Cannabis as an intoxicant

If parts of the female hemp plant (mostly cannabis sativa , cannabis indica or their hybrids) are consumed in such a way that they produce an intoxicating effect , cannabis is used as an intoxicant .
Colloquial names for these plant products are for example grass, weed or marijuana (for the female flowers) and hashish (for the resin extracted and pressed from it ). Extracts such as hash oil are also used as intoxicants. Possession and distribution of such cannabis products are prohibited in most countries . This is also the case in Germany, Austria and Switzerland, where cannabis, as in many other countries around the world with cannabis prohibition , is the most commonly used illegal drug .
However, not all cannabis strains are suitable as intoxicants. Because z. B. Industrial hemp varieties (but also some medicinal cannabis varieties) contain the necessary active ingredient tetrahydrocannabinol (THC) only in extremely small, imperceptible amounts. THC influences the central nervous system of humans and is primarily responsible for the muscle relaxing , calming and nausea suppressing effects. According to conservative estimates, around 192 million people (≈3.9% of the world's population) use cannabis as an intoxicant.
history

Medical history
The first writings on the medical use of cannabis, for which the female flowers of the hemp plant are almost exclusively used due to the high amount of cannabinoids it contains, go back to a roughly 4,700 year old Chinese textbook on botany and healing arts. The oldest marijuana found dates back to around 700 BC. Chr. And was a grave goods. In excavations in the Yanghai tombs in Xinjiang , an autonomous region in western China , the remains of seedlings , leaves and fruits of Cannabis sativa were found . With radiocarbon dating , their age could be determined to be about 2500 years.
Reports on the use of the ingredients for medicinal or ritual purposes can also be found in Indian literature about 2400 years ago (400 BC). Medical literature of the period also describes uses in epilepsy and pain.
Herodotus reports of the Scythians that they put hemp seeds on hot stones in their tents and cheered them on because of the euphoric effect. This steam bath (gr. Πυρία pyria ) was mainly used for cleaning.
Cannabis has been introduced into European folk medicine since the First Crusade (1096-1099) and appears in many monastic medicines. Areas of application were rheumatic and bronchial diseases. In addition, cannabis was widely prescribed as a substitute for opium . From the 16th century onwards, cannabis found its way into the herbalist books. In the 19th century it was used against migraines, neuralgia, epilepsy-like cramps and sleep disorders, among other things. Marijuana was the most widely used pain reliever in America until it was superseded by acetylsalicylic acid in 1898 and eventually replaced as a remedy by a wide variety of new, synthetic drugs. Between 1842 and 1900, cannabis preparations made up half of all drugs sold there. Over 100 different cannabis medicines were available in Europe between 1850 and 1950. Due to dosing difficulties, paradoxical effects and the development of synthetic drugs, prescriptions decreased in the 20th century until cannabis was banned almost completely worldwide in the middle of the 20th century. Today the medicinal use of cannabis is allowed again in many countries. However, it is almost impossible in Austria to get cannabis legally as a drug.
In France , the mind-altering properties of the ingredients were emphasized, particularly in literary circles such as Alexandre Dumas the Elder , Charles Baudelaire and Fitz Hugh Ludlow , while in England medical applications were in the foreground; W. B. O'Shanghnessy calls calm, seizure and convulsion relief. Hemp was often used as a cheap tobacco substitute and in this context was often casually referred to as knaster or strong tobacco in the literature .
Use as an intoxicant and prohibition
Cannabis, usually in the form of alcoholic extracts, was a readily available drug until the first third of the 20th century and was one of the most widely prescribed drugs in the 19th century. At the second opium conference in Geneva on February 19, 1925, Germany signed a revised agreement from the first opium conference on drug trafficking. It came into effect on September 25, 1928. As a result, drugs such as heroin , cocaine and, at the urging of Egypt , cannabis were added to the list and treated as opiates . India , the only country able to show scientific research, disagreed on religious and cultural reasons. Germany also saw no reason to include cannabis. As a result, Egypt threatened import restrictions for cocaine ( Merck KGaA ) and heroin ( Bayer AG ). Bayer intervened with the German government at the time, which then joined the ban, so that a new opium law was passed in 1929. The current illegalization of cannabis came in the second half of the 20th century through the direct transfer of the Opium Act of the German Empire in the version of December 10, 1929 ( RGBl. I, p. 215) into the Narcotics Act on December 24, 1971 ( BGBl. 1971 I p. 2092 ).
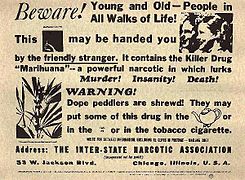
At the beginning of 1936, targeted lobbying , racist- tinged propaganda by the Hearst Corporation of media mogul William Randolph Hearst against marijuana, perceived as a new drug, began in the USA ; that marijuana and hemp are identical was not recognized. Crime was often linked to marijuana in Hearst's newspapers. The term marijuana comes from the language of Mexican immigrants. Marijuana has been described in films such as Reefer Madness as "the drug of the perverts , ailing subhumans , mindless negroes and Mexican immigrants ". Critics say that this campaign was initiated because hemp was an inexpensive raw material for paper and raw material production and could therefore have resulted in high financial losses for the forest and paper mill owner Hearst and the chemical company DuPont . During this time DuPont patented nylon and rayon , which competed with hemp fiber. Ultimately, this could have led to the de facto ban in 1937. Critics of this theory are of the opinion that Hearst, as a capitalist, could also have benefited from hemp. In this way, author Herer would describe the general xenophobic and racist mood in society, such as: B. the well-known racial segregation in the USA, hide. Shortly after the ban, Popular Mechanics magazine reported the invention and production of efficient harvesting machines for the hemp, which was previously difficult to harvest. Popular Mechanics had not yet recognized the ban on hemp as such and prophesied golden times for it. One of the driving forces behind the US cannabis ban was Bureau of Narcotics Chairman Harry J. Anslinger . He had been appointed and installed by then Treasury Secretary of the United States, Andrew W. Mellon , an uncle-in-law of Anslinger who was also a banker and financier of William Randolph Hearst and DuPont.
The production of hemp was revived in the USA during the Second World War . Hemp farmers were exempted from military service and commercials such as Hemp for Victory were shot because hemp was needed as a raw material for uniforms, bandages, aircraft construction and the like. After the Second World War, all hemp fields were again banned and burned. The German version of it was the The Funny Hanffibel , 1939, ed. from Reichsnährstand Berlin from the book series Funny Fiebeln , which should show the hemp cultivation in a simple way.
1935 Advertisement from the Federal Bureau of Narcotics
Hemp for Victory from 1942
Products
Cannabis flowers (marijuana)
The dried unfertilized female inflorescences (with or without attached leaves) are smoked or vaporized. An active ingredient content of up to over 30% is possible with certain cannabis varieties under the best conditions. Medical cannabis in Germany currently offers THC values between under 1 and up to 22%, depending on the variety. The CBD content of official medical cannabis in Germany is between 0.05 and 10.2%.
Cannabis extracts (hash oil, dab)
The oil extracted from the plant with mostly aprotic-non-polar solvents is evaporated and inhaled (dabbing), smoked or used to prepare drinks and meals containing THC. Cannabis extracts with butane or propane as solvents are called dab , BCO (butane cannabis oil), BHO (butane hash oil) or PHO (propane hash oil). The fractions of the extract can be divided into cannabinoids (including in acid form), monoterpenes and sesquiterpenes . The THC content can be up to 90%, when using supercritical CO 2 the cannabinoid fraction was up to 92%. Decarboxylated cannabis extract can also be produced, which can be used orally, e.g. B. by trickling under the tongue, which would not lead to intoxication with pure THC acid extract. The THC carboxylic acid of the plant is converted into THC.
hashish
The pressed resin of the hemp plant is smoked or, dissolved in fat , used to prepare drinks and meals that contain THC.
Kief
Kief (also called keef or skuff) is a powdery substance made from the trichomes of the hemp plant.
Types of Consumption

There are different ways of supplying cannabis active ingredients, but only the routes via the lungs or the gastrointestinal tract are common. Depending on the form of application and the product, the time until the onset of intoxication varies from a few minutes when inhaled and between 30 and 60 minutes when ingested orally. The effect after inhalation lasts for two to three hours, and significantly longer when consumed orally. Oral consumption or vaporizing in a vaporizer can reduce the burden on the respiratory tract by avoiding the carcinogenic substances produced during combustion.
Via the lungs
In order for cannabinoids to be absorbed through the lungs, they must be brought into an inhalable form. By heating above the vaporization point of the cannabinoids, for example by evaporation ( vaporizer ) or by burning (smoking), e.g. B. by means of a joint and bong , but also pipe , blunt , shillum or bucket smoking , they are converted into the gaseous phase. Inhaling these cannabinoid-containing gaseous products is also smoke pot and consumers Kiffer called, which in the 20th century from the English kif was borrowed and the Arabian kaif back (well-being).
Via the gastrointestinal tract
For oral consumption, as cannabinoids are fat-soluble, cannabis is processed with foods with a high fat content or dissolved in fat-containing carrier substances; Cannabis can be baked in baked goods directly or as cannabis butter or bound with cocoa or chocolate. In corresponding consumer groups, this variation is often referred to as a space cookie . As a drink, cannabis butter is e.g. B. mixed in hot tea with the addition of honey. In medical applications, the preparation of an aqueous extract (tea preparation) and the pharmaceutical production of plant extracts or THC in its pure form are common.
Sublingual - Via the mucous membranes of the mouth
The absorption of alcoholic extracts of the cannabis plant through the oral mucous membranes is still not very common. The effect sets in much faster than when it is absorbed via the gastrointestinal tract and is therefore easier to control. The tincture is typically dripped under the tongue, from where the active ingredients enter the bloodstream.
A bong is being smoked
effect
Biochemical principles and active ingredients


Cannabis active ingredients develop their effects by influencing the body's own endocannabinoid system . So far, a class of receptors with two subtypes has been identified in the organism of vertebrates : CB 1 and CB 2 . However, because of the complex spectrum of effects of cannabinoids, it is assumed that additional receptors (i.e. non-CB 1 and non-CB 2 ) exist .
The CB 1 receptor is primarily located in the central nervous system; however, there are also fewer receptors in cells of the immune system , such as mast cells or T-helper cells . A particularly large number of receptors are identified in the brain regions responsible for memory, movement and pain perception. The CB 2 receptor is present in the entire organism, but especially in cells that are part of the immune system. CB 2 receptors play an important role in regulating the immune response and in inflammation.
Δ 9 - Tetrahydrocannabinol (THC) is mainly responsible for the psychotropic effects of cannabis through its binding to the CB 1 and CB 2 receptors (CB 1 : K i = 10 nM; CB 2 : K i = 24 nM) . THC was first isolated in 1964, making it the longest researched cannabinoid; it also makes up the largest proportion of the isolated cannabinoids from the cannabis plant (possible mass fraction in the flower of over 20%). Based on studies in mice, it is assumed that Δ 9 -THC acts as a partial agonist . This means that it occupies a certain receptor ( lock and key principle ) and thereby partially imitates or replaces a neurotransmitter (mediator) in its effect.
So far, in addition to THC 113, other cannabinoids have been identified, the mass fraction of which is usually below 0.1%. The proportion of the cannabinoids cannabigerol (CBG), cannabichromene (CBC), cannabidiol (CBD) and cannabinol (CBN) can be higher: Depending on the cannabis variety, contents of well over 1% can be present:
- CBG accounts for 94% of the cannabinoid fraction in a variety of French fiber hemp discovered in 1987.
- CBC can make up to 5% of the cannabinoid fraction in some plants.
- The CBD content of the Harlequin hemp varieties, specially bred with this in mind, is around 4%.
- CBN is formed as a breakdown product of THC after cannabis is harvested and is thus an artifact.
Of the aforementioned cannabinoids, the non- or only weakly psychoactive CBD is considered to be of particular pharmacological interest. The exact mechanism of action of CBD is unclear. Some sources assume that CBD does not directly affect the response of the CB 1 or CB 2 receptors, but only indirectly through an unexplained metabolic mechanism ; other sources suggest an affinity preferentially for the CB 2 receptor. Regarding the effects of CBD, one is therefore largely dependent on indirect empirical data. It is believed that CBD counteracts the psychotropic, head-heavy properties of THC; it lessen the effect and at the same time increase the duration of action. Cannabis varieties with a high CBD content, such as Cannabis indica , have a central dampening, body-focused effect. CBD has relaxing, anticonvulsant, anti-anxiety and anti-inflammatory effects, but it is not scientifically clear whether this effect is due to the higher CBD content or whether other active ingredients in cannabis are responsible for it. While the THC content has increased over the years, cannabidiol has been deliberately crossed out or down to an extremely low level in many breeds.
The other main components of cannabis, which are not or barely psychoactive, have been little researched. The ratio of these active ingredients is determined by the genetic variant, especially with Cannabis sativa and Cannabis indica , and the time of harvest. The cannabinoids interact with each other .
Active ingredient contents
The active ingredient content of cannabis products has increased over decades. The breeding of new varieties with higher THC contents, mostly under artificial light indoors, has largely replaced the production of marijuana (cannabis herb) from outdoor-suitable varieties with lower THC values, while outdoor cultivation in "classic" countries of origin such as Morocco or Afghanistan as well as in countries with better climatic conditions is still very common. The THC content in the Netherlands was around 8% for cannabis resin ( hashish ) in 1997 and 18% in 2003, and in Germany it was 7.5% to 14%. In the UK , the resin increased from less than 7% in 1977 to around 9% in 2003, and for marijuana from 9.4% to 12.3%. At the European level, there was a further increase in the THC content between 2006 and 2014 until it stabilized in 2015. In 2015, national average active ingredient contents between 3 and 22% for marijuana with a quartile gap of 7 to 11% and 4 to 28% for hashish with a quartile interval of 11 to 19%.
Intoxication effect

The intoxication can bring about a shift in consciousness with associative, erratic thinking and an impairment of the short-term memory. This change in consciousness can cause positive as well as negative sensations. Mostly reports of an intensification of the emotional life, as a rule of a more positive attitude towards life and the feeling of a more intimate connection with familiar people; Occasionally, the emotions can turn into fear, sadness, suspicion, or depersonalization . Common physical effects are reddened eyes, dry mouth, increased feeling of hunger, increased pulse, lower blood pressure and tiredness or listlessness.
The acute effects of cannabis can vary greatly depending on the person, the proportion of the active ingredient, the current physical and psychological state or experience with the drug. An inexperienced cannabis user can therefore not reliably assess the expected effect, but regular users can.
Toxicity
Cannabis itself is not toxic to humans in and of itself; the lethal dose LD 50 of the main active ingredient THC in mice in the case of intravenous administration is 29 mg per kilogram of body weight, but in the case of oral administration 482 mg / kg. In rats, the oral LD 50 is 666 mg / kg and the intravenous is 29 mg / kg. Animal lethality studies show that the doses of cannabis required to induce death go well beyond what a human could consume. It is therefore excluded that there was ever a human death from cannabis as a result of an overdose.
Mixed use with other drugs
As with all other combinations of different psychoactive substances, interactions between cannabis and other drugs can occur.
caffeine
Studies on squirrel monkeys ( Saimiri Sciureus ) who had previously been accustomed to self-administration of THC and subsequently received MSX-3 , a water-soluble A2A antagonist, showed a dose-dependent increase in cannabinoid receptor activation, but at higher doses a suppression, from which it was concluded it was found that A2A antagonists like caffeine potentiate the effects of threshold doses of THC.
alcohol
With mixed consumption of cannabis and alcohol , the alcohol effect can be intensified and, depending on the affect , cause nausea and fainting or increased friendliness, vitality and euphoria. Mixed consumption with alcohol is considered to be particularly hazardous to traffic, because the opposing effects of drive and risk-increasing alcohol and cannabis, which has a hallucinatory effect, significantly increase the risk of accidents.
tobacco
By consuming cannabis with tobacco, it is possible that a cannabis user who previously did not smoke tobacco could develop a nicotine addiction . There is also an increased risk of respiratory diseases. Nicotine suppresses the effect of THC, while THC increases the effect of nicotine, so that mixed consumption with tobacco also increases the chance of experiencing a more unpleasant intoxication experience than when consuming it neat.
MDMA
Studies with mice and rats have shown that delta-9-tetrahydrocannabinol , as well as the artificial cannabinoid CP 55,940, completely prevent the hyperthermal effect of MDMA . The resulting hypothermia reduces neurotoxic damage. However, a double-blind, placebo-controlled study in humans showed the opposite effect. Although the peak of the MDMA-related temperature increase due to the addition of cannabis was delayed by about 45 minutes, it was the same. A clear reinforcement effect from cannabis was given by the fact that the MDMA-related maximum temperature lasted longer than 2.5 hours (end of the measurements), while without the addition of cannabis it had already decreased after 45 minutes and after a further 2.5 hours had completely returned to the pre-MDMA level.
opiate
Delta-9-tetrahydrocannabinol increases the effectiveness of opioids such as morphine in animal models . The analgesic effect of THC is mediated , at least in part, by δ and κ opioid receptors , so that a connection between cannabinoid and opioid signaling pathways in the modulation of pain perception is suspected.
Possible health effects

This section deals with the harmful aspects of cannabis use. For the medicinal options see: Cannabis as a medicine .
Whether and which health consequences arise from cannabis use is controversial and cannot be answered across the board. Even effects on the respiratory system and a possible increased risk of cancer when smoking cannabis are largely controversial. The data situation regarding health effects on the psyche, the development of addiction and similar questions is also inconsistent. It is unclear whether and, if so, for which group of people which dose has a harmful effect and whether, under certain circumstances, even single or infrequent consumption can cause health problems.
The health effects of cannabis use are not well understood and depend on a variety of complex, sometimes interlocking factors and circumstances:
- Drug addiction
- amount consumed, form of consumption
- Mixed consumption with other drugs (including alcohol and especially tobacco / nicotine)
- personal maturity and biological age (brain maturation)
- the personal constitution and environment, the form of the day (see set and setting )
- Stability of the psyche, individual susceptibility to the development of addiction
- immediate environment, presumably also genetic requirements.
Effects on the respiratory system
Smoking cannabis can potentially have negative effects on the lungs. This is certainly the case when cannabis is mixed with tobacco, which is common in Europe. These mixtures, known as joints , are particularly harmful to health , also because of the additional damaging effects of nicotine on blood vessels .
A cohort study on 5115 smokers (of both cannabis and tobacco) showed that infrequent to occasional consumption of pure cannabis (up to 20 times a month) has no negative effects on the performance of the lungs, but that it drops sharply with intensive consumption. However, due to the small number of strong, pure cannabis smokers and significant differences in consumption behavior, the statistical power of this study is limited. The tobacco users in this study smoked significantly more on average (8 to 9 cigarettes a day) than people who only consumed marijuana (an average of 2 to 3 times a month).
If cannabis is smoked, carcinogenic substances are produced when it is burned, similar to tobacco , but - in contrast to tobacco smoke - it is controversial that pure cannabis smoke can cause cancer. Two overview studies published in 2014 concluded that the risk of lung cancer due to the effects of tobacco was difficult to determine statistically, although one study found a two-fold higher risk of lung cancer among marijuana smokers. A large-scale study examining the medical records of 50,000 Swedish recruits over a 40-year period also found that the incidence of lung cancer doubled among pure cannabis users. The World Health Organization refers in its brief assessment of oncogenic potential in selected studies that conclude that cannabis use does not increase the risk of lung, head and neck cancer. If cannabis is not smoked but vaporized , only a comparatively small proportion of the carcinogenic substances is produced, as a study by the University of Leiden has shown. When vaping, the intoxicant is only heated to the point that primarily the psychotropic substances, above all THC, evaporate; combustion does not take place if operated correctly.
Cannabis and cancer
How exactly THC or other cannabinoids affect cancer development is a central research topic. Many studies point to the medicinal potential of cannabis in cancer . However, there is no known alleviation or cure for cancer through its use as an intoxicant. In studies of cannabis smoke, it was found that its composition is similar to that of tobacco smoke with its often carcinogenic ingredients. The WHO only considers a two and a half times higher risk of prostate cancer to be proven. A higher incidence of bronchial carcinomas among cannabis users cannot yet be conclusively assessed on the basis of the current data, even if many studies consider the connection between cannabis use and the likelihood of malignant lung carcinomas to be probable.
Cannabis and psychosis
Cannabinoid-induced psychotic disorder (ICD-10 F12.50-.53)
Investigations into a possible connection between the COMT genotype and the likelihood of developing psychosis in cannabis users have so far (as of 2018) produced inconsistent results and an extremely complex picture. It has also remained unclear whether cannabis acts as the sole factor or in combination with other factors (alcohol, previous illnesses) as a trigger for psychoses. Among other things, an increased THC content in illegal cannabis products and an increased consumption behavior are associated with a higher probability of developing a psychotic disorder (e.g. schizophrenia). A 2007 meta-analysis of 35 individual studies in the medical journal The Lancet reported that the user group who used cannabis most often was at greater risk . A disruption of dopaminergic systems caused by cannabinoids was discussed as a possible neurobiological mechanism . The rate of possibly cannabis-induced psychosis may be lower in patients who start using cannabis in adulthood. The psychotic disorder induced by cannabinoids ( ICD-10 F12.50-.53) is often paranoid-hallucinatory with clearly affective components (schizoaffective characteristics). It lasts from days to a few weeks, rarely months.
The World Health Organization stated in its 2018 review:
"The vast majority of people who use cannabis will never develop a psychotic disorder, and those who do are likely to have some genetic vulnerability to cannabis-induced psychosis."
"The vast majority of people who use cannabis will never develop psychotic disorder, and those who do are likely to be genetically susceptible to cannabis-induced psychosis."
Cannabis and schizophrenia
The claim that cannabis causes schizophrenia has not yet been proven. According to the current state of science, cannabis cannot be assumed to cause schizophrenia. The International Classification of Diseases has not provided a code for this, and the causal chain is unclear. Furthermore, cannabis use has risen sharply since 1960, but the number of schizophrenia cases has remained relatively constant.
There is some evidence that cannabis use may increase the risk of developing schizophrenia in certain people or make an existing schizophrenic illness worse. Most of the evidence that cannabis could cause schizophrenia comes from studies of people who use during puberty . Puberty is the period when you are most at risk of developing schizophrenia. According to a Mendelian randomization study (2017), the risk of developing schizophrenia through cannabis use is increased by 37% from around 0.7 to 0.96% ( odds ratio : 1.37; 95% confidence interval , 1.09 to 1, 67; p-value = 0.007). The risk is further increased by 43% from about 0.7 to 1% if similar studies and symptoms are taken into account in the meta-analysis. (Odds ratio: 1.43; 95% confidence interval, 1.19 to 1.67; heterogeneity : 0%). However, it could not be ruled out that incorrect conclusions were drawn, e.g. B. that cannabis use is a form of self-medication or tobacco is the trigger of psychosis. A systematic review from 2017 came to the following conclusion on this question:
"There is substantial evidence of a statistical association between cannabis use and the development of schizophrenia or other psychoses, with the highest risk among the most frequent users."
"There is substantial evidence of a statistical relationship between cannabis use and the development of schizophrenia or other psychoses, with the highest risk among the most frequent users."
A genome-wide association study published in 2018 with almost 185,000 participants, in which, among other things, 23andMe data was used, found only weak evidence for a causal influence of cannabis on schizophrenia, but significantly stronger evidence for the opposite relationship, i.e. that schizophrenics or people with genetic susceptibility tend to be more inclined to use cannabis:
"Our findings further indicated a causal influence of schizophrenia on cannabis use and substantial genetic overlap between cannabis use and use of other substances, mental health traits, and personality traits, including smoking and alcohol use, schizophrenia, ADHD, and risk-taking."
"Our results also showed a causal impact of schizophrenia on cannabis use and significant genetic overlap between cannabis use and use of other substances, mental health traits, and personality traits, including smoking and alcohol use, schizophrenia, ADHD, and risk taking."
Motivation and Neural Reward Systems
The German headquarters for addiction risks is of the opinion that the special group of users, in which cannabis use and personal and social risk factors come together, is a particular risk, which is described as follows:
“The consumer himself has a feeling of increased efficiency, but objectively this is decreasing more and more. In place of orderly thinking and logical conclusions, there is often a kind of sham profundity, which primarily affects due diligence. [...] In connection with the aforementioned amotivation syndrome, there is an increasing general disinterest, coupled with reduced resilience. The consumer withdraws more and more into himself and becomes more and more indifferent to himself and to the tasks of everyday life: He gradually feels less and less committed to the demands of the performance society, but also less and less able to cope, and more and more cares about his previous social structure out."
The amotivation syndrome (AMS) had not been adequately investigated until 2015. A more recent study from 2018 also assessed the amotivational syndrome as inconsistently documented:
"In conclusion, studies examining the effects of cannabis use on motivation and reward sensitivity have yielded mixed findings. We conclude that cross-sectional evidence supporting the presence of amotivational syndrome among cannabis users or an adverse cannabis-specific effect on motivation is currently equivocal. "
“In summary, it can be said that studies examining the effects of cannabis use on motivation and sensitivity of the reward system led to different results. We come to the conclusion that cross-sectional studies on the amotivational syndrome among cannabis users or on a negative cannabis-specific effect on motivation are currently inconclusive. "
Investigations into the changes in the reward systems of the brain caused by cannabis use showed functional impairments both in behavior and directly in the relevant regions of the brain during imaging procedures . Earlier studies had already indicated that the reward systems normalize again after a long period of non-consumption. This was seen as an important indication that actual cannabis use - and not a previously disrupted reward system (resulting in self-medication by the user) - should be viewed as the cause of the connection.
Organic brain changes

Some studies, in which only a few participants were involved, have found structural abnormalities in regions of the brain that are important for cognitive function, mood, and reward. However, such effects do not appear to be present in larger studies that were checked for confounding factors such as alcohol consumption, tobacco consumption, gender, age and other variables.
A meta-analysis from 2013 relating to a large number of brain studies with imaging methods came to the result that there was insufficient data on structural changes for many relevant brain regions. Wherever usable amounts of data existed, however, there was still no uniform picture when comparing the studies. An exception was found in the hippocampus , which has a key role in all memory functions . Here, cannabis users showed a smaller hippocampus than non-users in all studies. According to the authors' assessment, the results indicate that brain regions that are rich in cannabinoid receptors, such as the hippocampus, could be affected by nerve-damaging ( neurotoxic ) effects with prolonged use of cannabis .
In young people
Because of the importance of the body's own cannabinoid systems during the development of the brain (formation of neural networks ), the influences of cannabis use are particularly pronounced in adolescents. Local reductions in brain volume and functions correspond to reduced cognitive performance, but after a few weeks of abstinence, these performance are regulated again. A lower number of cannabinoid receptors in the brain could be detected in heavy adolescent cannabis users.
In adults
Meta-analyzes from 2013 and 2014, which evaluated brain studies using imaging methods, came to the result that cannabis users had a reduced brain volume and impaired white matter in the prefrontal cortex (frontal side of the frontal lobe of the cerebral cortex) , as well as a bilateral reduced volume of the hippocampus . In the latter brain region, there was also a correlation (correspondence) between the decrease in volume and the amount of cannabis consumption to date. So far it has not been possible to clarify whether the use of cannabis increases existing peculiarities or whether it is the cause of organic brain peculiarities.
intelligence
Acutely , cannabis has a negative effect on some cognitive functions , including a. in the area of attention, memory functions and psychomotor functions. Effects on these functions can persist for days or weeks after prolonged (chronic) use, even if no further cannabis is consumed. It is unclear to what extent cannabis users can assume persistent impairment of cognitive functions even after long periods of abstinence. Only two prospective long-term studies also included the cognitive functional level before cannabis use: An evaluation of data from the New Zealand Dunedin Multidisciplinary Health and Development Study came to the conclusion that cannabis consumption permanently increases the intelligence quotient (IQ) - even after consumption has ceased. impaired and that this effect strongly with earlier age of onset and duration of consumption correlated ; Another study found a statistically significant decrease in general intelligence, the speed at which information was processed and in short- and long-term memory in young adults with chronic cannabis use . In contrast, three months after cessation of consumption, no effects were found in this study.
A meta-analysis (2018) of 69 cross-sectional studies with 2152 cannabis users and 6575 controls (mean age: 20.6 years, 68.4% male) showed only a small effect size for reduced cognitive functions in frequent or heavy cannabis users. In view of the small effect size , the authors of the study asked about the clinical significance of such cognitive impairments for the majority of cannabis users. No relationship could be found between the age at which cannabis use began and cognitive functions. In addition, studies with abstinence periods greater than 72 hours failed to find a link between cannabis use and impaired cognitive function, suggesting that the effects of cannabis use on cognition are reversible. Those who started cannabis use in early adulthood and had been abstinent for a year showed no decrease in IQ, suggesting a lack of residual effects.
Dependency

With regular, intensive consumption, a tolerance effect (necessary dose increase in order to achieve the usual effect) can develop. In the diagnostic manual ICD-10 the World Health Organization WHO is listed cannabis dependence (F12.2), but no withdrawal criteria are defined.
It is assumed that in the case of cannabis addiction, withdrawal symptoms such as irritability, restlessness or sleep disorders, which occur after 24 to 48 hours and can last up to three weeks (sleep disorders possibly longer), are due to an underactive mesolimbic system ( subcortical reward systems) that will take effect after consumption has ceased are conditional. The assumption was confirmed by imaging tests in 2016 .
In Germany, the Federal Ministry of Health assumes that 0.5% of the 18 to 64 year old population is addicted to cannabis. Epidemiological studies estimate that around 4.5% of all people who have ever used cannabis will develop cannabis addiction at some point in their life.
It should be borne in mind that the figures on which such calculations are based could well be far too high in Germany, as they are based on the fact that convicted criminals can evade their prison sentence or part of their prison sentence if they undergo therapy for drugs ( § 35 BtMG: “Therapy instead of punishment”). According to conservative estimates, around 30 to 45% of all drug therapy starts in Germany are made in accordance with Section 35 BtMG. Probation sentences and juvenile sentences or conditions in return for discontinued procedures can include coercive therapy, so that the Federal Ministry of Health states: "The vast majority of patients are on the basis of a criminal sanction in drug treatment, be it according to § 35 BtMG or according to §§ 36 , 37 BtMG (suspension of the (remaining) sentence on probation). “The number of those who start drug therapy in Germany without pressure from the judiciary is estimated by the Federal Ministry of Health at around 20%.
pregnancy
There is strong population-based evidence that cannabis smoking during pregnancy reduces the birth weight of offspring. A meta-analysis found that female cannabis users gave birth to babies with a birth weight that was on average 109 grams lower than that of mothers who did not use cannabis. Another meta-analysis showed a reduction in birth weight of 131 grams. It is unclear whether the lower birth weights can be specifically attributed to cannabinoids. It could also be explained by the carbon monoxide in cannabis smoke. A 2016 study associates prenatal cannabis use with premature births and reduced birth weight. Here, the probability of a premature birth with cannabis use before and during pregnancy was twice as high. Continuous cannabis use after the 20th week of pregnancy is associated with a five-fold higher risk of premature birth.
Cannabis in the entry-level drug hypothesis
The term gateway hypothesis or gateway hypothesis is an expression of the question of whether the use of one drug is linked to an increased likelihood of using other drugs.
The Federal Constitutional Court found in 1994 that the thesis of cannabis as a gateway drug was "largely rejected".
According to the review by Hoch et al. (2015) there is a correlation , but the question of causality (see also fallacy: irrelevant reference value ) is open:
“Various studies have shown a connection between early, regular cannabis use and continued use of other illegal drugs or alcohol. The fact that cannabis functions as an access substance for the use of other substances ("gateway hypothesis") has not been empirically proven. "
In 2017, the entry-level drug hypothesis was generally confirmed to have significant gaps in knowledge by Miller and Hurd:
"Overall, the concept of the gateway hypothesis has inspired a large body of research, but there remain significant gaps of knowledge before we are able to fully accept or refute the hypothesis."
"Overall, the concept of the gateway hypothesis has stimulated an extensive body of research material, but there are still significant gaps in knowledge before we can fully accept or refute the hypothesis."
Cultivation

Cannabis is grown worldwide. There are male and female hemp plants ( diocese ), and hermaphrodites can occasionally develop . The unfertilized female plant is (almost) exclusively used as an intoxicant or to obtain it, as its flowers have the highest concentration of active substances in THC.
Hemp species and varieties
Several thousand cultivars were created from the species hemp ( Cannabis sativa ) and Indian hemp ( Cannabis indica ) by crossing them, e.g. B. Kush or White Widow . For a long time, ruderal hemp ( Cannabis ruderalis ) hardly played a role in the production of intoxicants, but in the meantime it is used to develop autoflowering (also called "automatic") cannabis varieties that, in contrast to conventional cannabis varieties, after a certain light duration usually a very short period of about eight weeks to initiate flowering. Whether C. indica and C. ruderalis are separate species or just subspecies of C. sativa is controversial. In general, the ratio of CBD to THC is higher in Indian hemp. This fact is attributed to the more calming and more physical effects of Indian hemp.
Main growing countries
Afghanistan was the world's largest producer of cannabis in 2010, with an estimated 1500 to 3500 tons of crops. Although the cultivation is illegal, it is practiced in at least 17 out of 34 provinces and plays an important role there economically. The majority is exported as hashish. Other important growing countries are Jamaica , Colombia , Lebanon , Morocco , Nigeria , Pakistan , Thailand and Turkey . In 1990, hemp was grown on around 120,500 hectares in Morocco ; Back then, around 80% of the hashish seized in Europe came from there. Due to changed cultivation methods in Morocco, the THC content increased dramatically between 2006 and 2016.
Situation in Austria and Germany
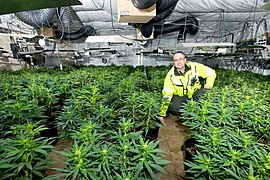
Most of the marijuana available in Austria and Germany is now cultivated illegally in Germany under artificial light, and less often imported from Switzerland, the Czech Republic or the Netherlands. Outdoor cultivation is also possible in principle in countries like Austria and Germany, especially in warmer regions. The cultivation can be spotted relatively easily because of the characteristic appearance of the plants.
Growing marijuana under artificial light in one's own apartment, indoor growing , for example in the grow cabinet , has apparently increased significantly in Austria and Germany in recent years:
In the report on the drug situation in Austria published by the Ministry of Health for 2014 and 2015, it is stated that cannabis production is increasing and in 2015 "cultivation in Austria [...] mostly for personal use or for trade on a smaller scale."
According to the Federal Government's Drugs Commissioner, cannabis species (in contrast to industrial hemp ) grown for the production of intoxicating drugs are mainly grown in indoor facilities in Germany, with 665 cannabis plants discovered in 2012, compared to only 619 in the previous year. The Hamburg police spokeswoman Ulrike Sweden stated in 2013 that the sharp increase in cannabis plantations was "mainly due to the use of grow cabinets". In connection with such few discoveries of cannabis plants in German-speaking countries, it is interesting that 25,000 cannabis cuttings are sold every week in the stores of the Flowery Field chain in Vienna, the approximately 20 other stores in Vienna and other stores in Austria, who also sell cuttings, not counting. Selling cuttings, as opposed to letting them flower, is legal in Austria.
Indoor growing
Indoor growing is the cultivation of cannabis inside greenhouses. Cultivation, including for obvious personal use, is a criminal offense (Germany: Section 29 (1) No. 1 Narcotics Act; Austria: Section 27 (1) No. 2 of the Narcotics Act; Switzerland: Chapter 4, Section 1, Art. 19 Narcotics Act ). The reasons for illegal cultivation are, on the one hand, of a financial nature, since despite the considerable costs for the long-term amount of energy used for lighting and the high workload, attempts are made to avoid black market prices of around five to over ten euros per gram (as of 2010). In order to reduce the risk of discovery, attempts are being made to reduce the odor nuisance caused by the intensely smelling plant using a ventilation system and carbon filter.
Indoor Growing in Growtent growth phase
Growing outdoors
Outdoor growing is the cultivation of cannabis outside of greenhouses.
Growing cannabis outdoors is similar to growing industrial hemp or other field crops that depend on the nitrate content of the soil. The energy requirement for this cultivation is very low compared to production in the greenhouse or indoor growing, the hemp plant can benefit here from field management and direct sowing .
Cannabis thrives best in well-drained soils that are rich in organics. The soil pH should be neutral or slightly below.
Growing outdoors in the garden
Spread in the population
Consumption statistics
According to surveys from 2015, around 7% of 12 to 17-year-olds and around 6% of adults in Germany consumed cannabis in the twelve months prior to the survey.
In 2014, a study by the Federal Center for Health Education in Germany estimated that 17.7% of young adults between the ages of 18 and 25 had consumed cannabis at least once in the past twelve months. For 14 to 17 year olds it was 11.4%. The proportion of those who regularly use cannabis (more than ten times in the last twelve months) has consistently been below 5% in the surveys since 2001 among 18 to 25-year-olds and below 3% in the 14 to 17-year-old age group %.
In the Health behavior in school-aged children (HBSC) survey carried out in North America and Europe between October 2005 and May 2006 , 18% of 15-year-old schoolchildren said they had used cannabis before, including 28% in Switzerland (girls) or 36% (boys), in Austria 13% each, in Germany 14% and 18%.
When the survey was repeated between 2013 and 2014, 15% of the 15-year-olds surveyed stated that they had previously consumed cannabis, including 19% (girls) and 29% (boys) in Switzerland, 7% and 13% in Austria %, in Germany 15% and 18%.
For Switzerland, a population survey carried out in 2014 showed that 31.5% of the population over the age of 15 had experienced cannabis at least once in their life, with 6.7% of those surveyed also in the last 12 months 3.0% also in the last 30 days. Based on these data, 210,000 people in Switzerland had used cannabis in 2014.
In a representative study with 9th grade adolescents from Germany published in 2016, the lifetime prevalence of cannabis (i.e., ever tried the substance in a lifetime) was 12.9%. Of the adolescents aged 15 on average, 11.7% had consumed cannabis in the last 12 months, the proportion of regular users (more than 12 times a year) was 3.2%. The average first-time consumption was 14.3 years.
There were differences in the consumption behavior of adolescents with and without a migration background: 15.2% of adolescents with a migration background and 12.6% of adolescents without a migration background had ever consumed in their life. The proportion of consumers in the last 12 months was 13.6% for young people with a migration background and 11.5% for young people without a migration background.
Effects of cannabis legalization and prohibition on the number of users
A systematic review by the Scientific Services of the German Bundestag on November 21, 2019 dealt with the question of whether legalization could lead to an increasing number of consumers and whether young people in particular could be encouraged to use cannabis. The question of whether there are already data or studies that establish a connection between the legalization of cannabis and / or other drugs and the number of (first) users was also investigated. The countries examined were Belgium, the Netherlands, Canada, Portugal, Uruguay and the USA, in which cannabis prohibition was partially or completely lifted.
The study by the Scientific Services of the German Bundestag cites, among other things, observations from a further overview study by Eastwood et al. (2016), which the decriminalization movements in Holland, the USA and Portugal a. a. since 1976 to 2016 and came to the following conclusion:
“That the pursuit of a strict drug policy has little or no influence on consumption behavior”. Rather, "some of the countries with the most stringent legal regulations had some of the highest prevalence rates for drug use, while countries that pursued liberalization policies had some of the lowest prevalence rates."
A short summary of some selected results from Eastwood (2016) for some countries (Portugal, Belgium, the Netherlands, USA) can be found in German in the statement of the Association for Drugs and Addiction Aid, funded by the EU and the German Federal Ministry of Health (2019 ): Decriminalization of cannabis users and shaping of regulation.
Cannabis in popular culture
Cannabis has been common in European and American youth culture since the late 1960s. Cannabis has been an issue in various youth cultures since the 1990s , especially in hip-hop and reggae . The genre of the stoner movie developed in film. There are also themed magazines such as Grow! and Highway in German-speaking countries or High Times in the USA. Various museums such as the Hash Marihuana & Hemp Museum , the Hash Marihuana & Hemp Museum (Barcelona) and the Hemp Museum are dedicated to the presentation of cannabis as an intoxicant. Examples of musical works on the topic are the album Legalize It or the song Gebt das Hanf frei! . There are also themed festivals such as the Portland Hempstalk Festival and there are computer games such as HighGrow .
Surveys on possible legalization in Germany
In a survey by the opinion research institute Forsa from the end of 2017, 63% of those questioned rejected the legalization of cannabis in Germany. In contrast, 34% are in favor of such legalization. The rejection was particularly high among women (70%), citizens over 60 years of age (72%) and supporters of the Union and SPD (72% each). People under 30 years of age (43%), supporters of the Left Party (55%), the Greens (46%) and the AfD (41%) spoke out in favor of legalization .
In a survey conducted by the opinion research institute infratest dimap in 2018, 52% of those surveyed rejected the legalization of cannabis for recreational purposes in Germany. On the other hand, 46% are in favor of such legalization. Legalized access to cannabis is most likely to find support among younger German citizens (56%), men and people with a high level of education (53% each). In contrast, older (62%), women (58%) and formally low-educated people (60%) are particularly negative. Legalized access to cannabis is clearly popular among supporters of the left (77%), the Greens (58%) and the AfD (50%). In contrast, the majority of the supporters of the Union (68%), SPD (63%) and FDP (63%) are against legalization.
Driving under the influence of cannabis
There are contradicting studies on the subject of cannabis and the ability to drive or fitness to drive. Most studies agree that the ability to drive is impaired up to an hour after consumption while in an acute cannabis intoxication. Two to three hours after consumption, on the other hand, there is a reduced risk of accidents for one-time users because the users drive more cautiously and more slowly. However, experts like Franjo Grotenhermen criticize the informative value of experimental studies in this area, as they can only estimate whether cannabis has a potential to impair driving ability and fitness to drive - but not whether and to what extent this potential is also manifested in road traffic. The question of whether cannabis increases the risk of accidents is best answered through epidemiological studies. The largest epidemiological study on this topic with over 9,000 participants was published in 2015 by the US National Highway Traffic Safety Administration (NHTSA). Accordingly, after correcting for age, gender, origin and alcohol consumption, there is no increased risk of a traffic accident after cannabis use compared to the control group without cannabis use.
Germany
In Germany, judgments by the Federal Constitutional Court (June 2002, December 2004) ensured a certain liberalization of the previously relatively strict practice of the authorities. The Federal Constitutional Court ruled in December 2004 that up to a limit value of 1.0 ng / ml active THC in the serum (blood) there is not necessarily a risk for road traffic.
After driving under the influence of drugs (above the limit value 1.0 ng / ml active THC or above 150 ng / ml of its breakdown product THC -COOH , in the case of direct blood sampling after consumption - in the case of previous consumption above 75 ng / ml), the responsible driving license authority the driver's license is usually withdrawn immediately and a medical-psychological examination (MPU) is required. In the event of repeated attention, even below the limit value, the authorities can request a drug test or a medical certificate (ÄG), since it then assumes that there is occasional to regular drug abuse. The driver's license will be withdrawn for the duration of the required, verifiable abstinence period (usually 12 months), if this has not already happened before. The driver's license holder bears the costs of the MPU. If cannabis use is on record without active participation in road traffic, this is usually reported to the administrative authority and at least leads to an entry in the driver's license file. This measure can also be taken after mere unlawful possession or a positive drug test as a passenger. Depending on the result of the medical report, the person concerned may keep the driving license or an MPU is ordered to clarify doubts about suitability.
Austria and Switzerland
In Austria and Switzerland it is forbidden to drive a vehicle under the influence of cannabis. People who have THC in their blood are considered impaired.
Legal position
According to the provisions of the 1961 Single Convention on Narcotic Drugs , which has been ratified by almost all countries in the world, the production, possession and trade of cannabis are prohibited in many countries, and in some countries its use is illegal. In Germany, the mere consumption of cannabis or other narcotics is de jure not punishable, on the other hand cultivation, manufacture, procuring, acquisition, possession, importing, exporting and transit, selling, dispensing and prescribing are all illegal , administering and leaving for direct consumption is punishable under the Narcotics Act or subject to approval.
Exceptions
- An exception is the Netherlands with its coffee shops , where the acquisition and possession of small amounts of cannabis (up to 5 grams or 30 grams) are tolerated and thus de facto exempt from punishment, although cannabis is still de jure illegal and prohibited in the Netherlands .
- There are several hundred cannabis social clubs in Spain , where Spaniards and foreigners can legally purchase and smoke cannabis.
- Uruguay has legalized the possession of cannabis.
- Canada also legalized adult cannabis nationwide on October 17, 2018. See: Legal Status of Cannabis Use in Canada
- Ten of the 50 states in the United States : Alaska , California , Colorado , Oregon , Massachusetts , Maine , Michigan , Nevada , Vermont, and Washington (state) , as well as Washington DC Federal District, have legalized cannabis as a narcotic. 33 of the 50 US states also allow the use of cannabis as medicine. See also: Legal Status of Cannabis Use in the United States
- In many other countries, the possession of a small amount of cannabis for personal use has also been partially decriminalized, with different amounts being considered small from country to country.
Effects of illegality
The vast majority of cannabis users in Europe are served by unregulated and illegal markets. The quality of the products with regard to admixtures or contamination with pesticides is not guaranteed under these circumstances. For example, harmful amounts of lead have sometimes been found in illegal cannabis products. Another risk of illegality “exists for all habitual consumers in the rigid criminal prosecution in Germany. More than 100,000 proceedings initiated against consumers each year lead to a high number of fines and prison sentences, in particular to problems in school, training and work as well as often to the loss of a driver's license, ”says the German headquarters for addiction issues . Furthermore, the Association for Drug and Addiction Aid 2019 states that the costs of repression for police and judicial authorities are significantly higher than the costs for offers of help for cannabis users with health problems.
See also
literature
General representations
- Ivan D. Montoya, Susan RB Weiss: Cannabis Use Disorders . Springer, 2018, ISBN 978-3-319-90365-1 .
- Roger G. Pertwee: Handbook of Cannabis . Oxford University Press, 2014, ISBN 978-0-19-966268-5 .
- Bernhard van Treeck : The great cannabis lexicon. Schwarzkopf & Schwarzkopf, Berlin 2000, ISBN 3-89602-268-7 .
Review articles
- Eva Hoch, Miriam Schneider, Chris Maria Friemel (eds.): Cannabis: Potential and Risk - A Scientific Inventory . Springer, Heidelberg 2019, ISBN 978-3-662-57291-7 , doi : 10.1007 / 978-3-662-57291-7 (478 pages, bundesgesundheitsministerium.de [PDF]). , Short report, 8 pages, PDF (PDF)
- World Health Organization , Expert Committee on Drug Dependence (Ed.): Critical Review of Cannabis and cannabis resin (PDF) Delta-9-tetrahydrocannabinol (PDF) Extracts and tinctures of cannabis (PDF) Isomers of THC (PDF). Department of Essential Medicines and Health Products, 2018. (English Abstract: WHO endorses decisions of Expert Committee on cannabis and other substances ).
- National Academies of Sciences, Engineering, and Medicine : Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research . 2017, Washington, DC: The National Academies Press. doi: 10.17226 / 24625 . ISBN 978-0-309-45304-2
Web links
- School and cannabis - rules, measures, early intervention. Handout for teachers in grades 7 to 13. Federal Center for Health Education (BZgA), accessed on October 20, 2014 (teaching materials).
- The cannabis consumption of adolescents and young adults in Germany 2012. Results of a current representative survey and trends. Federal Center for Health Education (BZgA), 2012, accessed on October 20, 2014 .
- Lisa Schnell: 360 ° legalization of cannabis - why the drug is legalized. And what that means. In: sueddeutsche.de . Retrieved March 29, 2016 .
Individual evidence
- ↑ United Nations Office of Drug and Crime (UNODC): World Drug Report 2017: Executive Summary Conclusions And Policy Implications. (PDF) United Nations Office of Drug and Crime (UNODC), accessed on March 7, 2018 .
- ^ A b Samuel D. Banister, Jonathon C. Arnold, Mark Connor, Michelle Glass, Iain S. McGregor: Dark Classics in Chemical Neuroscience: Δ9-Tetrahydrocannabinol. In: ACS Chemical Neuroscience. 2019, doi: 10.1021 / acschemneuro.8b00651 .
- ↑ Hong-En Jiang, Xiao Li, You-Xing Zhao, David K. Ferguson, Francis Hueber, Subir Bera, Yu-Fei Wang, Liang-Cheng Zhao, Chang-Jiang Liu, Cheng-Sen Li: A new insight into Cannabis sativa (Cannabaceae) utilization from 2500-year-old Yanghai Tombs, Xinjiang, China. In: Journal of Ethnopharmacology , Volume 108, Issue 3, December 6, 2006, pp. 414-422, doi: 10.1016 / j.jep.2006.05.034 .
- ↑ The world's oldest marijuana find is a grave object. ( Memento of March 7, 2014 in the Internet Archive ) Message in Shortnews.de of November 30, 2008.
- ↑ Ethan Russo: Cannabinoids as Therapeutics . Ed .: Raphael Mechoulam. Birkhäuser, Basel 2005, ISBN 978-3-7643-7055-8 , chapter: Cannabis in India: ancient lore and modern medicine , p. 1–22 , doi : 10.1007 / 3-7643-7358-X_1 .
- ↑ Herodotus ; Histories , 4, 75
- ↑ Jack Herer , Mathias Bröckers: The rediscovery of the useful plant hemp, cannabis marijuana. 11th edition, Nightshade, 2008, ISBN 3-03788-181-X (German translation)
- ↑ Manfred Fankhauser: Hashish as a drug: on the importance of cannabis sativa in Western medicine. 1996.
- ↑ Cannabis as medicine. In: cannabislegal.de. Retrieved April 2, 2016 .
- ^ A b c Jack Herer: The rediscovery of the useful plant hemp . Edited by Mathias Bröckers (17th edition), Zweiausendeins, Frankfurt am Main 1994, p. 146 ff.
- ^ League of Nations 1925; Records of the Second Opium conference . Volume I, Plenary Meetings, pp. 132-135
- ^ Hemp Museum: The Hemp Conspiracy Entschwört , special exhibition for the Long Night of the Museums on January 31, 2009
- Jump up ↑ New Trillion-Dollar Crop . In: Popular Mechanics . tape 69 , no. 2 . Hearst Magazines, February 1, 1938, p. 238 ( limited preview in Google Book search).
- ↑ Cannabis as medicine: What can pharmacies have in store? In: pharmische-zeitung.de. Avoxa Mediengruppe Deutscher Apotheker GmbH, accessed on November 14, 2017 .
- ↑ a b World Health Organization , Expert Committee on Drug Dependence (Ed.): Critical Review of Extracts and tinctures of cannabis. Department of Essential Medicines and Health Products, 2018 (PDF)
- ^ Luigi L. Romano, Arno Hazekamp: Cannabis Oil: chemical evaluation of an upcoming cannabis-based medicine . In: Cannabinoids 2013; 1 (1): 1-11 .
- ↑ D. Gloss: An Overview of Products and Bias in Research. In: Neurotherapeutics: the journal of the American Society for Experimental NeuroTherapeutics. Volume 12, number 4, October 2015, pp. 731-734, doi: 10.1007 / s13311-015-0370-x , PMID 26202343 , PMC 4604179 (free full text) (review).
- ↑ Laura J. Rovetto, Niccolo V. Aieta: Supercritical carbon dioxide extraction of cannabinoids from Cannabis sativa L. In: The Journal of Supercritical Fluids. 129, 2017, p. 16, doi: 10.1016 / j.supflu.2017.03.014 .
- ↑ CP Grof: Cannabis, from plant to pill. In: British journal of clinical pharmacology. Volume 84, number 11, November 2018, pp. 2463-2467, doi: 10.1111 / bcp.13618 , PMID 29701252 , PMC 6177712 (free full text) (review).
- ^ Houghton Mifflin Harcourt Publishing Company: The American Heritage Dictionary entry: kif .
- ↑ US20170197217A1 - Dual Purpose Female Cannabis Seedless Flower Bud Trimmers, Kief Separators and Methods - Google Patents. In: patents.google.com. Retrieved July 31, 2018 .
- ↑ Rosanna Smart, Jonathan P. Caulkins, Beau Kilmer, Steven Davenport, Greg Midgette: Variation in cannabis potency and prices in a newly legal market: evidence from 30 million cannabis sales in Washington state. In: Addiction. 112, 2017, p. 2167, doi: 10.1111 / add.13886 .
- ↑ MA ElSohly, Z. Mehmedic, S. Foster, C. Gon, S. Chandra, JC Church: Changes in cannabis potency Over the last two Decades (1995-2014): Analysis of Current Data in the United States. In: Biological psychiatry. Volume 79, number 7, April 2016, pp. 613–619, doi: 10.1016 / j.biopsych.2016.01.004 , PMID 26903403 , PMC 4987131 (free full text).
- ↑ Rudolf Hänsel, Ernst Steinegger (Ed.): Pharmakognosie - Phytopharmazie . 9., revised. and act. Edition. Springer, Heidelberg 2010, ISBN 978-3-642-00962-4 .
- ^ Friedrich Kluge: Etymological dictionary of the German language . Ed .: Elmar Seebold. 24., through and exp. Edition. de Gruyter, Berlin, New York 2002, ISBN 3-11-017472-3 , pp. 487 .
- ↑ Effective smoke-free cannabis use. In: alternative-drogenpolitik.de. Retrieved June 16, 2018 .
- ↑ Why a sublingual cannabis tincture is best. In: zamnesia.com. Retrieved June 16, 2018 .
- ↑ Cannabis Tinctures Background & Manufacture. In: 1000seeds.info. Retrieved June 16, 2018 .
- ^ Gerhard founder: Manual of psychopharmacotherapy . Ed .: Otto Benkert. 2., completely revised and act. Edition. Springer, Berlin, Heidelberg 2012, ISBN 978-3-642-19844-1 , pp. 219-222 .
- ↑ FH Meyers, E. Jawetz, A. Goldfien: textbook of pharmacology. For medical students of all stages of study and for doctors Springer-Verlag, 2013, ISBN 3-642-66183-1 , pp. 46–49.
- ↑ S. Rome, Y. Persidsky: Cannabinoid receptor 2: potential role in immunomodulation and neuroinflammation. In: Journal of neuroimmune pharmacology: the official journal of the Society on NeuroImmune Pharmacology. Volume 8, number 3, June 2013, pp. 608-620, doi: 10.1007 / s11481-013-9445-9 , PMID 23471521 , PMC 3663904 (free full text) (review).
- ↑ PDSP Database - UNC . NIMH Psychoactive Drug Screening Program. Retrieved June 11, 2013.
- ↑ Yehiel Gaoni, Raphael Mechoulam: Isolation, structure and partial synthesis of an active constituent of hashish . In: Journal of the American Chemical Society . tape 86 , no. 8 , 1964, pp. 1646–1647 , doi : 10.1021 / ja01062a046 .
- ↑ CA Paronis, SP Nikas, VG Shukla, A. Makriyannis: Δ (9) -Tetrahydrocannabinol acts as a partial agonist / antagonist in mice. In: Behavioral pharmacology. Volume 23, Number 8, December 2012, pp. 802-805, ISSN 1473-5849 . doi: 10.1097 / FBP.0b013e32835a7c4d . PMID 23075707 . PMC 3697741 (free full text).
- ↑ Pertwee RG: The pharmacology of cannabinoid receptors and their ligands: An overview . In: International Journal of Obesity . 30, 2006, pp. S13-S18. doi : 10.1038 / sj.ijo.0803272 . PMID 16570099 .
- ↑ Abir T. El-Alfy, Kelly Ivey, Keisha Robinson, Safwat Ahmed, Mohamed Radwan, Desmond Slade, Ikhlas Khan, Mahmoud ElSohly: Antidepressant-like effect of Δ9-tetrahydrocannabinol and other cannabinoids isolated from Cannabis sativa L . In: Pharmacology, Biochemistry and Behavior . 95, No. 4, 2010, pp. 434-42. doi : 10.1016 / j.pbb.2010.03.004 . PMID 20332000 . PMC 2866040 (free full text).
- ^ EP de Meijer, M. Bagatta, A. Carboni, P. Crucitti, VM Moliterni, P. Ranalli, G. Mandolino: The inheritance of chemical phenotype in Cannabis sativa L. In: Genetics. Volume 163, Number 1, January 2003, pp. 335-346, PMID 12586720 , PMC 1462421 (free full text).
- ↑ David Castle, Robin M. Murray, Deepak C. D'Souza: Marijuana and Madness . Cambridge University Press, 2011, ISBN 978-1-139-50267-2 , pp. 40 ( limited preview in Google Book search).
- ↑ Harlequin Medical Cannabis Strain Guide. (No longer available online.) In: harborsidehealthcenter.com. Archived from the original on March 30, 2016 ; Retrieved April 2, 2016 .
- ↑ McCallum ND, Yagen B, Levy S, Mechoulam R: Cannabinol: a rapidly formed metabolite of delta-1- and delta-6-tetrahydrocannabinol In: Experientia. Volume 31, Number 5, May 1975, pp. 520-521, PMID 1140243 .
- ↑ P. Pacher, S. Bátkai, G. Kunos: The endocannabinoid system as an emerging target of pharmacotherapy. In: Pharmacological reviews. Volume 58, number 3, September 2006, pp. 389-462, doi: 10.1124 / pr.58.3.2 , PMID 16968947 , PMC 2241751 (free full text) (review).
- ↑ Fidelia Cascini, Carola Aiello, Gianluca Di Tanna: Increasing delta-9-tetrahydrocannabinol (Δ-9-THC) content in herbal cannabis over time: systematic review and meta-analysis . In: Current Drug Abuse Reviews . tape 5 , no. 1 , March 1, 2012, p. 32-40 , doi : 10.2174 / 1874473711205010032 , PMID 22150622 .
- ^ Zerrin Atakan: Cannabis, a complex plant: different compounds and different effects on individuals . In: Therapeutic Advances in Psychopharmacology . tape 2 , no. 6 , December 1, 2012, p. 241-254 , doi : 10.1177 / 2045125312457586 , PMC 3736954 (free full text).
- ↑ emcdda.europa.eu An overview of cannabis potency in Europe . EMCDDA, Lisbon, January 2004, pp. 38–48, Figures 10, 11, 12, 14.
- ↑ Further consideration of the classification of cannabis under the Misuse of Drugs Act 1971 (PDF) badscience.net. P. 14. Retrieved July 28, 2012.
- ↑ Drug supply and market. (PDF) In: European Drugs Report 2017. European Monitoring Center for Drugs and Drug Addiction , p. 23 , accessed on January 19, 2018 : “The analysis of the indexed trends in those countries that regularly transmit relevant data shows that the active substance content (ie the content of tetrahydrocannabinol, THC) of cannabis herb and cannabis resin increased sharply between 2006 and 2014 and stabilized in 2015. "
- ↑ Drug supply and market. (PDF) In: European Drugs Report 2017. European Monitoring Center for Drugs and Drug Addiction, p. 21 , accessed on 19 January 2018 .
- ↑ a b c Illegal drugs: cannabis. German headquarters for addiction issues V., accessed March 1, 2013 .
- ↑ a b c drug dictionary: cannabis. Federal Center for Health Education, accessed on March 1, 2013 .
- ↑ Cannabis / THC. (No longer available online.) Drug-Infopool.de, formerly in the original ; accessed on March 1, 2013 . ( Page no longer available , search in web archives )
- ↑ Entry on Tetrahydrocannabinole. In: Römpp Online . Georg Thieme Verlag, accessed on August 21, 2011.
- ↑ a b c d WHO Expert Committee on Drug Dependence: Critical Review - Cannabis and cannabis resin. (PDF) World Health Organization, 2018, accessed April 2, 2019 .
- ↑ Zuzana Justinová, Sergi Ferré, Godfrey H. Redhi, Paola Mascia, Jessica Stroik, Davide Quarta, Sevil Yasar, Christa E. Müller, Rafael Franco, Steven R. Goldberg: Reinforcing and neurochemical effects of cannabinoid CB1 receptor agonists, but not cocaine , are altered by an adenosine A2A receptor antagonist . In: Addiction biology . tape 16 , no. 3 , July 1, 2011, p. 405-415 , doi : 10.1111 / j.1369-1600.2010.00258.x , PMC 3115444 (free full text).
- ^ Gary L. Wenk: Does Coffee Enhance Marijuana? In: psychologytoday.com. Psychology Today , May 9, 2014, accessed April 2, 2016 .
- ↑ AM Wycoff, J. Metrik, TJ Trull: Affect and cannabis use in daily life: a review and recommendations for future research. In: Drug and alcohol dependence. Volume 191, 10 2018, pp. 223-233, doi: 10.1016 / j.drugalcdep.2018.07.001 , PMID 30149283 , PMC 6201696 (free full text) (review).
- ↑ Wolfgang Ferner, Peter Xanke: Alcohol and drugs in road traffic - measuring procedures, fine proceedings, criminal proceedings . Deubner Verlag, 2006, ISBN 3-88606-633-9 , p. 64 ( limited preview in Google Book search).
- ↑ Cannabis - drugscouts.de. In: drugscouts.de. Retrieved June 9, 2015 .
- ↑ Clara Touriño, Andreas Zimmer, Olga Valverde, Dawn N. Albertson: THC Prevents MDMA Neurotoxicity in Mice. In: PLoS ONE. 5, 2010, p. E9143, doi: 10.1371 / journal.pone.0009143 .
- ^ KC Morley, KM Li, GE Hunt, PE Mallet, IS McGregor: Cannabinoids prevent the acute hyperthermia and partially protect against the 5-HT depleting effects of MDMA ("Ecstasy") in rats. In: Neuropharmacology . Volume 46, Number 7, June 2004, pp. 954-965, doi: 10.1016 / j.neuropharm.2004.01.002 . PMID 15081792 .
- ↑ GJ Dumont, C. Kramers, FC Sweep, DJ Touw, JG van Hasselt, M. de Kam, JM van Gerven, JK Buitelaar, RJ Verkes: Cannabis coadministration potentiates the effects of "ecstasy" on heart rate and temperature in humans. In: Clinical pharmacology and therapeutics. Volume 86, Number 2, August 2009, pp. 160-166, doi: 10.1038 / clpt.2009.62 . PMID 19440186 , PDF, pp. 121-138. (PDF) accessed on October 23, 2015.
- ↑ Diana L. Cichewicz: Synergistic interactions between cannabinoid and opioid analgesics . In: Life Sciences . tape 74 , no. 11 , January 30, 2004, p. 1317-1324 , doi : 10.1016 / j.lfs.2003.09.038 , PMID 14706563 .
- ↑ David J Nutt, Leslie A King, Lawrence D Phillips: Drug harms in the UK: a multicriteria decision analysis. In: The Lancet. 376, 2010, pp. 1558-1565, doi: 10.1016 / S0140-6736 (10) 61462-6 .
- ↑ Mark J. Pletcher, Eric Vittinghoff, Ravi Kalhan, Joshua Richman, Monika Safford, Stephen Sidney, Feng Lin, Stefan Kertesz: Association Between Marijuana Exposure and Pulmonary Function Over 20 Years . In: Journal of the American Medical Association . tape 307 , no. 2 , January 11, 2012, p. 173–181 , doi : 10.1001 / jama.2011.1961 (English, online ).
- ↑ a b M. Underner, T. Urban, J. Perriot, I. de Chazeron, JC Meurice: Cannabis smoking and lung cancer. In: Revue des maladies respiratoires. Volume 31, number 6, June 2014, pp. 488-498, doi: 10.1016 / j.rmr.2013.12.002 . PMID 25012035 (Review).
- ^ National Institute on Drug Abuse: What are marijuana's effects on lung health? Retrieved April 2, 2019 .
- ^ A b M. Joshi, A. Joshi, T. Bartter: Marijuana and lung diseases. In: Current opinion in pulmonary medicine. Volume 20, number 2, March 2014, pp. 173-179, doi: 10.1097 / MCP.0000000000000026 . PMID 24384575 .
- ^ A b Russell C. Callaghan, Peter Allebeck, Anna Sidorchuk: Marijuana use and risk of lung cancer: a 40-year cohort study . In: Cancer Causes & Control . tape 24 , no. 10 , October 2013, ISSN 0957-5243 , p. 1811–1820 , doi : 10.1007 / s10552-013-0259-0 ( springer.com [accessed September 10, 2019]).
- ↑ a b WHO Expert Committee on Drug Dependence: Critical Review - Cannabis and cannabis resin. (PDF) World Health Organization, 2018, accessed April 2, 2019 .
- ↑ A. Hazekamp, R. Ruhaak, L. Zuurman, J. van Gerven, R. Verpoorte: Evaluation of a vaporizing device (Volcano) for the pulmonary administration of tetrahydrocannabinol . In: Journal of Pharmaceutical Sciences . tape 95 , no. 6 , June 2006, ISSN 0022-3549 , p. 1308-1317 , doi : 10.1002 / jps.20574 , PMID 16637053 (English).
- ↑ National Cancer Institute at the National Institutes of Health : Cannabis and Cannabinoids (PDQ®) (English)
- ^ Institute of Medicine, Marijuana and Health, Washington, DC: Marijuana vs Tobacco smoke compositions. In: erowid.org. National Academy Press, 1988, accessed March 7, 2016 .
- ^ Robert Melamede: Cannabis and Tobacco Smoke Are Not Equally Carcinogenic. In: Harm Reduction Journal. Volume 2, 2005, No. 21, PMC 1277837 (free full text) (English).
- ↑ M. Joshi, A. Joshi, T. Bartter: Marijuana and lung diseases . In: Current opinion in pulmonary medicine . tape 20 , no. 2 , March 2014, p. 173-179 , doi : 10.1097 / MCP.0000000000000026 , PMID 24384575 (English, review article).
- ↑ JR Biehl, EL Burnham: Cannabis Smoking in 2015: A Concern for Lung Health? In: Chest. Volume 148, number 3, September 2015, pp. 596-606, doi: 10.1378 / chest.15-0447 , PMID 25996274 , PMC 4556119 (free full text) (review).
- ↑ B. Misiak, F. Stramecki, Gawęda, K. Prochwicz, MM Sąsiadek, AA Moustafa, D. Fryd: Interactions Between Variation in Candidate Genes and Environmental Factors in the Etiology of Schizophrenia and Bipolar Disorder: a Systematic Review. In: Molecular neurobiology. Volume 55, number 6, June 2018, pp. 5075-5100, doi: 10.1007 / s12035-017-0708-y , PMID 28822116 , PMC 5948257 (free full text) (review).
- ↑ a b c T. H. Moore, S. Zammit, A. Lingford-Hughes, TR Barnes, PB Jones, M. Burke, G. Lewis: Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. In: Lancet. Volume 370, Number 9584, July 2007, pp. 319-328, doi: 10.1016 / S0140-6736 (07) 61162-3 , PMID 17662880 (review).
- ^ JA McLaren, E. Silins, D. Hutchinson, RP Mattick, W. Hall: Assessing evidence for a causal link between cannabis and psychosis: a review of cohort studies. In: The International journal on drug policy. Volume 21, Number 1, January 2010, pp. 10-19, doi: 10.1016 / j.drugpo.2009.09.001 , PMID 19783132 (review).
- ↑ S. Minozzi, M. Davoli, AM Bargagli, L. Amato, S. Vecchi, CA Perucci: An overview of systematic reviews on cannabis and psychosis: discussing apparently conflicting results. In: Drug and alcohol review. Volume 29, Number 3, May 2010, pp. 304-317, doi: 10.1111 / j.1465-3362.2009.00132.x , PMID 20565524 (review).
- ^ A b Daniel Cressey: Drug Policy: The Cannabis Experiment. Translation from Nature . In: Spektrum.de. Spectrum of Science , September 2, 2015, accessed September 6, 2015 .
- ↑ M. Di Forti, D. Quattrone et al. a .: The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. In: The lancet. Psychiatry. [Electronic publication before printing] March 2019, doi: 10.1016 / S2215-0366 (19) 30048-3 , PMID 30902669 (free full text).
- ↑ R. Kuepper, PD Morrison, J. van Os, RM Murray, G. Kenis, C. Henquet: Does dopamine mediate the psychosis-inducing effects of cannabis? A review and integration of findings across disciplines. In: Schizophrenia research. Volume 121, number 1-3, August 2010, pp. 107-117, doi: 10.1016 / j.schres.2010.05.031 , PMID 20580531 (review).
- ↑ Musa Basser Sami, Eugenii A. Rabiner, Sagnik Bhattacharyya: Does cannabis affect dopaminergic signaling in the human brain? A systematic review of evidence to date. In: European Neuropsychopharmacology. 25, 2015, p. 1201, doi: 10.1016 / j.euroneuro.2015.03.011 .
- ↑ a b c d e World Health Organization , Expert Committee on Drug Dependence (Ed.): Critical Review of Cannabis and cannabis resin (PDF) (PDF) , Department of Essential Medicines and Health Products, Section 3: Toxicology, 1.8 Mental health , P. 7, 2018.
- ↑ a b Euphrosyne Gouzoulis-Mayfrank : Comorbidity Psychosis and Addiction - Basics and Practice: With manuals for psychoeducation and behavioral therapy . Springer-Verlag, 2013, ISBN 978-3-662-12172-6 , p. 237.
- ↑ a b Laura C. Andreae: Cannabis use and schizophrenia: Chicken or egg ?. In: Science Translational Medicine. 10, 2018, p. Eaav0342, doi: 10.1126 / scitranslmed.aav0342 .
- Jump up ↑ Martin Frisher, Ilana Crome, Orsolina Martino, Peter Croft: Assessing the impact of cannabis use on trends in diagnosed schizophrenia in the United Kingdom from 1996 to 2005. In: Schizophrenia Research. 113, 2009, p. 123, doi: 10.1016 / j.schres.2009.05.031 .
- ↑ L. Degenhardt, W. Hall, M. Lynskey: Testing hypotheses about the relationship between cannabis use and psychosis. In: Drug and alcohol dependence. Volume 71, Number 1, July 2003, pp. 37-48, PMID 12821204 .
- ^ M. Rotermann, R. Macdonald: Analysis of trends in the prevalence of cannabis use in Canada, 1985 to 2015. In: Health reports. Volume 29, Number 2, February 2018, pp. 10-20, PMID 29465739 .
- ↑ H. Bugra, C. Rapp, E. Studerus, J. Aston, S. Borgwardt, A. Riecher-Rössler: Can cannabis increase the risk of schizophrenic psychosis? In: Advances in Neurology · Psychiatry . tape 80 , no. 11 , November 1, 2012, p. 635-643 , doi : 10.1055 / s-0032-1325415 .
- ↑ Heekeren: Does cannabis use lead to schizophrenia? In: PRACTICE . tape 100 , no. 22 , November 1, 2011, p. 1361-1367 , doi : 10.1024 / 1661-8157 / a000714 .
- ↑ David M. Semple, Andrew M. McIntosh, Stephen M. Lawrie: Cannabis as a risk factor for psychosis: systematic review . In: Journal of Psychopharmacology . tape 19 , no. 2 , March 1, 2005, p. 187-194 , doi : 10.1177 / 0269881105049040 ( sagepub.com ).
- ↑ J. Vaucher, BJ Keating, AM Lasserre, W. Gan, DM Lyall, J. Ward, DJ Smith, JP Pell, N. Sattar, G. Paré, MV Holmes: Cannabis use and risk of schizophrenia: a Mendelian randomization study . In: Molecular psychiatry. [electronic publication before printing] January 2017, doi: 10.1038 / mp.2016.252 , PMID 28115737 , online (accessed July 4, 2017).
- ↑ J. Zheng, D. Baird, MC Borges, J. Bowden, G. Hemani, P. Haycock, DM Evans, GD Smith: Recent Developments in Mendelian Randomization Studies. In: Current epidemiology reports. Volume 4, number 4, 2017, pp. 330-345, doi: 10.1007 / s40471-017-0128-6 , PMID 29226067 , PMC 5711966 (free full text) (review).
- ^ National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda: The Health Effects of Cannabis and Cannabinoids. The Current State of Evidence and Recommendations for Research National Academies Press, 2017, ISBN 9780309453042 , pp. 291-295.
- ↑ a b J. A. Pasman, KJ Verweij u. a .: GWAS of lifetime cannabis use reveals new risk loci, genetic overlap with psychiatric traits, and a causal influence of schizophrenia. In: Nature Neuroscience . Volume 21, number 9, September 2018, pp. 1161–1170, doi: 10.1038 / s41593-018-0206-1 , PMID 30150663 , PMC 6386176 (free full text).
- ^ A b E. Hoch, U. Bonnet, R. Thomasius, F. Ganzer, U. Havemann-Reinecke, UW Preuss: Risks associated with the non-medicinal use of cannabis . In: Deutsches Ärzteblatt international . tape 112 , no. April 16 , 2015, p. 271–278 , doi : 10.3238 / arztebl.2015.0271 , PMID 25939318 , PMC 4442549 (free full text) - ( online version in German: Risks associated with non-medical use of cannabis , PDF - review article).
- ^ A b I. Pacheco-Colón, JM Limia, R. Gonzalez: Nonacute effects of cannabis use on motivation and reward sensitivity in humans: A systematic review. In: Psychology of addictive behaviors: journal of the Society of Psychologists in Addictive Behaviors. Volume 32, number 5, 08 2018, pp. 497-507, doi: 10.1037 / adb0000380 , PMID 29963875 , PMC 6062456 (free full text).
- ^ KR Hefner, MJ Starr, JJ Curtin: Altered subjective reward valuation among drug-deprived heavy marijuana users: Aversion to uncertainty. In: Journal of abnormal psychology. Volume 125, number 1, January 2016, pp. 138–150, doi: 10.1037 / enth0000106 , PMID 26595464 , PMC 4701603 (free full text).
- Jump up ↑ E. van de Giessen, JJ Weinstein, CM Cassidy, M. Haney, Z. Dong, R. Ghazzaoui, N. Ojeil, LS Kegeles, X. Xu, NP Vadhan, ND Volkow, M. Slifstein, A. Abi- Dargham: Deficits in striatal dopamine release in cannabis dependence. In: Molecular psychiatry. [Electronic publication before printing] March 2016, doi: 10.1038 / mp.2016.21 , PMID 27001613 .
- ↑ K. MacDonald, K. Pappas: WHY NOT POT ?: A Review of the Brain-based Risks of Cannabis. In: Innovations in clinical neuroscience. Volume 13, Number 3-4, 2016 Mar-Apr, pp. 13-22, PMID 27354924 , PMC 4911936 (free full text) (review).
- ^ MA Bloomfield, AH Ashok, ND Volkow, OD Howes: The effects of Δ (9) -tetrahydrocannabinol on the dopamine system. In: Nature. Volume 539, number 7629, 11 2016, pp. 369–377, doi: 10.1038 / nature20153 , PMID 27853201 , PMC 5123717 (free full text) (review).
- ↑ Review in: MA Bloomfield, CJ Morgan, A. Egerton, S. Kapur, HV Curran, OD Howes: Dopaminergic function in cannabis users and its relationship to cannabis-induced psychotic symptoms. In: Biological psychiatry. Volume 75, number 6, March 2014, pp. 470–478, doi: 10.1016 / j.biopsych.2013.05.027 , PMID 23820822 (free full text under DOI link).
- ^ J. Jacobus, D. Goldenberg, CE Wierenga, NJ Tolentino, TT Liu, SF Tapert: Altered cerebral blood flow and neurocognitive correlates in adolescent cannabis users. In: Psychopharmacology. Volume 222, number 4, August 2012, pp. 675-684, doi: 10.1007 / s00213-012-2674-4 , PMID 22395430 , PMC 3510003 (free full text).
- ↑ a b c d e World Health Organization , Expert Committee on Drug Dependence (Ed.): Critical Review of Cannabis and cannabis resin (PDF) (PDF) , Department of Essential Medicines and Health Products, Section 3: Toxicology, 1.7 Effects on cognitive function, p. 6, 2018.
- ↑ M. Rocchetti, A. Crescini, S. Borgwardt, E. Caverzasi, P. Politi, Z. Atakan, P. Fusar-Poli: Is cannabis neurotoxic for the healthy brain? A meta-analytical review of structural brain alterations in non-psychotic users. In: Psychiatry and clinical neurosciences. Volume 67, Number 7, November 2013, pp. 483-492, doi: 10.1111 / pcn.12085 , PMID 24118193 (review).
- ↑ M. Maccarrone, M. Guzmán, K. Mackie, P. Doherty, T. Harkany: Programming of neural cells by (endo) cannabinoids: from physiological rules to emerging therapies. In: Nature reviews. Neuroscience. Volume 15, Number 12, December 2014, pp. 786-801, doi: 10.1038 / nrn3846 , PMID 25409697 (review).
- ↑ P. Campolongo, V. Trezza, M. Palmery, L. Trabace, V. Cuomo: Developmental exposure to cannabinoids causes subtle and enduring neurofunctional alterations. In: International review of neurobiology. Volume 85, 2009, pp. 117-133, doi: 10.1016 / S0074-7742 (09) 85009-5 , PMID 19607965 (review).
- ↑ S. Anavi-Goffer, J. Mulder: The Polarized life of the endocannabinoid system development in CNS. In: Chembiochem: a European journal of chemical biology. Volume 10, Number 10, July 2009, pp. 1591-1598, doi: 10.1002 / cbic.200800827 , PMID 19533710 (review).
- ^ DI Lubman, A. Cheetham, M. Yücel: Cannabis and adolescent brain development. In: Pharmacology & therapeutics. Volume 148, April 2015, pp. 1-16, doi: 10.1016 / j.pharmthera.2014.11.009 , PMID 25460036 (review).
- ↑ B. Chadwick, ML Miller, YL Hurd: Cannabis Use during Adolescent Development: Susceptibility to Psychiatric Illness. In: Frontiers in psychiatry. Volume 4, 2013, p. 129, doi: 10.3389 / fpsyt.2013.00129 , PMID 24133461 , PMC 3796318 (free full text) (review).
- ↑ DT Malone, MN Hill, T. Rubino: Adolescent cannabis use and psychosis: epidemiology and neurodevelopmental models. In: British journal of pharmacology. Volume 160, number 3, June 2010, pp. 511-522, doi: 10.1111 / j.1476-5381.2010.00721.x , PMID 20590561 , PMC 2931552 (free full text) (review).
- ↑ N. Realini, T. Rubino, D. Parolaro: Neurobiological alterations at adult age triggered by adolescent exposure to cannabinoids. In: Pharmacological research: the official journal of the Italian Pharmacological Society. Volume 60, Number 2, August 2009, pp. 132-138, doi: 10.1016 / j.phrs.2009.03.006 , PMID 19559364 (review).
- ↑ J Hirvonen, RS Goodwin, CT Li, GE Terry, SS Zoghbi: Reversible and regionally selective downregulation of brain cannabinoid CB1 receptors in chronic daily cannabis smokers . In: Molecular Psychiatry . tape 17 , no. 6 , June 2012, ISSN 1359-4184 , p. 642–649 , doi : 10.1038 / mp.2011.82 , PMID 21747398 , PMC 3223558 (free full text).
- ↑ J Hirvonen, RS Goodwin, CT Li, GE Terry, SS Zoghbi: Reversible and regionally selective downregulation of brain cannabinoid CB1 receptors in chronic daily cannabis smokers . In: Molecular Psychiatry . tape 17 , no. 6 , June 2012, ISSN 1359-4184 , p. 642–649 , doi : 10.1038 / mp.2011.82 , PMID 21747398 , PMC 3223558 (free full text).
- ↑ a b J. Wrege, A. Schmidt, A. Walter, R. Smieskova, K. Bendfeldt, EW Radue, UE Lang, S. Borgwardt: Effects of cannabis on impulsivity: a systematic review of neuroimaging findings. In: Current pharmaceutical design. Volume 20, number 13, 2014, pp. 2126-2137, PMID 23829358 , PMC 4052819 (free full text) (review).
- ↑ A. Batalla, S. Bhattacharyya, M. Yücel, P. Fusar-Poli, JA Crippa, S. Nogué, M. Torrens, J. Pujol, M. Farré, R. Martin-Santos: Structural and functional imaging studies in chronic cannabis users: a systematic review of adolescent and adult findings. In: PloS one. Volume 8, number 2, 2013, p. E55821, PMID 23390554 , PMC 3563634 (free full text) (review).
- ↑ a b S. J. Broyd, HH van Hell, C. Beale, M. Yucel, N. Solowij: Acute and Chronic Effects of Cannabinoids on Human Cognition-A Systematic Review. In: Biological psychiatry. Volume 79, Number 7, April 2016, pp. 557-567, doi: 10.1016 / j.biopsych.2015.12.002 , PMID 26858214 (review).
- ^ MH Meier, A. Caspi, A. Ambler, H. Harrington, R. Houts, RS Keefe, K. McDonald, A. Ward, R. Poulton, TE Moffitt : Persistent cannabis users show neuropsychological decline from childhood to midlife. In: Proceedings of the National Academy of Sciences . Volume 109, number 40, October 2012, pp. E2657 – E2664, doi: 10.1073 / pnas.1206820109 , PMID 22927402 , PMC 3479587 (free full text).
- ^ TE Moffitt , MH Meier, A. Caspi, R. Poulton: Reply to Rogeberg and Daly: No evidence that socioeconomic status or personality differences confound the association between cannabis use and IQ decline. In: Proceedings of the National Academy of Sciences . Volume 110, Number 11, March 2013, pp. E980-E982, PMID 23599952 , PMC 3600438 (free full text).
- ↑ Fried PA, Watkinson B, Gray R. (2006): [ Neurocognitive consequences of marihuana - a comparison with pre-drug performance .] Neurotoxicology and Teratology, Volume 27, Issue 2, pp. 231-9
- ↑ JC Scott, ST Slomiak, JD Jones, AF Rosen, TM Moore, RC Gur: Association of Cannabis With Cognitive Functioning in Adolescents and Young Adults: A Systematic Review and Meta-analysis. In: JAMA psychiatry. Volume 75, number 6, June 2018, pp. 585-595, doi: 10.1001 / jamapsychiatry.2018.0335 , PMID 29710074 , PMC 6137521 (free full text).
- ^ RS Gable: Drugs and society: US public policy . Rowman & Littlefield, Lanham, Md. 2006, ISBN 978-0-7425-4245-7 , chapter "Acute toxicity of drugs versus regulatory status" , p. 149–162, diagram p. 155 ( limited preview in Google Book search).
- ↑ EB Oleson, JF Cheer: A brain on cannabinoids: the role of dopamine release in reward seeking . In: Cold Spring Harbor perspectives in medicine . tape 2 , no. 8 , 2012, p. 1–13 , doi : 10.1101 / cshperspect.a012229 , PMID 22908200 , PMC 3405830 (free full text) - (English, review article).
- Jump up ↑ E. van de Giessen, JJ Weinstein, CM Cassidy, M. Haney, Z. Dong, R. Ghazzaoui, N. Ojeil, LS Kegeles, X. Xu, NP Vadhan, ND Volkow, M. Slifstein, A. Abi- Dargham: Deficits in striatal dopamine release in cannabis dependence . In: Molecular Psychiatry . tape 22 , no. 1 , January 2017, p. 68–75 , doi : 10.1038 / mp.2016.21 , PMID 27001613 , PMC 5033654 (free full text) - (electronic publication before printing, March 2016).
- ^ A b Eva Hoch, Miriam Schneider: Cannabis: Potential and Risks. A Scientific Analysis (CaPRis) - Brief Report. (PDF) Federal Ministry of Health, November 2018, accessed on April 5, 2019 .
- ↑ Heike Zurhold, Uwe Verthein, Alesha Lara Savinsky: Medical Rehabilitation drug sick according to § 35 Narcotics Act ( "therapy instead of punishment"): Efficacy and trends - short report. (PDF) Federal Ministry of Health, February 7, 2019, accessed on April 5, 2019 .
- ↑ a b Heike Zurhold, Uwe Verthein, Alescha Lara Savinsky: Medical Rehabilitation drug patient according to § 35 Narcotics ( "therapy instead of punishment"): efficacy and trends. (PDF) Federal Ministry of Health, February 7, 2019, accessed on April 5, 2019 .
- ↑ a b World Health Organization , Expert Committee on Drug Dependence (Ed.): Critical Review of Cannabis and cannabis resin (PDF) (PDF) , Department of Essential Medicines and Health Products, Section 3: Toxicology, 1.6 Fertility and teratogenesis, p . 6, 2018.
- ↑ DR ENGLISH, GK HULSE, E. MILNE, CDJ HOLMAN, CI BOWER: Maternal cannabis use and birth weight: a meta-analysis . In: Addiction . tape 92 , no. November 11 , 1997, ISSN 0965-2140 , p. 1553-1560 , doi : 10.1111 / j.1360-0443.1997.tb02875.x .
- ↑ Shalem Y. Leemaqz, Gustaaf A. Dekker, Lesley M. McCowan, Louise C. Kenny, Jenny E. Myers: Maternal marijuana use has independent effects on risk for spontaneous preterm birth but not other common late pregnancy complications . In: Reproductive Toxicology . tape 62 , July 2016, ISSN 0890-6238 , p. 77-86 , doi : 10.1016 / j.reprotox.2016.04.021 .
- ^ Eva Hoch, Miriam Schneider, Chris Maria Friemel (eds.): Cannabis: Potential and Risk - A Scientific Inventory . Springer, Heidelberg 2019, ISBN 978-3-662-57291-7 , doi : 10.1007 / 978-3-662-57291-7 (478 pages, bundesgesundheitsministerium.de [PDF]). see page 57, 2.7 Limitations.
- ↑ Prof. Dr. Axel Tschentscher, LL.M., MA: DFR - BVerfGE 90, 145 - Cannabis. Retrieved March 11, 2018 .
- ↑ Mahrenholz, Böckenförde, Klein, Graßhof, Kruis, Kirchhof, Winter, Summer: BVerfG, decision of the Second Senate of March 9, 1994 - 2 BvL 43/92 - Rn. (1-259) . Ed .: Federal Constitutional Court. March 9, 1994.
- ^ ML Miller, YL Hurd: Testing the Gateway Hypothesis. In: Neuropsychopharmacology . Volume 42, number 5, 04 2017, pp. 985-986, doi: 10.1038 / npp.2016.279 , PMID 28096528 , PMC 5506797 (free full text).
- ↑ Cannabis basic information. (PDF; 431 kB) (No longer available online.) Deutsche Hauptstelle für Suchtfragen e. V. , 2004, archived from the original on March 27, 2015 ; accessed on September 20, 2019 .
- ↑ Wolfgang Ferner, Peter Xanke: Alcohol and drugs in road traffic - measuring procedures, fine proceedings, criminal proceedings . Deubner, Recht und Praxis, Cologne 2006, ISBN 978-3-88606-633-9 , p. 68 ( limited preview in Google Book search).
- ↑ Jörg Fengler (Ed.): Handbook of Addiction Treatment: Advice, Therapy, Prevention . ecomed-Storck, Landsberg 2002, ISBN 978-3-609-51980-7 , p. 228 ( limited preview in Google Book search).
- ↑ Orrin Devinsky, Maria R. Cilio, Helen Cross, Javier Fernandez-Ruiz, Jacqueline French, Charlotte Hill, Russell Katz, Vincenzo Di Marzo, Didier Jutras-Aswad, William G. Notcutt, Jose Martinez-Orgado, Philip J. Robson, Brian G. Rohrback, Elizabeth Thiele, Benjamin Whalley, Daniel Friedman: Cannabidiol: Pharmacology and potential therapeutic role in epilepsy and other neuropsychiatric disorders . In: Epilepsia . tape 55 , no. 6 , June 1, 2014, p. 791-802 , doi : 10.1111 / epi.12631 , PMC 4707667 (free full text).
- ↑ Jonathon Burch: Afghanistan now world's top cannabis source: UN . Report dated March 31, 2010 at Reuters.com .
- ↑ Entry on cannabis. In: Römpp Online . Georg Thieme Verlag, accessed on May 3, 2011.
- ↑ Cannabis products are getting stronger . Spiegel Online , December 30, 2018; accessed on January 16, 2019
- ↑ Tom P. Freeman, Teodora Groshkova, Andrew Cunningham, Roumen Sedefov, Paul Griffiths, Michael T. Lynskey: Increasing potency and price of cannabis in Europe, 2006-16 . In: Wiley Online Library (Ed.): Addiction . August. doi : 10.1111 / add.14525 .
- ↑ Marion Weigl, Martin Busch, Alexander Grabenhofer-Eggerth, Ilonka Horvath, Charlotte Klein, Elisabeth Türscherl: Report on the drug situation 2014 . Published by Gesundheit Österreich GmbH on behalf of the EMCDDA , Lisbon and the BMG . Vienna 2014, ISBN 978-3-85159-187-3 ( PDF; 2.4 MB ).
- ^ Marion Weigl, Judith Anzenberger, Martin Busch, Ilonka Horvath, Elisabeth Türscherl: Report on the drug situation 2015 . Published by Gesundheit Österreich GmbH on behalf of the EMCDDA , Lisbon and the BMG . Vienna 2015, ISBN 978-3-85159-194-1 ( PDF; 2.8 MB ).
- ↑ Drug Commissioner of the Federal Government : Situation in Germany. (No longer available online.) In: drogenbeauftragte.de. January 12, 2016, archived from the original on June 15, 2016 ; Retrieved April 2, 2016 .
- ↑ Per Hinrichs: Germany becomes a stoner republic. In: Welt Online . November 25, 2013, accessed April 2, 2016 .
- ↑ Hemp: The green gold rush in Austria . In: The press . ( diepresse.com [accessed March 6, 2018]).
- ↑ No blooming: hemp shops in Vienna . In: profil.at . July 7, 2014 ( profil.at [accessed March 6, 2018]).
- ↑ Michael O'Hare, Daniel L. Sanchez, Peter Alstone: Environmental Risks and Opportunities in Cannabis Cultivation. (PDF) In: lcb.wa.gov. BOTEC Analysis, June 28, 2013, accessed on January 21, 2017 (PDF; 3.9 MB, English).
- ^ Cheryl Kaiser, Christy Cassady, Matt Ernst: Industrial Hemp Production. (PDF) In: uky.edu. University of Kentucky College of Agriculture, Food and Environment, September 2015, accessed January 21, 2017 (PDF; 1.2 MB, English).
- ↑ a b c Based on data from: The cannabis consumption of adolescents and young adults in Germany 2014 . Federal Center for Health Education, 2015
- ↑ German headquarters for addiction issues e. V .: DHS Yearbook Addiction 2018. (PDF) Deutsche Hauptstelle für Suchtfragen e. V., March 28, 2018, accessed April 3, 2018 .
- ^ Child and Adolescent Health Research Unit (CAHRU): Health Policy for Children and Adolescents, No. 5. (PDF) 2006, p. 136 , accessed on March 29, 2016 .
- ^ Health Policy for Children and Adolescents, No. 7. (PDF) (No longer available online.) In: euro.who.int. Child and Adolescent Health Research Unit (CAHRU), 2014, p. 172 , archived from the original on March 29, 2016 ; accessed on March 29, 2016 .
- ↑ Addiction monitoring Switzerland: Cannabis overview - current situation. 2014, accessed March 29, 2016 .
- ↑ C. Donath, D. Baier, E. Graessel, T. Hillemacher: Substance consumption in adolescents with and without an immigration background: a representative study — What part of an immigration background is protective against binge drinking? In: BMC Public Health . tape 16 , 2016, p. 1157 , doi : 10.1186 / s12889-016-3796-0 , PMID 27842534 .
- ↑ a b Scientific Services of the German Bundestag : Legalization of Cannabis: Effects on the Number of Users in Selected Countries, file number: WD 9-3000-072 / 19, 2019
- ↑ Eastwood, N. et al. (2016): A Quiet Revolution: Decriminalization Across the Globe. In: tni.org. August 22, 2017, accessed February 9, 2020 .
- ^ A b Association of Drugs and Addiction Aid eV: Decriminalization of cannabis users and structuring of regulation, page 10. In: fdr-online.info. November 21, 2019, accessed February 9, 2020 .
- ↑ Friederike Neugebauer: fdr + press release “Decriminalization of cannabis users”. In: fdr-online.info. January 30, 2020, accessed February 9, 2020 .
- ↑ Sven Reichardt , Authenticity and Community. Left alternative life in the seventies and early eighties, Berlin 2014, p. 834f.
- ^ Patrick Matthews: Cannabis Culture. Bloomsbury, 2003, ISBN 978-0-7475-6614-4 .
- ↑ Two thirds of Germans are against cannabis legalization. Der Spiegel, November 13, 2017, accessed on September 21, 2018 .
- ↑ infratest dimap: Legalization of Cannabis 2018. (PDF) 2018, accessed on April 2, 2019 .
- ↑ Supraregional: Study by the Hanfverband: Legalization of cannabis would bring in billions annually. In: infranken.de . November 16, 2018, accessed April 6, 2019 .
- ↑ Doctors newspaper : Hash forecast: Cannabis prohibition costs the state billions. In: aerztezeitung.de. November 20, 2018, accessed April 6, 2019 .
- ↑ Cannabis and driving: a review of the literature and commentary (No.12). (No longer available online.) In: webarchive.nationalarchives.gov.uk. Archived from the original on October 23, 2008 ; accessed on June 9, 2015 .
- ↑ Wolfgang Müller: Driving safety: Risk-conscious thanks to hash? In: Focus Online . July 14, 2013, accessed May 16, 2015 .
- ↑ Franjo Grotenhermen: Fitness to drive, fitness to drive and cannabis use . March 26, 1999, doi : 10.1007 / 978-3-642-56070-5_9 .
- ^ NHTSA Releases Two New Studies on Impaired Driving on US Roads , Department of Transportation's National Highway Traffic Safety Administration. February 6, 2015.
- ↑ Stoned drivers are a lot safer than drunk ones, new federal data show , Washington Post. February 9, 2015. Accessed February 13, 2015.
- ^ R. Compton, A. Berning: Drug and Alcohol Crash Risk . In: Department of Transportation's National Highway Traffic Safety Administration (Ed.): Traffic Safety Facts . February 2015.
- ↑ Federal Constitutional Court, 1st Senate: Federal Constitutional Court - Decisions - Violation of Article 2, Paragraph 1 of the Basic Law by conviction according to § 24a, Paragraph 2, § 25, Paragraph 1 of the StVG after cannabis use that was already significantly earlier . December 21, 2004.
- ↑ THC-COOH value and forms of cannabis consumption. In: verkehrslexikon.de. Retrieved February 20, 2017 .
- ↑ §3 Narcotics Act
- ↑ The drug policy of the Netherlands. In: cannabislegal.de. Retrieved April 2, 2016 .
- ↑ Oliver Meiler Barcelona: Smoking weed against the crisis . In: sueddeutsche.de . January 19, 2015, ISSN 0174-4917 ( sueddeutsche.de [accessed April 2, 2019]).
- ↑ In Barcelona, smoking weed is now allowed in cannabis clubs. Retrieved April 2, 2019 .
- ↑ Legalization of marijuana: Uruguay starts free cannabis sales . In: The time . July 19, 2017, ISSN 0044-2070 ( zeit.de [accessed April 10, 2018]).
- ↑ According to market valuation: Canadian companies found the world's largest stoner group . In: Spiegel Online . January 25, 2018 ( spiegel.de [accessed April 10, 2018]).
- ↑ Marijuana industry gets a boost after Michigan voters just say yes to recreational cannabis . November 6, 2018.
- ^ Franklin Apfel: Addictions and Lifestyles in Contemporary Europe - Reframing Addictions Project ; opinionpublicaucab.weebly.com (PDF) p. 7.
- ↑ a b Claire Cole, Lisa Jones (2010): A Guide to Adulterants Bulking Agents and other Contaminants found in illicit drugs . (PDF) Center for Public Health, Faculty of Health and Applied Social Sciences, Liverpool John Moores University, p. 37 (PDF).
- ↑ Lead-contaminated marijuana poisoning in Leipzig. In: ntv. ntv, November 7, 2007, accessed March 31, 2016 .
- ↑ Franziska Busse, Leyla Omidi, Alexander Leichtle, Michael Windgassen, Eyleen Kluge, Michael Stumvoll: Lead Poisoning Due to Adulterated Marijuana . In: New England Journal of Medicine . tape 358 , no. 15 , April 10, 2008, pp. 1641–1642 , doi : 10.1056 / NEJMc0707784 , PMC 2696942 (free full text).