitecture of the spinal gray matter:
- Root cells , the axons of which form the anterior root, can be of different sizes. Particularly large ones are located in the anterior horn and, as motor neurons, conduct their signals to muscle fibers in skeletal muscles.
-
Internal cells whose axons do not leave the spinal cord. They represent the so-called self - apparatus of the spinal cord, also called the propriospinal system . The neural networks of this internal system of the spinal cord realize the spinal integration services. For example, you can use simple (monosynaptic) reflex arcs to link motor neurons with each other and thus relate individual muscles in muscle groups as players or opponents and coordinate their activity. Switch cells, association cells and commissure cells belong to the self-apparatus.
- Switching cells are interneurons whose processes do not leave the gray matter of a spinal cord segment. On the same side ( ipsilateral ), they create links between cells of the same segment (intrasegmental) and mediate e.g. B. Self-reflexes . These interneurons also include the Renshaw cells , which have an inhibitory feedback on motor neurons .
- Association cells are propriospinal neurons that connect different spinal cord segments with one another. Its processes also run ipsilaterally, but longitudinally between different segment planes (intersegmental), in the gray matter and the adjacent tracts of the basal bundles (
- Commissure cells are neurons of the self-apparatus, the neurites of which cross the median plane and pull (as commissura ) to the other side. They connect within a spinal cord segment with the opposite side ( contralateral ) and ensure that excitation impulses also reach the other side. In this way, they also convey crossed reflexes, in which the other side of the body reacts, as is typical for various tetrapodic movement patterns.
- Strand cells are projection neurons whose axons leave the gray matter and move on in the white matter. Here they descend, or, more commonly, ascend in strands and carry signals to other spinal cord segments and to sections of the brain. They therefore only partially belong to the spinal cord's own apparatus.
Association, commissure and cord cells are often involved in triggering external reflexes .
Back horn
The posterior horn receives sensitive information from the periphery via the dorsal , sensitive root of the spinal nerve. This information is passed on to the brain, but some of it is already processed in the spinal cord.
The dorsal root is formed by axons of pseudounipolar nerve cells whose cell bodies lie outside the spinal cord in the spinal ganglion . Their axons enter the spinal cord via the dorsal (sensitive) root, where a part in the posterior horn is switched to a second neuron. Other dorsal root axons run without switching into the medulla oblongata .
The dorsal horn, which emerges embryologically from the wing plate, consists of a thin marginal zone from dorsal to ventral ( from the back to the abdomen ), to which the substantia gelatinosa adjoins, in which pain afferents of the skin receptors are switched to the second neuron before they pull in the lateral spinothalamic tract to the thalamus . Here interneurons, which are activated by the transmitter serotonin, inhibit the transmission of pain by releasing endorphins. This makes the substantia gelatinosa clinically extremely relevant and offers approaches to explain the mechanisms of the controversial acupuncture or the pain-relieving effect of some antidepressants.
The nucleus proprius is located in laminae 3 and 4 and is found at the entire level of the spinal cord. It is the target of sensitive afferents of deep sensitivity and forms the anterior spinocerebellar tract in its cranial course (leading to the head).
Laminae 5 and 6 finally contain the nucleus dorsalis (Stilling- Clarke ), which is also called the nucleus thoracicus posterior . Just like the nucleus proprius, the nucleus dorsalis receives afferents of deep sensitivity (muscle spindles, joint and tendon receptors), which are conducted to the cerebellum via the tractus spinocerebellaris posterior.
Front horn
The anterior horn arises from the baseplate and contains perikarya, the axons of which leave the spinal cord as a radix anterior to innervate the skeletal muscles. In the layered structure, the anterior horns consist of laminae 8 and 9. This is where the large multipolar α-motor neurons and also the somewhat smaller ɣ-motor neurons and Renshaw cells occur. This is where the impulses of the pathways coming from the brain ( pyramidal pathways and extrapyramidal pathways ) as well as the impulses of the muscle reflexes end and are passed on as a "common motor end route" to the organ of success - the skeletal muscles .
Side horn
In the area of the thoracic cord and, somewhat less clearly, in the lumbar cord, between the anterior and posterior horns, there is the so-called lateral horn, which is formed by the cell bodies of vegetative neurons and belongs to the sympathetic nervous system . Their efferent fibers leave the spinal cord via the anterior root, pull to the border cord and are partly connected to the second neuron there. The rest of them move to the prevertebral ganglia to be interconnected there. Sympathetic-afferent fibers come from the periphery with the posterior root to the lateral horn. Cell bodies of parasympathetic neurons are located at an equivalent point in the sacral cord , but without forming a recognizable lateral horn. The axons run as the pelvic splanchnic nerves to the pelvinum ganglion and to the intramural ganglia.
White matter
In the white matter of the spinal cord there are ascending (mostly sensitive) pathways that lead to the brain, and descending (mostly motor) pathways that come from the brain. The cause of the white color is the myelination of the axons .
Ascending orbits
The posterior column web passes information from the mechanoreceptors for epikritische sensitivity and low sensitivity respectively the same side of the body, first to in the medulla oblongata ( medulla oblongata ). The cell bodies of the axons ascending in the posterior cord are located in the spinal ganglia and are each assigned to different segments of the spinal cord. Without switching in the posterior horn, the fibers move into the medullary brain and end in the core areas there, the nucleus gracilis for information from the lower half of the body and the nucleus cuneatus for information from the upper half of the body.
The posterior cord shows in the upper spinal cord on each side a subdivision into the fasciculus cuneatus and the fasciculus gracilis , the primary afferent fibers of which are switched to secondary afferent neurons in the nuclei of the same name. The ascending fibers of these (2nd) neurons in the posterior cord nuclei cross in the medulla oblongata to the opposite side ( decussatio lemniscorum medialium ) and run in the lemnicus medialis to contralateral thalamic nuclei (VPL). This section of the path gives the lemniscale system its name .
On the other hand, the lateral and ventral spinothalamic tracts, as the anterior tract, carry information for protopathic sensitivity (pain, temperature and gross pressure sensation) to various core areas in the thalamus (including MD, VPL, VPM). The fibers of the spinothalmic tract emanate from nerve cell bodies in the spinal cord, the axons of which cross to the opposite side at the level of the original segment. These cord cells in the dorsal horn are secondary (2nd) afferent neurons; they receive primary afferents of the spinal ganglion cells with information from mechanoreceptors as well as from nociceptors and thermoreceptors . This spinothalamic pathway in the anterior and lateral cord is part of the so-called anterolateral system .
The anterior spinocerebellar tract ( lateral cerebellar tract or Gower's bundle ) arises primarily from the dorsal nucleus of the posterior horn and ends in the cerebellum . It either runs uncrossed or crosses the side twice and carries proprioceptive (= information about the location and position of joints, muscles, tendons) information.
The tractus spinocerebellaris posterior ( Flechsig bundle ) emanates from the cells of the nucleus thoracicus and reaches the cerebellum uncrossed via the anterior strand. It is used for deep sensitivity .
Descending orbits
The pyramidal tract ( corticospinal tract ) extends from the motor cortex of the cerebral cortex to the anterior horn.
As extrapyramidal pathways is any motor pathways that do not belong to the pyramidal tract. They include the rubrospinal tract , the vestibulospinal tract , the reticulospinal tract, and the tectospinal tract . They all also end in the Vorderhorn.
Neurotransmitters
The main inhibitory neurotransmitter in the spinal cord is glycine . Interneurons and z. B. the Renshaw cells are glycinergic ; that is, they release glycine from their synaptic terminals .
embryology
In the vertebrate embryo , the spinal cord arises from the neural folds of the ectoderm , immediately above the notochord . The neural folds close to form the neural tube , a fluid-filled canal that is surrounded by an epithelium . If this occlusion is disturbed, various forms of dysraphy occur. A spina bifida aperta ("open back") can develop, in which the vertebral arches remain incomplete on the back. Only the membranes of the spinal cord ( meningocele ) or also the spinal cord ( meningomyelocele ) can bulge outwards through this defect. Where the neural groove itself does not close, creating a Myeloschisis ( rachischisis ). If this defect occurs at the rostral (front) end of the neural groove, the brain may even fail to form ( anencephaly ).
The nerve and glial cells differentiate from the neural epithelium . The spinal ganglia and sympathetic neurons arise from the so-called neural crest . Around the neural tube, the mesenchyme gives rise to the primal vertebrae , from which, among other things, the spine arises.
First, proneurons (the precursors of neurons) leave the neuroepithelium and form a mantle layer (mantle zone) from which the gray matter arises. Most of the axons of these proneurons grow towards the surface and thus form the edge layer (marginal zone ), which later becomes white matter.
Within the mantle layer, two thickenings develop through cell division and cell migration, the wing plate (alar plate) and the base plate (basal plate), which gradually take on the appearance of a butterfly. The marginal layer is divided into 3 strands by the further ingrowth of ascending and descending axons, their myelination and the enlargement of the wing and base plates: posterior strand, lateral strand and anterior strand.
With the tethered cord, the relative shortening of the spinal cord does not occur.
Blood supply
Three arteries supply the spinal cord: in front the arteria spinalis anterior , behind two arteriae spinales posteriores . In animals with a horizontal body position, the term arteria spinalis ventralis and dorsalis is used instead . These three arteries originate in the neck area on both sides from the vertebral arteries that run laterally in the spine . In the thorax and lumbar region, they receive segmental inflows from the intercostal arteries ( Arteriae intercostales posteriores ) and the lumbar arteries ( Arteriae lumbales ). The largest and most important segmental artery is the Adamkiewicz artery ( Arteria radicularis magna ), which is usually between the 9th and 12th breast segment. Closure of this vessel is particularly serious for the blood supply to the thoracic spinal cord.
In the area between the 4th and 6th thoracic vertebrae, the formation of such inflows is low, so that this section is particularly at risk of suffering a spinal cord infarction in the event of a vascular occlusion . The venous blood is transported away via two large veins, some of which run parallel to the arteries: anterior spinal vein and posterior spinal vein.
phylogenesis
In the form described here, the spinal cord is built up in all representatives of the cranial animals (Gnathostomata), although there are slight differences in detail in the various taxa .
In the basal chordates , which include the acrania (Acrania) and tunicates (tunicates) are, there is no differentiated spinal cord. Instead, there is only the neural tube, which is homologous to the later spinal cord . At its front end it has a thickening called a cerebral vesicle, but which has little in common with the vertebrate brain. The neural tube itself is made up of partially highly differentiated neurons, but little is known about their interconnections and functions. The main axons come from the so-called colossal cells, which represent large intermediate neurons and whose axons form giant ventromedian fibers. Segmentally there are dorsal nerve roots that correspond to the later dorsal root ganglia, but are offset from one another due to the offset myomers . While in the acranians this structure exists up to the adult animal, in the tunicata it is only found in the larval state.
The hagfish (Myxinoida) and the lampreys (Petromyzontida), which as jawless (Agnatha) represent the most original taxa of the craniota, already have a spinal cord in which the neural tube, as in the later vertebrates, only represents the lumen . In the hagfish it is structured in the form of a ribbon and has various motor neurons and interneurons without a segmental arrangement, the roots of the spinal nerves only unite in the somatic muscles, and a number of organs are innervated directly by spinal nerves. The lamprey's spinal cord, on the other hand, is more similar to that of later vertebrates. It is separated into white and gray matter, and the cell bodies of the giant axons are mainly located in the brain stem. On the other hand, the interconnection of the neurons in the spine is so complex that the animals can swim in a coordinated manner even after they have been severed in front of the brain, for example by removing the head. The dorsal and ventral roots of the spinal nerves unite in the animals close to the spinal cord, but do not protrude segmentally from the spinal cord at the same height.
The cartilaginous fish (Chondrichthyes), to which the sharks and rays belong, have a spinal cord with segmental spinal nerves, as is typical for the skull animals. However, they have some peculiarities. Their spinal cord is also very autonomous, and a shark can swim in a coordinated manner even if the spinal cord is severed at the neck. In contrast to all other vertebrates, the number of sensory and motor root ganglia increases throughout life during growth. In addition to other differences in the fine structure, such as a separate descending cord for the nuclei of cranial nerve VIII , the cartilaginous fish have a caudal neurosecretory system , which plays an important role in osmoregulation and reproduction.
In all of the following taxa, from the ray fins to the amphibians , the various reptile taxa as well as birds and mammals , the structure and function of the spinal cord corresponds to the basic pattern shown and only differs from one another in very specific details.
Myelopathies
Myelopathies (damage to the spinal cord) are caused by:
- Degeneration ( degenerative myelopathy in dogs ), syringomyelia
- Pressure ( tumor , herniated disc , whiplash )
- Circulatory disorders
- Severing ( paraplegia )
- Inflammation ( multiple sclerosis )
- Infections such as neurolues , sepsis
- Spinal abscesses
- Malformations like the Chiari malformation
Examination of the spinal cord
The spinal cord itself is not directly accessible to clinical examination due to its position in the bony spinal canal. Reflex tests and the distribution profile (→ reference muscles ) of paralysis ( paralysis ) or sensory disturbances give the neurologists but important clues to the nature and location of the injury. Neurophysiological examination methods such as motor and somatosensitive evoked potentials allow a functional examination of individual tract systems of the spinal cord such as the corticospinal tract and the posterior cord tract. Investigations of reflex pathways via motor neurons in the spinal cord are possible with the help of the H-reflex and the F-wave.
Structural changes, on the other hand, can be detected with the imaging methods , especially magnetic resonance tomography , computed tomography and myelography . Malformations in the blood vessel system of the spinal cord can also be visualized with angiography . The lumbar puncture and examination of the spinal cord fluid can also provide evidence of inflammation .
literature
- F.-V. Salomon, H. Geyer, U. Gille: Anatomy for veterinary medicine . Enke-Verlag, Stuttgart 2004, ISBN 3-8304-1007-7
- Th. H. Schiebler (Ed.): Anatomie . Springer-Verlag, 9th edition, 2005, ISBN 3-540-21966-8
- W. Westheide, R. Rieger: Special Zoologist; Part 2: vertebrates and skulls . Gustav Fischer Verlag, Stuttgart, Jena, 2004, ISBN 3-8274-0307-3
- Emil Villinger: Guide for studying morphology and fiber orientation . Published by Wilhelm Engelmann, Leipzig 1905, p. 7, 8, 95, 151 ( online ).
- E. Villiger: Brain and Spinal Cord: Guide to the Study of Morphology and Fiber Orientation . Nabu Press, 2010, ISBN 978-1-141-47426-4
Web links
Individual evidence
- ↑ Federative Committee on Anatomical Terminology (1998). Terminologia Anatomica . Stuttgart: Thieme
- ^ Siebenhaar, FJ (1850). Terminological dictionary of the medical sciences. (Second edition). Leipzig: Arnoldische Buchhandlung.
- ↑ a b Liddell, HG & Scott, R. (1940). A Greek-English Lexicon. revised and augmented throughout by Sir Henry Stuart Jones. with the assistance of. Roderick McKenzie. Oxford: Clarendon Press.
- ↑ also according to magnetic resonance imaging of dead fetuses, see OJ Arthurs, S. Thayyil, A. Wade, WK Chong, NJ Sebire, AM Taylor: Normal ascent of the conus medullaris: a post-mortem fetal MRI study. In: The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. Volume 26, Number 7, May 2013, pp. 697-702, ISSN 1476-4954 . doi: 10.3109 / 14767058.2012.746307 . PMID 23211127 .
- ^ MA England: Color Atlas of Life Before Birth. Normal fetal development. Mosby, 1983, ISBN 0-8151-3119-4 .
- ^ AF Reimann, BJ Anson: Vertebral level of termination of the spinal cord with report of a case of sacral cord. In: Anatomical Record-advances in Integrative Anatomy and Evolutionary Biology. Volume 88, pp. 27-138, 1944.
- ↑ DA Hertzler, JJ DePowell, CB Stevenson, FT Mangano: Tethered cord syndrome: a review of the literature from embryology to adult presentation. In: Neurosurgical Focus . Volume 29, Number 1, July 2010, p. E1, ISSN 1092-0684 . doi: 10.3171 / 2010.3.FOCUS1079 . PMID 20593997 . (Review).
- ^ W. Möller, W. Kummer: The blood-brain barrier of the chick glycogen body (corpus gelatinosum) and its functional implications . In: Cell Tissue Res . Volume 313, No. 1, July 2003, pp. 71-80. PMID 12768407 .



