tuberculosis
| Classification according to ICD-10 | |
|---|---|
| A15 | Tuberculosis of the respiratory system, bacteriologically or histologically confirmed |
| A16 | Tuberculosis of the respiratory organs, neither bacteriologically nor histologically confirmed |
| A17 | Tuberculosis of the nervous system |
| A18 | Tuberculosis of other organs |
| A19 | Miliary tuberculosis |
| ICD-10 online (WHO version 2019) | |
The Tuberculosis (abbreviated TB or TB , so named from the Würzburg clinicians Johann Lukas Schönlein because of the characteristic histopathological image of Latin Tuberculosis , from Latin tubercle , small tumor ') is a cosmopolitan bacterial infectious disease . The disease is caused by various types of mycobacteria ( Mycobacterium tuberculosis complex ) and, in humans, most commonly affects the lungs as pulmonary tuberculosis ; if there is an immunodeficiency , an infection outside the lungs is also more common.
Tuberculosis, which affects around 10 million people worldwide every year, leads the global statistics on fatal infectious diseases. According to the World Health Organization (WHO) Global tuberculosis report , around 1.4 million people died of tuberculosis in 2015. In addition, there were 400,000 deaths from additional HIV- infected people. Tuberculosis is most commonly caused (at least now in Germany) by Mycobacterium tuberculosis , less often - in descending order - by Mycobacterium bovis , Mycobacterium africanum or Mycobacterium microti .
The description of the pathogen Mycobacterium tuberculosis by Robert Koch 1882 was a milestone in medical history. Tuberculosis is therefore also called Koch's disease . The names tuberculosis ( phthisis or phthisis ) or colloquially the moths , white plague and White death are out of date, as well as the terms Lungendärre , Darre and Dörre .
Only around five to ten percent of those infected with Mycobacterium tuberculosis actually become ill in the course of their life; people with a weakened immune system or genetic susceptibility are particularly affected . The transmission usually takes place through droplet infection of sick people in the vicinity. If germs are detectable in the sputum , one speaks of open tuberculosis, if germs are detected in other external body secretions, it is referred to as potentially open tuberculosis. Coughing creates an infectious aerosol that loses its infectivity through sedimentation, ventilation and natural UV light sources. Since cattle can also develop tuberculosis, ( unpasteurized ) raw milk used to be a common source of infection in Western Europe and is still a common source of infection in parts of the world. Because it can be transmitted from animals to humans, tuberculosis is a zoonosis . Conversely, the transmission from humans to animals is an important aspect of the conservation of rare primates.
Only with the direct detection of the pathogen or its genetic material is the disease confirmed by laboratory diagnostics. Indirect, d. H. Immunological findings or skin tests only contribute to the diagnosis, as they cannot distinguish between a disease and a previous infection. They can also turn out to be false-negative if the immune system has collapsed.
Various antibiotics are available for treatment , which are especially effective against mycobacteria and are therefore also called antituberculotics . In order to avoid the development of resistance and relapses, these must be taken in combination and in accordance with the guidelines of the WHO for at least six months, i.e. well beyond the persistence of the symptoms. There is a vaccination, but it has not been recommended in Germany since 1998 due to insufficient effectiveness and is no longer available. A primary prophylaxis with a antituberkulös effective drug is recommended in Germany primarily in children or severely immunocompromised contacts. In adults who have an intact immune system (and are therefore referred to as immunocompetent ), on the other hand, secondary prophylaxis or prevention only takes place after an infection has been determined by means of preventive administration of anti-tuberculous drugs, taking into account the resistance situation. Tuberculosis is subject to registration by name in the European Union and most of the world .
Epidemiology and relevance to health policy
Worldwide
About a third of the world's population is infected with tuberculosis pathogens. However, only a small proportion of the infections lead to disease. According to the WHO Global tuberculosis report 2016 , there were 10.4 million new infections and 1.8 million deaths worldwide in 2015. Both numbers have been falling steadily since 1990.
Treatment options are often inadequate because it requires expensive antibiotics, takes a long time and is often impracticable given the social circumstances of those affected. Laboratories for diagnosis and treatment are often lacking in affected regions. In Eastern Europe in particular, there has been a worrying increase in tuberculosis due to poverty and deficiencies in the health system , especially with multi-resistant strains of pathogens. The disease is also caused by such drug-resistant tuberculosis strains around the world.
A tuberculosis infection is particularly problematic in HIV- infected people with manifest AIDS . Due to the immune deficiency , HIV increases the likelihood of an outbreak of tuberculosis many times over. Along with AIDS, tuberculosis is the leading cause of death in Africa. Both diseases occur in close correlation with one another, particularly in residents of metropolitan slums. The immunodeficiency caused by HIV often leads to negative results in routine tuberculosis examinations, even though the disease is present (see also errors 1 and 2 ). This is because the skin tests ( tuberculin test , tine test) check the immunological reaction to pathogen components, but this is inhibited by AIDS. The course of tuberculosis is then considerably accelerated. In poor countries, TB is a sign of the AIDS outbreak and kills the majority of people with HIV. The WHO therefore calls for and promotes global coordination of tuberculosis and AIDS research.
Surprisingly, an Italian study found a prevalence (frequency of disease) of latent tuberculosis infections of nine percent among healthy employees in the healthcare sector and 18 percent among a good 400 people with psoriasis . 30 percent of those with pneumonia and lung cancer were also latently infected.
Germany, Austria and Switzerland
In 2016, 5915 tuberculosis sufferers were reported to the Robert Koch Institute (RKI) in Germany, including 233 children under the age of 15 (2005: 230). In 2016 there were 7.2 diseases per 100,000 inhabitants in Germany. The official statistics indicated 100 fatalities for 2015. The data should not quite correspond to the real figures, as the number of unreported cases for this disease is relatively high due to its unspecific symptoms. According to a pathology study from Germany, the diagnosis of only one third of postmortem diagnosed tuberculosis was made during lifetime.
In Germany, the disease is particularly widespread in Hamburg , Bremen and Berlin . In the case of sick people born in the country, the older cohorts predominate due to the tendency to activate and reactivate as a result of the decreasing immune defense. The middle age groups predominate among the migrants, as fresh infections are more likely to trigger the disease. The preliminary tuberculosis statistics for 2017 show a plateau in Germany at the level of 2016 after an increase in tuberculosis diseases due to increased immigration was recorded in autumn 2015. In Switzerland and Austria , the number of cases also decreased slightly up to 2017. A feared greater increase in the number of cases due to the migration wave of 2017 has therefore not yet occurred.
In Austria in 2015 583 were disease detected with tuberculosis, Switzerland during the same year 546 diseases.
The following table shows the number of new cases per 100,000 population ( incidence ) and the number of new cases per year in Germany (D), Switzerland (CH) and Austria (A).
| year | Incidence D |
Reported cases (new cases) D | Incidence CH |
Reported cases (new cases) CH | Incidence A |
Reported cases (new cases) A | Incidence GDR |
|---|---|---|---|---|---|---|---|
| 1940 | 156.8 | 109.508 (Reich territory) | about 100 | 3.127 | only figures for the Reich territory | ||
| 1950 | 277 | 137,721 (only Germany) | 68.1 | approx. 8200 | about 500 | ||
| 1960 | 126.6 | 70,325 (only Germany) | about 40 | approx. 4600 | approx. 210 | ||
| 1970 | 79.3 | 48,262 (only Germany) | approx. 25 | 2,850 * | about 80 | ||
| 1980 | 42.1 | 27,845 (only Germany) | approx. 20 | 1,396 | 2,191 * | ||
| 1990 | 19.6 | 12,184 (only Germany) | 18.4 | 1,278 | 20.4 | 1,521 * | |
| 2000 | 11.0 | 9,064 | 8.7 | 629 | 15.3 | 1,226 | |
| 2006 | 6.5 | 5,402 | 6.9 | 520 | 10.8 | 894 | |
| 2007 | 6.1 | 5,020 | 6.3 | 478 | 10.7 | 891 | |
| 2008 | 5.5 | 4,543 | 6.7 | 520 | 9.9 | 817 | |
| 2009 | 5.4 | 4,444 | 7.1 | 556 | 8.4 | 697 | |
| 2010 | 5.4 | 4,388 | 6.9 | 548 | 8.2 | 688 | |
| 2011 | 5.3 | 4,317 | 7.1 | 577 | 8.2 | 687 | |
| 2012 | 5.2 | 4,220 | 5.7 | 463 | 7.7 | 648 | |
| 2013 | 5.3 | 4,318 | 6.5 | 526 | 7.7 | 649 | |
| 2014 | 5.6 | 4,488 | 5.7 | 473 | 6.8 | 582 | |
| 2015 | 7.3 | 5,865 | 6.4 | 546 | 6.7 | 583 | |
| 2016 | 7.2 | 5,915 | 7.2 | 611 | 7.2 | 634 | |
| 2017 | 6.7 ** | 5,476 ** | 6.3 ** | 536 ** | 6.5 ** | 569 ** | |
| 2018 | 6.5 | 5,513 | |||||
| 2019 | 4,735 |
* contagious only ** provisional figures
Tuberculosis pathogen
The main causative agent of tuberculosis, Mycobacterium tuberculosis, is an aerobic gram-positive rod-shaped bacterium that divides every 16 to 20 hours. Compared to other bacteria that have division rates on the order of minutes, this is extremely slow. The microscopic detection is made possible by the typical coloring properties: The bacterium retains its color after treatment with an acidic solution and is therefore referred to as an acid-resistant rod. In the most common coloring of this type, the Ziehl-Neelsen coloring , the red colored germs stand out against a blue background. The detection is still possible by fluorescence microscopy and by the auramine-rhodamine staining . Mycobacteria are hardly visible in the Gram stain, but the structure of the peptidoglycan is very similar to that of gram-positive bacteria, so that M. tuberculosis is formally classified as gram-positive. This was confirmed by sequence analyzes of the RNA .
Other mycobacteria , which are also counted among the causative agents of tuberculosis, belong to the same group of bacteria : M. bovis , M. africanum and M. microti . These pathogens are only found sporadically in tuberculous diseases in Germany. M. kansasii and also M. avium can in rare cases, like a number of other mycobacteria, cause tuberculosis-like clinical pictures. However, atypical mycobacteria ( mycobacteria other than tuberculosis, MOTT ) do not usually pose a risk of infection .
M. tuberculosis, M. bovis, M. africanum, M. microti, M. canetti , M. pinnipedi , M. caprae and the vaccine strain Bacillus Calmette-Guérin (BCG) are summarized as Mycobacterium tuberculosis complex.
Transmission routes
Inhalation of infectious droplets ( aerosols ) is the most common and therefore most important transmission route: In this case, the inhalation of a few microdroplets (2–5 µm in diameter), each containing 1–3 pathogens, is sufficient for an infection . Transmission via the bloodstream, organ transplants or other body secretions is far less common. In principle, any of the following transmission routes are possible and described as secure in the literature:
- aerogenic , i.e. via microdroplets in the air that contain the pathogen Mycobacterium tuberculosis , with the entry ports alveoli , open wounds, fresh tattoos and mucous membranes
- gastral by the ingestion mykobakterienhaltiger foods (milk, raw meat etc.)
- parenterally using diagnostic and therapeutic instruments contaminated with blood and secretions (transfusions, syringes, needles, scalpels, lancets, biopsy needles, endoscopes, etc.)
- Transplant-related through heterogeneous grafts of infected tissue (kidneys, etc.)
- sexual (only if genital organs are affected)
- through smear infections on the non-intact skin (fissures, eczema or injuries)
- intrauterine for infections of the uterus
- sub partu (during childbirth) as a result of urogenital tuberculosis in the mother
The infestation of cockroaches and their faeces with Mycobacterium tuberculosis has been repeatedly proven . This fact is regularly cited by pest controllers. A review of the literature did not reveal a single confirmed transmission case.
Excretory tuberculosis is a medical term that is no longer in use for those forms of tuberculosis in which the pathogens are spread through the excretory organs in the body and lead to a secondary infestation of other organs.
The airborne infections usually originate in adults, since the amount of bacteria excreted in children is too small, even with open pulmonary tuberculosis (paucibacillary = low-pathogen tuberculosis). Organ involvement outside the lungs, with the exception of highly contagious laryngeal tuberculosis (laryngeal tuberculosis), only poses a risk of infection if the foci of infection are connected to the outside of the body by natural routes (gastrointestinal tract) or fistula formation, or if there are needle stick injuries or contact during diagnostic punctures / interventions comes to wounds. A historically significant, now almost forgotten special form are the corpse tubercles (English prosectors wart), whereby anatomists, pathologists, butchers, etc. become infected again through hand wounds. Infection from infected milk is also possible. However, such infections have become very rare in industrialized countries, where cattle herds are largely tuberculosis-free and the milk is pasteurized. Newborns from mothers with pulmonary tuberculosis rarely get infected through the bloodstream. However, if the tuberculosis infection has seized the placenta , the child can become infected by swallowing bacterial amniotic fluid. If the mother's urinary tract and the associated sexual organs are affected, the newborn can become infected at birth.
Immunology and pathology
After infection, the pathogens are in most cases already repelled in the airways. Of all those infected, only about a tenth actually develop tuberculosis. Whether an organism can defend itself sufficiently against the mycobacteria depends on many factors. The nutritional status, a genetic disposition (there are about 20 known gene polymorphisms that increase the risk of disease up to a factor of 5) as well as a drug, infection-related or toxic suppression of the immune system , but also the amount of bacteria ingested and the frequency of contact are important. The size and ventilation of a room and the lack of UV light sources can also play a role as factors. The literature describes outbreaks among cannabis smokers who have smoked the drug together in a car or in a narrow room without external ventilation (so-called hotboxing ), as well as among drug users who have used the same injection cannula without cleaning (so-called needle sharing ).
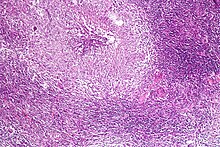
Specialized phagocytes ( alveolar macrophages ) in the pulmonary alveoli represent a first defense bulwark . These can absorb the pathogens into their cell interior ( phagocytize ), but then cannot kill them. Even other phagocytes that have been called are not able to do this. The process of phagocytosis is activated by various substances on the surface of pathogens. These can be components of the cell wall, but also host molecules that have bound to the intruder's cell wall. Mycobacteria prevent the cell components of the phagosomes in which they are located, the so-called phagosomes, from further maturing. This ensures the survival of Mycobacterium tuberculosis. The immune system therefore forms a wall of several rings of different defense cells around the initial focus of infection. This defense wall of scavenger cells (macrophages), so-called epithelial cells, Langhans giant cells and lymphocytes is formed around a central focus of inflammation with tissue destruction ( necrosis ). This particular form of necrosis, which is also pathognomonic for TBC, is called caseating necrosis . The entire structure is called a tuberculous granuloma (or tuberculoma ). It isolates Mycobacterium tuberculosis at the point of entry and prevents it from spreading. This requires a functioning interaction of the various immune cells, which call and activate each other via various messenger substances ( cytokines ). In particular, the release of tumor necrosis factor causes nitrosative stress in the phagosome, which together with the encapsulation forces the bacterium to go into a dormant state.
The mycobacteria in turn react to the encapsulation with a change in their state of activity. Since the genome of the most important mycobacterial strains was deciphered in 1998, various mechanisms for this have been discovered. They are able to temporarily stop their metabolism in the granuloma or to adjust it in such a way that they metabolize the fats occurring here and thus require particularly little oxygen. You are now in the stage of dormancy , d. that is, they share even less often. This dormant primary infection can develop into (post-primary) active tuberculosis through a renewed transition to an active state. However, since it has been proven that this can also result from an (exogenous) reinfection (exogenous relocation), it must be assumed that a previous infection does not provide sufficient protection against the onset of the disease in the event of renewed contact. This makes it clear why it is so difficult to develop an effective vaccine against tuberculosis.
Symptoms
Basically, the course of the disease in tuberculosis is divided into different stages. Symptoms that manifest themselves immediately after infection are called primary tuberculosis . However, since the bacteria dormant in the body for life even with an intact immune defense without signs of disease or after primary tuberculosis has passed and can be reactivated at any time, one speaks of a latent tuberculosis infection (LTBI) in the case of an initial infection that does not lead to the disease or, after an initial illness, of post-primary tuberculosis or secondary tuberculosis. Since the infection usually takes place in the lungs, but in principle also in any other organ, pulmonary tuberculosis is also differentiated from organ tuberculosis .
Primary tuberculosis, closed tuberculosis, early form
After infection via infected droplets, small inflammations with involvement of the associated lymph node (primary complex) form in the lungs of the person concerned in the following three to six weeks as a reaction to the bacteria . The foci of inflammation (early infiltrates) are enclosed by blood defense cells. Small nodules (tubercles) form. Encapsulated in this way, the tuberculosis foci do not cause any complaints and usually have no connection to the airways (the bronchial system ). With this primary tuberculosis (formerly also primary herbal phthisis or first herbal tuberculosis ) one speaks of a closed tuberculosis, which by definition is not contagious, since no pathogens are excreted. The mycobacteria can survive in the body for years.
If the infected individual is not able to encapsulate the pathogen in this way, an active infection with mostly uncharacteristic symptoms (B symptoms) can occur because the pathogen continues to spread. These can include tiredness and weakness, loss of appetite and weight loss, swollen lymph nodes , a low level fever , especially in the afternoon, night sweats and constant coughing without much sputum. Hoarseness can indicate a larynx involvement with an increased risk of infection. In severely ill people, these symptoms can be weak and sometimes absent despite the risk of infection. The formation of exudate as part of an infection of the pleura can also lead to a pleural effusion in tuberculosis (the pH value of the pleural fluid then shows acidosis ). Severe courses with bloody sputum ( haemoptysis ), severe anemia and underweight are not rare in Central Europe either. The number of deaths from tuberculosis has flattened far less than the total number of cases in the last few decades. Since the 1980s, there has been a decline in the lighter closed forms in particular.
If mycobacteria are sown in a weakened person via the bloodstream with involvement of both halves of the lungs and many organs at the same time, one speaks of miliary tuberculosis . It is named after the miliary ( millet-like , from Latin milium "millet, millet grain ") sowing ( metastasis ) shown in the X-ray image and presents itself as a serious clinical picture with considerable impairment of the general condition, fever, loss of appetite, weight loss, cough and shortness of breath. Also Meningitis (tubercular meningitis ) can develop in this way. This first shows up in uncharacteristic symptoms such as irritability and change in personality. Later, meningitic signs with headache, neck stiffness, hallucinations, impaired consciousness, seizures and fever, i.e. a severe impairment of the general condition, can occur. If left untreated, it leads to coma and death. It can also tubercle of the choroid occur (Chorioidaltuberkel). Extremely weak immune systems can lead to fulminant sepsis , usually fatal, which is often referred to as Landouzy sepsis .
Post-primary tuberculosis, secondary tuberculosis
In at least ten percent of people who have contracted tuberculosis, the disease breaks out later as secondary tuberculosis . The patients then often complain of various symptoms: coughing persistent for weeks with coughing up yellowish-green phlegm, exhaustion, fatigue, subfebrile temperatures in the evening and night sweats. Chest pain and shortness of breath may occur when coughing. Bloody sputum can be an expression of erosion of the bronchi or the mucous membrane of the trachea (bronchial tuberculosis, tracheal mucous membrane tuberculosis), often an open, contagious disease is already present. Bloody sputum should therefore be clarified immediately by a doctor.
The tuberculosis bacteria multiply in the lungs and destroy the tissue. If smaller or medium-sized branches of the bronchial tree are eroded, the destroyed tissue is connected to the airways and is then coughed up. The sputum now contains bacteria - the patient has overt tuberculosis. In the advanced stage, further organs can be attacked by sowing the bacteria via the bloodstream (haematogenic spread) . Then, for example, painful swellings appear on the knees and other joints ( Poncet's disease or Poncet's disease , named after the surgeon Antonin Poncet, who described tuberculous rheumatoid or rheumatism tuberculosus in 1897) or the spine ( joint tuberculosis, bone tuberculosis ). A special form of tuberculosis is skin tuberculosis (lupus vulgaris) , which in Central Europe used to be seen as a result of drinking raw milk and the associated infection with Mycobacterium bovis , but has now become very rare . Non-healing small wounds, cracks, wart-like foci of pus and circumscribed ulcers include. typical symptoms of skin tuberculosis.
Organ tuberculosis, extrapulmonary tuberculosis
In addition to involvement of the lungs, which is by far the most frequently affected organ at around 80%, tuberculosis can also manifest itself in numerous other organs. This organ tuberculosis (formerly also called organ phthisis ) can arise either as a result of primary infection at entry points other than the respiratory tract or as a result of spreading via the bloodstream as part of primary tuberculosis of the lungs. This in turn affects the lymph nodes ( lymph node tuberculosis ) most frequently.
- Skin tuberculosis ( Skrophuloderm , see Skrophulosis ) can develop if there is a tendency to melt down in the cheesy tissue deposits ( necroses ) that are typical for tuberculosis.
- Tuberculosis of muscles and tendon sheaths can also occur.
- The lower thoracic and lumbar spine is often affected and the inflammation leads to softening and deformation with gibbus formation (so-called Pott's disease ). In the past, the differential diagnosis of rickets was often difficult to make. This form of manifestation can lead to the formation of an abscess in the area of the psoas muscle . The localization near the spinal cord and the nerve tracts exiting there often manifests itself clinically in the form of neurological deficits or neuropathic pain that often radiates into the legs and buttocks.
- Tuberculosis of the brain or meninges (tuberculous meningitis, tuberculous meningitis) can be visualized with today's imaging methods. It can be secured microbiologically by a lumbar puncture. It mostly affects the basal (lower) sections of the brain and clinically often leads to damage to the cranial nerves exiting there .
- Involvement of the kidneys , adrenal glands , the urinary tract and the genital tract is called renal tuberculosis, genital tuberculosis or urogenital tuberculosis and usually occurs through the bloodstream.
- Bone tuberculosis (with damaged bones, also known as bone caries ) is a rare form of manifestation that occurs through the bloodstream.
- The intestinal tuberculosis is very rare, but it occurs mostly through a primary infection with Mycobacterium bovis in infected milk.
- When laryngeal tuberculosis ( Larynxtuberkulose ) is a highly infectious complication of (open) pulmonary tuberculosis.
- A rare manifestation is tuberculosis of the teeth, the oral mucosa and the tongue, which can usually result from bronchogenic spread in pre-existing lesions. Oral findings can include tooth granulomas, ulcers of the gums and oral mucosa, and an enlarged tongue. Oral involvement is found in around 1.4% of those suffering from tuberculosis, according to studies. Oral tuberculosis can also occur in isolation.
Diagnosis
A history of infection , a tuberculin skin test, an interferon-γ blood test, tissue examinations, imaging diagnostics and, if at all possible, the detection of the cultural pathogen contribute to the diagnosis. The diagnosis is only confirmed if the case definitions, in Germany those of the Robert Koch Institute , are met, for example if, in addition to the clinical picture, there is evidence of a cultural pathogen of Mycobacterium tuberculosis . These methods can be supplemented by modern molecular biological or immunological test procedures for special questions . However, a reliable diagnosis is made more difficult by the extremely different presentation.
Tuberculin skin testing
When tuberculin skin test , a defined amount of purified and filtered (also called Mantoux test) antigens of mycobacteria (tuberculin) into the skin ( epidermis injected). Also common stamp tests are very unreliable and therefore not recommended. If the immune system of the person tested has already had contact with mycobacteria, a defense reaction occurs at the relevant point within three days with immune cells migrating into the skin, which leads to thickening. This is a type IV reaction (according to COOMBS). The test becomes positive just six weeks after infection with TBC.
A palpable hardening at the test site is called a positive reaction. This can mean that a tuberculosis infection has taken place. However, the test says nothing about a disease. A positive test reaction is also possible after a tuberculosis vaccination. If the skin at the test site remains unchanged or if it only shows reddening, this is rated as negative. A tuberculosis infection is then ruled out with a high degree of probability.
The tuberculin test is harmless and well tolerated. It can also be carried out without hesitation for pregnant women, nursing mothers or small children.
Tuberculin tests are only reliable to a limited extent. On the one hand, they can remain negative, especially in severe cases, such as miliary tuberculosis. On the other hand, an earlier vaccination or contact with atypical mycobacteria ( mycobacteria other than tuberculosis, MOTT ) lead to a false positive reaction.
Imaging
If there is a suspicion of tuberculosis based on symptoms and previous history, X-ray examinations or, in the case of special questions, CT of the lungs are useful imaging methods even if the tuberculin test is negative . They often reveal the characteristic, moth-eaten picture of the lung infestation of tuberculosis, which has earned the disease the nickname the moth . These examinations also show a finding in closed tuberculosis. The disadvantage, however, is that an X-ray cannot differentiate between tuberculosis and other lung diseases with sufficient certainty.
In children under 15 years of age and pregnant women, if tuberculosis is suspected, an immunological test method such as γ-interferon test or a tuberculin skin test should be preferred instead of an X-ray .
Pathogen detection
The diagnosis of tuberculosis is confirmed when there is cultural evidence of the pathogen. However, this is only possible without further ado from the sputum in the case of open tuberculosis, i.e. when the tuberculous tissue changes are connected to the bronchial system , the urinary tract or the intestines and can be excreted. Otherwise, an attempt can be made to obtain material through punctures with needles or directly by removing tissue. The advantage of cultural evidence lies in the possibility of being able to carry out a resistance test and should therefore always be aimed for, since the treatment can then be carried out in a targeted manner.
Since children firstly have hardly any sputum and secondly only a few bacteria cough up, a conventional sputum test is hardly reliable for them. The gastric fasting juice is therefore examined in childhood, because this is where all the secretion that the children coughed up during the night and then swallowed collects . The mycobacteria, in turn, are acid-resistant and can survive in gastric juice. South African researchers were able to prove that the pathogen detection is also possible in infants and children from the sputum. If you let them inhale beforehand with a high-percentage saline solution (induced sputum), the detection of mycobacteria from the subsequently coughed up secretion is as reliable as from gastric juice.
Due to the slow growth of the germs, you have to wait four to six weeks for a result on conventional, solid culture media. In liquid cultures with modern detection methods for mycobacterial growth, the detection can be successful after about two weeks. The animal experiment that was often used in the past, in which guinea pigs were injected with the material to be examined into the abdominal cavity, is no longer used. Modern detection methods include molecular genetic methods such as the polymerase chain reaction .
Immunological test procedures
In addition to the tuberculin skin test, a further immunological test procedure, the so-called γ-interferon test, has been available as a further diagnostic option since 2005 . Defense cells from the test person's blood are stimulated with a mixture of antigens from Mycobacterium tuberculosis . If the person concerned has already had contact with the pathogen due to a tuberculosis infection, they increasingly produce the messenger substance interferon-γ . The concentration of this interferon-γ can be determined in the cell supernatant and in blood samples from infected people is significantly higher than that in a negative control to be carried . Since the selected antigens should only occur in Mycobacterium tuberculosis , but not in most of the atypical mycobacteria and also not in the vaccine strains of the mycobacteria used for the BCG vaccination, this method can theoretically be used to pass between infections if the tuberculin skin test is positive Differentiate tuberculosis bacteria and atypical mycobacteria. The sensitivity of these tests is given in various papers with 82% to 100%, the specificity with 98%.
However, performing the tests is associated with difficulties and uncertainties in practice. The time window for the incubation and the necessary temperature constancy of 37 ° C offer sources of error, as well as the necessary experience with the method in the laboratory itself. The specified values for sensitivity and specificity are therefore far from being achieved in practice. With the two tests introduced, the ELISPOT (especially the T-SPOT test) seems to have an advantage, especially in children and with an extremely low number of helper cells. But here, too, there are sources of error in the preanalytical phase.
As with all examination methods, the sensitivity and specificity of which is not 100%, the informative value also depends on the frequency of the real infection. Therefore, these in vitro tests are also unsuitable for screening population or occupational groups with low levels of contamination. In the case of doubtful exposure and positive failure or confirmed close exposure and negative failure, a precise clinical examination using the Mendel-Mantoux method and, if necessary, a repetition with the alternating Y interferon test is recommended. The time of infection cannot be determined with the newer in vitro test methods either. The test often turns negative again in the following decades after the infection has healed. There have been reports of disturbances from previous BCG vaccinations or booster effects after previous testing according to Mendel-Mantoux.
In 2010, a British research group presented a test based on changes in the transcription signature in neutrophils. This test should make it possible to differentiate between a past and an active infection. The market readiness remains to be seen.
therapy
Since the pathogens divide very slowly and can also rest for a long time in the tubercular granulomas, the risk of developing resistance in mycobacteria is particularly high. In the case of confirmed tuberculosis or even high-grade suspicion of tuberculosis, all patients must therefore be treated with a combination therapy consisting of several antibiotics (also known as antituberculotics) that are especially effective against Mycobacterium tuberculosis . In addition, because of the low rate of division, the duration of the treatment must be long enough to avoid relapses.
Standard therapy
According to the 2011 guidelines, the treatment of uncomplicated tuberculosis should consist of a four-fold combination of isoniazid , rifampicin , ethambutol and pyrazinamide and should initially be carried out for two months. Thereafter, treatment with isoniazid and rifampicin must be continued for another four months. So it takes a total of at least six months. In children, only a triple combination (without ethambutol) is initially used. In particularly mild cases, this is exceptionally possible for adults. Streptomycin is also available as a reserve medication in the event of intolerance . Thiacetazone , a sixth substance, is not used in industrialized nations due to an unfavorable side effect profile. It is not recommended for the treatment of co-infected patients with HIV. However, the majority of tuberculosis sufferers in some poor countries, where the substance is still used because of the low price, are also HIV-positive.
The most common side effect of isoniazid is peripheral polyneuropathy . As with rifampicin and pyrazinamide, liver damage can also occur. Ethambutol can cause inflammation of the optic nerve, while streptomycin damages the kidneys and inner ear . These organs should be examined before starting and monitored during the course of therapy.
Since the patients often feel relatively healthy, many of them no longer take the tablets regularly after a certain period of time (this is referred to as low compliance ). Since several new tuberculosis drugs are about to be approved, mouse studies are already being carried out to determine which drug combination could shorten the treatment time. With the combination of TMC207, pyrazinamide and rifapentine / moxifloxazine, 100 percent of the germs in the mouse could be killed despite the shortening to two months.
Should a resistance be found in the microbiological bacterial culture, a change to other antibiotics, to which the specific bacterial strain is actually sensitive, must be considered in terms of a specific therapy. In liquid cultures (Bactec MGIT), growth of mycobacteria can be detected after one week with a high initial concentration and without pretreatment. A positive growth in the liquid culture system alone does not allow a species diagnosis of the mycobacteria, but it represents the basis for an exact species differentiation by means of further diagnostic methods. The parallel incubation of solid culture media (Löwenstein-Jensen and Stonebrink medium) usually takes longer, but allows one Assessment of colony morphology. The final result of the culture is available in the festival culture after a maximum of 8-10 weeks. The conventional resistance test of the standard drugs takes at least ten days. There are now commercial rapid tests that can detect resistance earlier using molecular biological methods. However, these newer methods have not yet proven themselves in practice.
Therapy of multi-resistant tuberculosis
If there is resistance to the standard drugs, after testing all available antituberculotics, the treatment should be expanded to include at least two effective substances. Apply combinations of different active compounds: The aminoglycosides capreomycin and kanamycin , the fluoroquinolones , ofloxacin / levofloxacin , ciprofloxacin and moxifloxacin , the thionamides ethionamide , prothionamide , as well as a bacteriostatic active substances 4-aminosalicylic acid (PAS), and cycloserine or terizidone .
Streptomycin, amikacin and protionamide can also be used as secondary therapy for resistance .
For some time, the antibiotic linezolid was considered a miracle weapon against multi-resistant tuberculosis and is still used today in particularly severe cases. However, in a recent study by Lee, 82% of patients may develop linezolid-associated side effects. The most common adverse effects are myelosuppression with anemia and neutropenia, optic neuropathy, and peripheral neuropathy.
The treatment of multidrug-resistant tuberculosis ( English multidrug-resistant tuberculosis - MDR-TB ) is taking multiple drugs simultaneously over a period of at least 21 months. For the first three months, patients are given a mixture of five different drugs. In principle, the chances of successful treatment of multi-drug-resistant tuberculosis are lower than with treatment of uncomplicated tuberculosis, even if the patient receives the most efficient therapy.
The use of ofloxazine and levofloxazine is hardly feasible in poorer countries due to the comparatively high product prices. Both active ingredients are patented by the manufacturer. Capreomycin is only sold by a single manufacturer ( Eli Lilly ) at a price that enormously restricts its use.
In the meantime, newer drugs are also included in the treatment of multi-drug resistant tuberculosis. So were in a mouse model successfully combinations of Bedaquiline , PA-824 and Sutezolid and rifapentine used.
Bedaquiline (trade name Sirturo ) has meanwhile been approved by the European Commission . Two other drugs - the new chemical entity Delamanid (trade name: Deltyba ; manufacturer: Otsuka Pharmaceuticals ) and the long-known substance 4-aminosalicylic acid (trade name: Granupas ; manufacturer: Lucane ) - were approved across Europe in May 2014.
In a Turkish study, the additional use of pulmonary resection resulted in permanent cure in 12 of 13 MDR-TB patients.
Among other things, thioridazine reduces the activity of antibiotic resistance in Mycobacterium tuberculosis, which is why its use in combination with antibiotics is being investigated.
Therapy of complex tuberculosis
In the event of additional complications, such as obstruction of part of the airway by an involved lymph node, the treatment should be extended to a total of nine to twelve months. Miliary tuberculosis or tuberculous meningitis (meningitis) require an initial quadruple therapy, even in childhood, for more than three months and an extension of the total duration of treatment to nine to twelve months. In addition, the patients should be treated for at least six weeks with prednisolone or, in the case of meningitis, with dexamethasone in descending doses.
The treatment of tuberculosis in simultaneously HIV-infected patients represents a particular therapeutic challenge. In particular, the standard drug rifampicin must not be administered at the same time as certain active substances that are used to treat HIV infection due to significant interactions. Therefore, either the HIV therapy or the tuberculostatic therapy must be changed by appropriately experienced specialists.
Supportive treatment
Due to the difficulty and length of the standard therapy, attempts were made to support the therapy by adding various substances. The most promising were L- arginine , an amino acid that is supposed to support the formation of reactive nitrogen species in macrophages , for example through daily consumption of 30 peanuts, which contain about 1 g of L-arginine, and vitamin D , its general supportive role in infections is occupied. Both substances are insufficiently available in sick people.
In a randomized study by Queen Mary University of London, high-dose vitamin D therapy in patients with pulmonary tuberculosis even accelerated microscopic sputum conversion. H. the length of time patients are contagious decreased significantly from 36 to 23 days. The concentration of various inflammatory cytokines and chemokines in the blood was reduced and life-threatening inflammatory symptoms decreased faster than in the control group.
In a study with rabbits, Subbian and others also investigated the influence of a PDE-4 inhibitor on the innate immune response in the lungs and the effect that their weakening in turn had on the expression of various bacterial genes. There was a reduced expression of the INH resistance genes and, related to this, a better clearance of the tissue after treatment with isoniazid .
Another possibility is to weaken the granuloma formation in the lungs using lactoferrin . There are no clinical studies on this yet.
Prevention
Since there is currently no effective vaccination against tuberculosis, the most important preventive measure is to detect infected people as early as possible and treat them both quickly and effectively. Because of the low number of cases in Germany, serial examinations in the form of tuberculin tests or X-ray examinations are not useful. The active search for infected people in the form of a surrounding investigation of contact persons of patients with infectious tuberculosis is an indispensable prerequisite for reducing the incidence of the disease. The group of people with an increased risk of tuberculosis who should be actively searched for an infection also includes, for example, people from countries with a high tuberculosis rate, the homeless, drug addicts, prison inmates, but also HIV-positive people. The personal risk of illness can now be assessed algorithmically taking into account important influencing factors . A sophisticated example of this, which also takes into account drug intolerance, is the online TST / IGRA interpreter, which was developed at McGill University in Canada by Dick Menzies and his colleagues.
vaccination
Until 1998 an active vaccination (live vaccination) with the weakened mycobacteria vaccine strain Bacillus Calmette-Guérin (BCG) against tuberculosis was carried out in Germany. Due to the decreasing protective effect, local complications and side effects and the changed epidemiological situation, the indication for BCG vaccination has only rarely been made in Germany since 1998. When the vaccine was introduced, the Lübeck vaccination accident occurred in Lübeck in 1930 . 208 children were infected with virulent tuberculosis bacteria through incorrect processing of the BCG culture obtained from Paris into a vaccine. 77 of them died. Because of this vaccination accident, we now know a lot about the course of the disease from observing these children. The introduction of vaccination in Germany was delayed until after the Second World War. The BCG vaccination is no longer recommended by the Standing Vaccination Commission because the limited effectiveness could not outweigh the vaccination complications. In addition, the tuberculin test in vaccinated people is occasionally slightly to moderately positive even after decades. For this reason, this test (e.g. after contact with a person suffering from open TBC) is only rated positive if there is a stronger reaction in the form of a hardened swelling (induration) of more than 15 mm across the forearm axis. The BCG vaccination was also unable to curb the spread of tuberculosis worldwide, although it is one of the most widespread vaccinations. Only the particularly fulminant and feared courses in childhood in the form of tuberculous meningitis or miliary tuberculosis can the BCG vaccination be able to prevent relatively reliably. Various researchers are currently trying to increase the effectiveness of the BCG vaccine strain through genetic engineering changes in which the vaccine bacteria produce additional antigens that enable the immune system to react better to the real mycobacteria.
The BCG vaccine is very poorly effective , especially in the tropics and subtropics . Animal models as well as vaccination studies with humans have shown that the poor effectiveness is due to existing immune responses to soil and (drinking) water-dwelling, non- pathogenic Mycobacterium species. Many of the mycobacteria have cross-reactive antigens , so that infection with one mycobacterium gives some protection against infection with the other. This has consequences for vaccination protection: On the one hand, there are antibodies against the BCG live vaccine - the vaccine is destroyed by the body before it can stimulate the immune system itself. And secondly, the mycobacteria ingested in daily life provide such good protection against the tuberculosis bacterium that the vaccination does not provide any additional protection worth mentioning. It is assumed that the better hygiene and drinking water treatment in industrialized countries lack this natural vaccination and that BCG vaccination has been effective up to now. In the 1970s, a tuberculosis vaccine study was carried out on 260,000 people in India. This showed that more cases of tuberculosis occurred in the vaccinated than in the unvaccinated.
A phase I study with a new vaccine VPM1002 was tested in Neuss in 2009 and 2010 with 80 volunteers and rated as being well tolerated. The vaccine VPM1002 will be tested in a phase III study in 2000 people in India until 2020.
The so far promising vaccine MVA85A showed weaknesses in the phase II study in 2013. There is no improvement over the previous vaccine in vaccinated, healthy and HIV-negative infants. However, it remains to be seen whether the vaccine will be of benefit in adults or HIV-positive people (who are not allowed to receive the live vaccine). In addition to this, 12 other tuberculosis vaccines are currently in the clinical phase, AERAS-402 / Crucell Ad35 and GSK M72 are currently being tested on adults and children in South Africa.
At the end of 2010 it was shown that intranasal vaccination with mRNA (Hsp-65) of M. leprae effectively and safely protects against infection with M. tuberculosis in a mouse model .
Another new development is H4: IC31. This is a recombinant fusion protein H4 and the adjuvant IC31. H4 consists of the tubercle antigens Ag85B and TB10.4. Ag85B is also called α-antigen and is a Mycolyl - transferase . TB10.4 is one of three very similar proteins in the ESAT-6 group of Mycobacterium tuberculosis. A test in South Africa on BCG-vaccinated youths was promising.
Chemoprophylaxis and chemoprevention
Since small children under five get sick more often and faster than adults after an infection (according to the literature, 20% of infected children get sick with a minimum latency period of around three weeks to years or even decades), special conditions apply to them after contact with people suffering from tuberculosis Precautionary measures. Even if the tuberculin test is negative, they should be treated prophylactically with antituberculotics (e.g. isoniazid ) for two months according to the guidelines of the Swiss Lung League . If after these two months the tuberculin test is still negative, treatment can be stopped. However, if the tuberculin test has become positive in the meantime, active tuberculosis must be ruled out by an X-ray examination of the lungs. In Europe, this is done through a breast photograph; overseas as in Australia, on the other hand, computed tomography of the chest organs is recommended, especially for children. Treatment with the anti-tuberculosis drug is then continued for additional months as chemoprevention. If the pathogen at the source of infection is known to be resistant to the antituberculotic, chemoprophylaxis must of course be carried out with another active ingredient, preferably rifampicin . In the case of multiple resistances, it should even be carried out with two different active substances.
Reporting requirement
In Germany, tuberculosis “requiring treatment” in humans is a notifiable disease within the meaning of the Infection Protection Act (IfSG), even if there is no bacteriological evidence ( Section 6 (1) sentence 1 number 1a letter a IfSG). Illness and death are to be reported. In addition, the public health department must be reported “if people who are ill with pulmonary tuberculosis that require treatment refuse or discontinue treatment” ( Section 6 (1) sentence 2 IfSG). In addition, there is also a notification obligation for the management of communal facilities according to Section 34 (6) IfSG.
In the case of animals, the disease in Germany is a notifiable animal disease according to Section 26 of the Animal Health Act (TierGesG) in conjunction with Section 1 and the annex of the ordinance on notifiable animal diseases. Exceptions are Mycobacterium bovis - including their subspecies infections, which are even notifiable animal diseases according to Section 4 TierGesG in conjunction with Section 1 of the Ordinance on Notifiable Animal Diseases .
In Austria, tuberculosis in humans is a notifiable disease in accordance with Section 3 of the Tuberculosis Act . According to this, every evidence of a tuberculosis pathogen, every active or contagious tuberculosis disease and every death that can be traced back to it must be reported. In addition, any suspicion of tuberculosis must be reported if the person with tuberculosis eludes the diagnostic work-up. According to Section 2 of the Tuberculosis Act, there is also an obligation to seek treatment (treatment obligation).
In Austria, tuberculosis in cattle is notifiable according to Section 16 of the Animal Diseases Act.
In Switzerland tuberculosis in humans also a notifiable disease and that after the Epidemics Act (EpG) in connection with the epidemic Regulation and Annex 1 of the Regulation of EDI on the reporting of observations of communicable diseases of man. The start of treatment with three different antituberculotics or evidence of mycobacteria of the tuberculosis complex in clinical material must be reported.
In Switzerland, tuberculosis is notifiable as an animal disease to be eradicated within the meaning of Article 3 of the Animal Diseases Ordinance (TSV) with extensive obligations under Articles 158–165a.
Tuberculosis in other living things
Tuberculosis occurs in almost all vertebrates and, in addition to M. tuberculosis, can be triggered by numerous other mycobacteria of the Mycobacterium tuberculosis complex .
Mycobacterium tuberculosis
M. tuberculosis can cause disease in both domestic animals and wild animals (such as deer and springboks ). The infection is described due to the closer contact with humans in many domesticated species, e.g. B. in domestic dogs , house cats and parrots , and in zoo animals such as elephants .
In most animal species, the primary focus is mainly in the lungs, so the disease is similar to pulmonary tuberculosis in humans. In pigs , the mesenteric lymph nodes are almost exclusively affected. In cattle, the infection with M. tuberculosis usually proceeds without any pathological processes, but what is important is that the pathogen is excreted with the milk, which is why pasteurization of the milk was an essential measure for combating tuberculosis in humans. Raw milk should only be consumed from tuberculosis-free cattle herds.
Other mycobacteria
The tuberculosis in cattle is from animal tuberculosis to humans most significantly. Their pathogens, Mycobacterium bovis and Mycobacterium caprae , have a relatively high host specificity, but can also cause diseases in humans and other mammals (including many domestic animals and numerous wild animals), making it a zoonotic pathogen. Bovine tuberculosis is a notifiable animal disease . For infections in other domestic animals as cattle, as well as in wild mammals is reporting obligation .
The poultry tuberculosis is M. avium causes. It was one of the most common diseases in domestic chickens , but is rare today. In principle, all bird species , but also humans, cattle , pigs , sheep , goats , cats and, above all, rabbits are susceptible. Avian tuberculosis is one of the notifiable animal diseases .
In snakes , tuberculosis is rare and usually runs chronically infected with tubercle in the internal organs, the subcutaneous or in its mouth. The main pathogens are M. thamnopheos , M. marinum and M. chelonae . In lizards , the disease is also rare and runs as a non-specific general disease or with manifestations in the skin. The main pathogens are M. ulcerans , M. marinum and M. thamnopheos. M. ulcerans causes Buruli ulcer in humans .
The fish tuberculosis is M. marinum, M. fortuitum and M. chelonae produced and affects both freshwater and saltwater fish. When fed to infected fish, M. chelonae can also cause ulcerative changes in the upper digestive tract, pneumonia and skin diseases in turtles .
The paratuberculosis is a by M. paratuberculosis induced bowel disease of ruminants .
Pseudotuberculosis
Two different clinical pictures that are very similar to tuberculosis, but which are not caused by mycobacteria, are referred to as pseudotuberculosis .
Pseudotuberculosis in goats and sheep - cattle, horses, pigs and increasingly camels are more rarely affected - is an infectious disease caused by the bacterium Corynebacterium pseudotuberculosis, which is related to the mycobacteria . In humans, after massive contact with Corynebacterium pseudotuberculosis , infections with lymph node inflammation can occur.
Likewise, the yersiniosis caused by Yersinia pseudotuberculosis in rabbits, rodents and birds is called pseudotuberculosis, and in rodents it is also called rodentiosis. Yersinia pseudotuberculosis is potentially pathogenic to many mammalian and avian species , including humans.
history
Paleolithic and Neolithic
Investigations of an approximately 500,000 year old fossil of the early man Homo erectus from Turkey showed that tuberculosis occurred much earlier in human history than previously thought. On the roof of the skull there were traces of meningitis caused by tuberculosis ( leptomeningitis tuberculosa ). The researchers speculate that this early man, who came from Africa, was dark-skinned and was therefore able to produce significantly less vitamin D compared to fair-skinned people , which could have made him particularly susceptible to this disease. This assumption of a disease of tuberculosis, which is based only on morphological skeletal changes, as well as the further, now for the first time molecular-biological confirmed finding of a 9,000-year-old sample confirm the assumption of modern research that tuberculosis did not occur in the Neolithic during the domestication of cattle from them to Skipped humans, but developed in parallel with Homo erectus during a long period that began much earlier . Also skeletal remains of prehistoric people dating back to approx. 4000 BC. BC show traces of the disease. It is also not a question of geographically isolated findings; rather, Mycobacterium tuberculosis was detected as early as 2001 in Wyoming , North America, in 17,000 year old finds.
antiquity
Tubercular destruction was found in the bones of Egyptian mummies from 3000 to 2400 BC. Similar findings from ancient America date to around 2000 BC. According to written records there is evidence of a tuberculosis epidemic in India around 1300 BC. Chr.
In the 5th century BC Chr. Featured Hippocrates consumptive ( Greek. Φθίσις Phthisis loss, wasting) as one of the epidemics, which was almost always fatal. Impressive descriptions of illnesses have come down to us from him.
middle Ages
In the early Middle Ages, tuberculosis played a subordinate role in Europe due to the sparse population. It was only more strongly represented in the few metropolitan areas. This primarily included Byzantium . The tuberculosis victims of the time came from all classes up to members of the imperial family. The medical literature from Byzantium describes tubercular disease patterns at all times. Significant innovations in the treatment of tuberculosis, however, were not introduced in the Middle Ages. Until the early modern period, the level of Hippocratic writings and their Galen was maintained . One of the few exceptions was Alexander von Tralleis from Lydia in the 6th century , who further developed or differentiated therapeutic measures.
Early modern age
After a previous outbreak in Italy in the second half of the 15th century, the largest and longest historical wave of tuberculosis began in the 17th century. It reached its peak in the 18th century and, after a temporary flare-up of the epidemic shortly after the First and Second World Wars, continues in the last foothills to this day.
With regard to the conception of pathogenesis, different traditions existed in the European countries of the 18th century. Many medical writers that time considered the tuberculosis or the not always so synonymous consumption (from Middle High German Swinden "dwindle, lose weight, lose weight, etc.") as the worst among the then-known disease. The cause they saw was an uneven distribution of body fluids , ominous evaporation from the soil, urbanization or the decay of morals. In Italy, on the other hand, there was traditionally a tendency towards contagious, i.e. H. communicable cause. Consequently, in the middle of the 18th century, the Republic of Venice introduced compulsory written notification of illnesses caused by phthisis (consumption in the case of pulmonary tuberculosis). The personal effects of those who died of the disease were burned to reduce the risk of infection.
In England and the Nordic countries, on the other hand, it was commonly believed that the disease was due to a hereditary (hereditary) cause. A major exception in England was the publication Benjamin Martens from 1720: A New Theory of Consumptions, in which Marten, 162 years before Robert Koch, attributed the cause of the disease to an infection by microorganisms. Martens published a small edition publication, however, found no further reception. In France, Germany and Switzerland, representatives of both schools mixed. In some cases, the hereditary theory was expressly represented here, but at the same time measures were introduced to reduce the risk of infection.
Johann Jakob Wepfer in Schaffhausen played a prominent role among the phthisiologists of his time , who had adopted the idea of the contagious etiology of the disease during his study visit to Italy . He was the first to describe the formation of the lung caverns ( hanc calamitatem ) from tubercles ( tubercula ). His work and studies on the epidemiology of tuberculosis went in many ways qualitatively beyond the achievements of the following two centuries. They were only published posthumously by his son in 1727 and remained unknown outside a small circle of experts.
19th century
Due to the multitude of its symptoms, the disease was not differentiated from others with symptoms similar to those of scrofula, which is rare today, until the 19th century . It was not until 1819 that René Laënnec explained the uniformity of tubercles with miliary nodules and (tuberculous) caverns and recognized that tuberculous matter can also form in other organs in addition to the lungs. It was not until 1839 that Johann Lukas Schönlein coined the uniform term tuberculosis.
Tuberculosis gained general interest as the endemic disease of the urban poor in the 19th and early 20th centuries . In 1815 a quarter of deaths in England and in 1918 in France a sixth of deaths were caused by tuberculosis. In the age group of 15 to 40 year olds, every second death in Germany around 1880 was due to this disease. Tuberculosis was also the most common cause of death in rural areas. Of the 2188 deaths recorded in the Liechtenstein municipality of Triesen between 1831 and 1930, 15% were due to tuberculosis.
In the 19th century, the air cure , in which patients had to lie in the open air for several hours a day, became the preferred therapy for tuberculosis. This took place in our own tuberculosis sanatoriums ( lung sanatoriums ); Hermann Brehmer built the first one in the world in 1855 in Görbersdorf, Lower Silesia (today Sokołowsko , Poland).
After it was recognized in the north that the disease was contagious, tuberculosis became notifiable in Great Britain in the 1880s. Back then there were campaigns to avoid spitting out in public places. The infected poor were encouraged to go to sanatoriums that were more like prisons. Despite the alleged use of fresh air and the work in the sanatorium, 75 percent of the inmates died within five years (1908).
In addition to such measures, which were still attached to the hygienic-dietary treatment concept, there were also very different local treatment concepts in the 19th century with increasingly better surgical options. In particular, the pneumothorax technique or pneumolysis found widespread use in numerous variants. An affected lung was artificially made to collapse in order to cause the lungs to come to a standstill and the changes to heal. The Italian physician Carlo Forlanini is considered to be the inventor of this collapse therapy for pulmonary tuberculosis (since 1892). This technique was of little use and was gradually discontinued after 1946. In addition, ever finer resection procedures were developed with which the affected lung sections were removed. The internationally renowned French cardiac surgeon Théodore Tuffier was the first to resect the tip of the lung in tuberculosis.
The bacterium Mycobacterium tuberculosis was described by Robert Koch on March 24, 1882. In 1905 he received the Nobel Prize in Physiology or Medicine for his discovery of the pathogen . Koch did not believe that bovine and human tuberculosis were similar, which delayed the detection of infected milk as the source of the disease. This source was later eliminated by pasteurization . In 1890, Koch brewed a glycerine extract of the tubercle bacilli as an aid to the treatment of tuberculosis and named it tuberculin . However, it was not effective when it was used euphorically at first. The observation of local skin reactions when using tuberculin later led to the development of a test procedure for the detection of infection or disease by Clemens von Pirquet in 1907, Felix Mendel and Charles Mantoux around 1910.
In 1883, Robert Koch first detected tubercle bacilli in the tissue of lupus vulgaris, a skin disease that was first described as an independent clinical picture at the beginning of the 19th century, and thus showed its cause as skin tuberculosis. According to the experience of a Bielefeld doctor named Gerson, a diet rich in minerals but salt-free apparently showed (allegedly in 448 of 450 cases) by the surgeon Ferdinand Sauerbruch in Munich, where he had set up a lupus ward at the university clinic (in the first quarter of the 20th century) ) Successes in the treatment of skin tuberculosis.
20th century
Albert Calmette and Camille Guérin had the first success with immunization against tuberculosis in 1906 with their BCG vaccine. It was first used on humans in France on July 18, 1921. Nationalist currents, which used the Lübeck vaccination accident for their own purposes, prevented widespread use in Germany until after the Second World War .
Nevertheless, the death rate caused by tuberculosis fell significantly in Europe in the hundred years from 1850 to 1950 from 500 to 50 per year, based on 100,000 inhabitants. Improvements in the public health system, especially the establishment of a dense network of tuberculosis welfare offices from 1905, reduced the number of illnesses even before the introduction of antibiotics. The concept changed several times. Until 1945, the focus was on the treatment of early and slightly ill cases. The inpatient treatment concept was fundamentally changed in 1945 based on the experience of the war-influenced years 1917 to 1919. Primarily only seriously ill and contagious patients came to the sanatoriums. The medical facilities have been upgraded with equipment to be able to offer maximum care, including lung surgery procedures.
With the development of the antibiotic streptomycin in 1943, active treatment became possible in addition to prevention. The success, however, clouded the frequent resistance of the mycobacteria to streptomycin. The almost simultaneous production of para-aminosalicylic acid (PAS) initially received little attention, although the combination of these two substances makes the formation of resistant strains more difficult. From 1952 isoniazid found increasing use as another tuberculosis drug. Combination therapy to avoid the development of resistance became the standard for tuberculosis treatment from that time on. The breakthrough in anti-tuberculosis treatment, which continues to this day, was achieved in the 1960s with the addition of ethambutol and, most recently, rifampicin.
Due to the abolition of the public health system in New York in the 1970s, there was an increase in diseases there in the 1980s. The number of those unable to take their medication was high. As a result, more than 20,000 people in New York suffered a preventable infection with antibiotic-resistant strains.
Since the emergence of antibiotic-resistant strains (i.e., resistant to at least rifampicin and isoniazid) in the 1980s, hopes that the disease could be eradicated completely have diminished. There were 50,000 cases of tuberculosis in Great Britain around 1955. From 1987 to 2001 the number of tuberculosis sufferers in Great Britain rose again from 5500 to over 7000 confirmed cases.
The resurgence of tuberculosis caused the WHO to declare a global health emergency in 1993. In 1996 she declared March 24th World Tuberculosis Day .
21st century
In countries outside of Europe and North America, such as B. Bangladesh , tuberculosis remains a major health problem in the 21st century . A renewed increase in cases has been linked several times to the problem of climate change .
Tuberculosis in Art
Because of its enormous importance, the disease is reflected in many ways in art. Some artists dealt with the confrontation with their early (own) death in an impressive way. Even in the performing arts of the Egyptians, from the Middle Kingdom onwards, the representation of the gibbus, the striking external expression of Pott's Disease, was found . Similar representations have also come down to us from ancient American cultures.
- In the last years of his life, the German writer Friedrich Schiller showed more and more symptoms of tuberculosis. During this time, one of his most important works was created, the drama Wilhelm Tell . On May 9, 1805, the writer died of acute pneumonia caused by tuberculosis in Weimar.
- Three of the six Brontë siblings died of tuberculosis. Charlotte Brontë took up the subject in her novel Jane Eyre , in which Jane's friend Helen Burns dies from it. Tuberculosis is also an issue in her sister Emily Brontë's novel Sturmhöhe . Hindley's wife, Frances, dies of tuberculosis at a very young age.
- As early as 1848 Alexandre Dumas the Elder had J. in his novel La Dame aux Camélias - The Lady of the Camellias (EA Paris, Alexandre Cadot) the main female character dying of tuberculosis. The material was used by Giuseppe Verdi (music) and Francesco Maria Piave (libretto) in the opera La traviata (Italian: The Stumped or The Derailed), which premiered in 1853 . In this, Violetta Valery realistically perishes three acts of the white plague . At the time of its creation, it was almost a scandal to stage death so realistically.
- In the novel Anna Karenina , the author Leo Tolstoy lets his character Nikolaj Dmitrijewitsch Levin die of tuberculosis.
- In the opera La Bohème by Giacomo Puccini , which premiered in 1896 , the main character Mimì died of tuberculosis in the fourth act.
- In Knut Hamsun's story Victoria (1898), too , the heroine last died of tuberculosis.
- The Czech poet Jiří Wolker died of tuberculosis at the age of 24; he dealt with his illness and the approaching death in his later work.
- One of the best-known examples is probably Thomas Mann's Zauberberg (first edition from 1924). Inspired by the illness of his wife Katia , he locates the plot of the world-famous novel in Davos at a time without effective medication.
- Franz Kafka's pulmonary tuberculosis disease, from which he died in an Austrian sanatorium near Vienna in 1924, is the subject of the biographical novel The Glory of Life by Michael Kumpfmüller (2011). In Franz Kafka's parable Auf der Galerie , the rider mentioned in the first part suffers from tuberculosis, called "lung addiction" there. Franz Kafka suffered from tuberculosis all his life.
- The American country musician Jimmie Rodgers sings several songs about his TB illness, from which he died in 1933 at the age of 35 (TB Blues, 1931; Whippin 'That Old TB, 1933).
- In the song TB Sheets , published in 1967, the Northern Irish musician Van Morrison describes the suffering of a young girl who is dying in the tuberculosis ward of a hospital from the perspective of her boyfriend who is completely overwhelmed by the situation.
- In John Schlesinger's film Asphalt-Cowboy (1969) the small crook Ratso - played by Dustin Hoffman - is languishing with tuberculosis.
- In the novel The Diary of Jutta S. by Inge Stolten , the diagnostic and therapeutic methods of the 1950s are described in detail, including a longer stay in the climatic cure for the main character.
- In the novel Les trois quarts du temps (I want to live), Benoîte Groult describes the treatment methods used in 1945 until the sick Jean-Marie died.
- The French graphic artist Józef Gielniak , who died of tuberculosis in a sanatorium in 1972, artistically portrayed the subject of tuberculosis with its health and social consequences as well as the closed world of sanatoriums in his linocuts.
- One carries the other's burden ... (1987), award-winning DEFA film, director: Lothar Warneke : During the GDR era, a police officer and a Protestant pastor had to share a room in a tuberculosis clinic. They discuss God, love, the meaning of life, death and illness. The initial aversion turns into friendship.
- Thomas Bernhard , who had suffered from tuberculosis himself from an early age, dealt with the disease in almost all plants. Many of his protagonists are sick and suffering. This becomes particularly clear in his autobiographical volumes Die Kälte and Der Atem . Bernhard died in 1989 from the consequences of this disease.
- In the novel The Eternal Gardener, John le Carré describes a 2001 conspiracy by a multinational company that uses a new type of drug against tuberculosis that is still being developed in a field trial on local people in Kenya without their knowledge, thereby exceeding ethical boundaries.
- Further examples from literature and film are in novels by Fyodor Dostojewski Ippolít Teréntjeff in The Idiot and Katerina Ivanovna in Guilt and Atonement ; Julika Stiller-Tschudy in Stiller (novel by Max Frisch ); Patrice Hollmann (Pat) in Erich Maria Remarque's novel Three Comrades ; Lilian in Remarque's novel Heaven has no minions ; Ruby Gillis in Anne at Kingsport (novel by Lucy Maud Montgomery ); Red Stovall (played by Clint Eastwood ) in the film Honkytonk Man (US 1982); Satine (played by Nicole Kidman ) in the film Moulin Rouge (USA 2001), based on Verdi's opera or Dumas' novel, see above.
- Angorichina is a 2011 novel by Marion Grace Wolley about people in a tuberculosis sanatorium in Australia in the 1930s.
- In the 2014 film Winter's Tale , starring Colin Farrell , Beverly Penn, the lover of the main hero, played by Jessica Brown Findlay , dies of tuberculosis.
- In the novel, Ana in Venice by João Silvério Trevisan one of the main characters, the black former slave suffers Ana, in their final years of tuberculosis.
- In the video game Red Dead Redemption 2, the main character falls ill with tuberculosis in the course of the game.
museum
On December 1, 2011, the Museum of Tuberculosis was opened in the Rohrbacher Schlösschen in Heidelberg on the grounds of the Thorax Clinic. To a large extent it consists of the exhibits and specialist literature from the former tuberculosis archive in Fulda , which was headed by the pulmonary specialist Robert Kropp; it has been open to the public since early 2012.
World tuberculosis day
World Tuberculosis Day takes place on March 24th every year . It was proclaimed by the World Health Organization (WHO) and is supported by the European Medicines Agency (EMA). Its purpose is to raise public awareness and to point out that tuberculosis is still an epidemic in many countries around the world, mostly in developing countries . The date commemorates the day on which Robert Koch announced in 1882 that he had discovered the causative agent of tuberculosis.
literature
19th century
- August Predöhl: The history of tuberculosis. Leipzig 1888; Reprint: Sendet, Wiesbaden 1966.
20th century
- ML Holbrook: The prevention, hygienic treatment and cure of pulmonary consumption. Concord, Munich 1900. (digitized version)
- Erich Stern : The psyche of the lung patient. The Influence of Pulmonary Tuberculosis and Sanatorium Life on the Soul of the Sick. Halle on the Saale in 1925.
- Kurt Lydtin: Pulmonary tuberculosis as an indication area. In: Reichsärztekammer (Ed.): Guidelines for the termination of pregnancy and sterility for health reasons. Edited by Hans Stadler. J. F. Lehmanns Verlag, Munich 1936, pp. 58-79.
- Norman Meachen: A short history of tuberculosis. London 1936; Reprint New York 1978.
- Richard Bochalli : The History of Consumption . Leipzig 1940.
- Wilhelm Roloff : The pulmonary tuberculosis. Springer, Berlin / Göttingen / Heidelberg 1948.
- Wilhelm Roloff: The tuberculosis lexicon. 2nd Edition. Thieme, Stuttgart 1949.
- Walter Schaich: Tuberculosis. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition, ibid. 1961, pp. 224-308.
- Paul-Georg Schmidt: Pulmonary tuberculosis - diagnosis and therapy. Georg Thieme Verlag, Stuttgart, 3. Edition 1956
- Michel Oury: History of Tuberculosis. In: Illustrated History of Medicine. German adaptation by Richard Toellner , Salzburg 1980–1982 and as a special edition there in 1986, Volume V, pp. 2734–2755.
Recent literature
- T. Schaberg, T. Bauer, F. Brinkmann et al .: S2k guideline: Tuberculosis in adulthood. In: Pneumology. Volume 71, 2017, pp. 325-397.
- German Society for Pediatric Infectious Diseases V. (DGPI) (Ed.): Handbook infections in children and adolescents. 4th edition. Futuramed, Munich 2003, ISBN 3-923599-90-0 .
- Werner E. Gerabek : pulmonary tuberculosis. In: Werner E. Gerabek, Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (Eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , pp. 871 f.
- Juan Carlos Palomino, Sylvia Leão, Viviana Ritacco and others: Tuberculosis 2007. From basic science to patient care. (PDF; 8.3 MB) TuberculosisTextbook.com, winner of the Amedeo Textbook Award (English), well-illustrated overview
- Peter D. Davies, Peter Barnes, Stephen B. Gordon: Clinical Tuberculosis. Hodder Arnold Publishers, 2008, ISBN 978-0-340-94840-8 .
- Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , pp. 238–245.
- German Society for Pneumology and Respiratory Medicine (Ed.): 100 Years of German Pneumology. Springer, Berlin / Heidelberg 2010, ISBN 978-3-642-11453-3 .
- Christine Wolters: Tuberculosis and Human Attempts in National Socialism. The network behind the TB experiments in the Sachsenhausen concentration camp. Steiner, Stuttgart 2011, ISBN 978-3-515-09399-6 .
- Jörg Braun: Infectious Diseases. In: Jörg Braun, Roland Preuss (Ed.): Clinical Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 437-519, here: pp. 462 f. ( Tuberculosis ).
- Ulrike Moser: Consumption. Another German social history. Matthes and Seitz, Berlin 2018, ISBN 978-3-95757-556-2 .
Articles in magazines
- Hans Gertler: History of the diagnosis and therapy of tuberculosis. In: Medical Monthly Bulletin 11, 1957, pp. 386-388.
- American Thoracic Society: Diagnostic Standards and Classification of Tuberculosis in Adults and Children. In: American journal of respiratory and critical care medicine. No. 161, 2000, pp. 1376-1395. PMID 10764337
- Flurin Condrau : treatment without cure. On the social construction of treatment success for tuberculosis in the early 20th century. In: Medicine, Society and History. Volume 19, 2000, pp. 71-94.
- B. Hauer, D. Rohde, R. Loddenkemper: Tuberculosis. In: The pulmonologist. No. 4, Heidelberg 2005, pp. 291-306, ISSN 1613-5636
- Horst Kremling : Historical considerations on preventive medicine. In: Würzburg medical history reports. 24, 2005, pp. 222-260, here pp. 225-227.
- Peter-Philipp Schmitt: Pathogen behind barbed wire. In: Frankfurter Allgemeine Zeitung . April 13, 2007, p. 9.
- S. Ahmad: Pathogenesis, immunology, and diagnosis of latent Mycobacterium tuberculosis infection . In: Clinical and Developmental Immunology . Vol. 2011, 2011, pp. 814943 , doi : 10.1155 / 2011/814943 , PMID 21234341 , PMC 3017943 (free full text).
- K. Luong, LT Nguyen: Impact of vitamin D in the treatment of tuberculosis. In: The American journal of the medical sciences. Volume 341, No. 6, June 2011, pp. 493-498. doi: 10.1097 / MAJ.0b013e3182070f47 , PMID 21289501 . (Review).
- SH Kaufmann: Fact and fiction in tuberculosis vaccine research: 10 years later. In: The Lancet Infectious Diseases . Volume 11, No. 8, August 2011, pp. 633-640. doi: 10.1016 / S1473-3099 (11) 70146-3 , PMID 21798463 . (Review).
- M. Möller, EG Hoal: Current findings, challenges and novel approaches in human genetic susceptibility to tuberculosis. In: Tuberculosis. Volume 90, No. 2, March 2010, pp. 71-83. doi: 10.1016 / j.tube.2010.02.002 , PMID 20206579 . (Review).
- Thaddäus Zajaczkowski : Genitourinary tuberculosis: historical and basic science review: past and present. In: Central European Journal of Urology, 65, 2012, pp. 182-187.
- Urs Ehehalt: Tbc - common worldwide. In: Hamburger Ärzteblatt, 10/2014, pp. 12–15.
- Rüdiger Döhler , Loukas Konstantinou: Skeletal tuberculosis - one of the oldest diseases of mankind. In: Chirurgische Allgemeine , Volume 16, Issue 10 (2015), pp. 556–558.
- Isabelle Suárez et al .: Diagnosis and therapy of tuberculosis. In: Deutsche Ärzteblatt. Volume 116, Issue 43, October 25, 2019, pp. 729-735.
Broadcast report
- Claudia Doyle, Mathias Tertilt: The fight against tuberculosis in India - "We will end the epidemic" , Deutschlandfunk - Science in focus from February 11, 2018
Web links
- Tuberculosis - Information from the Robert Koch Institute
- Website of the National Reference Center for Mycobacteria at the Borstel Research Center
- Site of the German Central Committee for Combating Tuberculosis
- Images of tuberculosis cutis luposa changes in DermIS
- Images of tuberculosis cutis verrucosa changes in DermIS
- Images of Tuberculosis Primaria Cutis Changes in DermIS
- Tb-specific side. WHO Regional Office for Europe
- stoptb.org - Initiative Stop the TB (English) accessed on November 8, 2009
- Tuberculosis in Europe and North America, 1800-1922. Harvard University Library, Open Collections Program, Contagion, Historical Views of Diseases and Epidemics
- German Leprosy and Tuberculosis Aid e. V.
- Competence Center Tuberculosis (Switzerland)
- German Lung Foundation
- Detailed information on tuberculosis in HIV patients
- Tuberculosis. Lungeninformationsdienst.de
- Journal inventory of the German Tuberculosis Archives (2009). (PDF)
- Carola Otterstedt: The children of Scheidegg. (Reports from a children's sanatorium for pulmonary and bone tuberculosis, documentation).
- Tuberculosis - Information from the Federal Office of Public Health (Switzerland)
Remarks
- ↑ Tuberculosis is considered an AIDS-defining disease. Jörg Braun (2016), p. 462.
- ↑ Global tuberculosis report 2016. (PDF) WHO , p. 1 , accessed on June 11, 2017 .
- ↑ Did immigrants bring the “White Death” to us? News.de from November 10, 2015.
- ↑ Max Höfler: German disease names book. Munich 1899, pp. 93 and 99.
- ↑ Matthias Kreienkamp: The St. Georgen Rezeptar. An Alemannic pharmacopoeia of the 14th century from the Karlsruhe Codex St. Georgen 73 , Part II: Commentary (A) and textual comparison, Medical Dissertation Würzburg 1992, p. 68 f.
- ↑ JT Lejeune, PJ Rajala-Schultz: Food safety: unpasteurized milk: a continued public health threat. In: Clinical Infectious Diseases . Volume 48, Number 1, January 2009, pp. 93-100. doi: 10.1086 / 595007 . PMID 19053805 . (Review).
- ↑ Fact sheet tuberculosis. WHO, as of October 2019; accessed on December 31, 2019.
- ↑ V. Bordignon, p Bultrini u a. .: High prevalence of latent tuberculosis infection in autoimmune disorders: such as psoriasis and in chronic respiratory diseases, Including lung cancer. In: Journal of biological regulators and homeostatic agents. Volume 25, No. 2, Apr-Jun 2011, pp. 213-220. PMID 21880210 .
- ^ Report on the epidemiology of tuberculosis in Germany for 2016. (PDF) (No longer available online.) Robert Koch Institute , 2018, p. 112 , formerly in the original ; accessed on March 26, 2018 . ( Page no longer available , search in web archives ) Info: The link was automatically marked as defective. Please check the link according to the instructions and then remove this notice.
- ↑ Federal Gazette N ° 27, July 10, 1947 (information for 1940)
- ↑ HP Pöhn, G. Rasch: Statistics of reportable diseases. BGA Schriften 5/1993, MMV Verlag, Munich, 1004.
- ^ Robert Koch Institute : Archive of reports on the epidemiology of tuberculosis in Germany (since 2001). Retrieved November 13, 2011 .
- ↑ a b c tuberculosis. RKI guide for doctors. Robert Koch Institute , accessed November 13, 2011 .
- ↑ RKI report on the epidemiology of tuberculosis in Germany for 2011. (PDF) Robert Koch Institute , accessed on March 18, 2013 .
- ↑ No all-clear for tuberculosis. In: Deutsches Ärzteblatt, March 18, 2013.
- ↑ Epidemiological Bulletin of the RKI No. 3/2020 (PDF) January 16, 2020
- ↑ A. Koul et al .: The challenge of new drug discovery for tuberculosis . In: Nature . tape 469 , no. 7331 , 2011, pp. 483-490 , PMID 21270886 .
- ^ R. Riley: Aerial dissemination of pulmonary tuberculosis . In: Am Rev Tuberc . tape 76 , no. 5980 , 1957, pp. 931-941 , PMID 13488004 .
- ↑ a b German Society for Pediatric Infectious Diseases V. (DGPI) (Ed.): Handbook infections in children and adolescents. 4th edition. Futuramed, Munich 2003, ISBN 3-923599-90-0 .
- ^ Walter Schaich: The tuberculosis. 1961, p. 282 ( The tuberculoma of the lungs. ).
- ↑ JL Flynn, MM Goldstein, J. Chan et al .: Tumor necrosis factor-alpha is required in the protective immune response against Mycobacterium tuberculosis in mice . In: Immunity . tape 2 , no. 6 , June 1995, pp. 561-572 , PMID 7540941 .
- ^ ST Cole et al .: Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. In: Nature . No. 393, London 1998, pp. 537-554. PMID 9634230 .
- ↑ Walter Schaich: The tuberculosis. 1961, pp. 251-254.
- ↑ a b T. Ulrichs et al .: Immunology of tuberculosis and new vaccine approaches. In: Monthly Pediatrics. No. 154, Springer, Berlin 2006, ISSN 0026-9298 , pp. 132-141.
- ^ Walter Schaich: The tuberculosis. 1961, p. 233 f. And 265 f.
- ↑ Berthold Jany, Tobias Welte: Pleural effusion in adults - causes, diagnosis and therapy. In: Deutsches Ärzteblatt. Volume 116, No. 21, (May) 2019, pp. 377-385, here: pp. 379-383.
- ↑ a b c K. Magdorf: Tuberculosis in childhood. Pathogenesis, Prevention, Clinic and Therapy. In: Monthly Pediatrics. No. 154, Springer, Berlin 2006, ISSN 0026-9298 , pp. 124-132.
- ↑ Karl Wurm, AM Walter: Infectious Diseases. 1961, p. 131.
- ↑ Karl Wurm, AM Walter: Infectious Diseases. 1961, p. 131.
- ^ Walter Schaich: The tuberculosis. 1961, p. 281 f.
- ↑ Ludwig Heilmeyer , Wolfgang Müller: The rheumatic diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition, ibid. 1961, pp. 309-351, here: p. 322.
- ^ A. Poncet: Polyarthrite tuberculeuse simulant des lésions rhumatismales chroniques déformantes. In: Gaz. Hôp. Volume 70, (Paris) 1897, p. 1219.
- ↑ Barbara I. Tshisuaka: Poncet, Antonin. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1175.
- ^ Walter Schaich: The tuberculosis. 1961, pp. 286-289.
- ↑ Gerald Metz: The archive of the Würzburg University Clinic for Skin and Venereal Diseases and its holdings. In: Würzburg medical history reports. Volume 9, 1991, pp. 37-55, here: pp. 47, 50.
- ↑ Walter Schaich: The tuberculosis. 1961, p. 291 f.
- ↑ S. Jodra, C. Alvarez: Images in clinical medicine. Pott's disease of the thoracic spine. In: N Engl J Med. 368 (8), 2013, p. 756. doi: 10.1056 / NEJMicm1207442 . PMID 23425168 .
- ↑ Rüdiger Döhler, Loukas Konstantinou: The skeletal tuberculosis - one of the oldest diseases of mankind. In: Surgical General. Volume 16, Issue 10 (2015), pp. 556–558.
- ^ Walter Schaich: The tuberculosis. 1961, pp. 283-285.
- ↑ Walter Schaich: The tuberculosis. 1961, p. 289 f.
- ↑ A. Müller, RW Schlecht, Alexander Früh, H. Still The way to health: A faithful and indispensable guide for the healthy and the sick. 2 volumes, (1901; 3rd edition 1906, 9th edition 1921) 31st to 44th edition. CA Weller, Berlin 1929 to 1931, Volume 2 (1929), p. 266 f.
- ↑ Walter Schaich: The tuberculosis. 1961, p. 285 f.
- ↑ Ravikran Orgole: Textbook of Oral Medicine, Oral Diagnosis and Oral Radiology, Elsevier Health Services, 2014, p. 215.
- ↑ a b A. Detjen et al .: Immunological diagnosis of tuberculosis - interferon-γ tests. In: Monthly Pediatrics. No. 154, Springer, Berlin 2006, ISSN 0026-9298 , pp. 152-159.
- ↑ DD Singh, M. Vogel et al .: TB or not TB? Difficulties in the diagnosis of tuberculosis in HIV-negative immigrants to Germany. In: European journal of medical research. Volume 16, No. 9, Sept. 2011, pp. 381-384. PMID 22024436 .
- ↑ Recommended action for dealing with patients with suspected tuberculosis of the GPR
- ↑ HJ Zar et al .: Induced sputum versus gastric lavage for microbiological confirmation of pulmonary tuberculosis in infants and young children, a prospective study. In: The Lancet. Vol. 365, No. 9454, London 2005, pp. 130-134. PMID 15639294 .
- ↑ M. Pwiwitzer et al .: False-positive interferon-γ test? In: Pneumology. 2007.
- ↑ Nina Pollock et al .: Screening Health Care Workers with Quantiferon-Gold: Possible False Negative Results in Individuals with High Pre-Test Probability of Latent Tuberculosis Infection. In: Chest. 2007.
- ↑ Matthew PR Berry, Christine M. Graham, Finlay W. McNab, Zhaohui Xu, Susannah AA Bloch et al .: An interferon-inducible neutrophil-driven blood transcriptional signature in human tuberculosis. In: Nature. Vol. 466, August 19, 2010, pp. 973-977 ( abstract as html ).
- ↑ J. van Ingen, RE Aarnoutse et al .: Why Do We Use 600 mg of Rifampicin in Tuberculosis Treatment? In: Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. Volume 52, No. 9, May 2011, pp. E194 – e199. doi: 10.1093 / cid / cir184 , PMID 21467012 (review).
- ↑ R. Tasneen, SY Li u a. .: Sterilizing activity of novel TMC207- and PA-824-containing regimens in a murine model of tuberculosis. In: Antimicrobial Agents and Chemotherapy . Volume 55, No. 12, Dec. 2011, pp. 5485-5492. doi: 10.1128 / AAC.05293-11 . PMID 21930883 . PMC 3232786 (free full text).
- ↑ Tuberculosis - Leaflet for Doctors. ( Memento from September 29, 2007 in the Internet Archive ) Robert Koch Institute
- ↑ Marianne Abele-Horn (2009), p. 239.
- ↑ M. Lee, J. Lee et al .: Linezolid for treatment of chronic extensively drug-resistant tuberculosis. In: The New England Journal of Medicine . Volume 367, Number 16, October 2012, pp. 1508-1518. doi: 10.1056 / NEJMoa1201964 . PMID 23075177 . PMC 3814175 (free full text).
- ↑ S. Heinzl: Antibiotic therapy of tuberculosis: Linezolid for highly resistant pathogens. In: Dtsch Arztebl. 109 (49), 2012, pp. A-2467 / B-2020 / C-1976.
- ^ FDA advisory panel backs J&J TB drug , Reuters, November 29, 2012.
- ↑ K. Williams, A. Minkowski et al .: Sterilizing activities of novel combinations lacking first- and second-line drugs in a murine model of tuberculosis. In: Antimicrobial agents and chemotherapy. Volume 56, Number 6, June 2012, pp. 3114-3120. doi: 10.1128 / AAC.00384-12 . PMID 22470112 . PMC 3370712 (free full text).
- ↑ Summary of the European public assessment report (EPAR) for Sirturo - Bedaquiline , EPAR of the EMA, accessed on April 7, 2014.
- ↑ a b World TB Day - three new medicines recommended in last six months for patients with multidrug-resistant tuberculosis , EMA report on World TB Day on March 21, 2014, accessed on April 7, 2014.
- ↑ Deltyba - Delamanid , EMA notification on the occasion of the positive vote by the CHMP on November 21, 2013, accessed on April 7, 2014.
- ↑ Para-aminosalicylic acid Lucane , EMA notification on the occasion of the positive vote by the CHMP on November 21, 2013, accessed on April 7, 2014.
- ↑ Summary of the European public assessment report (EPAR) for Deltyba delamanid , EPAR of the EMA, accessed on May 22, 2014.
- ↑ Summary of the European public assessment report (EPAR) for Para-aminosalicylic acid Lucane , EPAR of the EMA, accessed on May 22, 2014.
- ↑ S. Yaldiz, S. Gursoy et al .: Surgery offers high cure rates in multidrug-resistant tuberculosis. In: Ann Thorac Cardiovasc Surg. Volume 17, No. 2, April 2011, pp. 143-147. PMID 21597410 .
- ↑ L. Amaral, A. Martins, G. Spengler, A. Hunyadi, J. Molnar: The Mechanism by which the Phenothiazine Thioridazine Contributes to Cure Problematic Drug-Resistant Forms of Pulmonary Tuberculosis: Recent Patents for "New Use". In: Recent patents on anti-infective drug discovery. [Electronic publication before printing] December 2013, PMID 24320229 .
- ↑ L. Amaral, M. Viveiros: Why thioridazine in combination with antibiotics cures extensively drug-resistant Mycobacterium tuberculosis infections. In: International journal of antimicrobial agents. Volume 39, Number 5, May 2012, pp. 376-380. doi: 10.1016 / j.ijantimicag.2012.01.012 . PMID 22445204 .
- ↑ S. Sharma, A. Singh: Phenothiazines as anti-tubercular agents: mechanistic insights and clinical implications. In: Expert opinion on investigational drugs. Volume 20, Number 12, December 2011, pp. 1665-1676. doi: 10.1517 / 13543784.2011.628657 . PMID 22014039 .
- ↑ K. Magdorf et al .: Tuberculosis. In: Pediatric Guidelines. Munich 2006, ISBN 3-437-22060-8 .
- ↑ T. Schön, J. Idh et al .: Effects of a food supplement rich in arginine in patients with smear positive pulmonary tuberculosis - a randomized trial. In: Tuberculosis. Volume 91, Number 5, September 2011, pp. 370-377. doi: 10.1016 / j.tube.2011.06.002 . PMID 21813328 .
- ^ AP Ralph, PM Kelly, NM Anstey: L-arginine and vitamin D: novel adjunctive immunotherapies in tuberculosis . In: Trends Microbiol. tape 16 , no. 7 , July 2008, p. 336-344 , doi : 10.1016 / j.tim.2008.04.003 , PMID 18513971 .
- ^ LT Ho-Pham, ND Nguyen, TT Nguyen et al .: Association between vitamin D insufficiency and tuberculosis in a Vietnamese population . In: BMC Infect. Dis . tape 10 , 2010, p. 306 , doi : 10.1186 / 1471-2334-10-306 , PMID 20973965 , PMC 2978214 (free full text).
- ↑ M. Fabri, S. Stenger et al .: Vitamin D is required for IFN-gamma-mediated antimicrobial activity of human macrophages. In: Science Translational Medicine . Volume 3, number 104, October 2011, p. 104ra102. doi: 10.1126 / scitranslmed.3003045 . PMID 21998409 . PMC 3269210 (free full text).
- ↑ Tuberculosis: Vitamin D accelerates the antibiotic action. In: Deutsches Ärzteblatt. 5th September 2012.
- ↑ AK Coussens, RJ Wilkinson u a. .: Vitamin D ACCELERATES resolution of inflammatory responses during tuberculosis treatment. In: Proceedings of the National Academy of Sciences . Volume 109, Number 38, September 2012, pp. 15449-15454. doi: 10.1073 / pnas.1200072109 . PMID 22949664 . PMC 3458393 (free full text).
- ↑ S. Subbian, L. Tsenova et al .: Phosphodiesterase-4 inhibition alters gene expression and improves isoniazid-mediated clearance of Mycobacterium tuberculosis in rabbit lungs. In: PLOS Pathogens . Volume 7, number 9, September 2011, p. E1002262. doi: 10.1371 / journal.ppat.1002262 . PMID 21949656 . PMC 3174258 (free full text).
- ↑ KJ Welsh, SA Hwang et al .: Lactoferrin modulation of mycobacterial cord factor trehalose 6-6'-dimycolate induced granulomatous response. In: Translational research: the journal of laboratory and clinical medicine. Volume 156, Number 4, October 2010, pp. 207-215. doi: 10.1016 / j.trsl.2010.06.001 . PMID 20875896 . PMC 2948024 (free full text).
- ^ McGill University: The Online TST / IGRA Interpreter. Retrieved March 24, 2014 .
- ^ P. Andersen, TM Doherty: The success and failure of BCG - implications for a novel tuberculosis vaccine. In: Nature reviews. Microbiology. Volume 3, No. 8, August 2005, pp. 656-662. doi: 10.1038 / nrmicro1211 , PMID 16012514 . (Review).
- ^ BCG: bad news from India. In: Lancet. Volume 1, Number 8159, January 1980, pp. 73-74. PMID 6101419 .
- ↑ L. Grode, CA Ganoza, C. Brohm, J. Weiner, B. Eisele, SH Kaufmann: Safety and immunogenicity of the recombinant BCG vaccine VPM1002 in a phase 1 open-label randomized clinical trial . In: Vaccine . 2012, doi : 10.1016 / j.vaccine.2012.12.053 , PMID 23290835 .
- ↑ MPG: Vaccine candidate against tuberculosis in phase II / III study
- ↑ MD Tameris, M. Hatherill, BS Landry, TJ Scriba, MA Snowden, S. Lockhart, JE Shea, JB McClain, GD Hussey, WA Hanekom, H. Mahomed, H. McShane: Safety and efficacy of MVA85A, a new tuberculosis vaccine, in infants previously vaccinated with BCG: a randomized, placebo-controlled phase 2b trial. In: The Lancet. doi: 10.1016 / S0140-6736 (13) 60177-4 .
- ↑ Aeras Developing new tuberculosis vaccines for the world
- ↑ JC Lorenzi, AP Trombone, CD Rocha et al .: Intranasal vaccination with messenger RNA as a new approach in gene therapy: use against tuberculosis . In: BMC Biotechnol . tape 10 , 2010, p. 77 , doi : 10.1186 / 1472-6750-10-77 , PMID 20961459 , PMC 2972232 (free full text).
- ↑ Elisa Nemes, Hennie Geldenhuys, Virginie Rozot, Kathryn T. Rutkowski, Frances Ratangee: Prevention of M. tuberculosis Infection with H4: IC31 Vaccine or BCG Revaccination . In: New England Journal of Medicine . July 11, 2018, doi : 10.1056 / NEJMoa1714021 , PMID 29996082 , PMC 5937161 (free full text) - ( nejm.org [accessed December 21, 2018]).
- ↑ JT Belisle, VD Vissa, T Sievert, K Takayama, PJ Brennan, GS Besra: Role of the major antigen of Mycobacterium tuberculosis in cell wall biogenesis. In: Science . tape 276 , 1997, pp. 1420-1422 .
- ^ Tuberculosis: RKI-Ratgeber. Reporting obligation according to IfSG. In: rki.de. Robert Koch Institute, February 21, 2013, accessed on March 15, 2020 .
- ^ Tuberculosis: RKI-Ratgeber. Notification obligation according to IfSG. In: rki.de. Robert Koch Institute, February 21, 2013, accessed on March 15, 2020 .
- ↑ a b Notifiable animal diseases. Federal Ministry of Food and Agriculture (BMEL), August 2, 2019, accessed on March 16, 2020 .
- ↑ Notifiable animal diseases. Federal Ministry of Food and Agriculture (BMEL), August 2, 2019, accessed on March 14, 2020 .
- ↑ Entire legal regulation of the Tuberculosis Act in the currently valid version.
- ↑ The Swiss Federal Council: Animal Disease Ordinance (TSV). In: admin.ch. Retrieved on March 16, 2020 (Swiss Standard German, from June 27, 1995 (as of January 1, 2020)).
- ↑ Tuberculosis in animals and humans. Federal Food Safety and Veterinary Office FSVO, March 10, 2010, accessed on March 16, 2020 (Swiss Standard German): “Tuberculosis is an animal disease that must be eradicated and therefore notifiable. Anyone who keeps or looks after animals must report suspected cases to the herd veterinarian. [...] "
- ^ TA Gous, MC Williams: The pathology of tuberculosis caused by Mycobacterium tuberculosis in a herd of semi-free-ranging springbok (Antidorcas marsupialis) . In: Onderstepoort J. Vet. Res. Band 76 , no. 4 , December 2009, p. 419-441 , PMID 21344792 .
- ^ R. Murphree, JV Warkentin et al .: Elephant-to-human transmission of tuberculosis, 2009. In: Emerging Infectious Diseases . Volume 17, No. 3, March 2011, pp. 366-371. PMID 21392425 .
- ↑ Ordinance on notifiable animal diseases in the version published on July 19, 2011 ( Federal Law Gazette I p. 1404 ), amended by Article 3 of the Ordinance of May 3, 2016 ( Federal Law Gazette I p. 1057 )
- ↑ Notifiable animal diseases on the website of the Federal Ministry of Food and Agriculture, accessed on March 19, 2020
- ↑ Annex to § 1 of the Ordinance on Notifiable Animal Diseases (TKrMeldpflV) in the version of the announcement of February 11, 2011 ( Federal Law Gazette I p. 252 ), last amended by Article 381 of the Ordinance of August 31, 2015 ( Federal Law Gazette I p. 1474 )
- ↑ Chemical and Veterinary Investigation Office (CVUA) Stuttgart: Pseudotuberculosis (Corynebacterium pseudotuberculosis) infections are on the rise.
- ↑ J. Kappelman, MC Alçiçek et al .: First Homo erectus from Turkey and implications for migrations into temperate Eurasia. In: American journal of physical anthropology. Volume 135, No. 1, January 2008, pp. 110-116. doi: 10.1002 / ajpa.20739 , PMID 18067194 .
- ↑ Stefan Weller: Oldest evidence of tuberculosis in humans? Universitätsmedizin Göttingen - Georg-August-Universität, press release from April 23, 2012 at the Informationsdienst Wissenschaft (idw-online.de), accessed on December 20, 2014.
- ↑ I. Hershkovitz, HD Donoghue et al .: Detection and molecular characterization of 9,000-year-old Mycobacterium tuberculosis from a Neolithic settlement in the Eastern Mediterranean. In: PloS one. Volume 3, No. 10, 2008, p. E3426. doi: 10.1371 / journal.pone.0003426 , PMID 18923677 . PMC 2565837 (free full text).
- ↑ Bruce M. Rothschild, Larry D. Martin, Galit Lev, Helen Bercovier, Gila Kahila Bar-Gal, Charles Greenblatt, Helen Donoghue, Mark Spigelman, David Brittain: Mycobacterium tuberculosis Complex DNA from an Extinct Bison Dated 17,000 Years before the Present. In: Clin Infect Dis. 33 (3), 2001, pp. 305-311. doi: 10.1086 / 321886 .
- ↑ Evert Dirk Baumann : De phthisi antiqua. In: Janus 34, 1930, pp. 209-225 and 253-272.
- ↑ Hippocrates: Epidemics.
- ↑ Walter von Brunn : Paracelsus and his theory of consumption. Leipzig 1941.
- ↑ Martin Risch: Cause of death statistics of the community Triesen from 1831 to 1930 . In: Yearbook of the Historical Association for the Principality of Liechtenstein . tape 36 , 1936, pp. 54 .
- ↑ Christoph Weißer: Thorax surgery. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1397.
- ↑ On the collapse therapy of pulmonary tuberculosis see also Walter Schaich: Die Tuberkulose. 1961, pp. 305-307.
- ↑ Barbara I. Tshisuaka: Tuffier, Théodore. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1424.
- ↑ Albrecht Scholz: Lupus vulgaris. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 872 f., Here: p. 873.
- ^ Ferdinand Sauerbruch, Hans Rudolf Berndorff : That was my life. Kindler & Schiermeyer, Bad Wörishofen 1951; cited: Licensed edition for Bertelsmann Lesering, Gütersloh 1956, pp. 180–286.
- ↑ Cf. on the activities of the municipalities collection of sources on the history of German social policy 1867 to 1914 , III. Department: Expansion and Differentiation of Social Policy since the Beginning of the New Course (1890–1904), Volume 7, Poor Care and Communal Welfare Policy , edited by Wilfried Rudloff, Darmstadt 2016.
- ↑ Md Abdul Kuddus, Emma S. McBryde, Oyelola A. Adegboye: Delay effect and burden of weather-related tuberculosis cases province in Rajshahi, Bangladesh, 2007-2012 . In: Scientific Reports . tape 9 , no. 1 , September 3, 2019, ISSN 2045-2322 , p. 12720 , doi : 10.1038 / s41598-019-49135-8 ( nature.com [accessed September 19, 2020]).
- ↑ tb-archiv.de
- ↑ Eckart Roloff , Karin Henke-Wendt: Old illness with new problems. (The German Tuberculosis Archive and Museum) In: Visit your doctor or pharmacist. A tour through Germany's museums for medicine and pharmacy. Volume 2: Southern Germany. Verlag S. Hirzel, Stuttgart 2015, ISBN 978-3-7776-2511-9 , pp. 51-53.
- ↑ Stop TB Partnership. The missed three million. Report on World Tuberculosis Day on March 24, 2014; Retrieved April 8, 2014.