Cardiopulmonary resuscitation
The cardiopulmonary resuscitation or CPR to a respiratory and cardiac arrest stop and the imminent death avert the person concerned. Other names for this are resuscitation , resuscitation and English cardiopulmonary resuscitation (CPR) . In the event of a cardiac arrest, it is essential to act quickly: after just three minutes, the brain is no longer supplied with enough oxygen , so that irreversible damage can occur there.
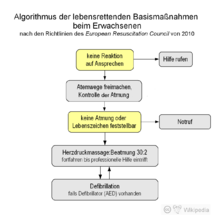
With chest compressions , the residual oxygen can circulate in the blood and thus the probability of survival can be increased significantly until the rescue service or specialist help arrives. Even without first aid knowledge , it is possible for the medical layperson to save or at least prolong life by means of the basic measures ( basic life support ). He should check whether the person is still breathing, call the ambulance service on the Europe-wide emergency number 112 and, in the case of adults, firmly and 100 to 120 times per minute press the sternum in the middle of the chest about five centimeters and not stop until help arrives. The ventilator is not the most important measure in people with sudden cardiovascular arrest. Cardiac massage is central. If possible, it should be supplemented by ventilation (e.g. mouth-to-mouth resuscitation ). The following rhythm is recommended: press 30 times and then ventilate twice.
If available nearby, an automated external defibrillator (AED) can also be used. Extended measures ( advanced life support ) require specially trained personnel with the appropriate aids or equipment and are carried out by employees of the rescue service, an emergency doctor or medical specialists in the hospital. The administration of medication , intubation , professional defibrillation and external (transcutaneous) pacemakers are used. Nevertheless, the prognosis of resuscitated patients is poor, the longer-term survival rate (time of hospital discharge) is between two and seven percent.
This article is based on the resuscitation guidelines of the European Resuscitation Council (ERC) from 2010. The practical implementation differs in different countries, medical institutions and aid organizations.
Causes and forms of cardiac arrest
The most common cause of cardiac arrest in western industrialized nations is sudden cardiac death with over 80% , caused by a heart attack or cardiac arrhythmia . In Germany 80,000 to 100,000 people die every year from sudden cardiac death, which corresponds to 250 cases per day. Other internal diseases such as lung diseases (e.g. pulmonary embolism ), diseases of the brain (e.g. stroke ) and others make up about 9%. In a further 9%, external influences such as accidents , suffocation , poisoning , drowning , suicide or electrical accidents are the cause of the cardiac arrest.
The distinction between hyperdynamic (shockable, electrically active, hypersystolic) and hypodynamic (non-shockable, electrically inactive, asystolic) cardiac arrests is particularly important for the measures of extended therapy . In the hyperdynamic form that is present in approximately 25% of cases in locating the patient, show muscle and conduction system of the heart activity, but which is disordered. There is no coordinated work of the heart and therefore no significant ejection of blood into the circulation. Pulseless ventricular tachycardia ( ventricular tachycardia, VT), ventricular flutter and ventricular fibrillation ( ventricular fibrillation, VF) are possible causes of this type of cardiac arrest. After a few minutes, it inevitably changes to the hypodynamic form in which no electrical activity can be detected and which is known as asystole . A special form is the electromechanical decoupling (EMD, PEA), in which an orderly electrical activity is observed, but this no longer causes ejection in the form of a pulse wave .
The data on the frequency of resuscitation measures in cardiac arrest are incomplete. The annual incidence of resuscitation in out-of-hospital cardiac arrest was between 50 and 66 per 100,000 inhabitants in a Scottish study. The rate of in-hospital cases varies from 150 (Norway) to 350 (England) per 100,000 enrolled patients.
Basic measures of resuscitation
The basic measures, which can be used without additional aids, also known as basic life support (BLS) in international terminology , serve to maintain a minimal circulation in the patient's body by means of cardiac massage and supply of sufficiently oxygenated blood through mouth-to-mouth resuscitation or oral resuscitation. to-nose ventilation (see respiratory donation ) until normal blood circulation is restored or to bridge the time until the use of extended therapeutic measures without irreversibly damaging the patient's vital organs. This mainly affects the brain , which is damaged by a lack of oxygen after just a few minutes. The blood flow that can be achieved through the basic measures corresponds at best to about a third of the healthy circulation. The basic measures can be carried out by one or two helpers. The ratio of chest compressions to ventilation is independent of this.
As a rule of thumb, an ABC scheme ( ABC basic measures , ABC of first aid ) for emergency life-saving measures was developed:
- A (clear airways and keep them free)
- B (ventilation or ventilation)
- C ( Circulation , in English, get going, especially with chest compressions ).
The basic measures (also in the context of first aid ) can now be divided into three simple steps:
- Check: Check whether the unconscious person reacts (e.g. by shaking the shoulder ), Check breathing : No or no normal breathing (e.g. gasping, gasping)?
- Call: Call for help - involve bystanders and make or initiate an emergency call
- Press: Press firmly and quickly (100 to 120 times per minute) in the middle of the chest (e.g. to the beat of Stayin 'Alive by the Bee Gees )
If possible, mouth-to-mouth resuscitation or mouth-to-nose resuscitation should be used: press 30 times and then ventilate twice. With chest compressions, the residual oxygen can circulate in the blood and supply the brain with oxygen . Until it is taken over by the rescue service, the probability of survival can be increased significantly. After three minutes, the brain is no longer supplied with enough oxygen - irreversible damage occurs.
Semi-automatic defibrillators ( automated external defibrillator , AED) specially designed for use by first aiders are also increasingly available at central locations in public buildings . These guide the untrained user through the defibrillation with voice instructions and in some cases also give instructions on how to perform chest compressions and ventilation. The automated defibrillation, originally an extended measure of professional helpers, is now counted among the basic measures of resuscitation. However, the use of AEDs is not a mandatory part of chest compressions; on the contrary, it must not delay or even replace the performance of chest compressions.
One of the basic measures for the first aider is also to call the emergency services immediately by means of an emergency call . This carries out the basic measures in the same way, but technical aids such as a defibrillator are available. In addition, extended measures to secure the airways and thus ensure ventilation are used. Oxygen can be made available to the patient in high concentration, for example, by means of a ventilation bag or a ventilator via an endotracheal or laryngeal tube . The same applies to resuscitation in medical facilities, which is often performed by "resuscitation teams".
Anyone who finds a motionless person is obliged to start immediately with life-saving emergency measures to the best of their knowledge, as otherwise they could be guilty of failure to provide assistance in Germany . Exceptions are bodies which already show clear signs of death such as strong signs of decomposition or injuries that are incompatible with life. Once started, the cardiopulmonary resuscitation must be continued without interruption until help is received (not just until the "arrival"!). Certain criteria (e.g. age, duration of cardiac arrest, prognosis of the underlying disorder) decide whether to interrupt the measures ) a doctor. This does not apply to not taking up or interrupting the measures if there is a risk to oneself, e.g. B. from health problems.
Recognizing a cardiac arrest, clearing the airways

|

|
| blocked airways | free airways |
| Airways on the head cut model of an adult, left before, right after hyperextension of the neck | |
To detect cardiac arrest , the patient's vital signs, consciousness and breathing are checked (also known as a diagnostic block ). A check of the circulatory activity is not necessary for lay helpers, since there is usually no circulation in the case of respiratory arrest and the check cannot be carried out safely for an inexperienced person. Taking into account their own safety, the helper checks the patient's reaction by speaking and shaking the shoulder. In some cases, pinching the arm or the like is more suitable than shaking the shoulder so that any damage to the spine etc. is not aggravated.
With the patient lying in a neutral head position , the tongue falls back into the pharynx and obstructs the airways . In order to be able to check the breathing or ventilation, the head or the neck must therefore be overstretched ( life-saving handle ). In order to protect the possibly injured (cervical) spine , this should be done by moving the chin and forehead , but not by grasping the neck . With the life-saving handle (see also Esmarch handle ), the person concerned may start breathing again.
The breathing activity is then checked by listening to the breathing noise, feeling the exhaled air against your own cheek and observing the breathing movements of the chest . If the patient is not breathing "normal", the first aider begins with the basic resuscitation measures. In layman resuscitation it happens that by mistake the gasping is perceived as non-threatening condition.
A breathing patient is brought into the stable lateral position. If there is a suspicion that foreign bodies (leftover food, dentures, chewing gum, etc.) are obstructing the airways, resuscitation is started in the unconscious without delaying the attempt to remove the foreign body. A few chest compressions during resuscitation can then remove the foreign body from the airway. Removable dentures are removed beforehand.
If a patient is still conscious with foreign bodies in the airways, an attempt is made to remove them first with cough-inducing, strong blows between the shoulder blades, then by repeated pressure on the upper abdomen ( Heimlich handle ). The Heimlich handle was no longer recommended in 2005 due to the risk of injury to the liver and spleen.
Medical personnel carry out the vital functions check with more detailed measures. Before checking the breathing , the oral cavity is also inspected for the presence of foreign bodies or vomit. These will be removed if necessary. This can be done with the help of your fingers , a suction pump or Magill forceps . After checking the breathing, a circulatory check is also carried out. In addition to observing general signs of life ( movement , breathing or coughing ), trained personnel also feel the carotid or femoral pulse . However, this can be difficult even for the most experienced. When an EKG / defibrillator device arrives, the heart rhythm is analyzed electrocardiographically. The measures to be introduced do not differ significantly from those carried out by laypeople.
Chest compressions
In the (external or extrathoracic) cardiac massage (repeated chest compression ) is the heart by pressure on the sternum pressed towards the spine. The pressure in the chest increases and blood is ejected from the heart into the circulation. In the next phase of relief, the heart fills again with blood. Both the compression of the heart by the pressure exerted from the outside and the pressure fluctuations inside the chest (“thorax pump mechanism”) caused by it were considered to be the cause of the effect of chest compressions. It is important to minimize interruptions (“no-flow time”) during chest compressions.
As a preparatory measure, the patient is laid flat on his back on a hard surface such as the floor or a resuscitation board and his chest is cleared. The pressure point is in the middle of the chest on the sternum.
For adults, the following applies: The breastbone is pressed down briefly and forcefully 30 times in a row and then ventilated twice. The depth of the impression is about four to six centimeters. The chest should be completely relieved between two pumps so that the heart can fill up with blood again. The desired frequency of chest compressions is at least 100 and a maximum of 120 compressions per minute. Correct posture makes work easier for the helper. He kneels upright next to the patient with his shoulders perpendicular to the patient's sternum. The helper presses rhythmically with the weight of his upper body while his arms are stretched and the elbows are pushed through. It is important to completely relieve the chest after each compression so that the heart muscle can fill up again sufficiently. Since the 1990s, devices with frequency and strength-controlled pistons have also been increasingly used as mechanical resuscitation aids for chest compressions . In babies and toddlers, the compression depth is around a third of the depth of the chest and only the fingertips are used for compression (for details see #Special features of newborns, babies and children ). If more than one helper is available, chest compressions and ventilation can be split between two people.
Chest compressions often lead to broken ribs , even if done correctly . These are to be accepted as a side effect and do not pose any further-reaching dangers for the patient. Therefore, chest compressions should be continued even after one or more rib fractures after checking the technique used.
Ventilation
Ventilation without further aids is provided as mouth-to-nose or mouth-to-mouth ventilation (see respiratory donation ). The affected person's neck is hyperextended. The nose must be closed for mouth-to-mouth resuscitation, the mouth for mouth-to-nose resuscitation. The correct volume is selected when the rib cage rises visibly. The ventilation phase should last about one second; Ventilation is repeated (as long as both can not take place in parallel or uninterruptedly as after the trachea has been intubated , alternating with cardiac massage and a ratio of ventilation to chest compression of 2:30) until the ventilated person breathes on their own again. In order to improve hygiene and overcome any disgust that may be present, there are various ventilation aids such as ventilation foils with a filter and various types of pocket masks, but their use requires practice. If there is a suspicion of poisoning with contact poisons (for example pesticides such as parathion ), donor breathing should be avoided. If a rescuer is not confident about ventilation, uninterrupted chest compressions are an acceptable alternative for them.
Appropriately equipped and trained helpers use a resuscitator with a face mask for ventilation , often in connection with a Guedel tube , laryngeal tube or after (endotracheal) intubation . The breathing air can also be enriched with oxygen , whereby concentrations of almost 100% can be achieved by setting the oxygen flow accordingly (maximum flow) and using an oxygen reservoir.
Advanced resuscitation measures
Extended measures should be available no later than ten minutes after the basic measures have been carried out. The aim of the extended measures, also known as advanced life support ( ALS , term of the European Resuscitation Council ) or advanced cardiac life support (ACLS, term of the American Heart Association ), is to restore the patient's physiological heart rhythm. These include securing the airway by means of intubation , creating a venous access for the administration of fluids and medication, basic drug therapy and the therapy of reversible causes of cardiac arrest. Diagnostics as part of the extended measures include EKG monitoring and checking the circulatory function, in particular through pulse controls. In therapy, as already described, a distinction is made between shockable and non-shockable forms of the circulation. With a shockable rhythm, usually ventricular fibrillation, the rapid use of a defibrillator has top priority; If necessary (with a slow basic rhythm ), a (transthoracic or external) pacemaker therapy with appropriate adhesive electrodes is also useful. The administration of antiarrhythmic drugs is also possible.
The procedure of the measures is described in the guidelines of the ERC as an algorithm , which enables a standardized and uniform implementation.
Defibrillation and pacemaker therapy
Defibrillation is the treatment of choice for ventricular fibrillation, ventricular flutter, and pulseless ventricular tachycardia, but not indicated for asystole. For defibrillators with a monophasic pulse, a shock of 360 joules is applied, for those with a biphasic shock course 150–200 joules for the first, 200–360 for all subsequent shocks. This current surge can break through the disordered electrical activity of the heart muscle and enable a restart with a regular rhythm. Immediately after each defibrillation, chest compressions and ventilation at a ratio of 30: 2 are continued for two minutes. Only then is the rhythm and pulse checked again, because if the defibrillation has successfully restored the heart rhythm, the initial ejection rate is too low to ensure adequate perfusion. In the case of pulseless electrical activity or asystole with P-waves in the ECG, the use of a transcutaneous pacemaker can be considered.
A development in recent years is the increasing use of automated defibrillators in public places. These automated external defibrillators (AED) have automated rhythm detection and, by means of acoustic instructions, also enable first aiders to perform a defibrillation. The device independently diagnoses the problem and gives the user precise instructions. If defibrillation is necessary, the helper only needs to press the release button following the announcement.
Airway management
The endotracheal intubation is considered the gold standard in the airway management in the context of resuscitation. A tube is pushed through the mouth or nose between the vocal folds of the larynx and into the windpipe (trachea). The advantages of intubation are protection against aspiration of gastric contents and the option of controlled manual or mechanical ventilation. Since endotracheal intubation is more difficult, the guidelines state that only trained and experienced helpers should use this method. The use of a laryngeal tube , combitubus or laryngeal mask is recommended as an alternative .
Cardiopulmonary resuscitation should not be interrupted or only briefly interrupted for intubation. An attempt at intubation should not last longer than 10 seconds. The correct position of the tube must be checked clinically (e.g. breathing sounds over the lungs) or by detecting CO 2 ( capnometry ) in the exhaled air. After successful intubation, chest compressions are performed continuously and ventilation is continued at a frequency of 10 / min.
Medication
Apart from oxygen, medication is preferably administered intravenously , as this access is quick and safe. An alternative is administration via an intraosseous access by puncturing the bone marrow, which is often used in young children. Administration of medication through the tube (endobronchial application) is generally not recommended, as safe absorption is not guaranteed and the plasma level of the medication cannot be predicted. An intracardiac administration directly into the heart is no longer carried out.
Adrenaline is the standard resuscitation drug. It is given because of its α-adrenergic vasoconstrictor properties, which lead to a narrowing of the peripheral blood vessels, which improves the blood flow to the heart and brain by increasing the peripheral resistance (in adults 1 mg, in children 10 µg / kg, every three to five minutes). The hopes that have been placed in vasopressin, which is also vasoconstricting, as an alternative to adrenaline have not been fulfilled. Several large randomized studies could not demonstrate any survival benefit from the administration of vasopressin; the administration is no longer recommended in the European guidelines.
If ventricular fibrillation or ventricular tachycardia persists and defibrillation occurs three times, the antiarrhythmic amiodarone (300 mg in adults) is often given. It has replaced the previously common lidocaine in the recommendations. A study published on May 5, 2016 in the New England Journal of Medicine came to the result that amiodarone is also ineffective in ventricular fibrillation.
The resuscitation guidelines, which were updated in 2010, no longer recommend the administration of atropine in the event of asystole or pulseless electrical activity , as an advantage of blocking the parasympathetic nervous system ( parasympatheticolysis ) could not be proven.
The previously practiced "buffering" of an acidosis caused by reduced blood flow and reduced carbon dioxide elimination ( acidosis , which can reduce the effectiveness of the catecholamines used in resuscitation) of the circulatory system in the context of cardiac arrest with sodium bicarbonate is no longer justified. The infusion of sodium bicarbonate produces CO 2 , which diffuses into the cells, worsening intracellular acidosis - that is, has the opposite effect. For this reason, sodium bicarbonate is only recommended for out-of-hospital resuscitation in the context of severe hyperkalemia and intoxication with low-dose tricyclic antidepressants .
In the case of special arrhythmias, the administration of magnesium sulfate can also be considered. Insufficient data are available on the use of a thrombolytic in suspected myocardial infarction; however, it should be considered if pulmonary embolism is suspected .
Causal treatment
In addition to the resuscitation measures, which are symptomatic therapy , attempts must also be made to diagnose the reversible causes of the cardiac arrest and to treat the cause ( causal therapy ). The reversible causes include insufficient oxygen supply to the patient ( hypoxia ), a lack of blood volume ( hypovolemia or hypovolemic shock ), hypothermia ( hypothermia ) and metabolic disorders, especially too much or too little potassium ( hyperkalaemia or hypokalaemia ) in the blood. Other causes that can be treated at short notice in the context of resuscitation include pericardial tamponade , poisoning (intoxication), thromboembolism (coronary or pulmonary vessels) and tension pneumothorax .
Possible measures derived from this include the use of thrombolytics in the event of a heart attack or a pulmonary embolism, the treatment of acute blood loss through infusion therapy , the correction of electrolyte disorders , the warming up of hypothermic patients , the administration of antidotes in the event of poisoning , the relief of tension pneumothorax as well as the therapy of other special clinical pictures such as acute obstructive airways diseases ( asthma attacks ) or anaphylaxis . The measures will be continued in the post-reanimation phase (see below).
Special features in newborns, infants and children
Children are not little adults; therefore, there are a few special features to consider during resuscitation. A distinction is made between newborns (children up to 28 days of age), infants (up to about 12 months) and older children (from about 12 months to puberty , with children from the age of nine being treated like adults).
While circulatory arrests are mostly cardiac-related in adults, in infants and children a breathing disorder is often the cause of a threatening slowdown in the heartbeat (even at a heart rate of less than 60 per minute) and cardiac arrest ("secondary cardiac arrest"). For this reason, children are given five initial breaths in a row before starting chest compressions. Another special feature is that the head is not overstretched for ventilation, especially with infants, but is left almost in the neutral position ("sniffing position"). Because of the size of the patient, ventilation is given in newborns (with possibly not yet fully expanded lungs) and infants through the mouth and nose at the same time (mouth to mouth and nose).
Only the heel of the hand is used to perform chest compressions on children. For babies, use two fingers or grasp the chest with both hands and press it in with your thumbs (if two helpers work together). The pressure depth should be about 1/3 of the chest diameter. The sequence after the five initial breaths for the first aider - as with adults - is 30 chest compressions for two breaths; A pressure ratio of 15: 2 applies for medical personnel if several helpers are present. A ratio of 3: 1 is used for newborns who also need to be protected from heat loss.
In principle, cardiopulmonary resuscitation is carried out in the same way as for adults and is only adapted to the physique of children and babies. In case of doubt, the procedure for adults should be followed, since, as the guidelines expressly emphasize, starting measures early is more important than carrying them out according to age.
When using an automatic external defibrillator (AED), pediatric electrodes should be used whenever possible. An AED should not be used in children under 1 year of age. Extended measures are adapted to suit the implementation in adults. As it is often difficult to find venous access in children, an intraosseous puncture is an alternative .
Post-reanimation phase
The care phase after successful resuscitation ( post-resuscitation care ) begins with the re-establishment of a spontaneous circulation ( return of spontaneous circulation , ROSC ). It includes further preclinical stabilization, transport to a suitable center and extended intensive care treatment and monitoring. The measures in this phase have a significant impact on the prognosis.
In this phase, the focus is on causal therapy measures such as B. reperfusion therapy after a heart attack or surgical treatment of injuries. In addition, the symptomatic treatment of respiratory and cardiovascular function takes place in order to ensure an adequate supply of oxygen, especially for the brain. This may require ventilation therapy under sedation , pacemaker therapy and the diverse use of drugs, including a. to ensure sufficient blood pressure to supply the organs with catecholamines or to treat cramps and myoclonus. In addition, other important body parameters are monitored and disorders treated if necessary. Among other things, blood sugar can be emphasized here, as a correct setting represents an important survival advantage regardless of the underlying disease.
To reduce cerebral damage, in 2010, unconscious adults with survived resuscitation were recommended to cool down to 32–34 ° C for 12 to 24 hours ( mild therapeutic hypothermia , MTH). This procedure, which is included in the international guidelines for resuscitation of adult patients, contributes to increasing the survival rate and improving the neurological condition after successful resuscitation and should be initiated as soon as possible. An evaluation of the INTCAR database ( international cardiac arrest registry ) from Sendelbach showed in 2012:
- Every five minute delay in initiating mild therapeutic hypothermia means an increase in the poor neurological outcome of 8%.
- A 30-minute delay in reaching the target temperature of 32 to 34 ° C increases the rate of poor neurological outcome by 17%.
- On average, clinics need 94 minutes to initiate MTH and 309 minutes to reach the target temperature.
Achieving an oxygen saturation greater than 96% does not seem to be indicated, since hyperoxemia in the post-reanimation phase generates oxidative stress and can thus damage neurons post-ischemically. Animal experiments have shown that the neurological outcome improves if, in the first hour after ROSC, the oxygen administration is aimed at a target oxygen saturation of 94–96%, i.e. the patient is reoxygenated in a controlled manner.
If the patients have to be artificially ventilated for a longer period (> 5 days), artificial feeding via the gastrointestinal tract or venous means makes sense.
forecast
Survival rates from cardiac arrest depend on many factors. The underlying cause, age and previous illnesses of the person affected as well as the point in time until the initiation of resuscitation measures are among other things decisive for this rate, which is why general statements about the prognosis are difficult. The long-term prognosis after a primarily successful resuscitation is determined by the underlying disease.
Of the human organs, the nerve cells in the brain are the most sensitive to a lack of oxygen. As early as three minutes after the cardiac arrest has started, there is a risk of permanent brain damage. Therefore, in addition to survival, the neurological sequelae are another important aspect of resuscitation. A large number of patients who have survived cardiac arrest suffer such damage. Predictions about neurological damage after surviving cardiac arrest are difficult to make. There are no reliable diagnostic procedures. With limitations, a high serum concentration of neuron-specific enolase (NSE) and the S-100 proteins indicate a poorer outcome.
The time it takes for resuscitation to begin is the most important of the factors influencing prognosis. For every minute that elapses before cardiopulmonary resuscitation begins, the patient's probability of survival is reduced by about 10%. With chest compressions with ventilation and defibrillation, survival rates of 50–75% are possible within the first three to five minutes without permanent cell damage, which then drop sharply - after four minutes to below 30%. Irrevocable cell damage and thus biological death do not occur until five minutes (or longer in the case of hypothermia) after so-called clinical death . Since in European countries the deadline for the arrival of the ambulance service is usually eight minutes or more, the measures taken by laypeople present are decisive for the patient's survival. A quick start of basic measures with a quick emergency call and extended measures, in particular early defibrillation, double to triple the overall survival rate, in adults and children.
The cause of cardiac arrest is an important prognostic factor. In a study of over 21,000 out-of-hospital cardiac arrest cases in Scotland from 1991–1998, approximately four-fifths were cardiac cause; Of these, around 7% survived until they were discharged, and 6% were still alive a year later. In contrast, the survival rate was approximately 2% for the remaining fifth non-cardiac cause. Resuscitation from cardiac arrest caused by trauma has a particularly poor success rate. The vast majority of survivors in this group suffered brain damage (> 98%). The prognosis for hypothermia and drowning accidents is better.
Ethical, legal and psychological aspects
- “ There remains a widespread divergence of views on ethical aspects of resuscitation with the countries of Europe that are largely unpredictable according to commonly perceived national characteristics. [...] For many ethical questions there can be no clear and correct didactic answers. ”
- (Many ethical aspects of resuscitation have a wide range of perspectives in Europe, most of which cannot be explained by supposed national peculiarities. [...] Therefore, there are no clear and correct answers to many ethical questions.)
In the event of a cardiac arrest, the question of the meaning of resuscitation measures and their termination inevitably arises. These decisions are influenced by individual, international and local cultural, legal, traditional, religious, social and economic factors. Along with many other questions, it is a topic of medical ethics and ethics in general.
The attending physician is bound by an advance directive , in which the omission of resuscitation measures can be formulated, in order to take patient autonomy into account . Such expressions of will by a patient are usually taken into account if the living will is known and contains instructions for the actual situation. In the preclinical area, however, an examination is often difficult or even impossible under the time pressure of the situation, so that resuscitation is started despite an order. There are considerable international deviations in the attitude of medical staff to written advance directives. The same also applies to statutory regulations on the binding nature of such living wills.
In addition to the start of resuscitation measures, their termination is also controversially discussed. Clear signs that correlate with a possible success or failure of resuscitation have so far not been clearly proven in any study. If the therapeutic options are exhausted, unsuccessful resuscitation lasts for a long time, or if there is no prospect of acceptable survival, the attending physician can end the measures. There can be no general decision-making rules for this passive euthanasia, which is legal in most countries, when the measures are discontinued or when treatment is terminated in the persistent vegetative state after resuscitation. In the Anglo-Saxon-speaking countries in particular, the decision to refrain from resuscitation or to terminate resuscitation is made by non-medical staff. This approach is strictly rejected in other countries.
There are very different perspectives on the question of research and training for the recently deceased. This is rejected in particular in the Islamic culture, but increasingly also in Western countries, especially in the USA. Various professional societies see the future of research in this area at risk from the increasingly strict legislation in many countries.
The concept of family presence during resuscitation emerged in the 1980s. Various research shows that it can help cope with this stressful event. This approach is in the process of becoming accepted practice in many European countries. An important development is the support of traumatized relatives after unsuccessful resuscitation by crisis intervention teams .
Resuscitation is also a psychologically stressful mission for doctors and rescue workers. This particularly applies to the resuscitation of children. A possible consequence in these professional groups is the development of post-traumatic stress disorders and burnout syndrome . In parallel to crisis intervention with relatives, there are methods available for the helpers to cope with particularly traumatizing experiences, which are called Critical Incident Stress Management (CISM) or stress handling after stressful events (SbE).
Professional societies and guidelines
Specialized societies such as the American Heart Association (AHA), the European Resuscitation Council and the International Liaison Committee on Resuscitation (ILCOR) regularly publish joint guidelines for performing resuscitation based on current scientific knowledge. The current guidelines are from 2010, which have been adopted to varying degrees by the medical associations of individual countries and implemented by aid organizations , hospitals and other institutions with a delay and often with differences. In 2015 the ERC updated its guidelines.
In Germany, the aid organizations represented in the Federal First Aid Working Group (BAGEH) and the “German Advisory Board for First Aid and Resuscitation at the German Medical Association” agreed on a national consensus in 2002, which was based on the previous version of the resuscitation guidelines from 2000. In March 2006 the German Medical Association published key points for an update based on the ERC guidelines from 2005. In Austria and Switzerland, the medical organizations and the organizations that carry out the rescue service and general training in first aid have agreed to apply the ERC guidelines.
In order to enable a scientific comparison of resuscitation worldwide, the leading associations created a uniform data set in the mid-1990s with the establishment of the Utstein Style Protocol. Numerous publications on resuscitation processes are based on this. In Germany, the German Society for Anaesthesiology and Intensive Care Medicine (DGAI) has been setting up a nationwide resuscitation register since 2003 .
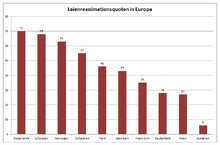
Since 2012 anesthetists in Germany, represented by the DGAI, the professional association of German anesthetists e. V., the German Resuscitation Council and the German Anesthesiology Foundation, supported by the Federal Ministry of Health , with their campaign “Save a life. 100 Pro Resuscitation “the increase in the rate of resuscitation by lay people. The aim is to strengthen people's self-confidence in their own abilities as first aiders and to increase the first aid rate sustainably and in the long term. For various reasons, too few people intervene to help in an emergency : They don't know what to do or they don't apply what they have learned - mostly out of fear of doing something wrong. The data from the German Resuscitation Register show that in 2012 the willingness to resuscitate by medical laypeople in Germany was 19.8 percent. This is a low value compared to other European countries, where the willingness to provide first aid ( first aid rate ) is significantly higher. For example, the Netherlands has a rate of 70 percent, followed by Sweden (68%), Norway (63%) and the Czech Republic (55%). With the campaign, a clear improvement in first aid readiness could be achieved. The readiness for resuscitation rose to almost 28 percent in the following year. In 2019, the lay resuscitation rate in Germany was 42%.
History of the resuscitation
antiquity
Attempts have been made for centuries to bring people back to life who no longer show clear signs of life. There have been various attempts to reanimate lifeless people through loud speech, touch, breath donation and chest compression.
The origin of the respiratory donation is not known, we only know that the method is very old. It is possible that the Egyptians had their first knowledge of ventilation techniques around 5,000 years ago, as evidence suggests. In the 2nd Book of Kings in the Old Testament (around 700 BC) it says:
“When Elisha came into the house, the child was dead on his bed. He went into the room, closed the door behind him and the child, and prayed to the Lord. Then he went to the bed and threw himself over the child; he put his mouth on his mouth, his eyes on his eyes, his hands on his hands. As he stretched out over the child, warmth came into his body. "
Modern times
For a long time, the teachings of Galen of Pergamon from the time of late antiquity determined the ideas of the processes in the human body. It was not until the 17th century that Galen's teaching was replaced by William Harvey's discovery of blood circulation. For the first time, this described the blood circulation and the function of the heart as a pressure pump in a coherent and coherent manner. Andreas Vesalius Galen had previously corrected errors in animal anatomy. In 1667, the London Royal Society demonstrated ventilation using the open chest of a dog and the visible ventilation of the lungs. In 1744, the surgeon Tossach performed successful mouth-to-mouth resuscitation on a miner for the first time. The French anatomist and royal personal physician Antoine Portal (1742-1832) published a description of mouth-to-mouth ventilation shortly afterwards. The importance of ventilation for resuscitation had thus been recognized, but new findings were not consistently implemented in resuscitation.
From today's perspective, there were curious recommendations for resuscitation, for example the recommendation to blow warm air into the intestines with a bellows or an enema syringe, or to blow tobacco smoke (fumigation) into the intestines. The later Grand Duke of Saxe-Weimar-Eisenach, Carl August , issued the following instructions for the revival in 1776:
“You then have to blow air into your mouth, either by means of a bellows or, which is better, in such a way that a person who has a healthy lungs puts his mouth on the mouth of the drowned person and also uses a broken pipe style or another Tube operated, but with this both the odor and tobacco smoke, someone else has to hold the drowned person's nose with one hand and stroke the chest back and forth with the other, primarily rubbing and moving from the pit of the heart to the chest. "

In the 19th century, a large number of different manual methods of donating breath using direct or indirect chest compression were tried and described, such as the Silvester method , in which ventilation is to be practiced by passive arm movements of the patient.
There were also different approaches to the question of chest compressions. The French cardiac surgeon Théodore Tuffier (1857–1929) had tried an (internal, i.e. open chest) massage for the first time. Open heart massage is only rarely used today (for example in the case of cardiac arrest with an open chest or after thoracotomy , in abdominal operations as a subdiaphragmatic heart massage through the diaphragm in the operating room or in the case of a chest trauma with open injuries). In 1904 the book Die Frau als Hausärzte by Anna Fischer-Dückelmann was published , in which instructions for an external heart massage can be found:
“Indirect heart massage: The diaphragm is influenced, as is the heart, if you push the intestines upwards with both palms of the hands and push them upwards to the left, then suddenly let them go. In this way the heart is pushed up and down, but the elevation of the diaphragm first narrows the height of the chest and, when it suddenly sinks again, expands. If there is still a spark of life, such stimuli are likely to get breathing and heartbeat going again. In the case of children who have had an accident, women can probably use this 'first aid in the event of an accident'. "
Development of modern resuscitation in the 20th century
Soviet medics experimented with resuscitation techniques on dogs by blood supply alone in the late 1930s. A promotional film by the Soviet film agency, Experiments in the revival of organisms , shown in New York in 1940 demonstrates a. a. neurological reactions of a dog skull that was cut off but supplied with blood and the supposed resuscitation of a dog after 10 minutes of cardiac arrest by an external blood supply machine.
Cardiopulmonary resuscitation has been practiced on a modern scientific basis since the 1950s. At the beginning of the 1960s, various research results led to the development of the resuscitation technique that is still valid today. In 1957, Greene succeeded in proving that the helper's exhaled air allowed sufficient gas exchange and that mouth-to-mouth ventilation was superior to the ventilation method previously used. In 1960 the effectiveness of external chest compressions was recognized, which had previously only been used as a procedure with the chest open ( William B. Kouwenhoven ).
However, the decisive step was taken by Peter Safar . The American anesthesiologist , who was born in Vienna , recognized the low success of the previous methods and was able to show that a combination of chest compressions and ventilation has higher success rates. To do this, he tested the effectiveness of his cardiopulmonary resuscitation on volunteer colleagues from his research team. Because of these research results, which form the basis of modern resuscitation techniques, Safar is often referred to as the "father of cardiopulmonary resuscitation".
At the same time, the resuscitator had been invented in the 1950s by the engineer Hesse and the doctor Ruben . To be able to practice handling the bag, the two inventors developed a doll that could be ventilated with it. The first training device was then sold to the Danish Red Cross in 1958 (Ambu-Phantom). In 1960, the device was supplemented by the functions of chest compression and mouth-to-mouth ventilation, so that the world's first "exercise phantom" was created. During a trip to Norway , Safar met the toy manufacturer Asmund Laerdal . Safar and Laerdal jointly developed the so-called Resusci-Anne . With this simple doll it became possible to train laypeople in cardiopulmonary resuscitation.
The first attempts at electroshock treatment for cardiac arrhythmias were made as early as the 1940s, initially with alternating current. At the beginning of the 1960s, the US cardiologist Bernard Lown developed defibrillation and electrical cardioversion using direct current. Such a method had been independently described in the Soviet Union as early as 1946 due to the Cold War . The further development of defibrillators finally led in the 1990s to devices that are also suitable for use by first aiders.
The basis for the resuscitation methods established at the end of the 20th century were recommendations of the American Heart Association and the European Resuscitation Council, and for Germany also the guidelines of the Resuscitation Advisory Board of the German Medical Association for performing resuscitation.
In 2012, a mobile heart-lung machine was used for resuscitation for the first time .
Current developments
In recent years, chest compressions have become more important than ventilation. For example, the ratio of chest compressions to ventilation was changed from 15: 2 to 30: 2 in order to lengthen the phase of continuous compressions.
Resuscitation concepts have been developed in which this ratio is stretched even further (approx. 100: 5) and those with continuous chest compressions with no need to donate breath, called Continuous Chest Compression (CCC) resuscitation . In individual studies, these increased the survival rate in the observed cardiac arrest with cardiac cause in adults (SOS-KANTO Study Group).
The European Resuscitation Council does not consider the data basis for an exclusive chest compressions as sufficient for a general recommendation of such an approach as standard treatment. However, only chest compressions without ventilation proved better than taking no action at all. Therefore, the current guidelines recommend that lay rescuers should at least perform chest compressions if they find themselves unable to provide ventilation.
A precordial punch , especially if cardiac arrest has been observed, is no longer generally recommended.
Automatic resuscitation devices for cardiac massage are increasingly being used pre- and in-hospital as part of professional care (advanced life support). A study carried out among rescue service personnel showed that the use of a resuscitation device was equivalent to manual chest compressions - there was no survival benefit. In another study, no higher complication rate could be determined through the use of such a device. The AHA and ERC guidelines consider the use of such devices for longer transports and for resuscitation in the cardiac catheter laboratory .
In Germany currently (as of 2019) around 80,000 resuscitations are performed outside the hospital per year, of which around 45 percent are primarily successful.
literature
- European Resuscitation Council Guidelines for Resuscitation. In: Resuscitation. Elsevier Science Ireland, Shannon 67.2005, S1, S1-S2. PMID 16321715 , ISSN 0300-9572
- German Resuscitation Council eV (Hrsg.): Reanimation 2015. Guidelines compact . Ulm 2015, ISBN 978-3-9814591-4-2 . - Current European Resuscitation Council Guidelines for Resuscitation 2015 in German.
- Focus on ERC guidelines 2005. In: Emergency & Rescue Medicine. Springer-Verlag, Berlin 2006, ISSN 1434-6222
- Assessment of the prognosis after cardiopulmonary resuscitation and therapeutic hypothermia. In: Deutsches Ärzteblatt 110 (9), 2013, pp. 137–143. doi: 10.3238 / arztebl.2013.0137
- H. L'Allemand: Revival. In: Surgery historically: beginning - development - differentiation. Edited by FX Sailer and FW Gierhake, Dustri-Verlag, Deisenhofen near Munich 1973, ISBN 3-87185-021-7 , pp. 217-228.
- Pschyrembel . Clinical Dictionary. 262nd, revised edition. 2010, ISBN 978-3-11-021152-8 .
- Walied Abdulla: Interdisciplinary Intensive Care Medicine. Urban & Fischer, Munich a. a. 1999, ISBN 3-437-41410-0 , pp. 4-22 ( cardiopulmonary resuscitation ).
- Harald Genzwürker, Jochen Hinkelbein: Case book anesthesia, intensive care medicine and emergency medicine. Georg Thieme, Stuttgart / New York 2005, ISBN 3-13-139311-4 , pp. 173–175 ( first aid for a newborn / resuscitation in children ) and 200–203 ( resuscitation for asystole ).
Historical literature (selection)
- Christian August Struve: Attempt on the art of reviving apparent deaths and on rescue in rapid mortal danger, a tabular paperback. Hanover 1797.
- Friedrich von Esmarch : The first aid in the case of sudden accidents. A guide for Samaritan schools in five lectures. Leipzig 1882; later under the title First aid in the event of sudden accidents. A guide for Samaritan schools in six lectures. ibid 1912, pp. 69-82.
- Ernst Engelhorn: The Samaritan Book. A guide for first aid in the event of an accident and for nursing in the home, especially for use in courses for women. Ferdinand Enke, Stuttgart 1909, pp. 71-82 and 97.
Web links
- Nationwide resuscitation register of the German Society for Anaesthesiology and Intensive Care Medicine V. (DGAI)
- Resuscitation guidelines of the German Council for Resuscitation
- European Resuscitation Council (ERC)
- Austrian Resuscitation Council website with complete guidelines (German)
Individual evidence
- ↑ Saving a Life. 100 per resuscitation. einlebenretten.de
- ↑ Campaign “ Saving a Life. 100 per resuscitation ". Professional Association of German Anesthetists V.
- ↑ a b campaign “Save a life. 100 per resuscitation ". German Society for Anaesthesiology and Intensive Care Medicine V.
- ↑ a b c J. P. Pell, JM Sirel, AK Marsden a. a .: Presentation, management, and outcome of out of hospital cardiopulmonary arrest: comparison by underlying aetiology . In: Heart , 89, 2003, pp. 839-842. PMID 12860852
- ↑ a b c d e f g h i R. W. Koster u. a .: European Resuscitation Council Guidelines for Resuscitation 2010 Section 2. Adult basic life support and use of automated external defibrillators. In: Resuscitation. 81 (10), Oct. 2010, pp. 1277-1292. PMID 20956051
- ↑ a b C. D. Deakin, JP Nolan, K. Sunde, RW Koster: European Resuscitation Council Guidelines for Resuscitation 2010 Section 3. Electrical therapies: Automated external defibrillators, defibrillation, cardioversion and pacing. In: Resuscitation. 81 (10), Oct. 2010, pp. 1293-1304. PMID 20956050
- ^ J. Nolan: European Resuscitation Council guidelines for resuscitation 2005. Section 1. Introduction. In: Resuscitation. 67 Suppl 1, 2005, pp. S3-S6. PMID 16321715 .
- ↑ Walied Abdulla (1999), p. 5.
- ↑ Walied Abdulla (1999), pp. 5-15.
- ↑ Walied Abdulla (1999), p. 5 f.
- ↑ Harald Genzwürker, Jochen Hinkelbein: Case book anesthesia, intensive care medicine and emergency medicine. Georg Thieme, Stuttgart / New York 2005, ISBN 3-13-139311-4 , p. 202.
- ↑ Harald Genzwürker, Jochen Hinkelbein (2005), p. 202.
- ↑ Walied Abdulla (1999), p. 13 f.
- ^ DAN Network of German Pharmacists - The Revival
- ^ A b R. W. Koster, LL Bossaert, JP Nolan, D. Zideman, on behalf of the Board of the European Resuscitation Council: Advisory statement of the European Resuscitation Council. ( Memento of April 13, 2016 in the Internet Archive ) (PDF; 52 kB). March 31, 2008.
- ↑ Walied Abdulla (1999), p. 5.
- ↑ a b c d e f g h i j k l C. D. Deakin u. a .: European Resuscitation Council Guidelines for Resuscitation 2010 Section 4. Adult advanced life support. In: Resuscitation. 81 (10), Oct 2010, pp. 1305-1352. PMID 20956049
- ↑ K. Aung, T. Htay: Vasopressin for cardiac arrest: a systematic review and meta-analysis. In: Arch Intern Med . 165 (1), 2005, pp. 17-24. PMID 15642869 .
- ^ P. Dorian, D. Cass, B. Schwartz, R. Cooper, R. Gelaznikas, A. Barr: Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. In: N Engl J Med. 346, 2002, pp. 884-890. PMID 11907287
- ↑ Peter J. Kudenchuk et al. a .: Amiodarone, Lidocaine, or Placebo in Out-of-Hospital Cardiac Arrest. In: N Engl J Med. 374, 2016, pp. 1711-1722. doi: 10.1056 / NEJMoa1514204
- ↑ a b J. Soar u. a .: European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances. In: Resuscitation. 81 (10), Oct 2010, pp. 1400-1433. PMID 20956045
- ↑ Harald Genzwürker, Jochen Hinkelbein (2005), p. 175 ( cardiopulmonary resuscitation in children ).
- ↑ KD Young, JS Seidel: Pediatric cardiopulmonary resuscitation: a collective review. In: Ann Emerg Med . 33 (2), 1999, pp. 195-205. PMID 9922416 .
- ↑ a b c D. Biarent u. a .: European Resuscitation Council Guidelines for Resuscitation 2010 Section 6. Pediatric life support. In: Resuscitation. 81 (10), Oct 2010, pp. 1364-1388. PMID 20956047 .
- ^ S. Richmond, J. Wyllie: European Resuscitation Council Guidelines for Resuscitation 2010 Section 7. Resuscitation of babies at birth. In: Resuscitation. 81 (10), Oct 2010, pp. 1389-1399. PMID 20956046 .
- ↑ A. Langhelle et al. a .: Recommended guidelines for reviewing, reporting, and conducting research on post-resuscitation care: the Utstein style. In: Resuscitation. (3), 2005, pp. 271-283. PMID 16129543 .
- ↑ German Society for Cardiology. 04/2014.
- ↑ Key points of the German Medical Association for Resuscitation 2010 ( Memento from January 1, 2015 in the Internet Archive ) (PDF)
- ↑ S. Sendelbach, MO Hearst u. a .: Effects of variation in temperature management on cerebral performance category scores in patients who received therapeutic hypothermia post cardiac arrest. In: Resuscitation. Volume 83, Number 7, July 2012, pp. 829-834, doi: 10.1016 / j.resuscitation.2011.12.026 , PMID 22230942 .
- ↑ CD Deakin et al. a .: Advanced resuscitation measures for adults ("advanced life support"). Section 4 of the European Resuscitation Council Guidelines for Resuscitation 2010. In: Emergency Rescue Med. 13, 2010, pp. 559-620.
- ↑ Guidelines for Enteral and Parenteral Nutrition. German Society for Nutritional Medicine, 2007, ISBN 978-3-13-148091-0 .
- ↑ Walied Abdulla (1999), p. 4 f.
- ↑ M. Kuisma, P. Suominen, R. Korpela: Pediatric out-of-hospital cardiac arrests: epidemiology and outcome. In: Resuscitation. Volume 30, 1995, pp. 141-150. PMID 8560103 .
- ↑ a b P. J. Baskett, A. Lim: The varying ethical attitudes towards resuscitation in Europe. In: Resuscitation. 62, 2004, pp. 267-273. PMID 15325445 .
- ^ PJ Baskett, PA Steen, L. Bossaert: European Resuscitation Council guidelines for resuscitation 2005. Section 8. The ethics of resuscitation and end-of-life decisions. In: Resuscitation. 67 Suppl 1, 2005, pp. S171-S80. PMID 16321712 .
- ↑ MJ Bonnin, PE Pepe, KT Kimball, PS Clark Jr: Distinct criteria for termination of resuscitation in the out-of-hospital setting. In: JAMA. 270, 1993, pp. 1457-1462. PMID 8204131 .
- ^ AC Naess, E. Steen, PA Steen: Ethics in treatment decisions during out-of-hospital resuscitation. In: Resuscitation. 33 (3), 1997, pp. 245-56. PMID 9044497 .
- ↑ RM Morag, S. DeSouza, PA Steen, A. Salem, M. Harris, O. Ohnstad, JT Fosen, BE Brenner: Performing procedures on the newly deceased for teaching purposes: what if we were to ask? In: Arch Intern Med. 165 (1), 2005, pp. 92-96. PMID 15642881 .
- ↑ CJ Doyle, H. Post, RE Burney, J. Maino, M. Keefe, KJ Rhee: Family participation during resuscitation: an option. In: Ann Emerg Med. (6), 1987, pp. 673-675. PMID 3578974 .
- ↑ S. Köberich: Presence of relatives during cardiopulmonary resuscitation . In: intense. 13, 2005, pp. 215-220.
- ↑ Key points of the German Medical Association for Resuscitation 2006 ( Memento of September 29, 2007 in the Internet Archive ) (PDF; 34 kB)
- ↑ AH Idris et al. a .: Utstein-style guidelines for uniform reporting of laboratory CPR research. In: Circulation. 94 (9), 1996, pp. 2324-2336. PMID 8901707 .
- ↑ Public annual report 2019 of the German Resuscitation Register. Retrieved August 3, 2020 .
- ↑ A. Ocklitz: Artificial ventilation with technical aids 5000 years ago? In: Anaesthesiologist. 45 (1), Jan 1996, pp. 19-21. PMID 8678274 .
- ↑ 2. Book of Kings, 4, 32–35 ( 2 Kings 4.32 EU )
- ↑ K. Wolff: History of Medicine. edition Medizin, pp. 8, 9 and 17.
- ↑ Barbara I. Tshisuaka: Portal, Antoine Baron. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. de Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1176.
- ^ History of modern emergency medicine . ADAC
- ↑ HR Silvester: A new method of resuscitating still-born children and of restoring persons apparently drowned or dead. In: BMJ. 2, 1858, pp. 576-579.
- ↑ Barbara I. Tshisuaka: Tuffier, Théodore. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. de Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1424.
- ↑ Anna Fischer-Dückelmann: The woman as a family doctor - a medical reference book. Süddeutsches Verlags-Institut, Munich 1922 (preface from 1901).
- ↑ Dog animation film of the Soviet Union 1940 at archive.org
- ↑ Walied Abdulla (1999), p. 5.
- ^ DG Greene, RO Bauer, CD Janney, JO Elam: Expired air resuscitation in paralyzed human subjects. In: J Appl Physiol . 11, 1957, pp. 313-318.
- ^ WB Kouwenhoven, JR Jude, GG Knickerbocker: Closed chest cardiac massage. In: JAMA. 173, 1960, pp. 1064-1067.
- ^ P. Safar, TC Brown, WJ Holtey, RJ Wilder: Ventilation and circulation with closed-chest cardiac massage in man. In: JAMA. 176, 1961, pp. 574-576. PMID 13745343 .
- ↑ The invention of the Ambu bag . , from Ambu
- ↑ CS Beck, WH Pritchard, HS Fell: Ventricular fibrillation of long duration abolished by electric shock. In: JAMA. 135, 1947, pp. 985-986.
- ↑ B. Lown, R. Amarasingham, J. Neuman: New method for terminating cardiac arrhythmias. Use of synchronized capacitor discharge. In: JAMA. 182, 1962, pp. 548-555. PMID 13931298 .
- ↑ NL Gurvich, SG Yuniev: Restoration of a regular rhythm in the mammalian fibrillating heart. In: Am Rev Sov Med. 3, 1946, p. 236.
- ↑ Walied Abdulla (1999), p. 5.
- ↑ Dennis Ballwieser : Mobile heart-lung machine: Clinic to go. In: Spiegel online. November 23, 2012.
- ^ M. Hassmann: Cardiopulmonary resuscitation with a compression-ventilation ratio of 100: 5 and 30: 2: Influence on gas exchange in the animal model. (PDF; 12 MB)
- ^ GA Ewy: Cardiocerebral resuscitation: the new cardiopulmonary resuscitation . In: Circulation . 111 (16), Apr 26, 2005, pp. 2134-2142. PMID 15851620 .
- ↑ SOS-KANTO study group: Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. In: The Lancet . 369 (9565), Mar 17, 2007, pp. 920-926. PMID 17368153
- ^ Statement ( memento of July 1, 2007 in the Internet Archive ) of the European Resuscitation Council (ERC) regarding the "Compression-only CPR study"
- ↑ SOS-KANTO Study Group: Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. In: Lancet. 369, 2007, pp. 920-926.
- ↑ T. Iwami, T. Kawamura, A. Hiraide et al. a .: Effectiveness of bystander-initiated cardiac-only resuscitation for patients with out-of-hospital cardiac arrest. In: Circulation. 116, 2007, pp. 2900-2907.
- ↑ Lars Wik, Jan-Aage Olsen, David Persse, Fritz Sterz, Michael Lozano: Manual vs. integrated automatic load-distributing band CPR with equal survival after out of hospital cardiac arrest. The randomized CIRC trial . In: Resuscitation . tape 85 , no. 6 , June 2014, ISSN 1873-1570 , p. 741-748 , doi : 10.1016 / j.resuscitation.2014.03.005 , PMID 24642406 .
- ↑ Rudolph W. Koster, Ludo F. Beenen, Van Der Boom, Esther B, Anje M. Spijkerboer: Safety of mechanical chest compression devices AutoPulse and LUCAS in cardiac arrest: a randomized clinical trial for non-inferiority . In: European Heart Journal . doi : 10.1093 / eurheartj / ehx318 ( oup.com [accessed October 7, 2017]).
- ↑ Anatol Prinzing, Stefan Eichhorn, Marcus-André Deutsch, Ruediger Lange, Markus Krane: Cardiopulmonary resuscitation using electrically driven devices: a review . In: Journal of Thoracic Disease . tape 7 , no. October 10 , 2015, ISSN 2072-1439 , p. E459 – E467 , doi : 10.3978 / j.issn.2072-1439.2015.10.40 , PMID 26623121 , PMC 4635271 (free full text).
- ↑ J. Wnent, JT Gräsner, Stephan Seewald, S. Brenner and others: Annual report of the German Resuscitation Register. In: Anaesthesiology & Intensive Care Medicine. Volume 60, 2019, pp. V91-C93.