prostate
The prostate ( ancient Greek προστάτης prostátēs , 'head', 'front man') or prostate gland is an accessory sex gland of all male mammals including humans and produces part of the sperm . In humans, it lies below (in animals, behind) the urinary bladder and surrounds the initial part of the urethra (urethra) up to the pelvic floor . In men, it resembles a chestnut in size and shape . At the back of the prostate which borders the rectum (rectum) . Therefore it can be felt and assessed with the fingers from the rectum and stimulated in a sexual context through prostate massage .
In terms of its glandular function, there is a female equivalent of the prostate, the paraurethral gland .
anatomy

The prostate is located subperitoneally, that is, under (in animals correspondingly behind) the peritoneum (peritoneum) . It rests on the urogenital diaphragm and hugs the fundus (clinically also "neck") of the urinary bladder from caudally (below in humans, behind in quadrupeds) . Dorsal (towards the back), it is through the rectum (rectal) limited, ventral (toward the abdomen) through the pubic (symphysis pubis) . It is connected to this by a ligament , the puboprostatic ligament . Through the center of the prostate which runs urethra (urethral) . For this reason, pathological enlargement of the prostate can lead to problems with urination and even bladder occlusion.
In humans, the paired injection channel (lat. Ductus ejaculatorius ) runs through the prostate , through which about 70% of the ejaculate volume flows during ejaculation , namely the fractions from the epididymis on the same side and the vesicle gland on the same side .
function
The prostate is an exocrine gland with ducts into the urethra. It consists of around 30 to 50 individual glands, more precisely tubuloalveolar glands . These produce a secretion that is released into the urethra during ejaculation , where it mixes with the sperm . The secretion makes up about 30% of the ejaculate in humans. The prostate secretion has a pH value of 6.4. On the other hand, the prostate secretion contains a biogenic amine for cell proliferation , which induces movement on the sperm. Furthermore, the prostate- specific antigen (PSA) is secreted from the epithelial cells of the prostate . It is a serine protease that makes the ejaculate thinner by breaking down certain proteins. The PSA is an important laboratory marker for diseases of the prostate, especially prostate cancer .
The prostate encloses the urethra below the bladder outlet. It can change its inner shape and acts like a soft tissue, in that when the penis erect it only lets sperm fluid through the injection channel of the spermatic duct and thereby constricts the urethra at the bladder outlet; without an erection, however, this part of the urethra receives its normal diameter, so that if necessary Urine can drain. It ensures that only urine or only sperm flows through the urethra, never both at the same time.
Blood supply and lymphatic drainage
The arteries supplying the prostate arise mainly from branches of the internal iliac artery (inner pelvic artery), especially the inferior vesical artery (lower bladder artery, referred to in animals as the posterior bladder artery, caudal vesical artery ), but also the internal pudendal artery (internal pubic artery) and Arteria rectalis media (middle rectal artery ).
The veins of the prostate form a plexus (braid) around their sides and base. This prostate venous plexus empties into the internal iliac vein (internal pelvic vein). In addition, it has connections cranially (towards the head) with the plexus venosus vesicalis (vein plexus of the urinary bladder) and dorsally (towards the back) with the plexus venosus vertebralis internus (inner vein plexus of the spine). Lymphatic drainage of the prostate occurs through lymphatic vessels that empty into the lumbar and cross lymph nodes .
Innervation
The prostate is innervated by the sympathetic and parasympathetic nerves. The sympathetic fibers originate from the inferior hypogastric plexus . They innervate the excretory ducts and the smooth muscle cells. The parasympathetic fibers originate from the spinal cord segments S2-S5. They also run as the pelvic splanchnic nerves to the inferior hypogastric plexus . They end under the basement membrane of the epithelium.
Feinbau
Mammals
In the case of non-primates, a comparative anatomical distinction is made between a compact glandular body ( corpus prostatae , absent in sheep and goats ) and individual glands embedded in the urethral wall ( pars disseminata , "scattered part", absent in horses ).
The prostate body is divided into left and right lobes in dogs , cats , cattle , pigs, and horses. In the dog it is relatively largest, both lobes fuse as much as possible and completely enclose the urethra, in the other animals it is on the side of the urethra and in the immediate vicinity of the seminal bladder gland in front of it . In rodents , the prostate consists of three paired lobes, with the anterior cranial lobe usually referred to as the coagulation gland . The other two lobes ( lobus dorsalis and ventralis ) lie behind, to the side and above or below the urethra. In rabbits , two lobes ( lobus dorsalis and ventralis ) can be distinguished on both sides .
The excretory ducts of the prostate open into the pelvic part of the urethra on the side of the seminal mound .
human
The cross section of the prostate can be divided into three zones, which differ in the excretory ducts of the glands: the periurethral mantle zone, the inner zone and the outer zone. The ducts of the glands in the inner zone terminate directly in the urethra. The glands in the outer zone collect their secretions in common excretory ducts before ending in the urethra. This classification is important in the development of tumors (see below).
The ducts ( ductuli prostatici ) of the prostate glands in the prostate open into the sinus prostaticus on both sides of the colliculus seminalis ( seed mounds ) of the urethra. Depending on their function, their glandular epithelium is either a single-layer squamous epithelium or a multi-row, highly prismatic epithelium . The cavity (lumen) of the glands contains prostatic concrete , concentrated, layered secretion.
The glandular epithelium is made up of three cell types: the most common are basal and luminal secretory cells that express different keratin subtypes and can thus be distinguished. Luminal cells are also characterized by the expression of prostate-specific antigen and androgen receptors . The third type of neuroendocrine cells, which can be identified using the neuron-specific enolase and various neuropeptides produced by them, is much less common . Stem cells in the basal cell layer are believed to be the precursors of all these cell types.
Between the glands are smooth muscle cells , which contract during ejaculation and thus expel the secretion, and connective tissue with elastic fibers , the so-called Stroma myelasticum prostatae .
On the outside, the prostate is enclosed by a connective tissue capsule, the capsula prostatica .
physiology
The prostate produces some of the seminal fluid that is expelled during ejaculation . This secretion , together with the sperm cells from the testes , the secretion of the seminal vesicle ( vesicula seminalis ) and the secretion of the bulbourethral gland, form the sperm . The function of the prostate is regulated by the hormone testosterone .
The secretion of the prostate is slightly acidic (pH value around 6.4), thin and cloudy and gives the sperm its characteristic odor. The secretion contains numerous enzymes that the sperm need for fertilization.
The polyamine spermine promotes the mobility and fertility of the sperm cells. The prostate secretion also contains phosphatase , citric acid , cholesterol and zinc .
As corpora amylacea or Prostatakörperchen admixtures are of prostatic fluid in the urine sediment called.
Ontogenetic development
The epithelium (covering tissue) that surrounds the urethra is of endodermal origin. In contrast, the connective tissue and the smooth muscles that surround it are of mesodermal origin. The epithelium begins to proliferate (multiply) towards the end of the third month of pregnancy and invades the surrounding tissue. The resulting buds form the prostate in men under the influence of the male sex hormones testosterone and dihydrotestosterone (DHT), and in the absence of these hormones (among other things in women) the paraurethral gland .
Investigation methods
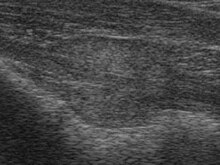
The possibilities of examining the prostate have become quite diverse, but one of the main questions, namely whether the prostate is affected by a malignant tumor or not, can still only be answered with uncertainty , at least with non-invasive methods such as ultrasound or computed tomography . The older man's prostate is prone to lump formation and it is difficult to distinguish benign from malignant nodules using non-invasive methods. The elastography is a new imaging technique, show the tumor areas and remove specific tissue samples. The so-called HistoScanning is also a new, likewise ultrasound-based method for the detection of tumor areas in order to enable a more targeted prostate biopsy. So far, however, this procedure is only available at a few clinics in Germany.
The prostate can be felt rectally with a finger . Ultrasound, magnetic resonance tomography (MRT) and computed tomography (CT) have been used as imaging methods . As a specific imaging technique for the diagnosis of prostate cancer is the positron emission tomography (PET) available, for example with 18 F-choline as a radioactively labeled substance ( tracer ), an ammonium compound with the radioactive fluorine isotope 18 F . If changes are suspected, a biopsy of the prostate gland with a so-called prostate punch can be performed. With elastography, cancer tissue can be differentiated from normal tissue because of its different hardness, so that tissue samples can be taken specifically. The HistoScanning does not measure the elasticity of the tissue, but rather scans the tissue and uses a large prostate tissue database by comparing the data with the ultrasound data and the database with the help of a computer. Structures suspected of being cancerous are color-coded and thus enable a targeted puncture during the biopsy.
For further diagnosis, laboratory values such as the prostate-specific antigen (PSA, increased in all diseases of the prostate - but also, sometimes for several days, after every mechanical stress in the pelvic area, for example through sport, e.g. cycling, sex or medical measures such as digital rectal Examination (DRU), transrectal prostate ultrasound , or urinary catheter ), the activity of acid prostate phosphatase (increased in prostate cancer) and general inflammation markers such as CRP and white blood cell count can be used. In addition, one is protein patterns diagnostic of urine available.
Examinations for the early detection of prostate cancer are not a service of the statutory health insurance companies. However, many medical practices offer them as an individual health service (IGeL). Because of the uncertain results, the unnecessary uncertainty of the patient and the risk of overdiagnosis and overtreatment, the relevant medical societies expressly do not recommend examinations for early diagnosis, but only inform the patient - with advantages and disadvantages - that such examinations are possible. For general practitioners , it is even recommended that doctors do not address this option of their own accord, but only when a patient expresses a corresponding request.
Diseases
As prostatitis refers to a inflammation of the prostate. The benign prostatic hyperplasia (BPH) is a benign enlargement of the prostate, often to a urine flow disturbance to a life-threatening bladder closure may result. Prostate cancer is called a malignant tumor of the prostate. It is the most common malignancy and, after lung and colon cancer, the third most common cause of cancer-related death in men in Germany. While BPH usually affects the central (paraurethral) organ zone, prostate cancer usually starts from the peripheral glandular parts. Both diseases are typically ailments of old age.
The male G-spot
The place in the rectum from which the prostate can be felt is also considered a male G-spot . Sexual stimulation can induce an orgasm that differs significantly from a phallic orgasm (see also prostate massage ). This difference in men is comparable to the difference between vaginal and clitoral orgasms in women. However, just like the G-spot in women, the prostate in men only becomes active as an erogenous zone once a certain degree of arousal has been reached .
Research history
See also the main article on urology .
The first anatomical description of the prostate was made 300 BC by Herophilos of Chalcedon . It was he who gave it the name The Foregoing . For a long time this was the only description. An anatomically more precise description was first written in 1536 by the Italian anatomist Niccolò Massa . Andreas Vesalius ' work Tabulae anatomicae from 1538 first contained illustrations showing the prostate as part of the male urogenital system. This was followed by more precise anatomical and physiological descriptions of the prostate. Ambroise Paré assumed that it consists of two parts, but otherwise made precise statements about its location in relation to the ejaculatory ducts and their role in ejaculation. The normal anatomy was first described by Reinier de Graaf in 1668.
Giovanni Battista Morgagni described in 1761 in his book De causis et sedibus morborum by anatomist indagatis the prostate . The first complete removal of the prostate ( prostatectomy ) for the treatment of prostate carcinoma was carried out in 1889 by Vincenz Czerny in Heidelberg . While he chose the route over the dam , Fuller performed it for the first time in 1898 via an abdominal incision. These interventions established the beginning of prostate surgery. The first prostatectomy in France was carried out by the surgeon Antoine Gosset (1872–1944).
literature
- Detlev Drenckhahn, Wolfgang Zenker: Benninghoff. Anatomy. Urban & Schwarzenberg, Munich 1994, ISBN 3-541-00255-7 .
- Uwe Gille: urinary and sexual system, urogenital apparatus. In: Franz-Viktor Salomon et al. (Ed.): Anatomy for veterinary medicine. 2nd Edition. Enke-Verlag, Stuttgart 2008, ISBN 978-3-8304-1075-1 , pp. 389-403.
- Robert Koch Institute : Prostate Diseases - GBE issue 36 in the federal health reporting series . January 2007 (also as PDF file)
- Haag, Hanhart, Müller: Gynecology and urology for study and practice. 2008/09. Medicine Publishing and Information Services, Breisach am Rhein 2008, ISBN 978-3-929851-73-1 .
Web links
- Prostate anatomy
- Anatomy and physiology of the prostate from the online urology textbook for doctors and healthcare professionals
- Info from the DKFZ
Individual evidence
- ^ H. Nguyen et al .: Normal Human Ejaculatory Duct Anatomy: A Study of Cadaveric and Surgical Specimens. In: The Journal of Urology . Volume 155, No. 5, pp. 1639-1642.
- ^ A b Theodor Heinrich Schiebler: Anatomy: histology, history of development, macroscopic and microscopic anatomy, topography . Springer, 9th edition 2005, ISBN 978-3-540-21966-8 , p. 624.
- ↑ S3 guideline for prostate cancer: early detection, diagnosis and therapy of the various stages of the German Society for Urology (DGU). In: AWMF online (as of 2018)
- ↑ Epidemiology of Prostate Cancer at www.urologielehrbuch.de
- ↑ History of Urology - From the Origins to the Renaissance ( Memento of February 6, 2010 in the Internet Archive )
- ↑ Barbara I. Tshisuaka: Gosset, Antoine Louis Charles Sébastien. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 504 f.