measles
| Classification according to ICD-10 | |
|---|---|
| B05 | measles |
| B05.0 | Measles complicated by encephalitis |
| B05.1 | Measles complicated by meningitis |
| B05.2 | Measles complicated by pneumonia |
| B05.3 | Measles complicated by otitis media |
| B05.4 | Measles with intestinal complications |
| B05.8 | Measles with other complications |
| B05.9 | Measles without complication |
| ICD-10 online (WHO version 2019) | |
Measles or morbilli are highly contagious infectious diseases that mainly affect children. In addition to the typical red patches of skin (measles rash ), the disease causes fever and a considerably weakened general condition . This so-called childhood disease is caused by the measles virus and in some cases can be life-threatening due to severe progress ( complications ) with pneumonia and brain infections . In most countries, the disease is notifiable .
The diagnosis is made by the clinical picture and an antibody detection in blood. There is no specific therapy, but the disease and thus also the complications can be prevented by vaccination from the age of twelve months. The World Health Organization (WHO) aims to eradicate measles worldwide. In the past, vaccinations have significantly reduced the number of illnesses, from 1980 to 2013 by over 95%. As a result of the increasing aversion to vaccination in industrialized countries and the global migration movement, measles cases have risen again by 30% worldwide in recent years. In January 2019, the WHO therefore declared measles a threat to global health. It is therefore strongly recommended that adults and children be checked and supplemented with measles vaccination coverage when preparing for travel. In regions with a high vaccination rate, such as North and South America, measles has already been de facto eradicated apart from a few imported cases, where fewer than 2000 cases were confirmed in 2014.
The Latin name morbilli is a diminutive ( diminutive ) of Latin morbus "disease".
Epidemic situation
world
| WHO region | 1980 | 1990 | 2000 | 2005 | 2010 | 2013 |
|---|---|---|---|---|---|---|
| Africa | 1,240,993 | 481.204 | 520.102 | 316.224 | 199.174 | 83,613 |
| America | 257.790 | 218,579 | 1,755 | 253 | 247 | 294 |
| Eastern Mediterranean | 341,624 | 59,058 | 38,592 | 15,069 | 10,072 | 20,884 |
| Europe | 851.849 | 234,827 | 37,421 | 37,332 | 30,625 | 26,396 |
| South East Asia | 199,535 | 224,925 | 78,558 | 83,627 | 54,228 | 31,246 |
| Western Pacific | 1,319,640 | 155,490 | 177.052 | 49,460 | 49,460 | 31,706 |
| Worldwide | 4,211,431 | 1,374,083 | 853.480 | 580.287 | 343,806 | 194.139 |
The measles virus occurs worldwide, with the incidence of the disease varying greatly. Local measles epidemics with high disease and mortality rates occur time and again, particularly in developing countries . Measles is one of the most common infectious diseases there. The WHO estimates that they caused nearly half of the 1.7 million vaccine- preventable deaths in children in 2000 , out of an estimated 30 to 40 million cases that year. The number of reported diseases is far below these estimated values due to the high number of unreported cases (see table).
On the other hand, the virus has already been largely eliminated through large-scale vaccination campaigns in various other regions, such as the entire American double continent (see graphic). This was made possible by the fact that humans are the sole hosts of the measles virus. In 2001 the WHO and UNICEF presented a plan with the aim of halving the child mortality rate by 2005 through global vaccination programs. While exact data are still pending, various reports show that this goal has been largely achieved. Between 1999 and 2003, measles mortality was reduced by 39% worldwide, with death rates still high in Africa and Southeast Asia. In 2005, the World Health Assembly of the WHO adapted these plans and formulated the goal of a 90 percent reduction in global mortality for 2010. According to the WHO, this goal was not achieved. From 535,300 (estimated) measles deaths worldwide in 2000, the number had fallen to 139,300 by 2010, a decrease of 74%.
At the beginning of 2020, the WHO said that a measles epidemic in the Congo that broke out one year earlier was "currently the worst measles outbreak worldwide". It has led to more than 6,000 deaths.
Europe
The total number of recorded diseases in Europe fell significantly from 1990 to 2004, while monitoring and reporting systems improved. The frequency of the cases is, due to the varying vaccination rates, very different. While it is very low in some regions, such as the Scandinavian countries - there have been only four imported cases in Finland since 1996 - it is often not yet the case in Central and Eastern Europe. There are repeated local outbreaks of disease due to vaccine picking. Despite mandatory reporting in most countries, there is probably a high number of unreported cases, and the number of actual cases of illness is significantly higher than the number of reported cases. In 2011, the World Health Organization (WHO) appealed to EU member states to step up measures to combat measles.
Far more cases of measles were reported in 2018 than in any other calendar year of the decade.
America
By 1994, nearly all states in the United Nations Region of America had introduced vaccination programs for children. As a result, the average number of new cases fell from 250,000 to around 100 cases per year, and measles is now considered to be effectively eradicated. There are still isolated outbreaks of disease regionally, almost all of which are imported or can be traced back to imported measles. America is thus cited as an example that measles can be controlled through vaccination programs worldwide.
In the meantime, genuine, i.e. not imported, measles diseases hardly occur in the states of North and South America, including the Caribbean. The Centers for Disease Control and Prevention no longer regards measles as an endemic disease in the United States . At the end of September 2016, the Pan-American health organization reported the American double continent as measles-free.
However, there was an increase in measles cases in the USA after 2016. The starting point was people who had come to the USA from countries with an endemic occurrence of measles and then spread the virus to subpopulations that are not herd immunity in the USA . As of the beginning of January, as of July 3, 2019, over 1,109 cases of measles have been reported in 28 states in the United States. This is the largest number of cases since 1992.
Situation by state
Germany
| year | cases |
|---|---|
| 2001 | 6039 |
| 2002 | 4656 |
| 2003 | 777 |
| 2004 | 123 |
| 2005 | 781 |
| 2006 | 2308 |
| 2007 | 566 |
| 2008 | 915 |
| 2009 | 572 |
| 2010 | 780 |
| 2011 | 1608 |
| 2012 | 165 |
| 2013 | 1768 |
| 2014 | 442 |
| 2015 | 2465 |
| 2016 | 325 |
| 2017 | 929 |
| 2018 | 544 |
| 2019 | 514 |
In 2005 there were two major measles outbreaks in Germany , in February in Hesse with one death in 223 cases and in May in Upper Bavaria with 110 cases. In 2006 measles accumulations were reported in Baden-Württemberg and North Rhine-Westphalia (well over 1500 cases there).
In 2013 there was an epidemic in Munich . According to the health department there, 220 cases were registered from April to early June, compared with 7 in the previous year. Over half of the patients had to be treated in clinics, especially adolescents and young adults who were ill. A schoolgirl then brought the virus to a Waldorf school in the Rhein-Erft district , where there was another measles outbreak in July 2013 with a vaccination rate of only 25% in 400 schoolchildren. 54 people fell ill, 29 of them young people and adults. Three patients had to be treated as inpatients in the hospital. Since the teachers' vaccination protection was very low, the school had to be closed for six days.
Between September 29, 2014 and September 27, 2015 (season year from calendar week 40) 1392 measles cases were reported in Berlin, which corresponds to an incidence of 407 per 1 million inhabitants. In Thuringia, Saxony, Hamburg and Brandenburg the incidences were between 45 and 75. In Germany, 2,465 cases reported during this period resulted in an incidence of 30.1. Most illnesses (over 1000 in Berlin) were reported from January to April. The virus strain was presumably brought in by asylum seekers from Bosnia and Herzegovina and Serbia , who were also the first to fall ill. In Bosnia and Herzegovina, a major measles epidemic has been raging since February 2014 with several thousand affected. The data in the Epidemiological Bulletin in 2013 raised concerns that measles would soon become endemic again in Germany ; however, this has not yet happened.
In the GDR there was compulsory vaccination against measles. In 2016, 93 percent of children in Germany were sufficiently vaccinated against measles when they entered school . As children attending Waldorf schools are less likely to be vaccinated, measles is a common occurrence there.
Between 2001 and 2018, eight deaths from measles have been registered, and complications have been reported in between 1.1 and 8.4 percent of all reported measles cases. In Germany, the mandatory vaccination was introduced on March 1, 2020.
Austria
In Austria , before the introduction of compulsory measles reporting in 2001, the Institute of Virology (Vienna) operated a voluntary reporting system that covered around 8% of the Austrian population. Thus, for the period from 1993 to 1997 about 28,000 to 30,000 measles cases could be extrapolated for the whole of Austria, with an increased incidence of measles cases in 1996 and 1997 in particular. The number of annual cases between 2003 and 2007 was less than 100 per year. From March 2008, a measles epidemic spread from a Waldorf school in the Salzburg area to almost all Austrian and two German federal states. 241 cases were reported in Salzburg, 146 in Upper Austria , 22 in Vienna , 13 in Tyrol and 10 in Vorarlberg . In connection with this epidemic, according to information from the Bavarian authorities, a total of 217 people fell ill in four Upper Bavarian districts between mid-March and mid-July 2008. The Department of Virology at the Medical University of Vienna, on the other hand, attributes only 50 measles cases in Bavaria, 2 in Baden-Württemberg and 4 measles cases in Norway directly to this outbreak. Only 21 of the total of 443 measles infections reported in Austria in 2008 were not part of the Salzburg outbreak, but were imported to Austria through trips from countries such as Switzerland, Germany, Spain and India.
Switzerland
In 1997 there was an epidemic in Switzerland with 6,400 diseases. The data from Switzerland is based on the Sentinella reporting system . After 574 cases in 2003, significantly lower incidence rates were reported with 39 cases in 2004 and 60 cases in 2005. From November 2006 a new epidemic spread. More than 1,100 illnesses had been reported by the end of 2007, with the focus being in the canton of Lucerne . At the beginning of 2008 the situation worsened, especially in north-western and eastern Switzerland, and by mid-March there were already 734 new measles cases. Various canton doctors therefore recommended preventive measles vaccinations. In February 2009 around 40 students at the Rudolf Steiner School in Crissier contracted measles. As a result, 250 students were banned from school for three weeks. In Geneva , a twelve-year-old girl from France died of measles. From December 2010 to January 2011, 31 cases were reported at the Rudolf Steiner School in Basel in Switzerland. In February 2017, a young adult died whose immune system was weakened as a result of leukemia. More than a thousand cases were reported in 2007 and 2009, and over two thousand in 2008. In 2011 and 2013 three-digit case numbers were reported, in 2010, 2012 and 2014 to 2016 double-digit case numbers were reported. In 2019, measles cases increased again significantly. By mid-April, 138 measles cases with two deaths had been reported. By the end of the month the number of sick people rose to 155; 2013 was the last time that so many case numbers were reported.
Finland
In Finland only four imported cases occurred between 1996 and 2003. Finland is one of the first countries in the world to have been able to eliminate measles (from 1996) and also mumps and rubella (1997). For the success in Finland, a large network of health facilities, which had already administered the majority of vaccinations, was established in the 1980s. Currently (2019) a few single vaccinated or unvaccinated people fall ill every year in connection with travel to endemic areas. The vaccination coverage is between 95 and 97%.
Israel
In 2008, the CDC reported an outbreak of measles in Israel, where more than 900 cases were reported, 700 of them in Jerusalem and Beth Shemesh .
Italy
In 2002, another local epidemic occurred in the Campania region of southern Italy , with 1,571 cases, three of which were fatal. Following the outbreak of a measles epidemic in early 2017 (with over 5,000 reported cases), compulsory vaccination against measles was introduced in Italy. In 2018, the reported cases of illness were halved to 2,548, and there were seven deaths.
Congo
At the beginning of 2019 there was a measles epidemic in which over 300,000 fell ill and around 6,000, mainly children, died.
Netherlands
In the Netherlands , an epidemic of measles is observed at regular intervals due to an orthodox- Protestant population group (Orthodox reformeerde kerken ) who refuse to be vaccinated for religious reasons. In the so-called Bible Belt , after outbreaks in 1976 and 1988, there was another outbreak in 1999 with 2961 diseases and three deaths, between May 2013 and March 2014 over 2600 measles cases were reported, 182 were treated in hospital and one child died. Because of the low vaccination rate of around 60% among children, measles epidemics of roughly the same proportions occur in the Bible Belt around every 12 years (around 2,500 cases of measles reported).
North Korea
In North Korea , measles has been considered eliminated since 2018.
East Timor
In East Timor , measles has been eliminated since 2018.
Pakistan
In Pakistan, after more than 300 measles deaths were counted in 2012, more than 300 children died of the disease in another severe measles outbreak in 2013. More than 8,000 measles cases were confirmed there in 2012 and 2013.
Romania
In Romania, more than 3,600 people contracted measles in 2005 and ten children died of it. There was also a major measles epidemic after 2016, in which over 11,000 people fell ill and at least 40 died of it.
Samoa
Around 200,000 people live in Samoa who had a particularly low vaccination rate of 28% to 40%. In mid-November 2019, so many measles cases had occurred that a state of emergency was declared and an exit ban was imposed. A vaccination campaign was started on November 20, 2019, in which 58,000 people between the ages of six months and 60 years, or almost 30% of the population, had been vaccinated by December 2, 2019. At the end of December 2019, the six-week state of emergency was declared over, from November 2019 to December 29, 2019 around 5,600 measles cases were reported and 81 people died from it, mostly babies and young children. The vaccination rate has now reached 95%.
South Africa
A measles epidemic raged in South Africa from 2009 to 2011 with over 18,000 reported cases (13,000 laboratory-confirmed).
Tanzania
According to WHO statistics, the vaccination rate for measles vaccination in Tanzania is 99%, even though the data are based on population projections from a 2012 census. Vaccinations accounted for 20% of the sharp decline in child mortality among children under five.
United States
Unlike in developing countries , as in other developed countries, the mortality rate from measles infections due to various causes (better general living conditions, effective treatment of measles pneumonia) had decreased in the USA - in 1912 25 deaths per 1000 reported measles cases were registered, in 1962 this rate fell to 1 Death per 1000 reported measles cases. Because the number of measles infections remained high, two vaccines were approved and increasingly used in the USA in March 1963: a live vaccine from MSD (attenuated vaccine strain Edmonston B) and a dead vaccine from Pfizer . In September 1963, 25,000 people were vaccinated with the live vaccine; By mid-1966, nearly 15 million children were receiving one of the two vaccines. The number of measles cases per year in the United States then fell from over 400,000 to under 100,000 since 1967 and to under 7,000 since 1981. However, there was an increase in the number of cases from 1989 to 1991. In these three years combined 55,622 cases were reported, of which 123 ended fatally. Mainly toddlers from Hispanic American and African American families were affected, in whom the rate of unvaccinated children was significantly higher than in the general population. From 1993 to 2016, the number of illnesses reported annually was between 963 and 37.
An unvaccinated teenager sparked an outbreak of measles in two Orthodox Jewish communities in Brooklyn , New York in 2013 after contracting it in London .
In September 2016 measles was declared eradicated in America, but local outbreaks have occurred several times since then: In Minnesota, several dozen people fell ill from April 2017, in 2018 there were 17 outbreaks with a total of 372 affected people, in January and February 2019 there were 206 cases, most of which were attributed to travelers. In late April 2019, the CDC reported a new high of measles cases, at 695. This is the highest level since the US health authority officially announced the eradication of the disease in the US in 2000. Cases of measles have been reported in 22 states registered, with New York and Washington DC recording the most infections. The 2019 New York measles outbreak is believed to be the largest since 1991 and resulted in a medical emergency and mandatory vaccination.
Pathogen
properties
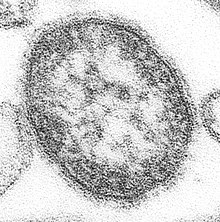
The measles virus is a single-stranded RNA virus from the family of paramyxoviruses (genus Morbillivirus) that occurs exclusively in humans ( pathogenic to humans ), about 120-140 nanometers in size. It is closely related to the canine distemper virus and most closely related to the meanwhile eradicated rinderpest pathogen .
The envelope of the measles virus contains the surface proteins hemagglutinin (H protein) and fusion protein (F protein) as well as a matrix protein (M protein). H and F proteins are responsible for fusion with and uptake by the host cell . The cellular receptors through which the virus is taken up into human cells are CD150 and nectin-4. Nectin-4 is presented by epithelial cells , CD150 by certain cells of the immune system ( lymphocytes , monocytes , macrophages and dendritic cells ). These cells therefore play a major role in the pathogenesis of measles infection (with the wild virus). The CD46 receptor serves as an additional cellular receptor in vaccinations with measles vaccines . The antibodies produced (induced) by the vaccination are directed against the surface proteins of the measles virus, in particular against the H protein.
The WHO defines 24 known genotypes (variations of the genetic information) in eight groups (A – H). The genome mutation rate is comparatively low, which means that worldwide (geographical) routes of infection can be traced. In Central Europe, the genotypes B3 and D8 mainly occur. The measles outbreaks in Switzerland and Lower Bavaria in 2006/2007, however, were caused by the genotype D5 from Thailand or Cambodia. This enabled the detection of a chain of infection from Switzerland to Lower Bavaria and from there to Austria and Hanover, since genotype D5 otherwise only occurs in individual cases in Central Europe. Furthermore, there is only one stable serotype (combination of surface features of the pathogen), which is why a highly effective vaccine could be produced.
The virus is very sensitive to external influences such as increased temperatures , ultraviolet radiation (light) and, due to its virus envelope, to fat solvents and disinfectants . The virus remains infectious for only two hours in the air.
Transmission and body defense
The measles virus is transmitted through direct contact or through droplet infection . Measles is infectious three to five days before the rash breaks out and up to four days afterwards. The measles virus enters the body through the epithelial cells of the lining of the respiratory tract or, less often, through the conjunctiva of the eyes. Due to its high infectiousness, the virus leads to an infection after a short exposure ( contagion index of almost 1). The viruses multiply in the regional lymph nodes and after about 48 hours spread via the bloodstream into the reticulohistiocytic system . This is accompanied by a mostly brief appearance of the virus in the blood ( viraemia ). After about 5–7 days, there is a second viraemia with subsequent infection of the skin and the respiratory tract. This triggers the characteristic rash (measles rash) and the runny nose-like symptoms, cough and acute bronchitis . The invasion of T-lymphocytes by the virus and increased levels of messenger substances ( cytokines ), especially interleukin-4 , cause a temporary weakness in the body's defenses. During this phase, which lasts about four to six weeks, this can lead to further (secondary) infections.
Before the rash begins, the body's defense is primarily based on the cellular immune system (cytotoxic T lymphocytes, natural killer cells ). Patients with decreased immunity due to a weakening of this part of the immune system are at high risk of measles infection, which can be severe. An immune deficiency that is limited to the area of the humoral immune system , however, does not lead to an increased risk of the disease. Immune reactions in small blood vessels ( capillaries ) play an important role in the development of the typical reddening of the throat (enanthemum, Koplik spots) and skin reddening (exanthema, see below) . Therefore, these signs may be absent in immunocompromised patients (white measles) , although the disease is severe. With the onset of the rash, the formation of antibodies begins , first of the IgM class , later also of IgG .
Clinical picture
Symptoms and course of the disease
A two-phase course of the disease is typical for measles: The incubation period of 8 to 10 days is followed by the three to seven days long, uncharacteristic prodromal stage , also known as the initial stage . This manifests itself as an inflammation of the mucous membranes of the upper respiratory tract ( catarrh with rhinitis ), partly also of the middle respiratory tract as dry bronchitis , as well as the conjunctiva ( conjunctivitis ). The symptoms in this stage of the disease are therefore also described with the words "rotten, weeping, swollen". This can lead to a fever of up to 41 ° C, nausea, sore throat and headache . The head stains on the cheek mucosa opposite the anterior molars ( premolars ), which only occur in measles , are rarely observed and are considered by some authors to be atypical signs of measles infection. These white, lime splatter-like spots on a reddened surface are 1–2 mm in size and appear shortly before the later rash appears.
On the 12th to the 13th day, the disease changes to the typical exanthema stage , which often begins with a typical reddening of the mucous membrane ( enanthemum ) on the soft palate . On the 14th to 15th day, a spotty, nodular ( maculo-papular ), partly confluent, large-spotted rash ( exanthem ) - typically starting behind the ears (retroauricular) - spreads over the entire body within 24 hours. Symptoms usually subside after another four to five days. As a remnant of the exanthema, bran-shaped scaling can remain for a short time. Concomitant swelling of the lymph nodes ( lymphadenopathy ) often occurs. The disease is often more severe in adults than in children, although the symptoms are the same. Since the disease is more difficult to diagnose in adults, treatment that starts later and resulting complications, such as measles pneumonia, occur.
The feverish course of the disease is often bimodal, with the first peak occurring during the prodromal and the second during the later exanthema stage. In between there is often a short defervescence. In uncomplicated cases, this is followed by rapid recovery and lifelong immunity .
Atypical progression pictures
Atypical courses occur in different situations. Infants with loan immunity from maternal antibodies or patients who have received antibody preparations develop a weakened form of the disease (mitigated measles) .
In people with immunodeficiency , the course can be very different, for example the typical rash may be missing (white measles) . This group includes patients with congenital defects of the cellular immune system, HIV infections, malignant tumors or immunosuppressive therapy . You have a high risk of developing a severe and protracted course of measles with increased complication and mortality rates.
Under atypical measles is defined as a severe form that occurred in patients after vaccination with a formalin vaccine when they were later confronted with a wild-type measles virus. These vaccines were used in the United States and Canada in the 1960s. In addition to the very pronounced symptoms, which mostly did not run in the typical order, there were pleural effusions , liver inflammation and edema of the arms and legs. Despite the severity of the disease, the prognosis was good and the patients made a full recovery.
Complications
While two thirds of the illnesses are uncomplicated, additional side effects and complications occur in around 20-30% of cases, with diarrhea (in 8% of cases), otitis media (7%) and pneumonia (6%) being the most common. There are also a number of other complications.
There are various statements about the death rate . The Robert Koch Institute states a mortality rate of 1: 1000. The American health authority CDC assumes a mortality of 1: 500 to 1: 1000. The Center for Prevention and Disease Control of the EU calculated a mortality rate of 3: 1000th In developing countries the death rate is much higher, sometimes up to 25%. Pneumonia is the most common fatal complication.
Measles Pneumonia
Under a primary measles pneumonia , pneumonia is the history image of a interstitial pneumonia with inflammation of the small bronchi ( bronchiolitis understood), mainly as a breathing disorder ( dyspnea expressed). It is difficult to diagnose with a physical exam so an X-ray will be required.
The epithelium of the respiratory system is directly damaged by the measles virus, thereby a loss of cilia (will cilia ) observed. This damage represents a predisposition to bacterial infections (bacterial superinfections ). Such an infection occurs as bronchopneumonia , especially after or with simultaneous interstitial viral pneumonia . However, it is also possible in isolation due to the measles-related weak immune system (see above).
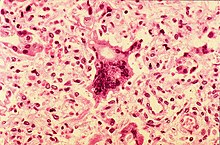
A rare form of viral pneumonia is giant cell pneumonia with multinucleated giant cells ( giant pike cells) derived from the alveolar epithelia , which is typical for measles and whooping cough , but rarely occurs in diphtheria or flu . It occurs mainly in debilitated patients and has a poor prognosis.
Meningoencephalitis
Inflammation of the brain and its skins ( meningoencephalitis ) is rare (in 0.1% of diseases), but is fatal in 10–20% of cases. Permanent brain damage remains in a further 20–30%.
Meningoencephalitis can develop four to seven days after the onset of the exanthema, more often in patients over six years of age than in young children. It manifests itself with fever, headache, meningeal irritation (neck stiffness, vomiting) and disturbances of consciousness up to coma . Severe forms of the course are expressed in epileptic seizures and other neurological dysfunction. During the lumbar puncture , the brain water obtained shows a cell proliferation ( pleocytosis ) and an increased protein concentration. After the introduction of measles vaccination, the incidence of measles-induced meningoencephalitis fell continuously and is less than ten cases per year in Germany.
In children with congenital or acquired immunodeficiencies , a special form of encephalitis caused by measles viruses ("inclusion body encephalitis ", measles inclusion-body encephalitis , MIBE, from English measles for "measles") can occur in rare cases . This complication usually manifests itself within a year of measles infection with difficult-to-treat focal seizures and usually ends fatally within a few months. The diagnosis can be made by taking a tissue sample from the brain ( biopsy ). Cases caused by the vaccine virus have also been reported. People with a severe congenital or acquired immunodeficiency should therefore not be vaccinated against measles.
Subacute sclerosing panencephalitis
The subacute sclerosing panencephalitis (SSPE) is a late complication of measles infection, a generalized inflammation of the brain with nerve demyelination ( demyelination draws) and severe damage to brand and fatal in more than 95% of cases ends. The origin of the SSPE is not fully understood. Mutations in the proteins of the virus envelope seem to play a role, especially in the amino acids at positions 64 ( Pro ), 89 ( Glu ) and 209 ( Ala ) of the M protein (so-called PEA motif ). The Ala209 in particular is responsible for the increased spread of viruses within the body. This motif does not appear in vaccine viruses or laboratory strains; the following amino acids were identified at the respective positions: Ser , Lys and Thr (so-called SKT motif). This could explain why only wild measles viruses and not measles vaccine viruses have been found in tissue samples from SSPE-infected brains; in addition, there is no evidence that vaccination against measles could cause or accelerate SSPE.
The disease occurs months to ten years after a measles infection, on average after seven years. The course is slowly progressive over one to three years - the SSPE is one of the so-called slow virus infections . An acute, faster (3 to 6 months) or a slower course (longer than three years) occurs in 10% of cases.
Four stages of the SSPE can be defined. The first stage is characterized by irritability, dementia , lethargy , speech disorders and a decline in social interactions, the second by motor disorders such as dyskinesia , dystonia and muscle cramps ( myoclonus ). In the third stage, an extrapyramidal syndrome , spastic paralysis, and decerebration syndrome , in which the cerebrum is severely damaged, manifest themselves . The EEG shows typical changes that are groundbreaking for the SSPE ( Radermecker complex ). In the last stage, there is functional failure of the cerebral cortex , which leads to a vegetative state , akinetic mutism , the failure of vegetative functions (such as breathing, pulse, blood pressure) and ultimately death.
The incidence of SSPE was previously reported as 5 to 10 per 1 million measles cases. The more recent literature, however, assumes a frequency of about 1: 1,000 to 1: 5,000 or 1: 10,000 infected people, with children under 5 years of age the risk is 2 to 6: 10,000. Evaluations from California even showed a risk of 1: 1367 for children under 5 years and 1: 609 for children under one year. The absolute frequency of SSPE has been significantly reduced by the measles vaccination since the 1980s.
SSPE occurs in most cases in children or adolescents who had measles before they were two years old. Since children can only be vaccinated against measles from the age of 12 months, the only way to protect infants under 12 months from measles is through exposure prophylaxis , i. H. in avoiding dealing with potentially infectious, d. H. unvaccinated people.
SSPE was initially described as a rare neurological disease (sporadic encephalitis with a subacute course) at the beginning of the 20th century. The SSPE-associated visible changes were observed microscopically through the work of James R. Dawson in 1933; a viral cause was suspected. The name "SSPE" was first used in 1939. The work of John H. Connolly and co-workers in 1967 finally identified the role of measles virus in SSPE.
Weakened immune system
Measles is considered to be the first immunosuppressive disease to be described. The measles viruses spread particularly in the lymphatic system . They penetrate some cells of the immune system, especially lymphocytes, monocytes, macrophages and dendritic cells. This initially leads to immunosuppression with lymphopenia in the acute phase of the disease in the form of a sometimes drastic decrease in the amount of T and B cells circulating in the blood . This makes measles sufferers more susceptible to other bacterial or viral pathogens shortly after the measles infection.
Measles viruses also attack the memory cells of the immune system . As a result, immunity to other diseases can be lost or impaired in the medium term (“immunamnesia”). The extent to which the body's immune memory is erased varies from person to person and it can take two to three years for the body's defenses to recover. After a measles infection, infections by other pathogens are more frequent during this time. The mortality is increased due to the lost immunogenicity up to three years after an all-nighter measles infection. Measles vaccinations, on the other hand, lead to a sharp decline in these diseases in regions in which protection against other diseases is only possible to a limited extent due to a lack of resources, especially developing countries .
In October 2019, the finding that after a measles infection, contrary to previous assumptions, the human immune system tends to be weakened instead of strengthened, was confirmed again in a study by the British Sanger Institute . Measles viruses destroy B memory cells that produce antibodies when infected. This leads to the loss of immune memory and weakens the defense against other diseases. However, the weakened measles viruses injected as part of a vaccination do not trigger this loss of immune memory.
Conjunctivitis
Conjunctivitis, sometimes associated with inflammation of the cornea ( keratitis ) of the eye with multiple, punctiform, epithelial lesions , can also occur as a complication of measles infection. In developing countries, measles is one of the most common causes of blindness in children, especially in connection with vitamin A deficiency and / or immunodeficiency disorders caused by HIV or other diseases.
Other complications
A laryngitis with swelling of the mucous membrane leads to hoarseness and shortness of breath in the preliminary stages (see pseudo croup ), this is called "measles croup". Further complications are appendicitis , liver inflammation ( hepatitis ) or generalized swelling of the lymph nodes ( lymphadenitis ). Inflammation of the heart muscle ( myocarditis ), inflammation of the kidneys ( glomerulonephritis ) or a drop in blood platelets ( thrombocytopenic purpura ) are rare .
diagnosis
The diagnosis on the basis of the clinical picture, in particular the "typical" measles rash, is subject to a high frequency of errors due to the increasingly rare occurrence and atypical course pictures, so that additional examinations are necessary in order to be able to diagnose the disease with certainty. In the event of an epidemic, however, the diagnosis can often be made clinically, especially by experienced investigators.
The safest way to make the diagnosis is to use the serological detection of IgM antibodies . Nowadays this is mostly achieved methodically with the help of an enzyme immunoassay ( ELISA ), in some laboratories the complement fixation reaction (CFR) or the hemagglutination inhibition test (HHT) are also carried out. When determining the IgM antibodies, false positive and false negative results can occur. However, an at least fourfold increase in the measles IgG titer within about a week or a new appearance of IgG antibodies is valid evidence of a fresh infection. The combined determination of IgM and IgG antibodies offers increased security. The detection of IgM is generally positive when the rash breaks out, but can also be negative in the first few days. From the third day to about 4 to 6 weeks after the rash occurs, the IgM antibodies are usually detectable, so that retroactive detection of a disease is possible. IgG antibodies are usually not detectable before the 7th day after the onset of the rash.
Direct pathogen detection (replication of virus RNA using RT-PCR or virus cultivation in cell cultures ) is more time-consuming than indirect detection (antibody detection) and only makes sense for specific questions. However, it has the advantage that the pathogen can be genetically typed so that the transmission chains of the infection can be traced in detail. The pathogen detection in the CSF is only possible if measles encephalitis is suspected; Due to the instability of the virus RNA in the CSF, a negative PCR result does not rule out measles encephalitis. If SSPE is suspected, the direct pathogen detection is usually not successful, but the detection of measles IgM in the CSF.
In addition to the specific virus diagnosis of measles, blood tests (laboratory diagnosis) show a reduction in white blood cells ( leukopenia ), in particular lymphocytes ( lymphopenia ) and eosinophilic granulocytes ( eosinopenia ), as well as a temporary reduction in blood platelets ( thrombocytopenia ). When the brain is infected, there is an increased protein concentration and an increase in lymphocytes (lymphocytic pleocytosis ) in the cerebrospinal fluid ( liquor ).
Differential diagnosis
In the differential diagnosis, scarlet fever and rubella are most likely to be considered in the clinical diagnosis . In scarlet fever, the rather fine-spotted rash begins in the groin or armpit region and rises from there to the head, where it leaves out the mouth-chin triangle. The so-called raspberry tongue and pharyngitis (sore throat) are also typical . The rubella usually shows only a mild clinical picture with moderate fever and a weak, non-confluent exanthem on the neck and chest. Strong swelling of the lymph nodes in the neck is typical here. In addition to these diseases, rubella , Pfeiffer glandular fever , toxoplasmosis , mycoplasma infections , Kawasaki syndrome and drug allergies are also possible . By detecting specific antibodies in the presence of anti-measles IgM antibodies, these diseases can be excluded.
Reporting requirement
In Germany, according to Section 6 of the Infection Protection Act (IfSG), suspected illness, illness and death from measles have been reportable since 2001 , as well as direct or indirect detection of the measles virus according to Section 7 IfSG . In addition, illness or death from SSPE as a result of a measles infection must be reported (Section 6 (2) sentence 1 IfSG). Heads of community facilities are obliged to report to the health department if they become aware of cases of illness according to Section 34 IfSG. If there is a suspicion or actual illness, there is a ban on working and staying in communal facilities.
In Austria there has been a reporting obligation since December 1997 (Federal Law Gazette II No. 456/2001 Ordinance: Notifiable Communicable Diseases, now in accordance with Section 1 (1) Epidemic Act 1950 ), in Switzerland since March 1999 (Reporting Ordinance, SR 818.141.1, now according to number 30 of Annex 1 of the Ordinance of the FDHA on the reporting of observations of communicable diseases in humans ).
therapy
There is no specific antiviral therapy against the measles virus. Bed rest should be observed in the acute phase of the illness. As symptomatic therapy, fever-lowering drugs ( antipyretics ) and cough suppressants ( antitussives ) can be used. Since the body needs more fluid when it is fever , it is essential to drink a lot. Bacterial superinfections ( secondary infections ) such as inflammation of the middle ear (otitis media) or pneumonia (pneumonia) are treated with antibiotics .
In children aged 6 months to 5 years, especially children under 2 years of age, various studies in developing countries have shown a beneficial effect of vitamin A administration on the complication rate (blindness or eye damage) and mortality in the presence of vitamin A deficiency. The mechanism of action is not yet fully understood; Vitamin A promotes the cell exchange of epithelial cells, particularly in the respiratory and digestive tract. The WHO recommends twice administering vitamin A in the event of illness. Repeated doses of 200,000 IU show clinical effects. There are no studies on vitamin A therapy in western industrialized countries. The recommendations of the Robert Koch Institute do not contain any vitamins. On the other hand, vitamin A administration is not suitable for prevention ; only protective vaccinations are effective for this.
The antiviral agent ribavirin is effective against the measles virus in vitro ; There are no studies on its use in humans; there are only individual case reports in which administration of ribavirin (possibly together with interferon α ) was beneficial. The German Society for Pediatric Infectious Diseases states that in immunosuppressed individuals with severe disease, antiviral therapy with ribavirin in combination with immunoglobulins should be considered in individual cases .
The role of steroids in treating measles pneumonia is also discussed, but again there are only case studies.
Community facilities may not be visited during the illness (see below). By passive or active immunization after exposure, the disease can be alleviated or prevented under circumstances ( post-exposure prophylaxis , s. U.).
prevention
quarantine
According to the German Infection Protection Act (IfSG) from 2001, infected people are not allowed to visit community facilities until they can no longer secrete viruses and no longer infect other people after the disease has subsided. Community facilities are understood to mean other institutions in which mainly infants, children or young people are cared for, such as crèches, kindergartens, day-care centers, day-care centers, schools or other training facilities, as well as homes and holiday camps. The same regulation also applies to the employees of these facilities ( Section 34 of the Infection Protection Act). Similar regulations exist in other countries. So-called " measles parties " - organized meetings at which children who have not been vaccinated against measles are supposed to infect children who are acutely infected with measles - are relevant under criminal law.
For hospitals and care facilities in Germany, the recommendation of the Commission for Hospital Hygiene and Infection Prevention (KRINKO) applies, according to which infected people should be isolated up to four days after the onset of the rash , and immunosuppressed patients for the entire duration of the symptoms.
vaccination
Vaccination against measles is considered to be the most effective way to prevent the disease from occurring. Vaccinations were estimated to have reduced measles deaths by 79% from 2000 to 2015. Vaccination is basically possible with a single vaccine, this is mainly done in Africa or Russia. In Germany, Europe and North America this is usually carried out as a measles-mumps-rubella vaccination (MMR) or measles-mumps-rubella-chickenpox vaccination (MMRV) with a combination vaccine.
In this context, the Robert Koch Institute announces that a "... combination vaccine ... is basically not worse tolerated than a single vaccine". The measles vaccination is an attenuated live vaccine which , after a single vaccination, provides sufficient protection against measles in 95% of children. Since sporadic measles epidemics are to be expected at intervals of several years with a vaccination coverage rate of less than 95%, vaccination gaps must be closed with a second vaccination four weeks after the first at the earliest, in order to guarantee vaccination failures ( non-responders ) . Therefore a second vaccination was recommended in the case of measles. Extensive studies show that excellent protection against measles is possible with two vaccinations. After a double MMR vaccination, over 99% develop lifelong immunity, which can be determined by a titer-independent detection of measles IgG. The MMR vaccination can be combined with other vaccinations. The vaccination does not lead to a lasting weakening of the immune system, as is the case with measles.
Contraindications to vaccination are acute infections , HIV- positive and other immunocompromised patients (e.g. corticosteroid therapy, leukemia ), pregnancy and a history of gelatin allergy or a history of blood platelets ( thrombocytopenia ). In the event of contact with measles viruses , immunoglobulins are injected as post-exposure prophylaxis for these contraindications .
According to the vaccination calendar of the Standing Vaccination Commission at the Robert Koch Institute , the first MMR vaccination is scheduled for all children between the ages of 11 and 14 months, and the second between 15 and 23 months. Since the summer of 2006, a combination vaccine has also been approved that also contains a chickenpox component and thus further simplifies the vaccination schedule. This vaccine is also given twice at the same times. “Care must be taken that the second MMR vaccination is made up as early as possible, but no later than the age of 18; In girls, this also ensures the essential protection against rubella embryopathy . ”In 2012, 92.4 percent of children who started school in Germany were vaccinated twice against measles.
In Austria , two partial vaccinations against measles, mumps and rubella are recommended from the age of 9 months, with a minimum interval of four weeks. When entering school or at the age of 12, the vaccination status (vaccination certificate) should be checked. Missing vaccinations can be made up for free at any age. A survey by the Ministry of Health from 2016 found that over 95 percent of 6-year-old children have been vaccinated against measles at least once. In the 2- to 5-year-old children, however, the vaccination rate is only 92 percent, and about 10 percent of them are only vaccinated once instead of twice.
The recommendations of the Federal Office of Public Health and the Swiss Commission for Vaccination Issues call for two MMR vaccinations at the age of 12 and 15–24 months. The WHO estimates the vaccination rate in Switzerland for 2006 at 86% for the first vaccination and 70% for the second vaccination.
If a child is about to be admitted to a children's facility, the MMR vaccination can also take place before the age of twelve, but not before the age of nine, as maternal antibodies that are still present in the infant's blood during the first year of life can neutralize the vaccine viruses. Even if parents or vaccinees indicate that they have already had measles, mumps or rubella, the MMR vaccination is recommended. Anamnestic information about measles or rubella disease is unreliable and not usable without microbiological-serological documentation of the disease. A serological test for measles-specific IgG antibodies before the second vaccination and the waiver of the same if the titer is sufficient is possible. However, all current vaccination recommendations provide for a routine second vaccination without prior diagnosis.
Vaccination not only protects the majority of those vaccinated, but also newborns and infants from the first vaccination or vaccination failures and immunosuppressed people who cannot be vaccinated, thanks to the herd immunity . An effective vaccination ideally not only protects the individual but also has a social dimension. To eradicate measles, a vaccination rate of over 95% of the population is required. While America achieved this goal back in 2016, measles is endemic in 11 out of 53 countries in Europe .
A third MMR (V) vaccination is discussed in the literature; further studies are required for this.
Introduction of mandatory vaccination
In May 2019, the German Federal Ministry of Health presented a draft bill for a measles protection law, which provides for the introduction of compulsory vaccinations , including fines and a ban on day-care centers. The ministerial draft and its details were discussed controversially both in politics and among medical associations. On July 17, 2019, the federal government approved the bill. The Bundestag approved a majority on November 14, 2019; the approval of the Bundesrat was not required. The law came into force on March 1, 2020 ( Section 20 (8 ) of the Infection Protection Act new).
Vaccination reactions and complications
| Symptom / illness |
Complication rate in measles disease |
Complication rate after MMR vaccination |
|---|---|---|
| Rash | 98% | 5%, attenuated |
| fever | 98%, mostly high | 3% to 5%, very rarely high |
| Febrile seizures | 7 to 8% | ≤ 1% |
| Drop in platelets | 1 / 3,000 | 1 / 30,000 to 1 / 50,000 |
| Encephalitis | 1 / 1,000 to 1 / 10,000 | 0 |
| Lethality | 1/500 to 3 / 1,000 | 0 |
As with all vaccinations, fever, fatigue, headache and local vaccination reactions such as redness, pain and swelling at the injection site can occur and are harmless side effects. More serious vaccination complications such as pronounced allergic reactions are very rare. However, when the vaccination is carried out, staff and equipment should be available to treat such anaphylaxis . The occurrence of inflammation of the brain (encephalitis) or thrombocytopenia (drop in blood platelet count ) is extremely rare, and the connection between the observed cases and vaccination is also controversial. The risk of febrile seizures is slightly increased after vaccination, but without long-term damage.
Since the measles vaccination is a vaccination with an attenuated live vaccine , so-called vaccination measles can occur in 3–5% of cases . These represent a mild form of measles and can show the typical symptoms, these usually occur in a weakened form. The vaccine fibers are not infectious.
Again and again, new side effects were brought up by the anti-vaccination scene . The assumptions that allergies , asthma , diabetes mellitus or Crohn's disease are triggered by vaccinations could not be confirmed. For example, former British surgeon Andrew Wakefield claimed a link between MMR vaccination and the occurrence of autism in 1998 . However, it turned out that Wakefield had falsified his investigations. Autism family members had paid Wakefield £ 3.5 million for it. Wakefield has now been banned from practicing the profession in Great Britain and its publications have been withdrawn (see also the Wakefield case ). In the meantime, the postulated connection has been contradicted as very unlikely in a large number of studies. In a study from Denmark published on March 5, 2019, the association between measles vaccination and autism was again refuted after evaluating 657,000 vaccinated children.
Vaccination against measles is considered necessary and safe; the studies examining the side effects of the MMR (V) vaccination are meanwhile sufficiently detailed and in some cases adequate with regard to the study design. At the end of 2013, the Paul Ehrlich Institute (PEI) evaluated all suspected cases reported between January 1, 2001 and December 31, 2012. No new risk signal could be detected, so the PEI remains with a positive risk-benefit assessment of the monovalent and combined measles vaccines.
Post exposure prophylaxis
In immune-compromised patients, the outbreak can possibly be prevented or weakened within three days by passive immunization with human immunoglobulin (mitigated course). In the case of healthy, unvaccinated or only once vaccinated contact persons without evidence of antibodies (seronegative), active immunization as described above is indicated within the same period of time. This so-called locking vaccination is intended to prevent further spread in the event of an epidemic.
Measles and Pregnancy
There is insufficient knowledge about the possible damage caused by measles infection during pregnancy . The disease may increase the rate of complications in the mother, a teratogenic influence of measles can neither be proven nor ruled out at the moment, but is considered to be very small if it does exist. There is no typical malformation pattern as with rubella . It can lead to premature delivery or spontaneous abortion come. Illness during childbirth does not necessarily have to cause infection in the newborn. However, such measles acquired perinatally (in the birth phase) is associated with increased complication rates in children.
Pregnant women with measles should be observed medically; invasive prenatal diagnostics are not recommended. Treatment is symptom-oriented. Under certain circumstances, administration of immunoglobulin may be indicated (see above).
The MMR vaccination is carried out with a live vaccine and is therefore not indicated ( contraindicated ) during pregnancy . Conception protection should take place three months after vaccination . However, accidental vaccination with MMR during pregnancy does not constitute a reason for termination of pregnancy .
history
The first reports of measles are said to date from the 7th century and were attributed to a Jewish doctor ("al-Yehudi") by the Persian doctor Rhazes (Abu Bakr Mohammad Ibn Zakariya al-Razi). The first known detailed description of measles was made in 910 by Rhazes, who referred to it as hasbah (Arabic for "outbreak"). He also stated that they were “more feared than smallpox ”. Even if he differentiated the two diseases, he (and others) assumed that they were closely related. He also assumed that the measles was not contagious.
Reports from antiquity cannot be found, so the measles is not passed down either in the texts of Hippocrates or in those of his successor Galen . Measles was not described in the Roman Empire either; Linguistic analyzes indicate that measles appeared in Europe in the early Middle Ages and was named accordingly. There they were first referred to as "Rubeola" or "Morbilli". Morbilli is the diminutive of Morbus (illness), the latter in those days meant the plague . The English term “measles” probably comes from “mesels”, the anglicized form of “misellus”, which in turn is the diminutive of “miser” (misery).
Despite these early reports, it was therefore also assumed that the measles virus did not evolve from the rinderpest virus until the 11th or 12th century .
By means of RNA sequencing of the lung preparation of a girl who died of measles in 1912 and a comparison with younger RNA samples, a molecular clock could be established, according to which the time of transition to humans was already in the 6th century BC. Could lie. The decisive factor for the transition to humans may have been the emergence of larger cities with sufficient population density in which the virus can circulate permanently.
In the Middle Ages , measles claimed many lives due to widespread epidemics. After the discovery of America , a large part of the native population died from diseases imported from Europe such as measles, smallpox , whooping cough and typhoid . The reason for this was that the native populations did not show any immunity to these pathogens. So there were devastating measles epidemics in Santo Domingo (1519), Guatemala (1523) and Mexico (1531). In 1529, a measles epidemic spread across Honduras and Central America, killing two thirds of the survivors of the smallpox epidemic that had previously broken out.
The phenomenon that the measles virus shows a high lethality when it hits a previously untouched, non-immune population, is found several times in the 19th century. So 40,000 of the 148,000 inhabitants of Hawaii died in 1848 and about a quarter of the population of the Fiji Islands died in 1874.
In the 17th century, it was thanks to Thomas Sydenham , during a major epidemic in London, to differentiate measles as an independent disease from scarlet fever and other febrile contagious exanthemic diseases, especially smallpox and rubella (German measles) , which had long been confused with measles . In 1882 the French doctor Antoine Louis Gustave Béclère published his sensational work The infection with measles . (The French name for measles is rougeole ). He and other French clinicians achieved that in the 19th century measles was finally differentiated as an independent disease unit from other diseases with rashes such as rubella. In the course of a measles epidemic on the Faroe Islands , an epidemiological and clinical clarification of the differences between scarlet fever and measles was carried out.
In 1911, Joseph Goldberger and John F. Anderson first succeeded in infecting monkeys with measles. In 1927 Rudolf Degkwitz developed the passive measles vaccination ( post-exposure prophylaxis ). In 1954 the virus was isolated and bred for the first time by Enders and Thomas C. Peebles . This led to the development of the first vaccine in 1958, which was generally available from 1963.
The measles and varicella working group was founded in 1999.
literature
- Measles . RKI Guide to Infectious Diseases - Leaflets for Doctors. Robert Koch Institute. updated May 2014.
- Measles. In: Epidemiology & Prevention of Vaccine-Preventable Diseases - “The Pink Book”. 9th edition. Public Health Foundation, pp. 129-148 (English) cdc.gov (PDF; 522 kB).
- M. Dietel, N. Suttorp, M. Zeitz, TR Harrison: Harrison's internal medicine . 16th edition. Abw Wissenschaftsverlag, 2005, ISBN 3-936072-29-9 .
- W. Moss, D. Griffin: Measles. In: The Lancet . 2011, doi: 10.1016 / S0140-6736 (10) 62352-5 .
- Andrea Misin et al .: Measles: An Overview of a Re-Emerging Disease in Children and Immunocompromised Patients . In: Microorganisms . tape 8 , no. 2 , February 18, 2020, doi : 10.3390 / microorganisms8020276 , PMID 32085446 , PMC 7074809 (free full text) - (English).
- Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 9-223, here: pp. 60-64.
Web links
- Measles - information from the Robert Koch Institute
- Further information from the WHO
- Alice Wittig: VacMap - Measles vaccination rates in Germany. Brockmann Lab - Institute for Biology - Humboldt Universität zu Berlin + RKI, 2017, accessed on March 6, 2020 .
Individual evidence
- ↑ PAHO / WHO Scientific and Technical Material. Measles Rubella Weekly Bulletin , (52) December 27, 2014
- ↑ a b c WHO: Global summary on measles , 2006.
- ^ Plan of Action for the Documentation and Verification of Measles, Rubella, and Congenital Rubella Syndrome Elimination in the Region of the Americas. Pan American Health Organization, 2011, accessed September 18, 2014 .
- ↑ Measles History , website of the Center for Disease Control and Prevention (CDC), provides an overview . Archive version ( Memento from January 11, 2005 in the Internet Archive )
- ^ William J Moss: Measles Still Has a Devastating Impact in Unvaccinated Populations. In: PLoS Medicine. 4, 2007, p. E24, doi: 10.1371 / journal.pmed.0040024 . PMID 17199409
- ↑ WHO-UNICEF joint statement on strategies to reduce measles mortality worldwide . In: Weekly epidemiological record. 27, 77, 2002, pp. 221–228, PMID 12125242 , who.int (PDF; 158 kB)
- ^ CP Muller, JR Kremer, JM Best, I. Dourado, H. Triki, S. Reef; WHO Steering Committee for Measles and Rubella: Reducing global disease burden of measles and rubella: report of the WHO Steering Committee on research related to measles and rubella vaccines and vaccination, 2005. In: Vaccine. 2007 Jan 2; 25 (1), pp. 1-9, PMID 17262908 .
- ↑ a b c d e Jorge Barinaga, Paul Skolnik: Epidemiology and transmission of measles. Review, UpToDate v15.1, 2007.
- ↑ Article. In: ÄrzteZeitung , April 24, 2012. WHO: Measles mortality still too high . In: Ärzteblatt , April 24, 2012.
- ↑ More deaths than Ebola: devastating measles epidemic rages in the Congo. In: t-online.de. January 9, 2020, accessed January 12, 2020 .
- ↑ a b Robert Koch Institute: Epidemiological Bulletin 05/2003 PDF, 98 KB
- ↑ Measles virus continues to spread in the European Region: WHO urges member states to step up their countermeasures , WHO press release of 25 October 2011.
- ↑ Wolfgang Geissel: WHO: Number of measles cases in Europe explodes. DoctorsZeitung, February 8, 2019, accessed January 12, 2020 .
- ↑ CA De Quadros, H. Izurieta, P. Carrasco, M. Brana, G. Tambini: Progress toward measles eradication in the region of the Americas. In: J Infect Dis . 2003 May 15; 187 Suppl 1, pp. S102-S110. PMID 12721900 .
- ↑ CA de Quadros: Can measles be eradicated globally? In: Bull World Health Organ. 2004 Feb; 82 (2), pp. 134-138. PMID 15042236 .
- ↑ WL Atkinson, WA Orenstein, S. Krugman: The resurgence of measles in the United States, 1989–1990. In: Annu Rev Med . 1992; 43, pp. 451-163, PMID 1580601
- ↑ Swiss Dispatch Agency, September 27, 2016
- ^ Measles Cases and Outbreaks. In: www.cdc.gov. July 3, 2019, accessed on July 11, 2019 .
- ↑ Elimination programs - epidemiological situation of measles and rubella in Germany in 2018. RKI, February 1, 2019, accessed on December 1, 2019 .
- ↑ Epidemiological Bulletin 3/2020. RKI, January 16, 2020, p. 17 , accessed on January 29, 2020 .
- ^ Measles: Situation report 2005, outbreaks in Baden-Württemberg and North Rhine-Westphalia in the first half of 2006. Epidemiological Bulletin 27/2006 of the RKI, July 7, 2006, rki.de (PDF; 140 kB)
- ^ Stefan Handel: Measles epidemic in Munich . In: Süddeutsche Zeitung . June 5, 2013, p. R1 (Munich edition) .
- ↑ Epidemiological Bulletin 33/2014 (PDF) of the Robert Koch Institute on the measles outbreak 2013 in a Waldorf school in the Rhein-Erft district
- ↑ SurvStat @ RKI 2.0. In: survstat.rki.de. Retrieved January 6, 2016 .
- ^ Measles: On the measles outbreaks in Berlin and in Bosnia and Herzegovina. Robert Koch Institute, February 2, 2015, accessed on February 26, 2015 (Link to Epid. Bulletin 5/2015).
- ↑ Current epidemiology and vaccination rates - Who gets measles in Germany? (PDF)
- ↑ Rafaela von Bredow, Lukas Eberle, Jan Friedmann, Michael Fröhlingsdorf, Annette Großbongardt, Veronika Hackenbroch, Julia Amalia Heyer, Dietmar Hipp, Julia Koch, Dirk Kurbjuweit , Cornelia Schmergal: Stich fürs Leben . In: Der Spiegel . No. 14 , 2019, pp. 12-19 ( online - March 30, 2019 ).
- ↑ Cosima Gill and Markus Pohl: How vaccination opponents and vaccine lazy people endanger the lives of children. rbb online , April 11, 2019, accessed on July 11, 2019 .
- ↑ Alina Schadwinkel, Sven Stockrahm: Measles: Put an end to the measles myths! In: The time . February 23, 2015, ISSN 0044-2070 ( zeit.de [accessed July 11, 2019]).
- ↑ Complications from measles are not uncommon. Deutsches Ärzteblatt , November 28, 2019, accessed on December 1, 2019 .
- ↑ Bundestag resolves compulsory measles vaccination - fines planned. Agency report. Die Welt , November 14, 2019, accessed on May 7, 2020 .
- ↑ a b Heidemarie Holzmann: Review of the measles outbreak in 2008 . ( Memento of April 2, 2015 in the Internet Archive ) (PDF) In: Virus epidemiological information , No. 14 / 09-3, of the Department of Virology at the Medical University of Vienna
- ^ Information from the Bavarian State Office for Health and Food Safety ; accessed on March 1, 2015.
- ^ Federal Office of Public Health, Department of Epidemiology and Infectious Diseases: Sentinella reports June 1986 – April 2003: Measles. Bulletin 23, June 2003, bag-anw.admin.ch ( Memento from November 16, 2011 in the Internet Archive ) (PDF; 50 kB)
- ↑ Federal Office of Public Health: Measles ( memento of July 7, 2016 in the Internet Archive ) Federal Office of Public Health: Measles ( memento of the original of June 10, 2017 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice.
- ^ Measles continues to advance ( memento of April 29, 2008 in the Internet Archive ). In: Tages-Anzeiger . March 25, 2008.
- ↑ Measles epidemic in Vaudois schoolhouse: 40 teenagers sick in: Berner Zeitung of February 11, 2009.
- ↑ a b Tages-Anzeiger - First measles death in Switzerland in years , accessed on March 28, 2017
- ↑ Press release from the school. ( Memento of March 4, 2012 in the Internet Archive ) (PDF; 78 kB) January 16, 2011.
- ↑ Figures on infectious diseases. (No longer available online.) Federal Office of Public Health, formerly the original ; accessed on June 8, 2017 . ( Page no longer available , search in web archives ) Info: The link was automatically marked as defective. Please check the link according to the instructions and then remove this notice.
- ↑ Two measles deaths in Switzerland. In: tagesanzeiger.ch . May 2, 2019, accessed May 2, 2019 .
- ↑ Karin Erni: Significantly more measles cases in Switzerland: Appenzell Innerrhoden recommends vaccination. In: tagblatt.ch . May 20, 2019, accessed May 20, 2019 .
- ↑ a b Berit Uhlmann: Finland: Europe's success story. Süddeutsche Zeitung , February 25, 2015, accessed on December 3, 2019 .
- ^ Finnish radio YLE
- ↑ Medical News Today: CDC Urges Travelers To Israel To Protect Themselves From Measles, April 15, 2008.
- ↑ Centers for Disease Control and Prevention (CDC): Measles Epidemic Attributed to Inadequate Vaccination Coverage - Campania, Italy, 2002 . In: MMWR Morb Mortal Wkly Rep. 2003 Oct 31; 52 (43), pp. 1044-1047. PMID 14586297
- ↑ a b Italy confronted with the measles epidemic. In: Wiener Zeitung . January 31, 2019, accessed March 3, 2020 .
- ↑ Measles: Italy introduces mandatory vaccination for children . In: The time . Hamburg May 19, 2017 ( zeit.de [accessed March 3, 2020]).
- ↑ a b Daniel Lingenhöhl: Vaccination: Why measles repeatedly afflict the Bible belt. Spektrum.de , January 25, 2019, accessed on February 29, 2020 .
- ↑ Centers for Disease Control and Prevention (CDC): Measles outbreak - Netherlands, April 1999 - January 2000. In: MMWR Morb Mortal Wkly Rep. 2000 Apr 14; 49 (14), pp. 299-303. PMID 10825086 - Measles . Rijksinstituut voor Volksgezondheid en Milieu
- ↑ a b c Bartosz Lisowski, Steven Yuvan, Martin Bier: Outbreaks of the measles in the Dutch Bible Belt and in other places - New prospects for a 1000 year old virus . In: Biosystems . tape 177 , March 1, 2019, p. 16–23 , doi : 10.1016 / j.biosystems.2019.01.003 .
- ↑ a b The Statesman: DRP Korea and Timor-Leste eliminate measles, six countries achieve rubella control , August 3, 2018 , accessed August 4, 2018.
- ↑ Inayat Ur Rehman, Allah Bukhsh, Tahir Mehmood Khan: Measles in Pakistan: Time to make steps towards eradication. Travel Medicine and Infectious Disease 18 (2017), pp. 67-69, doi: 10.1016 / j.tmaid.2017.08.002
- ↑ Octavian Coman Timisoara: Romania's Avoidable Epidemic. In: Neue Zürcher Zeitung . March 14, 2018, accessed March 3, 2020 .
- ↑ The island state of Samoa lifts the measles emergency. Bayerischer Rundfunk , December 29, 2019, accessed on January 7, 2020 .
- ↑ Measles Outbreak 2009 National Institute for Communicable Diseases, December 21, 2011. Communicable Diseases Surveillance Bulletin - Identifying high-risk areas for sporadic measles outbreaks: lessons from South Africa . WHO, doi: 10.2471 / BLT.12.110726 .
- ^ Josephin Mosch: Measles vaccination: vaccination success with side effects in Tanzania . Ed .: Bayerischer Rundfunk. October 15, 2017 ( br.de [accessed May 10, 2020]).
- ^ Robert T. Perry, Neal A. Halsey: The Clinical Significance of Measles: A Review , online May 1, 2004, accessed August 15, 2019
- ^ Sandra W. Roush et al .: Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States . In: JAMA . tape 298 , no. 18 , November 14, 2007, pp. 2155-2163 , doi : 10.1001 / jama.298.18.2155 , PMID 18000199 .
- ↑ Jan Hendriks and Stuart Blume: Measles Vaccination Before the Measles-Mumps-Rubella Vaccine . In: American Journal of Public Health . tape 103 , no. 8 , August 2013, p. 1393–1401 , doi : 10.2105 / AJPH.2012.301075 , PMID 23763422 , PMC 4007870 (free full text).
- ↑ Reported Cases and Deaths from Vaccine Preventable Diseases, United States (pdf), Centers for Disease Control and Prevention (CDC) , accessed July 30, 2018.
- ↑ American teenager caused measles outbreak in two communities with poor immunization , paediatricians online, August 20, 2018, accessed March 5, 2019.
- ↑ Measles declared eradicated in America . Süddeutsche Zeitung , September 27, 2016, accessed on August 25, 2020 . .
- ↑ Michael Remke: Vaccination opponents trigger measles outbreak among immigrants , Welt, May 11, 2017, accessed on March 5, 2019. According to the CDC website, 75 cases.
- ↑ a b Measles. Cases and outbreaks
- ↑ CDC: At Least 206 Measles Cases In US This Year , WLTZ 38 NBC, March 5, 2019, accessed March 5, 2019.
- ↑ a b ZEIT ONLINE: US health authority: USA registered highest number of measles cases for 20 years . In: The time . April 25, 2019, ISSN 0044-2070 ( zeit.de [accessed April 26, 2019]).
- ^ For parts of Brooklyn: New York declares a measles emergency . In: Spiegel Online . April 10, 2019 ( spiegel.de [accessed April 26, 2019]).
- ↑ a b Ariane Düx et al .: Measles virus and rinderpest virus divergence dated to the sixth century BCE. In: Science . Volume 368, No. 6497, 2020, pp. 1367-1370, doi: 10.1126 / science.aba9411 .
- ↑ a b c Brigitta M. Laksono et al .: Measles Virus Host Invasion and Pathogenesis . In: Viruses . tape 8 , no. 8 , July 28, 2016, doi : 10.3390 / v8080210 , PMID 27483301 , PMC 4997572 (free full text).
- ^ Y. Yanagi, M. Takeda, S. Ohno, F. Seki: Measles virus receptors and tropism. ( Memento of October 18, 2007 in the Internet Archive ) In: Jpn J Infect Dis. 2006 Feb; 59 (1), pp. 1-5. PMID 16495625
- ↑ Measles virus nomenclature update: 2012 . In: Releve Epidemiologique Hebdomadaire . tape 87 , no. 9 , March 2, 2012, p. 73-81 , PMID 22462199 .
- ^ WJ Bellini, PA Rota: Genetic diversity of wild-type measles viruses: implications for global measles elimination programs. In: Emerg Infect Dis . 1998 4 (1), pp. 29-35. PMID 9452396 .
- ^ Measles and Rubella Surveillance Data. WHO, March 13, 2020, accessed March 30, 2020 .
- ↑ Epidemiological Bulletin 37/2007. (PDF; 985 kB) Robert Koch Institute
- ↑ a b Köhler et al .: Medical Microbiology. Pp. 641-644.
- ↑ a b c d e f g h RKI - RKI-Ratgeber - Measles. Robert Koch Institute, May 19, 2014, accessed December 7, 2018 .
- ↑ JD Cherry: Textbook of pediatric infectious diseases. 5th edition. WB Saunders, Philadelphia 2004, pp. 2292-2293.
- ↑ K. Dittrich: Measles virus in adults ( Memento from May 9, 2015 in the Internet Archive ). 2010.
- ↑ a b Harrison's internal medicine (2005), pp. 1232-1235.
- ↑ a b c d e Jorge Barinaga, Paul Skolnik: Clinical presentation and diagnosis of measles. Review, UpToDate v15.1, 2007.
- ↑ a b Measles. In: Epidemiology & Prevention of Vaccine-Preventable Diseases - “The Pink Book”. 9th edition. Public Health Foundation, pp. 131–144, cdc.gov (PDF; 830 kB)
- ^ CDC website: Complications of Measles Disease
- ^ Measles factsheet ( Memento of March 21, 2012 in the Internet Archive ) on the website of the European Centers for Disease Prevention and Control , accessed on April 16, 2012.
- ^ AF Freeman et al .: A new complication of stem cell transplantation: measles inclusion body encephalitis . In: Pediatrics , 2004, 114 (5), pp. E657-60, PMID 15520095 . ISSN 0031-4005 pediatrics.aappublications.org (PDF; 157 kB)
- ↑ A. et al .: Bitnun Measles inclusion-body encephalitis Caused by the vaccine strain of measles virus. In: Clin Infect Dis . 1999 29 (4), pp. 855-861. PMID 10589903 . ISSN 1058-4838
- ↑ HT Chong et al .: Subacute measles encephalitis: A case of long term survival with follow-up MR brain scans. In: Neurology Asia. 2007; 12, pp. 121–125., Neurology-asia.org (PDF)
- ↑ a b Hasan Kweder et al .: Measles Virus: Identification in the M Protein Primary Sequence of a Potential Molecular Marker for Subacute Sclerosing Panencephalitis . In: Advances in Virology . tape 2015 , 2015, p. 769837 , doi : 10.1155 / 2015/769837 , PMID 26587021 , PMC 4637438 (free full text).
- ↑ H. Hotta, DP Jiang, M. Nagano-Fujii: SSPE virus and pathogenesis. In: Nippon Rinsho. 2007 Aug; 65 (8), pp. 1475-1480. PMID 17695286
- ↑ a b c Sidra K Jafri, Raman Kumar and Shahnaz H Ibrahim: Subacute sclerosing panencephalitis - current perspectives . In: Pediatric Health, Medicine and Therapeutics . tape 9 , June 26, 2018, p. 67-71 , doi : 10.2147 / PHMT.S126293 , PMID 29985487 , PMC 6027681 (free full text).
- ↑ DISCUSSION ABOUT MEASURE VACCINATION; 44: 85-7. arznei-telegram , October 11, 2013, accessed on January 2, 2020 .
- ↑ Robert Koch Institute-Berlin: Epidemiological Bulletin, Dec. 2013 (PDF)
- ↑ WJ Bellini et al .: Subacute sclerosing panencephalitis: more cases of this fatal disease are prevented by measles immunization than was previously recognized. In: J Infect Dis. 2005 192 (10), pp. 1686-1693. PMID 16235165
- ↑ a b c d e f g h Andrea Misin et al .: Measles: An Overview of a Re-Emerging Disease in Children and Immunocompromised Patients . In: Microorganisms . tape 8 , no. 2 , February 18, 2020, doi : 10.3390 / microorganisms8020276 , PMID 32085446 , PMC 7074809 (free full text).
- ^ A b J. I. Morrow et al .: Subacute sclerosing panencephalitis in Northern Ireland: twenty years' experience . In: The Ulster Medical Journal . tape 55 , no. 2 , October 1986, p. 124-130 , PMID 3811010 , PMC 2448355 (free full text).
- ↑ James R. Dawson: Cellular Inclusions in Cerebral Lesions of Lethargic Encephalitis . In: The American Journal of Pathology . tape 9 , no. 1 , January 1933, p. 7-16.3 , PMID 19970059 , PMC 2062741 (free full text).
- ↑ L. van Bogaert and J. De Busscher: Sur la sclérose inflammatoire de la substance blanche des hemisphéres (Spielmeyer). Ed .: Rev. neurol. tape 71 , no. 679 , 1939.
- ^ JH Connolly et al .: Measles virus antibody and antigen in subacute sclerosing panencephalitis . In: Lancet (London, England) . tape 1 , no. 7489 , March 11, 1967, p. 542-544 , doi : 10.1016 / s0140-6736 (67) 92117-4 , PMID 4163906 .
- ^ A b c d William J. Moss: Measles . In: The Lancet . tape 390 , no. 10111 , December 2, 2017, p. 2490-2502 , doi : 10.1016 / S0140-6736 (17) 31463-0 .
- ↑ Maya Wei-Haas: Measles vaccinations not only protect against measles. NatGeoDeutschland, March 5, 2019, accessed on August 27, 2019 .
- ↑ By Alina Schadwinkel: Infectious disease: the measles vaccination is an all-round protection package. May 7, 2015, accessed December 19, 2018 .
- ↑ Velislava N. Petrova et al .: Incomplete genetic reconstitution of B cell pools contributes to prolonged immunosuppression after measles . In: Science Immunology . tape 4 , no. 41 , November 1, 2019, doi : 10.1126 / sciimmunol.aay6125 , PMID 31672862 .
- ↑ Measles infection wipes our immune system's memory, leaving us vulnerable to other diseases. In: Sanger Institute, www.sanger.ac.uk. October 31, 2019, accessed November 1, 2019 .
- ↑ Annika Röcker: Immune system: measles as a memory killer. Spektrum.de , October 31, 2019, accessed on November 23, 2019 .
- ↑ a b Measles. WHO, December 5, 2019, accessed February 5, 2020 .
- ↑ a b c measles. RKI Guide to Infectious Diseases - Leaflets for Doctors. Robert Koch Institute. Status 09/2010.
- ↑ MJ Ferson, LC Young, PW Robertson, LR Whybin: Difficulties in clinical diagnosis of measles: proposal for modified clinical case definition. In: Med J Aust. 1995 Oct 2; 163 (7): 364-6. PMID 7565261
- ^ SA Oliveira et al .: Assessment of the performance of a definition of a suspected measles case: implications for measles surveillance. In: Rev Panam Salud Publica. 2006 Apr; 19 (4), pp. 229-235. PMID 16723063
- ^ WJ Bellini, RF Helfand: The challenges and strategies for laboratory diagnosis of measles in an international setting. In: J Infect Dis. 2003; 187 Suppl 1, p. S283 PMID 12721927 .
- ↑ Sean Kostolansky; James R. Waymack: "Erythema Infectiosum (Fifth Disease)", Section: "Differential Diagnosis"
- ↑ a b Cornelia Henke-Gendo: Paramyxoviruses . In: Sebastian Suerbaum, Gerd-Dieter Burchard, Stefan HE Kaufmann, Thomas F. Schulz (eds.): Medical microbiology and infectious diseases . Springer-Verlag, 2016, ISBN 978-3-662-48678-8 , pp. 492 , doi : 10.1007 / 978-3-662-48678-8_60 .
- ↑ Aamer Imdad et al .: Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age . In: The Cochrane Database of Systematic Reviews . tape 3 , March 11, 2017, p. CD008524 , doi : 10.1002 / 14651858.CD008524.pub3 , PMID 28282701 .
- ↑ a b c d e David Bekhor, Jorge Barinaga, Paul Skolnik: Prevention and treatment of measles. Review, UpToDate v15.1, 2007.
- ↑ Rene F. Najera: Vitamin A and Measles. In: History of Vaccines. March 12, 2019, accessed February 5, 2020 .
- ↑ AL Forni et al .: Severe measles pneumonitis in adults: evaluation of clinical characteristics and therapy with intravenous ribavirin . In: Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America . tape 19 , no. 3 , September 1994, pp. 454-462 , doi : 10.1093 / clinids / 19.3.454 , PMID 7811865 .
- ↑ Ebru Ortac Ersoy et al .: Severe measles pneumonia in adults with respiratory failure: role of ribavirin and high-dose vitamin A . In: The Clinical Respiratory Journal . tape 10 , no. 5 , September 2016, p. 673-675 , doi : 10.1111 / crj.12269 , PMID 25619709 .
- ^ L. Dillner: The return of the measles party. In: Guardian. July 26, 2001, accessed August 13, 2007 .
- ↑ Nicole Saddle Enzler, Brigitte Strasser-Vogel: 300 questions for vaccination. Graefe and Unzer Verlag, Munich 2008, ISBN 978-3-8338-1145-6 , p. 149.
- ↑ Overview of infectious diseases and required measures as a basis for stipulations in the hygiene plan. KRINKO 2016 (PDF); accessed on March 7, 2019
- ↑ Vaccination against measles: Frequently asked questions and answers . Robert Koch Institute ; accessed on March 10, 2015.
- ↑ Markus Frühwein and Brigitte Dietz: Measles - Safe protection against an underestimated danger. (PDF) Bayerisches Ärzteblatt, April 2016, accessed on May 16, 2019 .
- ↑ Christina Hucklenbroich: How do I explain it to my child ?: Why there is a dispute about the measles vaccination . Ed .: FAZ. February 27, 2015, ISSN 0174-4909 ( faz.net [accessed May 2, 2019]).
- ↑ Amra Uzicanin and Laura Zimmerman: Field effectiveness of live attenuated measles-containing vaccines: a review of published literature . In: The Journal of Infectious Diseases . 204 Suppl 1, July 2011, p. S133-148 , doi : 10.1093 / infdis / jir102 , PMID 21666154 .
- ↑ O. Wichmann and B. Ultsch: Effectiveness, population effects and health economics of vaccinations against measles and rubella . In: Federal Health Gazette - Health Research - Health Protection . tape 56 , no. 9 , September 1, 2013, ISSN 1437-1588 , p. 1260-1269 , doi : 10.1007 / s00103-013-1801-7 .
- ↑ a b Vaccination recommendations of the Standing Vaccination Commission (STIKO), Robert Koch Institute, Berlin 2006, rki.de (PDF; 164 kB)
- ↑ Epidemiological Bulletin No. 16/2014 (PDF) RKI , April 22, 2014.
- ↑ Vaccination plan Austria 2017
- ↑ Short report: Evaluation of measles vaccination rates, version 1. (PDF) Federal Ministry for Health and Women, September 9, 2016, accessed on April 5, 1017 .
- ↑ a b WHO: Reported estimates of MCV coverage .
- ^ Prevention of measles, mumps, and rubella . Recommendations of the Federal Office of Public Health (FOPH) and the Swiss Commission for Vaccination Issues (SKIF), PDF, 232 kB (PDF)
- ↑ C Storr, L Sanftenberg, J Schelling, U Heininger, A Schneider: Measles status — barriers to vaccination and strategies for overcoming them. In: Deutsches Ärzteblatt International , 2018, Volume 115, pp. 723–730. doi: 10.3238 / arztebl.2018.0723
- ^ Region of the Americas is declared free of measles . Panamerican Health Organization; accessed on December 8, 2018
- ↑ WHO: Measles no longer endemic in 79% of the WHO European Region. euro.who.int accessed on December 8, 2018
- ↑ a b c d Carlo Di Pietrantonj et al .: Vaccines for measles, mumps, rubella, and varicella in children . In: The Cochrane Database of Systematic Reviews . tape 4 , April 20, 2020, p. CD004407 , doi : 10.1002 / 14651858.CD004407.pub4 , PMID 32309885 , PMC 7169657 (free full text).
- ↑ Compulsory vaccination should protect children from measles , Federal Ministry of Health, May 5, 2019. Accessed June 11, 2019.
- ^ Draft of a law for the protection against measles and to strengthen vaccination prevention (measles protection law) (PDF) draft bill of the Federal Ministry of Health. Retrieved June 11, 2019.
- ↑ Compulsory measles vaccination: Doctors criticize Spahn , Merkur, May 8, 2019. Retrieved June 11, 2019.
- ↑ https://www.aerzteblatt.de/nachrichten/107417/Bundestag-beschliesst-Masenschutzgesetz
- ↑ https://www.bundesgesundheitsministerium.de/impfpflicht.html
- ↑ Measles Protection Act: Federal cabinet decides on mandatory measles vaccination zeit.de, July 17, 2019, accessed December 2, 2019.
- ↑ Federal Law Gazette . (PDF) Retrieved March 1, 2020 .
- ^ C. Meyer, S. Reiter: Vaccination opponents and vaccination skeptics - history, background, theses, handling . In: Bundesgesundheitsbl - Health Research - Health Protection . tape 47 , 2004, p. 1182-1188 , doi : 10.1007 / s00103-004-0953-x .
- ^ RT Chen: Vaccine risks: real perceived and unknown. In: Vaccine. 17/1999, pp. 41-46, PMID 10559533
- ↑ M. Vestergaard et al .: MMR vaccination and febrile seizures: evaluation of susceptible subgroups and long-term prognosis. In: JAMA. 2004 Jul 21; 292 (3), pp. 351-357. 15265850 PMID 15265850
- ↑ MMR row doctor Andrew Wakefield struck off register The Guardian , May 24, 2010. Retrieved May 24, 2013.
- ↑ KM Madsen, A. Hviid, M. Vestergaard, D. Schendel, J. Wohlfahrt, P. Thorsen, J. Olsen, M. Melbye: A population-based study of measles, mumps, and rubella vaccination and autism. In: N Engl J Med . 2002 Nov 7; 347 (19), pp. 1477-1482. PMID 12421889 .
- ^ T. Jefferson: Unintended events following immunization with MMR: a systematic review. In: Vaccine. 2003 Sep 8; 21 (25-26), pp. 3954-3960 PMID 12922131 .
- ↑ MMR vaccination is not associated with autism. In: aerztezeitung.de. March 5, 2019, accessed March 8, 2019 .
- ^ H. Meyer et al .: Safety of measles vaccines . In: Bulletin on drug safety 2013. (PDF) Edition 3/2013, pp. 12-14.
- ↑ Online information from the Robert Koch Institute
- ^ Francis L. Black: Measles. In: Alfred S. Evans (Ed.): Viral Infections of Humans. Epidemiology and Control. Plenum Publishing Corporation, New York 1982; 2nd, revised and expanded edition. Plenum Medical Book Company, New York / London, ISBN 978-1-4613-3239-8 , pp. 397-418, here: pp. 397 f.
- ↑ a b c Peter M. Strebel et al .: Measles vaccine . In: Vaccines . 6th edition. WB Saunders, London 2013, ISBN 978-1-4557-0090-5 , pp. 352-387 ( sciencedirect.com [accessed July 29, 2020]).
- ↑ Measles virus older than assumed. Deutsches Ärzteblatt , January 3, 2020, accessed on January 10, 2020 .
- ↑ Yuki Furuse et al .: Origin of measles virus: divergence from rinderpest virus between the 11th and 12th centuries . In: Virology Journal . tape 7 , no. 52 , March 4, 2010, doi : 10.1186 / 1743-422X-7-52 , PMID 20202190 , PMC 2838858 (free full text).
- ^ PJ Bianchine, TA Russo: The role of epidemic infectious diseases in the discovery of America. In: Allergy Proc. Volume 13, No. 5, September / October 1992, pp. 225-232. PMID 1483570
- ^ Roy Porter: The Art of Healing: A Medical History of Mankind . Spectrum, Heidelberg / Berlin 2003, ISBN 3-8274-1454-7 , p. 166.
- ↑ ibid. P. 24.
- ↑ Manfred Vasold: Measles. In: Werner E. Gerabek u. a. (Ed.): Encyclopedia of medical history. 2005, p. 894.
- ↑ J.-Ch. Sournia, J. Poulet, M. Martiny (Ed.): Illustrated history of medicine. Directmedia, Berlin 2004.
- ↑ Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition, ibid. 1961, pp. 9–223, here: p. 60.
- ^ John F. Anderson, MD The NIH Almanac.
- ↑ John F. Anderson and Joseph Goldberger: Experimental measles in the monkey: a supplemental note. 1911 . In: Samuel L. Katz (Ed.): Public Health Reports (Washington, DC: 1974) . 121 Suppl 1, 2006, p. 51-57; discussion 50 , doi : 10.1177 / 00333549061210S107 , PMID 16550765 .
- ↑ a b Werner Köhler : Infectious diseases. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , pp. 667-671; here: p. 671.
- ↑ Albert Herrlich: Handbook of protective vaccinations . Springer, Berlin / Heidelberg 2013, ISBN 978-3-642-92897-0 , pp. 525– ( limited preview in Google Book search).
- ↑ JF Enders and TC Peebles: Propagation in tissue cultures of cytopathogenic agents from patients with measles . In: Proceedings of the Society for Experimental Biology and Medicine. Society for Experimental Biology and Medicine (New York, NY) . tape 86 , no. 2 , June 1954, p. 277-286 , doi : 10.3181 / 00379727-86-21073 , PMID 13177653 .