epilepsy
| Classification according to ICD-10 | |
|---|---|
| G40.– | epilepsy |
| G41.– | Status epilepticus |
| ICD-10 online (WHO version 2019) | |
Epilepsy (from ancient Greek ἐπίληψις epílēpsis , German 'attack, attack' , through ἐπιληψία and Latin epilepsia , detectable since the 16th century), in German in earlier centuries, derived from fall “fall, fall”, epilepsy (also Middle High German “falling addiction "And Latin caducus disease ) and still sometimes called cerebral seizure disorder or cerebral convulsive disorder, describes a disease with at least one spontaneously occurring epileptic seizure that is not due to a currently existing, recognizable cause (for example an acute inflammation of the brain, a stroke or a Head injury) or a trigger (such as withdrawal from alcohol in the case of existing alcohol addiction or severe lack of sleep). A prerequisite for making a diagnosis after an attack is a recognizable high risk of recurrence, otherwise, by definition, epilepsy is only present after two attacks at least 24 hours apart.
An epileptic seizure is a result of suddenly occurring, synchronous electrical discharges from nerve cells (groups of neurons) in the brain , which lead to involuntary stereotypical movement or well-being disorders.
diagnosis
For diagnosis, the patient's medical history is recorded ( anamnesis or external anamnesis ) and an electroencephalogram ( EEG ; "brain wave") is taken both with the help of those affected and the relatives or third parties who have observed seizures . Also, imaging tests are usually for routine diagnosis, are reserved for special methods specific issues. The treatment consists initially in the administration of anti-seizure medication ( anticonvulsants ). In therapy-resistant cases, other methods such as epilepsy surgery are also used.
Epilepsy has a variety of effects on everyday life for those affected (such as suitability for certain jobs or driving a car), which must also be taken into account in treatment.
Epilepsy not only affects humans, but can also occur in a similar form in many animals. See under epilepsy in pets .
Epidemiology
The incidence (frequency of recurrence) of epilepsies depends on age. Each year around 60 out of 100,000 children develop new epilepsy, with a range of 43–82 / 100,000. This does not include febrile seizures and individual unprovoked seizures . In adulthood, the incidence initially drops to around 30–50 / 100,000 per year and increases in advanced age from 60 years to up to 140 / 100,000 per year. If you add up all epilepsies up to the age of 74, you get a frequency of around 3.4 percent. The prevalence of active epilepsies in childhood is 3–6 / 1000 children, depending on age. In early childhood, epilepsy with generalized seizures predominate, while in adulthood epilepsy with partial seizures predominate, some of which can develop into generalized seizures.
Causes of Epilepsy
If no organic brain or metabolic causes can be found for epilepsy , then we used to speak of genuine epilepsy , and if the causes were identifiable, symptomatic epilepsy . A genetic disposition can be determined for both groups of diseases and also for so-called occasional seizures (see section Epidemiology ) . With the technical advancement of imaging procedures and laboratory diagnostics , the diagnosis of genuine epilepsy is decreasing in number.
Causes of Symptomatic Epilepsies:
- perinatal brain damage, mostly in the form of a lack of oxygen at birth
- Brain tissue malformations (for example, focal cortical dysplasia )
- cerebral vascular malformations ( hemangiomas , aneurysms , cerebral arteriovenous malformations )
- Brain tumors
- Traumatic brain injuries in accidents
- Infection of the brain ( encephalitis ) with various pathogens
- Herpes viruses
- Meningococci
- measles
- Hepatitis C.
- TBE virus (tick encephalitis)
- Lyme disease (also transmitted by ticks )
- Autoimmune diseases of the brain
- Metabolic diseases, including
- Hyperparathyroidism with an increase in the concentration of calcium in the blood
- Hemochromatosis with iron deposits and the like a. in the brain
- Eclampsia
- vascular encephalopathy in the context of arteriosclerosis .
Causes of casual seizures:
- Fever ( febrile seizures in children )
- massive sleep deprivation
- excessive physical exertion
- Flicker light with stroboscopic effect , e.g. B. in discos
- Hypoglycemia (low blood sugar) in diabetics
-
Intoxicating drugs , e.g. B .:
- Alcohol poisoning
- (beginning) alcohol withdrawal
- MDMA
- cocaine
- amphetamine
- Ketamine
- Psychotropic drugs , e.g. B .:
Pathophysiology
Although knowledge about the development of epilepsy has increased significantly in the last few decades, the connections are still not fully understood. The occurrence of epileptic seizures is due on the one hand to over-excitability of nerve cells and on the other hand to an abnormal simultaneous electrical activity of larger groups of nerve cells ( neural networks ). It is believed that an imbalance of arousal and inhibition in these neural networks gives rise to epileptic seizures.
Increased excitation or reduced inhibition can be brought about by changes in the membrane properties of the nerve cells as well as in the transmission of excitation from nerve cell to nerve cell by the transmitter substances ( neurotransmitters ). Defects in the ion channels for sodium and calcium ions can contribute to the development and spread of seizure discharges. The amino acids glutamate and aspartate are involved as excitatory neurotransmitters, which open ion channels by binding to NMDA or AMPA receptors . Gamma-aminobutyric acid (GABA), as an inhibiting transmitter substance, represents the opponent, so to speak. Defects in biosynthesis , increased breakdown or inhibition of the receptors ( GABA receptors ) can also contribute to the occurrence of an attack. Electrolyte imbalances due to continued excitement inhibitory GABA-using synapses can this make-causing synapses (Kandel, 2001). The central inhibitory effect of some neuropeptides , such as neuropeptide Y and galanin , is discussed as the body's own mechanism for preventing epileptic convulsions.
The mechanisms that cause epilepsy to develop from individual seizures are far more complex and still unknown. Since the majority of seizures remain single events, they do not necessarily appear to cause epilepsy-inducing changes. However, the animal model of Kindling has also shaped the idea of the development of epilepsy in humans. Under Kindling is defined as a dynamic process in which induce the repeated application of electrical stimuli, which initially is not enough, a seizure, cause an increasing gain of the attack standby until finally seizures. The increased sensitivity to the stimulus then remains.
Clinical studies of the interval between seizures at the beginning of epilepsy could at least not show consistently that the intervals shorten because one seizure paves the way for the next.
Genetic Findings in Epilepsies
In a few cases, family trees and molecular genetic examinations revealed not only a mode of inheritance, but even a genetic location for the mutated genes . The table gives an overview. For example, voltage-dependent channels for sodium ions or neurotransmitter receptors could be identified as altered gene products .
| epilepsy | Inheritance | Locate | gene |
|---|---|---|---|
| benign familial neonatal seizures | autosomal dominant | 20q 8q24 |
KCNQ2 KCNQ3 |
| benign familial infantile seizures | autosomal dominant | 19q13 | CHRNA4 |
| Childhood absence epilepsy | complex | 8q24 | CLN8 |
| juvenile myoclonic epilepsy | complex | 15q4 6p |
? CHRNA7 n. B. |
| Nordic epilepsy syndrome | autosomal recessive | 8pter-p22 | CLN8 |
| generalized epilepsy with febrile convulsions plus | autosomal dominant | 19q13 | SCN1B |
| benign focal epilepsy with centro-temporal spikes | complex | 15q14 | nb |
| autosomal dominant nocturnal frontal lobe epilepsy | autosomal dominant | 20q13.2 15q24 |
CHRNA4 ? CHRNA3 / CHRN5 / CHRN5 |
| familial temporal lobe epilepsy | autosomal dominant | 10q22-q24 | LGI1 |
In addition, epilepsies can also occur in diseases that are based on a change in the genetic make-up, but where the seizure disorder is only a symptom of the disease. Examples of this are tuberous sclerosis or Angelman syndrome .
Classification of the types of seizures
Epileptic seizures can develop very differently. In the 1960s, the International League Against Epilepsy (ILAE) decided for the first time to create a uniform classification (division) of seizures and epilepsy and epilepsy syndromes. The first version of the seizure classification published in 1970 was revised in 1981, the next revision was not made until 2017, together with an explanation of its use. Because it will take a few years for the last revision to become generally accepted, the divisions from 1981 and 2017 are presented here one after the other. In both, a fundamental distinction is made between focal or focal attacks and so-called generalized attacks. By “generalized” it is meant that both halves of the brain are involved in the seizure, which can be seen either by its course, an EEG recorded during the seizure, or both. It is not uncommon for epilepsy to have multiple types of seizures, be it multiple focal, multiple generalized, or focal and generalized.
Classification of seizure types from 1981
Focal seizures
Other expressions for a focal epileptic seizure are herbal seizure or, earlier, partial seizure (the latter term was abandoned because it was more common to misunderstand a "partial" seizure). This type of seizure is characterized by the fact that it begins in a circumscribed region of one half of the cerebrum and is accordingly noticeable.
It does not matter whether it spreads to both halves of the brain in the further course (secondary) (= secondary generalization ). In particular, the start of an attack with an aura has a high informative value about the brain region in which the attack originated, because it is the result of a specific activation of nerve cell associations.
Subdivision:
- simple partial seizures (consciousness is retained)
- complex partial seizures (with impaired consciousness)
- partial seizures that develop into secondary generalized seizures
Generalized seizures
An attack is called generalized if the course and symptoms do not indicate an anatomically limited localization and no signs of a local ( focal ) onset can be seen.
Subdivision:
- Absence - seizures with a short pause in consciousness lasting only seconds without a fall, formerly known as petit mal in French .
- myoclonic seizures - with single or irregularly repeated twitches of individual muscle groups
- clonic seizures
- tonic seizures
- Tonic-clonic seizures - the typical "big" seizure with loss of consciousness, fall, cramping and then rhythmic jerking of both arms and legs, formerly also called convulsion or French grand mal .
- atonic (astatic) seizures
→ see also the section on Generalized Epilepsies and Syndromes
Unclassifiable epileptic seizures
- Seizures that cannot be classified due to insufficient or incomplete data or for which an assignment is not possible.
Classification of seizure types from 2017
The new classification differentiates between seizures with a focal, generalized and unknown onset, each with the two subgroups motor (= with movement disorders ) and non-motor (= without movement disorders) and, for focal attacks, the additional information as to whether there is a disorder of consciousness present or not. There is no adequate translation for the word awareness, which is used in English instead of consciousness .
Focal onset seizures
First of all (with all forms of focal seizures) it must be determined whether or not they are associated with a disturbance of consciousness.
Subdivision:
- focal seizures with motor disorders at the beginning:
- Automatisms
- atonic seizures
- clonic seizures
- epileptic spasms
- hyperkinetic seizures
- myoclonic seizures
- tonic seizures
- focal seizures without motor disorders at the beginning:
- autonomic seizures
- Seizures of arrest
- cognitive seizures
- emotional attacks
- sensory seizures
- focal seizures that develop into bilateral tonic-clonic seizures (replaces "secondary generalized seizures")
Seizures with a generalized onset
As with seizures with a focal onset, a distinction is made between seizures with or without motor disorders.
- generalized onset seizures with motor disorders:
- tonic-clonic seizures
- clonic seizures
- tonic seizures
- myoclonic seizures
- myoclonic-tonic-clonic seizures
- myoclonic-atonic seizures
- atonic seizures
- epileptic spasms
- generalized beginning seizures without motor disorders (absences):
- typical absences
- atypical absences
- myoclonic absences
- Absence with lid myoclonus
Seizures with an unknown onset
As with the other types of seizures, a distinction is made between seizures with or without motor disorders. This group also includes unclassifiable seizures.
- Seizures with motor disorders:
- tonic-clonic seizures
- other seizures
- Seizures without motor disorders
- Unclassifiable seizures
Special types of seizures
Occasional seizures
Occasional seizures ( oligoepilepsy ), which, according to a proposal by the International League in 2010, are also referred to as acute symptomatic seizures , experience has shown that they are not only likely in the case of epilepsy or a genetic disposition to epilepsy. They are epileptic fits that occur due to extraordinary circumstances or conditions (provoked epileptic fits), like
- Febrile seizures ,
- traumatic (e.g. traumatic brain injury or operations on the brain) or non -traumatic brain damage (e.g. stroke ) within the last week,
- Autoimmune diseases of the brain, such as multiple sclerosis , or infections within the "acute phase",
- Diagnoses (usually based on laboratory findings) within the last 24 hours of a metabolic derailment, toxic brain damage or systemic disease with specific biochemical or hematological changes, such as
- too low (less than 36 mg / dl – 2 mmol / l) blood sugar level or too high blood sugar level (more than 450 mg / dl – 25 mmol / l) in connection with ketoacidosis (regardless of known diabetes mellitus ),
- a hyponatremia , mg with a sodium ion concentration of less than 115 / dl,
- a hypocalcemia , with a calcium ion concentration below 5.0 mg / dl,
- a hypomagnesemia , mg with a magnesium ion concentration of less than 0.8 / dl,
- a urea nitrogen concentration above 100 mg / dl,
- a serum creatinine concentration above 10.0 mg / dl,
- acute alcohol or drug intoxication,
- Withdrawal from alcohol (within 48 hours of known abuse; no fixed limit for negative medical history) or withdrawal from drugs,
- acute exposure to known epileptogenic substances (such as crack , cocaine , glutarimide , meperidine , normeperidine or methaqualone ) or
- acute febrile infections in children with a minimum rectal temperature of 38.5 ° C.
These seizures do not justify the diagnosis of epilepsy, even if they occur repeatedly.
Isolated seizures
Individual epileptic seizures without a recognizable provocation ( “unprovoked” seizures ) do not fall under casual or acute symptomatic seizures according to the ILAE classification. According to the definition, epilepsy is also not present, unless there is evidence of a high risk of recurrence.
aura
The term aura comes from the Greek and means 'perception of a breath of air'. One could also paraphrase it with an "indefinite foreboding". If the aura remains isolated, it can be the only - subjective - symptom of a simple focal seizure. It is the result of an epileptic activation of the nerve cells in a circumscribed brain region. Due to the functional assignment of the symptoms to the corresponding areas of the cerebral cortex, they are of great importance in the localization diagnosis of epileptic foci. If the epileptic activity spreads, a so-called secondary generalized seizure can follow.
Examples of auras are the so-called epigastric or visceral aura, an ascent of indefinite unpleasant feelings from the epigastric region, as the most common aura in temporal lobe epilepsy, "numbness, tingling or pinpricks" as aura in parietal epilepsy, or "visual hallinous epilepsy " in occipital lobe epilepsy (Occipital lobe epilepsy). Other examples of an aura can include difficulty concentrating, forgetfulness and not being able to perceive the environment properly.
Status epilepticus
Most epileptic seizures end on their own after a few minutes and the affected person recovers even without therapeutic measures. But you can't rely on it.
If several seizures occur in quick succession as a series without the person affected being able to fully recover in between, and in the case of seizures lasting more than five minutes even without unconsciousness, this is status epilepticus . The longer such a condition lasts, the greater the risk of irreversible damage to the brain or, depending on the type of seizure, of fatal outcome , especially with grand males.
Classification of epilepsies
| Classification according to ICD-10 | |
|---|---|
| G40.0 | Localization-related (focal) (partial) idiopathic epilepsy and epileptic syndromes with focal onset seizures |
| G40.1 | Localization-related (focal) (partial) symptomatic epilepsy and epileptic syndromes with simple partial seizures |
| G40.2 | Localization-related (focal) (partial) symptomatic epilepsy and epileptic syndromes with complex partial seizures |
| G40.3 | Generalized idiopathic epilepsy and epileptic syndromes |
| G40.4 | Other generalized epilepsy and epileptic syndromes |
| G40.5 | Special epileptic syndromes |
| G40.6 | Grand mal seizures, unspecified (with or without petit mal) |
| G40.7 | Petit mal seizures, unspecified, excluding grand mal seizures |
| G40.8 | Other epilepsies |
| G40.9 | Epilepsy, unspecified |
| ICD-10 online (WHO version 2019) | |
As with the forms of epileptic seizures, the International League Against Epilepsy (ILAE) first decided in the 1960s to create a uniform classification of epilepsy and epilepsy syndromes. The first version of the epilepsy classification published in 1985 was revised in 1989. the next revision did not take place until 2017. Because it will take a few years for the last revision to become generally accepted, the divisions from 1989 and 2017 are presented here one after the other. In both, a fundamental distinction is made between focal and so-called generalized epilepsy.
Classification of Epilepsies from 1989
Localization-related epilepsies and syndromes
In this form of epilepsy - also called focal, local, partial or focal epilepsy - the seizure-like discharge is limited to a limited region of the cerebral cortex, at least at the beginning of the seizure, and starts from a focus or focus. In the course of the seizure activity can also spread and eventually affect the entire cerebral cortex. Then one speaks of a secondary generalized seizure disorder.
Childhood benign epilepsy with centro-temporal spikes
This type of seizure is also called Rolandi epilepsy or Rolandic epilepsy . It is associated with sleep-related seizures with tonic spasms of the facial muscles, increased salivation and the inability to speak verbally. The speech disorder can persist for a few minutes after the cramp has subsided, which is a pioneering symptom. It begins between the ages of two and twelve, with a peak in disease between the ages of five and nine. In the EEG there are typical changes, so-called centro-temporal waves Sharp . What is “benign” about these epilepsies is that they always heal at the end of puberty. With around 10-15 percent of all childhood epilepsies, these epilepsies are the most common type of seizure in childhood.
Childhood epilepsy with occipital paroxysms
This epilepsy (first described by Henri Gastaut in 1981 ) is much rarer than the one described above. It is characterized by seizures with visual symptoms followed by motor or psychomotor manifestations. The electro-encephalogram (EEG) shows repeated epilepsy-typical discharges in the region of the occipital lobe . The affected children are otherwise developed normally and the seizures would disappear in adulthood.
Reading epilepsy
In this form of reflex epilepsy, the seizures are triggered by reading, especially loudly. Other language activities can also trigger seizures. These manifest themselves in cramps in the masticatory muscles and sometimes in the arms. If the stimulus is not interrupted, they can also develop into generalized seizures. There is a strong genetic component. The electroencephalogram (EEG) shows changes typical of epilepsy, preferably in the left parietal-temporal region. The course is benign. Avoiding the specific trigger stimuli is the treatment of choice. If necessary, drug therapy is also possible. If only reading-induced seizures occur, it is also referred to as primary reading epilepsy. B. in juvenile myclonic epilepsy also other types of seizures, from secondary reading epilepsy.
Symptomatic epilepsies
In symptomatic epilepsies, the seizures are symptoms of an underlying brain damage. This category includes very different diseases, the classification of which is based on the anatomical location and the associated seizure characteristics as well as other clinical features.
Persistent focal childhood epilepsy
This in technical language Epilepsia partialis continua or " Kozhevnikov called -Epilepsie" form of epilepsy is in a body twitches that can last up for hours for months. Occasional spread can lead to other forms of seizure. It occurs in association with various types of brain damage (including circulatory disorders, neoplasms, brain damage due to lack of oxygen during childbirth). The twitches of individual muscles are resistant to therapy. In some special cases, epilepsy surgery can reduce the seizures.
Temporal lobe epilepsy
In this form of epilepsy ( temporal lobe epilepsy or earlier also psychomotor epilepsy ), the seizures have their origin in defined anatomical structures of the temporal lobe , the hippocampus , the curvature around the hippocampus and the tonsil nucleus . At around 30 percent, it represents the most common form of anatomically classifiable localization-related epilepsies. In the majority of cases, the neuropathological correlate is hippocampal sclerosis or mesial temporal sclerosis . The attacks are characterized by mostly visceral auras with unpleasant feelings rising from the epigastric region. They are usually followed by partial loss of consciousness seizures, which are manifested as smacking-chewing mouth movements - which are the patient's reaction to what they often describe as a "strange taste" in the mouth - followed by repetitive hand movements, then looking around, and finally movements of the whole body (automatisms). Drug therapy is difficult in temporal lobe epilepsy, only about a quarter of the patients become seizure-free, in a further third at least a decrease in the frequency of seizures is achieved. In therapy-resistant cases, epilepsy surgery is also an option here . Special forms of temporal lobe epilepsy include transient epileptic amnesia (TEA) and musicogenic epilepsy .
Frontal lobe epilepsy
In technical jargon, this epilepsy is called frontal lobe epilepsy . According to the diverse functional areas of the frontal lobe , the seizures emanating from it are very diverse in their appearance. Usually brief, predominantly sleep-bound focal clonic or asymmetrical tonic seizures, but also complex automatisms up to speech utterances occur. Minimal or no post-attack confusion also suggests an origin in the frontal lobe. In the case of frontal lobe epilepsy, after drug therapy, epilepsy surgery is also an option if a defined lesion can be found and removed without adverse consequences.
Parietal lobe epilepsy
These focal attacks have their origin in the parietal lobe . Characteristic of this form of epilepsies are so-called sensitive herbal attacks, which are expressed as abnormal sensations in the form of numbness, tingling or pinpricks. Attack-like burning pain, including abdominal pain or headache or an entire half of the body, is also rare. The therapy corresponds to that of the other symptomatic focal epilepsies. If the cause is localized damage to the parietal lobe, the results of an epilepsy surgical procedure are good.
Occipital lobe epilepsy
Occipital lobe epilepsy ( occipital lobe epilepsy) is the rarest form with 5–10 percent of all symptomatic focal epilepsies. They arise from the occipital lobe , where the visual cortex is also located. Typically, the seizures are accompanied by visual hallucinations in the form of persistent or flashing spots or simple geometric figures, temporary blindness, and, less often, tonic or clonic eye movements.
Cryptogenic
Epilepsy syndromes with focal seizures for which no cause can be found are categorized as cryptogenic .
Generalized epilepsies and syndromes
In generalized seizures, the entire cerebral cortex is always affected by the electrical seizure activity from the beginning. These types of seizures are therefore usually associated with a loss of consciousness (exception is juvenile myoclonic epilepsy). They are again differentiated into so-called small ( French petit mal 'small evil' ) and large (French grand times 'great evil' ) seizures.
Idiopathic
The term idiopathic is used in connection with diseases that arise on their own. In cryptogenic epilepsy, there is (still) no known, verifiable cause in the sense of an emergence through external influences (environmental factors), but it is presumably or has already been proven that it is inherited (hereditary) or another suspected underlying disease.
Benign familial neonatal convulsions
This is a benign ( benign ,) rare but well-defined autosomal dominant inherited disease. Two loci were identified on chromosome 20 and on chromosome 8 . Another, not yet identified, exists. This affects full-term newborns who, on the second or third day of life, show one to three minute seizures with respiratory arrests ( apneas ), eye movements, and tonic and clonic expressions. The seizures stop within the first six months of life. The children develop according to their age.
Benign neonatal spasms
This is a sporadic, non-hereditary forms of seizures in the neonatal period, which is typically on the fifth day of life ( English fifth-day-fits , Span 3.-7. Life) occur. They manifest themselves in clonic jerks and respiratory arrests, never in tonic seizures. They can hardly be influenced by medication, but they stop spontaneously. The prognosis is good.
Benign myoclonic epilepsy of infancy
Benign myoclonic epilepsy in infancy is a rare disease with around 0.2 percent of all childhood epilepsy. It is believed that it is an early form of juvenile myoclonic epilepsy. It occurs between the ages of four months and four years in normally developed children and manifests itself exclusively as brief generalized myoclonia . It responds well to drug therapy and has a good prognosis.
Childhood absence epilepsy
Another name for this epilepsy that is still used in the German-speaking world is pyknolepsy . Absence epilepsy is the most common form of idiopathic generalized epilepsy in childhood. This form of epilepsy is characterized by typical absenteeism that lasts five to fifteen seconds . They occur a few times to several hundred times a day with loss of consciousness and gaps in memory and begin before puberty in otherwise inconspicuous children. Grand mal seizures can follow. Familial accumulation, twin studies and the association with a gene location on chromosome 8 indicate a genetic cause of the syndrome. The diagnosis is supported by typical seizure patterns in the electro-encephalogram (EEG) (3 / s spike-wave complexes). The absences can be treated relatively well with medication ( ethosuximide , lamotrigine ). This epilepsy has a good prognosis with a risk of recurrence of 20 percent.
Juvenile absence epilepsy
In contrast to the previous form of epilepsy, this clinical picture is also known as non-pycnoleptic absences . Juvenile absence epilepsy also belongs to the hereditary generalized epilepsy with age-related manifestations. The beginning usually coincides with the onset of puberty and is at its peak at ten to twelve years. The seizures are similar to those in childhood absence epilepsy, but they are less frequent and last a little longer. Around 80 percent of patients also have generalized, tonic-clonic seizures (grand mal), usually after waking up. The drug therapy is not quite as promising as with pycnolepsy and accordingly the prognosis is somewhat more critical.
Juvenile myoclonic epilepsy (Janz syndrome)
Juvenile myoclonic epilepsy ( JME, Janz syndrome), sometimes also called impulsive petit mal epilepsy in German-speaking countries, is partly hereditary and manifests itself primarily in adolescence (12-20 years). The myoclonic seizures manifest themselves in sudden, short, mostly bilaterally symmetrical muscle twitches of the shoulders and arms, which are consciously perceived by the patient as "an electric shock". They occur singly or irregularly, especially in the morning hours and are of greatly varying strength. Consciousness remains with this form of seizure. In up to 95 percent of patients, generalized tonic-clonic seizures occur in the further course of the disease after months to years. Absence occurs less frequently (15–40 percent of patients). In addition to pharmacological therapy, the avoidance or reduction of factors that trigger attacks (fatigue / sleep deprivation, alcohol consumption) must be ensured.
Wake up grand mal epilepsy
This form, which is also one of the genetically caused epilepsies, manifests itself with a frequency peak around the age of 17 (range 14 to 24). Generalized tonic-clonic seizures without aura occur exclusively or predominantly in the first hours after waking up, less often also after the active phase of the day with relaxation as "after-work grandmothers". In addition to avoiding trigger factors, the therapy is based on the administration of an anti-seizure medication (including valproic acid ). The prognosis is more favorable the younger the patient is at the onset of the disease.
Other generalized epilepsies
Epilepsies with specifically triggered seizures
In these epilepsies, tonic-clonic seizures are triggered in response to specific, well-defined stimuli. Hence they are also called reflex epilepsies . They are mostly idiopathic. In rare cases of symptomatic reflex epilepsy, partial seizures also occur. The triggering stimuli mainly include flicker light and other visual stimuli (see photosensitivity ). This rare form of epilepsy occurs when seizures are triggered by television or video games. Screens can provoke epileptic seizures in susceptible people by changing light and dark, by changing color combinations and by patterns. In 1997, the episode Dennō Senshi Porygon of the children's show Pokémon in Japan triggered epileptic reactions in over 600 viewers without an epileptic history, mostly children, due to very rapid color and light-dark changes , so that 200 of them had to stay in the hospital. Similar effects are possible in computer games . An epilepsy warning can therefore be found prominently in many computer game manuals . Another form of reflex epilepsy are so-called startle attacks , also shock attacks, in which z. B. sudden noises or unexpected touches can trigger a mostly tonic or secondary generalized tonic-clonic reflex attack.
Cryptogenic or symptomatic
West Syndrome
The West syndrome , sometimes also called epilepsy with lightning, nodding, salaam cramps (BNS epilepsy) in German-speaking countries , is an age-related epilepsy that almost always occurs in infancy with series of 2 to 150 short-term Seizures begins and is associated with a typical pattern on the electro-encephalogram (EEG) called hypsarrhythmia . The prognosis is mostly unfavorable, especially with regard to cognitive development, even with successful drug therapy, whereby this is usually due to existing organic brain damage and not to the epileptic seizures themselves.
Lennox-Gastaut syndrome
The Lennox-Gastaut syndrome is one of the most severe epilepsies of childhood and adolescence. It is characterized by the frequent occurrence of various generalized forms of seizures, particularly tonic falls. There is usually a resistance to therapy and the patients usually have moderate to severe cognitive deficits. The differentiation from other epilepsy syndromes is often difficult, however.
Epilepsy with myoclonic astatic seizures
Myoclonic-astatic epilepsy, also known as Doose syndrome , usually begins in the first five years of life. In addition to the eponymous astatic falls due to sudden loss of tension in the muscles, usually initiated by brief jerks, absences and generalized tonic-clonic seizures can also occur. Patients respond differently to drug therapy, and the prognosis can be clouded with frequent generalized tonic-clonic seizures.
Epilepsy with myoclonic absences
This is a special epilepsy of childhood, in which absences occur exclusively or predominantly, which are accompanied by strongly pronounced, rhythmic and bilateral twitches, especially of the shoulders and arms, less of the legs. The electro-encephalogram (EEG) shows the seizure patterns that are typical for other absence epilepsies. Almost half of the children have a mental development disorder before the onset of epilepsy. Since a considerable number of children are not seizure-free, around a quarter will be added as the disease progresses. However, if the absences respond quickly and persistently to the therapy, the intelligence is retained.
Symptomatic
These epilepsies are based on proven brain damage of the past [condition after infection of the central nervous system, head trauma, vascular disease of the brain) or progressive (metabolic diseases with involvement of the central nervous system, tumors of the central nervous system ( primary brain tumor , brain metastasis ), chronic infection of the central nervous system] .
Epilepsies and syndromes that cannot be identified as localization-related or generalized
Neonatal cramps
This is the case with seizures that are strictly limited to the first four weeks of life, which in the vast majority of cases are due to damage to the brain, for example through infection, temporary lack of oxygen or hypoglycaemia and are therefore symptomatic in nature.
Dravet syndrome (severe childhood myoclonic epilepsy)
The Dravet syndrome is extremely rare. In otherwise healthy children, it begins in the first year of life with frequently recurring, generalized or unilateral seizures with and without fever, which tend to have a prolonged course. In the second to third year of life, individual or short series (two to three sequences) of twitches, especially of the trunk muscles, of very different strengths, occur. Therapy is difficult and the prognosis is correspondingly poor.
Epilepsy with persistent spike-wave discharges in synchronized sleep
The special thing about this epilepsy syndrome is the occurrence of continuous generalized epilepsy-typical discharges in the electro-encephalogram (EEG) during the entire so-called synchronized sleep . In connection with this, the children experience a mental deterioration as well as a considerable impairment of the language and the temporal and spatial orientation. Frequent and varied seizures (unilateral focal motor seizures, atypical absences, atonic seizures with falls, generalized tonic-clonic seizures - but never tonic seizures) begin at the age of four (on average).
Aphasia epilepsy syndrome
The aphasia-epilepsy syndrome is also known as Landau-Kleffner syndrome . In the ILAE classification, this syndrome is separated from epilepsy with sustained spike-wave discharges in synchronized sleep, although it is suspected that both syndromes are probably just different manifestations of the same disease. However, in the majority of cases between the ages of three and eight years, a loss of speech ability ( aphasia ) is the first symptom. In around 40 percent of children, the disease first manifests itself in various epileptic seizures. The prognosis for seizures is good, but it is critical for speech function.
Complications and consequences
Epileptic seizures can be associated with a number of complications, the main of which are:
- Injuries or damage that occur directly through muscle contractions during the attack, this often includes vertebral fractures due to extreme tension in the back muscles, lacerations, cuts, lacerations, bite wounds.
- Injuries from seizure-related accidents, such as falling from a ladder, road accidents, or drowning accidents.
- Cardiac arrest caused by excessive vagal stimulation during a severe seizure.
- Breathing disorder due to narrowing of the airways during a long, severe seizure with interruption of the protective reflexes.
After a mostly generalized tonic-clonic (grand mal) seizure, those affected can for some time - this can take up to several hours - fall into a harmless deep sleep ( terminal sleep ) or go through a postictal twilight state .
Diagnosis
- As with all other diseases, the first step is to collect the medical history ( anamnesis ). In epilepsy patients, in addition to the familial occurrence of epilepsy and other diseases of the nervous system, special attention should be paid to previous illnesses that may cause symptomatic epilepsy. These include disorders and risks during pregnancy, problems during childbirth that lead to a lack of oxygen, accidents with traumatic brain injuries or inflammatory diseases of the central nervous system.
- This is followed by a physical examination, particularly of the nervous system, with an examination of strength, feeling (sensitivity), reflexes, cranial nerve function, balance and coordination.
- Laboratory tests from the blood serve, on the one hand, to identify possible causes of symptomatic epileptic seizures (such as hypoglycaemia or mineral deficiency). On the other hand, the attending physician monitors the amount of the drug in the blood ( drug level or therapy level ) as well as possible side effects (blood count with blood platelets, liver enzymes, kidney function, blood clotting, calcium-phosphate metabolism) under drug therapy .
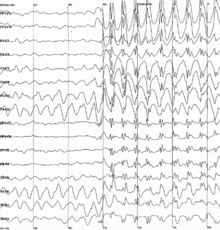
- By electroencephalography (EEG) the willingness of the brain can be displayed directly to epileptic discharges. For this purpose, the patient is put on a kind of cap with electrodes at defined intervals, from which the electrical surface activity of the cerebral cortex is derived via an AC voltage amplifier. Activation with hyperventilation and photostimulation is part of the routine derivation when asking about epilepsy . As part of the initial diagnosis, the EEG primarily serves to classify the seizure or epilepsy and to localize the focus in the case of focal seizures. Long-term recordings (for example over 24 hours, long-term EEG ) or recordings with simultaneous parallel video recording of the patient ( video double-image EEG ) can also be carried out for special questions .
- In contrast, magnetoencephalography (MEG) derives the magnetic activity of the brain with high temporal and spatial resolution. However, this is a very complex, expensive and new method that primarily serves to precisely localize areas of the brain that trigger epilepsy.
- Cerebral computed tomography (CCT) is a special X-ray layer examination and was the first imaging procedure with which coarse triggering changes in the brain tissue could be found. Their advantages lie in their quick availability and economy. Since its resolution of the tissue changes in the brain is inferior to other methods, it has also lost its importance because of the radiation exposure associated with it.
- In magnetic resonance tomography (MRT or MRI), the images are generated by changing, strong magnetic fields. The display has a significantly higher resolution and a better contrast between gray and white matter. Functional magnetic resonance imaging (fMRI) is available for special questions, especially in presurgical diagnostics , with which special brain functions can be assigned to the associated cortical areas.
- In newborns and infants, an ultrasound examination of the brain through the open fontanel can provide information on anatomical deviations.
- With positron emission tomography (PET), flumazenil-PET and single photon emission computed tomography (SPECT), further special procedures are available, with which, in particular, epilepsy-causing foci can be precisely localized and, in the case of presurgical diagnosis, neurological failures can be estimated during surgery.
Differential diagnosis
Various disease states associated with transient seizure-like phenomena may be very similar to, and therefore confused with, epileptic seizures. Misinterpretation of such conditions as epilepsy should be avoided as far as possible, as it not only leads to unnecessary uncertainty for the patient or relatives, but also to unnecessary treatment with anti-epileptic drugs. Conversely, real epileptic seizures can be misjudged as non-epileptic and necessary and helpful treatment can be omitted.
The most important differential diagnosis of epileptic seizures in adulthood is psychogenic non-epileptic seizures. They are also called dissociative seizures and can look similar to epileptic seizures. A reliable differentiation is often only possible with a long-term video EEG recording. Psychogenic seizures are not organic (caused by a functional disorder in the brain), but psychological. The cause can be, for example, depression , an anxiety disorder or a post-traumatic stress disorder . It is not uncommon to find traumatic experiences such as sexual abuse in the life story. These seizures are not simulated (feigned). They require psychiatric drug therapy or psychotherapy, often both. Treatment with anti-epileptic drugs is pointless.
An important differential diagnosis of epileptic seizures in children and adolescents - the occurrence of which is not limited to this age - is syncope due to circulatory regulation disorders or cardiac arrhythmias . Particularly in childhood, respiratory affect spasms, respiratory arrests or cyanosis when acidic gastric juice flows back into the esophagus and the benign paroxysmal dizziness of infancy should be taken into account. At this age, masturbation, especially in girls with sudden stiffening of the thighs or rocking movements, can resemble epileptic phenomena.
Other rare differential diagnoses are simple, only aura-related or complicated forms of migraine, nocturnal or sleep-related episodic events such as night terrors, sleepwalking, nightmares or narcolepsy , seizure-like motor phenomena such as tics and episodic psychiatric disorders such as daydreams, hyperventilation syndrome, anxiety attacks and panic attacks.
REM sleep behavior disorders are an important differential diagnosis, especially in older people.
Neuropsychology in the diagnosis of epilepsy
Neuropsychological diagnostics in epilepsy patients, i.e. the examination of various cognitive functions such as concentration, immediate memory or medium-term memory performance, basic or higher language performance, etc., is carried out to answer several questions:
While questions of lateralization and the localization of epilepsy were in the foreground in the past, today, as a result of the great advances in the field of structural and functional imaging, more questions are interested in the functional impairment of cognitive performance through epilepsy itself or its somatic basis, undesirable effects of drug treatment or the risk of cognitive loss due to a possible epilepsy surgery. These tasks of neuropsychology can ultimately be summarized quite well under the heading of quality control, i.e. the assessment of the justifiability and tolerability of a selected therapeutic method.
In addition, questions about the everyday relevance of epilepsy-associated cognitive disorders, for example on school performance or the job, should also be answered and also serve to determine the need to carry out a rehabilitation measure and, in turn, also to validate it.
Usually, many tests are still carried out with pen and paper, but some methods are already available today as computer-aided test methods. In addition, the specialized centers are increasingly using the method of functional imaging, such as functional magnetic resonance tomography, for the lateralization of hemispherical language dominance. If there is any ambiguity in the interpretation of the results, it may be necessary to carry out the invasive intra-carotid amobarbital test (also known as the Wada test ), which allows a fairly reliable statement to be made about the lateralization of the hemisphere for language via the temporary anesthesia of a cerebral hemisphere. The aim of these procedures is to keep the risk of further cognitive losses during epilepsy surgery as low as possible.
Further tasks of neuropsychology also concern the short-, medium- and long-term psycho-social consequences that a chronic illness such as epilepsy has on the life of those affected. With the help of more or less standardized questionnaires and interviews one tries to record these effects. Ultimately, it must also be possible to measure the effectiveness of the various therapy methods in terms of their effects on the psycho-social development of the patient.
treatment
The aim of treatment for epilepsies is complete freedom from seizures with as few or no side effects as possible. In addition, the therapy should ensure unimpaired development in children. All patients should be given a way of life that does justice to their abilities and talents. A distinction must be made between acute treatment of an epileptic seizure and long-term treatment. These therapeutic goals are primarily achieved through appropriate drug treatment . With the help of monotherapy with carbamazepine , eslicarbazepine acetate , lamotrigine , levetiracetam , oxcarbazepine , valproic acid or another anticonvulsant , seizures can be controlled in around two thirds of cases. The remaining patients are referred to as drug-resistant epilepsy. The additional use of other anti-epileptic drugs (add-on therapy) rarely leads to permanent freedom from seizures in drug-resistant epileptics (around 10 percent), but partial successes, such as a reduced frequency of seizures or milder types of seizures, can be achieved.
Pharmacoresistant epileptics should also be examined at an early stage to determine whether they are suitable candidates for epilepsy surgery. Epilepsy surgery can meanwhile - in drug-resistant focal epilepsy - "cure" epilepsy if the epileptogenic area in the brain can be precisely identified and is operable. The chance of being seizure-free through an epilepsy surgery is 50–80 percent, depending on the constellation of findings.
A comprehensive treatment concept also includes information and advice through to patient training, instructions for documenting seizures, if necessary by keeping an seizure diary, and helping people integrate into family, school, work and society. Society recommends an open discussion based on respect.
Acute treatment
Most epileptic seizures end on their own after a few minutes. Depending on the type of seizure, the person affected can still injure themselves by falling or - for example during a phase of twitching or by acting in a state of clouded consciousness - on objects in their surroundings. Exposing the protective reflexes can also lead to aspiration of food, stomach contents or - in the case of bathers - large amounts of water. Grand mal seizures in particular lead to acute oxygen deficiency due to ineffective breathing, which can damage the brain even further. The longer the seizures last without waking up in the meantime, the greater the risk ( status epilepticus ).
First aid
The main thing to ensure that those affected do not suffer any injuries, especially in the stage of clouding of consciousness:
- shield from danger
- Move dangerous objects out of reach
- Block falling edges (e.g. in the stairwell)
- Divert or stop traffic
- The previously widespread introduction of a bite wedge is no longer performed because it can cause additional injuries and also delay the resolution of the seizure.
- Likewise, one should not hold on to those affected during an attack, with the exception of bathers whose heads must be kept above water or who are to be rescued from the bathing water.
Avoid damage from lack of oxygen: Unless relatives or caregivers of a person with epilepsy have the option of acute treatment, an emergency call must be made. The emergency doctor or ambulance service personnel can end a prolonged seizure and prevent short-term secondary attacks by injecting medication.
In principle, it is also helpful for the attending physicians if the course of the seizure is closely observed and its duration is noted, as this facilitates the precise diagnosis and treatment.
Medical therapy
People who are known to have a severe form of epilepsy themselves or to their relatives usually carry a medically prescribed emergency medication with them, which can be administered by anyone who is trained in it if necessary. These are drops that, depending on the dosage form, are either placed in the cheek pouch or inserted into the rectum in the form of a micro- enema. The acute epileptic seizure can in most cases be interrupted by this administration of anticonvulsants from the group of benzodiazepines . In particular, diazepam , clonazepam , lorazepam , midazolam and nitrazepam have become established in acute therapy, with midazolam showing the fastest onset of action (<30 minutes). However, the effectiveness and tolerability of these drugs varies from person to person. Also, thiopental , a barbiturate is used as an intravenous solution for therapy in seizure. These drugs are only used in exceptional cases for long-term treatment, as they can lead to psychological dependence in particular when taken regularly .
Permanent treatment
A so-called epilepsy helmet protects against head injuries. A large number of drugs (anti-epileptic drugs) are now available to prevent epileptic seizures. Of the older active ingredients, carbamazepine is still used frequently for epilepsy with partial seizures and valproic acid for epilepsy with generalized seizures . Of the now numerous newer active substances, lamotrigine and levetiracetam are the most frequently prescribed. Instead of carbamazepine, its keto analogue oxcarbazepine or eslicarbazepine acetate is more often given preference because of its comparable effectiveness but weaker enzyme induction . Valproic acid is preferred in the long-term treatment of primarily generalized seizures, but only in the absence of alternatives in women of childbearing age. The classic anti- epileptic drugs phenytoin , phenobarbital and primidone are also available as monotherapeutic agents , albeit with a rather unfavorable side effect profile. Of the newer anti-epileptic drugs, topiramate and zonisamide are also approved for monotherapy, whereas brivaracetam, perampanel, rufinamide and stiripentol should only be used as additional treatment. A special group of epilepsies in childhood, the benign (“benign”) idiopathic partial epilepsies, are preferably treated with Sultiam . Ethosuximide has a special place in the treatment of absence epilepsy of school age, in which it has proven to be superior to lamotrigine and valproic acid in a large comparative study.
These drugs achieve their effects by increasing the stimulus threshold by inhibiting sodium ion channels (valproic acid, carbamazepine, oxcarbazepine and phenytoin) or by activating GABA receptors (phenobarbital and its prodrug primidone) in the central nervous system.
The number of patients who are not compliant is particularly high in neurology . In patients with epilepsy, the rate of drug refusal is 50 percent. Every second admission could be prevented if patients did not stop their medication on their own initiative.
Since the monotherapy of epileptic diseases does not lead to a satisfactory result in some of the patients, therapy using an additional therapeutic agent with a complementary mechanism of action can be considered. The GABA analogues gabapentin , pregabalin , tiagabine and vigabatrin , which increase the GABA concentration in the brain, have established themselves as additional therapeutic agents . Alternatively, the ion, calcium and sodium channel inhibiting suximides mesuximide and ethosuximide , lamotrigine , levetiracetam , felbamate , topiramate and eslicarbazepine acetate are available.
After a longer period of freedom from seizures - at least two years - depending on the risk of seizures recurring and the possible psychosocial effects of recurring seizures on the one hand and the impairments perceived by the therapy on the other hand, gradual cessation of drug therapy can be considered. Numerous studies have examined the risk of seizures recurring after stopping drug treatment. In summary, there is a 70 percent chance of permanent seizure freedom without medication, though
- was seizure-free for two to five years,
- there was only one type of seizure
- normal intelligence and normal neurological findings exist and
- the electroencephalogram has normalized during therapy.
Other methods of epilepsy treatment
Alternative pharmacological measures
In addition to the drugs that actually suppress seizures, there are other drug-based treatment approaches for various difficult-to-treat epilepsies. In West syndrome, treatment with ACTH (adrenocorticotropic hormone from the pituitary gland that stimulates the adrenal glands to produce more cortisone ) or corticosteroids have been shown to be effective directly. This treatment, rich in side effects (including high blood pressure, thickening of the heart muscles with restricted pumping function, kidney calcification, diabetes mellitus ) is also used in Landau-Kleffner syndrome, myoclonic astatic epilepsy and Lennox-Gastaut syndrome with different prospects of success.
The observation that in children suffering from epilepsy with hay fever an injection of immunoglobulins led to an improvement in the seizure disorder has led to the systematic use of this too. Why immunoglobulins are even effective in epilepsy is still unclear. There are also still no criteria to help predict the difficult-to-treat epilepsies for which this therapy is promising. A review that summarized 24 studies was able to show an overall freedom from seizures of around 20 percent and a reduction in the frequency of seizures of around 50 percent with significantly different treatment durations and dosages in the individual treatments.
Ketogenic Diet
Based on the experience that fasting temporarily leads to freedom from seizures in people with epilepsy , a diet with a very high fat, low carbohydrate and moderate protein content has been used since 1921 to produce a sustained metabolic state with predominant fat burning and the formation of ketone bodies (ketosis) mimicking the biochemical effect of fasting. This so-called ketogenic diet has been shown to be effective in epilepsy patients. The exact mechanism of action has not yet been clarified. However, numerous studies have shown that around a third of the patients treated become seizure-free and around another third experience a significant reduction in seizures by at least half. For practical reasons, it is particularly suitable for children from one to ten years of age, but it is also effective for young people and adults. Myoclonic and atonic seizures seem to address best, less well generalized tonic-clonic and focal seizures, and absenteeism worst. The diet should normally be carried out for two years, and in some patients the effect obtained lasts after the end. As side effects, vomiting, diarrhea, constipation and refusal to diet can occur at the beginning. Acidification of the body can occur, especially with additional acute illnesses. The risk of developing kidney stones is increased. Often there is also a sometimes massive increase in blood lipid levels. The possible long-term effects on cardiovascular diseases cannot be estimated. The ketogenic diet is an effective treatment alternative, especially for severe epilepsy.
Epilepsy surgery
If, despite the optimal selection of anti-epileptic drugs in the maximum tolerated dose, no satisfactory seizure control can be achieved and a structural lesion of the brain can be proven to be the cause of the seizures, surgical treatment of the seizure disorder can also be considered ( epilepsy surgery ). For this purpose, the area triggering the attack must be precisely localized in careful and extensive examinations before the procedure ( pre-surgical diagnostics ) and the functional impairment after loss of the corresponding brain tissue must be assessed ( e.g. Wada test ).
Vagus nerve stimulation (VNS)
In vagus nerve stimulation, an electrical stimulator is used to stimulate the left vagus nerve on the neck with electrical currents either at fixed intervals or when activated by the patient in the event of a pre-seizure . The stimulator with a battery is inserted on the chest wall. The stimulated vagus nerve transmits the excitation to the brain, which can lower the frequency of seizures.
Side effects can include local pain or abnormal sensations, changes in the pitch of the voice, shortness of breath, nausea and diarrhea. Although the vagus nerve also directly supplies the heart muscle and is involved in controlling the heart rate, changes in heart rate have not been reported.
Transcutaneous vagus nerve stimulation (without surgery)
Transcutaneous vagus nerve stimulation does not require surgery or hospitalization. Via an ear electrode connected to a stimulation device, a branch of the vagus nerve is stimulated through the skin at a specific point on the auricle. The patient adjusts the strength of the stimulation so that he feels a pleasant tingling sensation. Through the branch of the vagus nerve, the excitation is passed on to the brain, which can reduce and alleviate seizures.
The therapy is applied solely by the patient and can be easily integrated into everyday life. This form of epilepsy therapy can be used early on and has only minor side effects, which usually subside quickly after the stimulation is stopped. However, the only randomized double-blind study published to date could not prove any effectiveness.
Behavior therapy
Using a biofeedback model and behavioral therapy, some epilepsy patients were able to reduce the number of seizures. Before and after the seizure there is a change in brain activity, and behavior therapy enabled the patients to gain a certain influence on these activities, which prevented seizures.
Early warning systems
- Many dogs can predict a family member's seizure. Therefore, attempts have been made for several years to specifically train epilepsy dogs.
- Brain implant
- In severe and refractory epilepsies, 16 EEG probes used as brain implants were used to predict seizures. In this way, those affected were able to get “safe” and wait for the attack. This could greatly improve the quality of life of people with severe epilepsy and also preserve the ability to work longer.
forecast
The prognosis of epilepsy depends on various factors such as the present epilepsy symptom and its cause, the type and frequency of the seizures, the age of onset and any accompanying diseases of the nervous system. It can be viewed from the various aspects of long-term freedom from seizures (remission), psychosocial impairments or mortality.
Remission
If the different studies on prognosis are summarized, a total of around 50 to 80 percent of all epilepsy patients achieve lasting freedom from seizures. Children at the age of onset between one and ten years have the greatest statistical probability of becoming seizure-free. Genetic (idiopathic) and epilepsy of unknown cause generally have a better prognosis than those with a demonstrable cause. Accordingly, the prognosis worsens in patients with accompanying neurological diseases or mental disabilities. Persistent EEG changes are also associated with a lower remission rate. A good prognostic sign is the rapid response to the therapy, whereas so far it has not been proven that the long-term prognosis can be favorably influenced by an early onset of anti-epileptic treatment.
So-called epileptic change of character
The concept of a specific epileptic change of personality that has long been handed down in some psychiatric textbooks is now considered outdated. It has been described as supposedly typical in Germany since the 1930s in the form of disturbances of understanding, memory and judgment, general slowing down, sticking in thinking, awkwardness, pedantry, self-righteousness or good-natured dullness, which in retrospect was also part of the National Socialist race policy The aim of eradicating hereditary diseases must be seen (see also Action T4 and euthanasia ).
mortality
Basically, people with epilepsies have an increased risk of dying prematurely. Possible causes for this are direct consequences of a so-called status epilepticus, accidents during an attack - for example, falling or drowning - suicide , sudden unexpected death in epilepsy (SUDEP, Sudden Unexpected Death in Epilepsy , see below) or the underlying disease that causes epilepsy becomes. The relative mortality risk is about two to three times higher than that of the healthy reference population. It is lowest in genetic (formerly: idiopathic) epilepsy and highest in symptomatic epilepsy syndromes due to tangible changes in the brain, especially in children with neurological deficits that have existed from birth.
Sudden Unexpected Death in Epilepsy (SUDEP )
As SUDEP (of English sudden unexpected death in epilepsy ), a sudden unexpected death in epilepsy is called. The following risk factors were identified in a study:
- younger age
- symptomatic epilepsies with detectable brain changes
- male gender
- low serum concentration of the anti-epileptic drugs taken
- generalized tonic-clonic seizures
- sleep
Research into the causes of death of epileptics and the recording of their mortality is still poorly developed in Germany, which is why only little information on this can be found in the literature. For people with epilepsy, the death rate is 600 out of 100,000 people per year, and for newly affected people it is 60 out of 100,000 people per year. The risk for a SUDEP is around 50 in 100,000 to 100 in 100,000 people per year; if the patient has severe epilepsy or neurological impairment, it is up to 500 out of 100,000 people per year. In the UK , the number of people who die of or as a result of epilepsy is given as 1,000 per year. It is estimated that most of these deaths are SUDEP.
Psychosocial
Though many people with epilepsy rarely have seizures as a result of drug treatment, the effects can be severe. These can be objectively existing impairments such as drug side effects. However, there are also psychological factors. Having a grand mal seizure in public or at work is uncomfortable. Epilepsy differs from other “common diseases” like diabetes in that it still has a stigma attached to it, even when attitudes among the population have improved. However, due to the fact that epilepsy is practically non-existent in the media, the level of information is still insufficient. The unemployment rate among people with epilepsy is disproportionately high, even among people with disabilities in general. This high proportion cannot be explained solely by objectively existing reductions in performance.
The spectrum of the disease is wide, however, it ranges from forms with a good prognosis and few seizures to forms with a high frequency of seizures and occurring brain damage. Even if people with epilepsy still encounter difficulties in a number of areas of life, they usually lead relatively normal lives.
history
Epilepsy is older than mankind (since every brain of sufficient complexity can produce uniform discharges with epileptiform consequences) and is one of the most common chronic diseases. Because the appearance of seizures can be spectacular, people with epilepsy have been stigmatized both positively and negatively throughout history .
For example, epilepsy, although the ancient term - especially the Byzantine ἐπιλη nichtα - is not always to be seen as identical to today's clinical picture, affected people in some ancient cultures as saints, as the (apparent) transition into trance states was so easy for them . Epilepsy was already known and feared in ancient Egypt and at the time of the Babylonian king Hammurabi .
Ancient Greeks regarded epilepsy as a “holy disease”, “as obsession with divine power” and is therefore still sometimes referred to as sacer's disease . Depending on the type of attack, different gods were associated with her ( Cybele , Poseidon , Enodia, Apollon Nomios, Ares ). Around 400 BC However, the Greek physician Hippocrates or the author of On Sacred Disease turned against the sanctity of disease. He emphasized that this disease also had a natural cause and that the therapy had accordingly also taken place with natural means. In his opinion, the rationally understandable cause was: cold phlegm flows into the warm blood, whereupon the blood cools down and comes to a standstill. The treatment was carried out according to the healing principle contraria contrariis 'Fighting the opposite with the opposite' : dietetics , medicines , cupping , purge , bloodletting , branding iron and trepanation . Galen (approx. 129–200) first described the aura as a sign of an incipient seizure. Alexandros von Tralleis (approx. 525–605), who already assumed that the brain was the place of origin of epilepsy, recognized that alcohol can promote the occurrence of epileptic seizures and recommended plant components of hyssop and verbena .
In ancient Rome , prospective soldiers had to look into a light source (for example the sun) through a rotating cartwheel when they were being examined . If they had a seizure, they were retired.
The Gospel of Mark describes the spontaneous healing (9.17-29 EU ) of a case of epilepsy and constitutes “prayer and fasting” (9.29 EU ) as the only possible therapy (according to other text witnesses only prayer).
The finds of two manuscripts with the late Old High German spell or blessing ( Contra caducum morbum , from morbus caducus "falling addiction") against epileptic attacks date from the 11th and 12th centuries .
In the Middle Ages, a seizure was often interpreted as an “attack from above”, as divine punishment or “demonic possession” and could have serious consequences for the person concerned, for example an exorcism ( contra caducum morbum ). In the case of Anneliese Michel , this happened in Germany in 1976. Paracelsus (1493–1541) emphasized, however, that there was no unnatural, mystical cause, and pointed out that animals (“vih”) can also develop epilepsy. It is not always possible to cure the cause ("roots"), but the symptoms can be alleviated ("that the roots never wax"). Paracelsus believed that epilepsy could also have its seat in the liver, heart, intestines, or limbs. According to his conception of the correspondence between macro and microcosm, he assumed that “erdbidmen” ( earthquake ) was also epileptic in nature.
In the 17th and 18th centuries, epilepsy gradually (again) gained its modern status among other diseases, for example Simon-Auguste Tissot (1728–1797) made a distinction between idiopathic (predisposed) and sympathetic (from an underlying disease, for example one Brain tumor following) epilepsies, differentiated epilepsy from psychogenic seizures, differentiated the grand mal (large seizure) from petit mal (the small seizure) and used valerian ; But it was not until the second half of the 19th century that it was possible to scientifically prove that epilepsy has a natural origin. John Hughlings Jackson (1835–1911) published exact descriptions of seizures:
“The [focal, circumscribed] seizure usually begins, this must be noted, in that part of the face, arm, and leg that has the most varied uses. [...] So the attacks that begin in the hand usually begin in the index finger and thumb; Seizures onset in the foot usually begin in the big toe. [...] The frequency sequence in which certain parts of the body are seized by the cramps [reveals] perhaps only the frequency sequence in the disposition of certain parts of the brain to become ill. [...] Parts that have the most varied uses will be represented in the central nervous system by more ganglion cells. "
During the dictatorship of National Socialism in Germany, people who were affected by genetic or often only supposedly genetic epilepsy, like many other “ disabled people ”, were considered to be “ unworthy of life ”. According to the law for the prevention of hereditary offspring (GezVeN) of July 14, 1933, people with “hereditary epilepsy” were forcibly sterilized . Many of them fell victim to the murders of the so-called Operation T4 from 1940 onwards .
In earlier centuries epilepsy as epilepsy and falling sickness called. In the 19th century, diseases of small children associated with cramps were regionally referred to as "weeds", especially in the southwestern part of the Kingdom of Saxony. As the most important saints and helpers against epilepsy, muscle cramps and other nervous diseases, St. Valentine and St. Pope Cornelius were regarded among the faithful . Cornelius' invocation of epilepsy was so popular that it was also known as "Cornelius disease" or "Cornelius disease". In the Netherlands it was called Corneliuseuvel . In the Rhineland, Belgium and the Netherlands, a total of about 40 places are recorded where Cornelius was called about this ailment. Pilgrimages were made to many of these places on certain days, mostly until the middle of the 20th century.
museum
In Kehl-Kork (Baden-Württemberg) there has been the German Epilepsy Museum since 2001 , the only one in the world on the subject of epilepsy.
Epilepsy Day, Purple Day and International Epilepsy Day
Since 1996, around October 5th, Epilepsy Day has been taking place in German-speaking countries , a common day of action of the epilepsy specialist societies and lay organizations. Information days are held in many cities and at clinics and institutions to draw attention to this disease. Since 2008, Purple Day has been taking place annually on March 26th in the USA , an international day to educate people about epilepsy. For some years now, on the basis of a joint initiative by the International Bureau for Epilepsy (IBE) and the International League Against Epilepsy (ILAE), there has been an additional International Epilepsy Day (International Epilepsy Day).
Law, severe disabilities and fitness to drive
If a person has more frequent epileptic seizures and cannot remain seizure-free for at least a year even after treatment, they are not allowed to drive a car in Germany or do any activity that endangers themselves or others. Epilepsy sufferers therefore also have greater problems with choosing a career and should consult a specialist in neurology as well as a specialist in occupational medicine if necessary .
Many occupational disability insurances and also accident insurances refuse to accept epilepsy patients if they have not been seizure-free for at least two years.
Fitness to drive
In Germany, the following rules apply to people with epilepsy who are fit to drive:
Anyone who repeatedly suffers from epileptic seizures is not able to drive a motor vehicle as they endanger themselves and other road users. For further differentiation, the wagon drivers are divided into two groups:
- Group 1: includes driver license classes A, A1, A2, B, BE, AM, L and T.
- Group 2: includes the driving license classes C, C1, CE, C1E, D, D1, DE, D1E and the driving license for passenger transport (FzF)
Regulations for group 1:
The driving license is issued:
- after one year of observation of single partial seizures, which occur without a reduction in consciousness and do not show any motor, sensory or cognitive impairment in driving the vehicle
- after three years of observation for seizures that are exclusively related to sleep
- after a three- to six-month observation phase following a one-off occasional seizure, especially if it was provoked
- after one year of seizure freedom without an obvious tendency to relapse (in the case of previously therapy-resistant epilepsy, the observation period is two years)
- after six months of seizure freedom if the seizures are due to recent brain surgery
Regulations for group 2:
After two unprovoked epileptic seizures, the affected person is usually excluded from this group, the only exception being a five-year absence of seizures confirmed by a doctor without treatment with anticonvulsants.
| Disorder | Group 1 | Group 2 |
|---|---|---|
| First, unprovoked seizure without evidence of the onset of epilepsy | no fitness to drive for six months | no fitness to drive for two years |
| first-time, provoked seizure with an avoidable trigger | no fitness to drive for at least three months | no fitness to drive for at least three months |
| epilepsy | usually not suitable to drive
Exception :
|
usually not suitable to drive
Exception :
|
| persistent seizures without inevitable impairment of the ability to drive | only sleep-related seizures after at least three years of observation
only simple partial seizures without impairment of consciousness and without motor, sensory or cognitive impairment after at least one year of observation |
no suitability to drive |
| Recurrence of seizures if you are fit to drive after many years of seizure freedom | Fitness to drive again after six months (if there are no indications of an increased risk of repetition)
in the case of avoidable provocation factors, a three-month break from driving |
no suitability to drive |
| Termination of anti-epileptic therapy | No suitability to drive for the duration of the reduction of the last medication and the first three months without medication (exceptions possible in well-founded cases) | no suitability to drive |
Severe disability
In Germany, people with epilepsy have the option of applying for a severely handicapped ID card to allow them to compensate for tax and professional disadvantages. According to the "indications for the expert activity", the following degrees of disability (GdB) apply:
| Seizures by type, severity and frequency | GdB |
|---|---|
| very rare (generalized large and complex focal seizures with pauses of more than a year; small and single focal seizures with pauses of months) |
40 |
| rare (generalized large and complex focal seizures with pauses of months; small and single focal seizures with pauses of weeks) |
50-60 |
| Medium frequency (generalized large and complex-focal seizures with breaks of weeks; small and single-focal seizures with breaks of days) |
60-80 |
| common (generalized large or complex-focal seizures weekly or series of generalized seizures, of focal or multifocal seizures; small and single-focal seizures daily) |
90-100 |
| after three years of freedom from seizures (if treatment with anti-epileptic drugs is still necessary) | 30th |
| A seizure disorder is considered to have subsided if there has been no medication for three years without seizures.
Without proven brain damage, a degree of disability can no longer be assumed. |
- |
Marks
Depending on the type and frequency of the seizures, the following identification features may also be awarded:
- "RF" (entitlement to a reduction in the license fee )
- "B" (accompaniment required)
- "G" (significant impairment of mobility in traffic)
- "AG" (exceptional walking disability)
- "H" (helplessness)
| Marks | Requirements for marks | Minimum GdB / GdS |
|---|---|---|
| G | His mobility in traffic is significantly impaired:
Anyone who, as a result of a limited ability to walk ... or as a result of seizures or disorders of the ability to orientate, is unable to cover themselves or other distances (2 kilometers ) in local traffic without considerable difficulties or without danger that are usually covered on foot |
70 |
| B. | The same requirements as for G or H
An authorization for constant accompaniment is to be assumed for severely disabled people who meet the requirements for the marks “G”, “Gl” or “H” |
70 |
| H | This can be assumed for seizure disorders if they alone cause a GdB / GdS of 100 (complex-focal seizures weekly, single-focal seizures daily, series of generalized seizures, frequent status epilepticus seizures). Exception : With children (up to 18 years of age) helplessness can be assumed even with a lower GdB | 100 |
| RF | This mark can be issued to people with a GdB / GdS of at least 80 who, because of their disability, cannot take part in public events even with an accompanying person. | 80 |
| aG | Usually only possible if, due to the frequency and severity of the seizures, a wheelchair is often or constantly required or other orthopedic clinical pictures are present; z. B. moderate to severe osteoporosis as a side effect of the medication or seizure-related frequent bone injuries or fractures | 80-100 |
Professional societies and affected organizations
The authority responsible for epilepsy specialist company is at international level, the International League Against Epilepsy (ger .: International League Against Epilepsy, ILAE), the German-speaking sections are the
- German Society for Epileptology (DGfE),
- Austrian Society for Epileptology (ÖGfE) and the
- Swiss Epilepsy League .
The organization for those affected or for laypersons at the international level is the International Bureau for Epilepsy (IBE), national or regional organizations in German-speaking countries are among others. a.
Germany
- German Epilepsy Association V. (DE)
- Epilepsy Bundes-Elternverband e. V. (e. B. E.)
- State association for epilepsy self-help in North Rhine-Westphalia acc. e. V.
Austria
- Epilepsy Association Austria (EDÖ)
- Epilepsy Interest Group Austria
Switzerland
- Epi-Suisse - Swiss Association for Epilepsy
See also
- Abdominal epilepsy
- Postictal twilight state
- Ohtahara syndrome
- Sleep paralysis
- Purple Day
- Epilepsy Day
literature
Guidelines
- S1 guideline for the first epileptic seizure and epilepsy in adulthood of the German Society for Neurology. In: AWMF online (as of 2017)
- S2 guideline for diagnostic principles in childhood epilepsy of the German Society for Neuropediatrics. In: AWMF online (as of 2008)
- S1 guideline for epilepsy surgical treatment in children and adolescents of the Society for Neuropediatrics (GNP). In: AWMF online (as of 2009)
- S2k guideline for cerebral seizures in newborns of the Society for Neonatology and Pediatric Intensive Care Medicine (GNPI). In: AWMF online (as of 2012)
Textbooks and guides
- Hartmut Siemes, Blaise FD Bourgeois: Seizures and epilepsy in children and adolescents. Thieme, Stuttgart / New York 2001, ISBN 3-13-127031-4 . (Current edition: A. Panzer, T. Polster, H. Siemes: Epilepsies in children and adolescents. Diagnosis and therapy. 3rd, completely revised edition. H. Huber / Hogrefe AG, Bern 2015)
- Rolf Degen: Epilepsies and epileptic syndromes in children and adults. Electroencephalography. Blackwell, Berlin / Vienna 1999, ISBN 3-89412-366-4 .
- Ansgar Matthes, Hansjörg Schneble: Epilepsies - Diagnostics and Therapy for Clinic and Practice. Thieme, Stuttgart / New York 1999, ISBN 3-13-454806-2 .
- Günter Krämer : Epilepsy. Recognize, understand and live with the disease. 4th edition. TRIAS, Stuttgart 2013, ISBN 978-3-8304-6716-8 .
- Günter Krämer: Epilepsy from A – Z - Understanding medical terms. 4th edition. TRIAS, Stuttgart 2005, ISBN 3-8304-3229-1 .
- Günter Krämer: Diagnosis of epilepsy - in a nutshell. How to understand the disease, how to use the best therapies for yourself, how to optimize your everyday life. 2nd, completely revised edition. TRIAS, Stuttgart 2013, ISBN 978-3-8304-6695-6 .
- Günter Krämer, Richard Appleton: Epilepsy. An illustrated dictionary for children and adolescents with epilepsy and their parents. 4th, revised and considerably expanded edition. Hippocampus-Verlag, Bad Honnef 2011, ISBN 978-3-936817-71-3 .
- Günter Krämer, Rupprecht Thorbecke, Thomas Porschen: Epilepsy and driver's license . Hippocampus-Verlag, Bad Honnef 2011, ISBN 978-3-936817-73-7 .
- Günter Krämer, Anja D.-Zeipelt: Epilepsy - 100 questions you never dared to ask. 3. Edition. Hippocampus-Verlag, Bad Honnef 2014, ISBN 978-3-936817-68-3 .
- Andre Jaggy: Atlas and textbook of small animal neurology . Schlütersche, Hannover 2005, ISBN 3-87706-739-5 .
- Karl F. Masuhr, Marianne Neumann: Neurology . (= Dual row ). Georg Thieme Verlag, 2005, ISBN 3-13-135945-5 .
- Jürgen Bauer: Epilepsy: Useful information for treatment and advice. Springer, 2002, ISBN 3-7985-1357-0 .
Children's and young people's books on the subject of epilepsy
- Willi Fährmann : Jakob and his friends. Arena, Würzburg 1999, ISBN 3-401-02097-8 . (from nine years)
- Ellen Howard: Edith alone. From the American. by Doris Halter. Ueberreuter, Vienna 1989, ISBN 3-8000-2728-3 .
- Ellen Howard: Edith herself. Atheneum, New York 1987, Lions 1990, Collins, London 1987, 1990, 1994, ISBN 0-7857-3651-4 . (English original edition)
- Hansjörg Schneble: The own goal or the story of Peter Peep-in-the-air. Dgvt, Tübingen 2000, ISBN 3-87159-027-4 . (from 12 years)
- Sophie Brandes: Not a bit cool. DTV, Munich 2000, ISBN 3-423-78113-0 . (from 12 years)
history
- Owsei Temkin : The Falling Sickness. A History of Epilepsy from the Greeks to the Beginning of Modern Neurology . Baltimore 1945. (2nd ed. Baltimore and London 1971; 2nd continuous edition. Johns Hopkins, Baltimore 1994, ISBN 0-8018-4849-0 )
- Hansjörg Schneble: Illness of countless names. A contribution to the social, cultural and medical history of epilepsy based on its names from ancient times to the present. Bern / Stuttgart / Toronto 1987.
- Hansjörg Schneble: Hopeless, holy, curable. History of epilepsy. de Gruyter, Berlin 2003.
- Jutta Kollesch, Diethard Nickel (ed.): Ancient healing art - selected texts . Reclam, Stuttgart 2007, ISBN 978-3-15-009305-4 .
- Evert Dirk Baumann : The Holy Disease. In: Janus. 29, 1925, pp. 7-32.
- Helmut Heintel (ed.): Sources for the history of epilepsy. (= Huber's classics of medicine and the natural sciences. 14). Bern / Stuttgart / Vienna 1976.
- Epilepsy. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. Walter de Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 361 f.
Testimonials
- Anja D. Zeipelt: Epi on board - I think I'll have a fit. RG Fischer Verlag, 2005, ISBN 3-8301-0885-0 .
- Annette Fink: eye catcher. My life with epilepsy and anxiety. Kreuz-Verlag, Stuttgart 2006, ISBN 3-7831-2830-7 .
- Mechthild Katzorke, Volker Schöwerling, Bernd Pohlmann-Eden: Living with Epilepsy - a long-term film documentary. catlinafilm, Berlin 2005.
- Sue Cooke: Disheveled Owl. The emancipation of an epilepsy patient. 3. Edition. Fischer, Frankfurt am Main 1990, ISBN 3-596-23245-7 .
- Katrin Knigge: Moments out of control - living with epilepsy. Teer + Feder film production, 2003.
Review articles
- Konrad J. Werhahn: Age Epilepsy . In: Dtsch Arztebl Int . No. 106 (9) , 2009, pp. 135-142 ( Article ).
Web links
- German Epilepsy Association acc. e. V., Federal Association of Epilepsy Self-Help
- Helmut Volkers: The child on attacks. - Answers to technical questions about epilepsies in children and adolescents
- IZE / German Society for Epileptology
- Professional assessment in epilepsy and after the first epileptic attack . Occupational safety / DGUV Information 250-001, previously BGI 585
Individual evidence
- ↑ Kluge: Etymological dictionary of the German language. 24th edition.
- ↑ a b c d e Hartmut Siemes, Blaise FD Bourgeois: Seizures and epilepsies in children and adolescents. Thieme, Stuttgart / New York 2001, ISBN 3-13-127031-4 .
- ↑ Note: Diabetes mellitus is a metabolic disorder, but a diabetic can avoid hypoglycaemia by eating food after injecting insulin or taking tablets.
- ↑ Amphetamine (AMPH). Retrieved November 30, 2016 .
- ↑ a b Epilepsy / epileptic seizures. Retrieved November 30, 2016 .
- ↑ MS Hildebrand, HH Dahl u. a .: Recent advances in the molecular genetics of epilepsy . In: Journal of Medical Genetics . tape 50 , no. 5 , May 2013, p. 271-279 , doi : 10.1136 / jmedgenet-2012-101448 , PMID 23468209 (English).
- ↑ H. Gastaut: Clinical and electroencephalographical classification of epileptic seizures . In: Epilepsia . tape 11 , no. 1 , 1970, p. 102–113 , doi : 10.1111 / j.1528-1157.1970.tb03871.x (English).
- ^ Commission on Classification and Terminology of the International League Against Epilepsy: Proposal for a revised clinical and electroencephalographic classification of epileptic seizures . In: Epilepsia . tape 22 , no. 4 , 1981, p. 489–501 , doi : 10.1111 / j.1528-1157.1981.tb06159.x (English).
- ↑ Robert S. Fisher, J. Helen Cross, Jacqueline A. French, among others: Operational classification of seizure types by the International League Against Epilepsy: Position Paper of the ILAE Commission for Classification and Terminology . In: Epilepsia . tape 58 , no. 4 , 2017, p. 522-530 , doi : 10.1111 / epi.13670 (English).
- ↑ Robert S. Fisher, J. Helen Cross, Carol DʼSouza et al .: Instruction manual for the ILAE 2017 operational classification of seizure types . In: Epilepsia . tape 58 , no. 4 , 2017, p. 531-542 , doi : 10.1111 / epi.13671 (English).
- ↑ J. Dichgans, H.-Chr. Diener: Neurology (selected chapters). In: Rudolf Gross , Paul Schölmerich , Wolfgang Gerok (Eds.): 1000 memoranda of internal medicine. Schattauer, Stuttgart / New York 1971; 4th, completely revised edition ibid 1989 (= UTB for Science / Uni-Taschenbücher. Volume 522), ISBN 3-7945-1282-0 , pp. 230-234, here: p. 234.
- ↑ Ettore Beghi, Arturo Carpio, Lars Forsgren, among others: Recommendation for a definition of acute symptomatic seizure . In: Epilepsia . tape 51 , no. 4 , 2010, p. 671–675 , doi : 10.1111 / j.1528-1167.2009.02285.x (English).
- ↑ RS Fisher, W. van Emde Boas, W. Blume, C. Elger, P. Genton, P. Lee, J. Engel: Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). In: Epilepsia. Volume 46, Number 4, April 2005, pp. 470-472, doi: 10.1111 / j.0013-9580.2005.66104.x , PMID 15816939 , PDF
- ^ Commission on Classification and Terminology of the International League Against Epilepsy: Proposal for classification of epilepsies and epileptic syndromes . In: Epilepsia . tape 26 , no. 3 , 1985, pp. 268–278 , doi : 10.1111 / j.1528-1157.1985.tb05417.x (English).
- ^ Commission on Classification and Terminology of the International League Against Epilepsy: Proposal for a revised clinical and electroencephalographic classification of epilepsies and epileptic syndromes . In: Epilepsia . tape 30 , no. 4 , 1989, pp. 389–399 , doi : 10.1111 / j.1528-1157.1989.tb05316.x (English).
- ↑ Ingrid E. Scheffer, Samuel Berkovic, Giuseppe Capovilla, among others: ILAE classification of the epilepsies. Position paper of the ILAE Commission for Classification and Terminology . In: Epilepsia . tape 58 , no. 4 , 2017, p. 512-521 , doi : 10.1111 / epi.13709 (English).
- ^ Antonio Valentine Delgado-Escueta, Fe Enrile-Bacsal: Juvenile myoclonic epilepsy of Janz . In: Neurology . tape 34 , no. 3 , March 1984, p. 285-294 , doi : 10.1212 / WNL.34.3.285 , PMID 6422321 (English).
- ^ Günter Krämer: Small Lexicon of Epileptology . Thieme, Stuttgart / New York 2005, ISBN 3-13-133831-8 , pp. 268 , keyword "startle attacks" ( limited preview in Google book search).
- ↑ a b c S1 guideline for first epileptic seizures and epilepsies in adulthood of the German Society for Neurology. In: AWMF online (as of 2012).
- ↑ Specialist information on compendium.ch
- ^ Jost Kaufmann, Michael Laschat, Frank Wappler: Preclinical care of child emergencies. In: Anaesthesiology & Intensive Care Medicine. Volume 61, 2020, pp. 26–37, here: p. 34.
- ↑ Tracy A. Glauser, Avital Cnaan, Shlomo Shinnar, Deborah G. Hirtz, inter alia: Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy . In: The New England Journal of Medicine . tape 362 , no. 9 , March 4, 2010, p. 790–799 , doi : 10.1056 / NEJMoa0902014 (English).
- ↑ Tracy A. Glauser, Avital Cnaan, Shlomo Shinnar, Deborah G. Hirtz, ao: Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy: initial monotherapy outcomes at 12 months . In: Epilepsia . tape 54 , no. 1 , 2013, p. 141-155 , doi : 10.1111 / epi.12028 (English).
- ↑ Psychiatric practice. Volume 36, 2009, p. 258.
- ↑ a b Psychiatric Practice. Volume 36, 2009, p. 258, quoted from Süddeutsche Zeitung . January 26, 2010, p. 16.
- ↑ S. Bauer, H. Baier, C. Baumgartner et al .: Transcutaneous vagus nerve stimulation (tVNS) for treatment of drug-resistant epilepsy: a randomized, double-blind clinical trial (cMPsE02) . In: Brain Stimulation . tape 9 , 2016, p. 356–363 , doi : 10.1016 / j.brs.2015.11.003 (English).
- ↑ T. Hinterberger, B. Kotchoubey, J. Kaiser, A. Kübler, N. Neumann, J. Perelmouter, U. Strehl, N. Birbaumer: Applications of self-control of slow cortical potentials. In: behavior therapy. 10, 2000, pp. 219-227. doi: 10.1159 / 000056631
- ↑ Mark J Cook, Terence JO Brien, Samuel F Berkovic, Michael Murphy, Andrew Morokoff, Gavin Fabinyi, Wendyl D Souza, Raju Yerra, John Archer, Lucas Litewka, Sean Hosking, Paul Lightfoot, Vanessa Ruedebusch, W Douglas Sheffield, David Snyder , Kent Leyde, David Himes: Prediction of seizure likelihood with a long-term, implanted seizure advisory system in patients with drug-resistant epilepsy: a first-in-man study. In: The Lancet Neurology. June 2013, pp. 563-571. doi: 10.1016 / S1474-4422 (13) 70075-9
- ^ Rainer Tölle : Psychiatry . Child and adolescent psychiatric treatment by Reinhart Lempp . 7th edition. Springer Verlag, Berlin 1985, ISBN 3-540-15853-7 , p. 299.
- ↑ National Sentinel Clinical Audit of Epilepsy-Related Death 2002 . (PDF; English)
- ^ Karl-Heinz Leven : The "unholy" disease - epilepsia, moon addiction and obsession in Byzantium. In: Würzburg medical history reports. Volume 13, 1995, pp. 17-57, here: pp. 17-29.
- ↑ Evert Dirk Baumann: The Holy Disease. In: Janus. 29, 1925, pp. 7-32.
- ↑ L. Jilek-Aall: Morbus sacer in Africa: some religious aspects of epilepsy in traditional cultures. In: Epilepsia. Volume 40, Number 3, March 1999, pp. 382-386. PMID 10080524 .
- ↑ Hippocrates: About the sacred disease. Chapters 1, 2, 7.
- ↑ The Hippocratic pamphlet "On the Holy Disease". Ed., Translated and explained by Hermann Grensemann , Berlin 1968 (= Ars Medica. Texts and investigations on the sources of ancient medicine , II, 1).
- ^ Max Wellmann : The text "Peri hiërēs noúsou" of the Corpus Hippocraticum. In: Sudhoff's archive. Volume 22, 1929, pp. 290-312.
- ^ Owsei Temkin : The doctrine of epilepsy in the Hippocratic writings. In: Bulletin of the History of Medicine. 1, 1933, pp. 277-322.
- ↑ Jutta Kollesch , Diethard Nickel : Ancient healing art. Selected texts from the medical writings of the Greeks and Romans. Philipp Reclam jun., Leipzig 1979 (= Reclams Universal Library. Volume 771); 6th edition ibid. 1989, ISBN 3-379-00411-1 , pp. 30 and 127-133.
- ↑ Horst Kremling : On the development of clinical diagnostics. In: Würzburg medical history reports. 23, 2004, pp. 233-261, here: p. 248.
- ^ Karl-Heinz Leven: The "unholy" disease - epilepsia, moon addiction and obsession in Byzantium. In: Würzburg medical history reports. 13, 1995, pp. 17-57.
- ↑ a b c German Epilepsy Museum
- ↑ Susanne Hahn: Epilepsy (modern times). In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. de Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 362.
- ↑ People suffering from epilepsy during the National Socialism (topic on the website of the German Epilepsy Museum in Kork)
- ^ Max Höfler: German book of names of diseases. Piloty & Loehle, Munich 1899 (Reprographic reprint: Olms, Hildesheim and New York 1970 and 1979, ISBN 1-174-35859-9 ), p. 703 f.
- ↑ Victor Metzner: "Weeds", a fatal childhood disease. In: Würzburg medical history reports. Volume 13, 1995, pp. 417-422.
- ↑ epilepsiemuseum.de
- ↑ Eckart Roloff , Karin Henke-Wendt: Epilepsy, the disease of innumerable names. (The German Epilepsy Museum Kehl-Kork). In: Visit your doctor or pharmacist. A tour through Germany's museums for medicine and pharmacy. Volume 2: Southern Germany. Verlag S. Hirzel, Stuttgart 2015, ISBN 978-3-7776-2511-9 , pp. 62-65.
- ↑ Living together with epilepsy - German Epilepsy Association. In: www.epilepsie-vereinigung.de. Retrieved June 28, 2016 .
- ↑ epilepsie-vereinigung.de
- ↑ epilepsie-elternverband.de
- ↑ epilepsie-online.de
- ↑ epilepsie.at
- ↑ epilepsie-ig.at
- ↑ epi-suisse.ch