Ebola fever epidemic 2014 to 2016
The Ebola fever epidemic , which broke out in several West African countries in 2014 and was declared over at the beginning of 2016 , is considered to be the largest of its kind to date (as of June 2019) in terms of the number of diseases and deaths recorded since the discovery of the Ebola virus in 1976.
According to the World Health Organization affected during the epidemic - including the suspected cases - 28,639 people in Ebola fever , of whom died 11,316. The determination of these case numbers , which are based on reports from the health authorities of the countries concerned, may be a. not secured due to insufficient laboratory capacities, so that the WHO assumes a significantly higher number of unreported cases. The reported new infections doubled in the first 9 months about every three to four weeks, remained at a high level with large regional fluctuations in the last quarter of 2014 and fell significantly at the turn of the year. An examination of selected cases, in which the clinical course is documented, showed that in the first nine months after the outbreak of the epidemic (as of September 14, 2014) around 71% of those clearly affected by the disease died.
The epidemic began in southeast Guinea at the beginning of 2014 (index case December 2013) and was officially announced in March. In the months that followed, further illnesses were reported in the neighboring countries of Sierra Leone and Liberia , including in Nigeria at the beginning of August . The first cases occurred on August 29 in Senegal and on October 24 in Mali . At the end of September 2014, the first case of Ebola outside Africa was detected in the USA . The first confirmed infection in Spain followed on October 6 and in the United Kingdom on December 29, 2014 . The Ebola fever outbreak in the Democratic Republic of the Congo , which became known at the end of August 2014, had no direct epidemiological connection with the Ebola fever cases in West Africa.
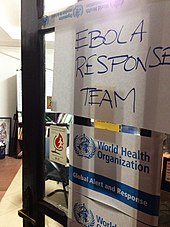
Because of the epidemic, Liberia and Sierra Leone first declared a state of emergency , and on August 8, 2014 Nigeria too. The borders between the states were closed and international traffic was partially restricted due to travel warnings . On the same day, the WHO declared the epidemic after consultation of the appropriate emergency committee to " public health emergency of international importance " ( Public Health Emergency of International Concern , PHEIC ). On August 12, 2014, the World Health Organization declared the use of experimental but not yet approved active ingredients to fight the epidemic to be ethically justifiable. On September 18, 2014 gave UN Secretary General Ban Ki-moon in the UN Security Council , the UN mission UNMEER known which is intended to make emergency response in affected by the epidemic.
The WHO declared the epidemic ended on October 17, 2014 for Senegal, October 20, 2014 for Nigeria and December 2, 2014 for Spain. Since December 24, 2014, the USA, since January 19, 2015, Mali and since March 7, 2015, the United Kingdom have been free of Ebola. From January 2015, the situation eased in Liberia, which was declared Ebola-free on May 9, 2015 as the first of the three most affected countries. On June 29, it was announced that there had been another Ebola death in Liberia on June 24. In Guinea and Sierra Leone, the epidemic continued to spread, at least regionally. On January 14, 2016, the epidemic in the last affected country, Liberia, was declared over. However, a new infection occurred in Sierra Leone the very next day. In mid-March 2016, shortly after the WHO declared West Africa free of ebola for the second time, new diseases and suspected cases also appeared in Guinea. The last time Liberia was declared ebola-free on June 9, 2016.
The severity of the epidemic was initially attributed to the first occurrence of the disease in this part of the continent. The lack of medical infrastructure after a long period of civil war also contributed to the course. Eventually it was revealed that the virus had been detected in Liberia for the late 1970s as early as the early 1980s, especially in forest areas on the border with Guinea, but the risk of hemorrhagic fever was ignored due to HIV and civil war.
Characterization of the virus variant
At the end of March 2014, the first sequence data from parts of the viral genome showed that the outbreak was caused by a variant of the virus species Zaire Ebolavirus (EBOV) of the genus Ebolavirus . These first data from the Pasteur Institute were based on partial sequences of the L gene that codes for the viral RNA polymerase .
A study from April 2014 showed with a high probability that the epidemic (excluding the outbreak in DR Congo ) of a single human infection spread in December 2013. Using the phylogenetic analysis of a first complete sequencing of the virus from 20 patient isolates, the study also showed that it was a separate cluster within the clade of virus species: It differed significantly from the clusters of the isolates from previous outbreaks in Gabon and the Democratic Republic of the Congo (formerly Zaire ) are known.
Further investigation suggested that it was a lineage of EBOV that had spread from central Africa to Guinea and West Africa over the past few decades and was not a deviant and endemic virus. The estimated split of the line that caused the outbreak from the Central African line that caused the outbreaks in Congo and Gabon occurred around 2002. When and how the virus variant got to West Africa could be without further gene sequencing, especially from the animal ones Reservoir hosts , not to be named.
A study on the determination of the family tree by means of a molecular clock confirmed the affiliation of the outbreak variant to the Central African line and concluded that the lines were separated around 1999 or 2001.
The variants of the Zaire Ebola virus identified so far are characterized by a high mortality rate, see below.
Propagation dynamics
overview
| country | Cases of illness |
Deaths |
|---|---|---|
|
|
14,124 * | 3,956 * |
|
|
10,675 * | 4,809 * |
|
|
3,804 * | 2,536 * |
|
|
20th | 8th |
|
|
8th* | 6 * |
|
|
4th | 1 |
|
|
1 | 0 |
|
|
1 | 0 |
|
|
1 | 0 |
|
|
1 | 0 |
| All in all | 28,639 | 11,316 |
| As of March 13, 2016, published March 16, 2016 * Confirmed, probable and suspected cases. |
||
The figures presented here are based on WHO publications in the context of the Situation Reports . The table shows all cases of the disease since the outbreak began. In this form, the number of cases does not allow any statement about the current sick leave. Since the middle of September, the WHO reports have pointed to the low reliability of the data from the countries concerned (especially Liberia). Since October the Situation Reports have contained a comment that the reported numbers are to be regarded as too low (“ EVD cases are under-reported ”). The Centers for Disease Control and Prevention (CDC) named a correction factor of 2.5. (For the collection of the numbers, unreported numbers, number of cases, see details in the section Determining the number of cases .)
In the course of 2014, around 20,200 people were infected and around 7,900 died.
The epidemic was declared over in Senegal on October 17, 2014 and in Nigeria on October 20. This after a period of 21 days without re-infection and monitoring of the identified contact persons of infected people. The same thing happened for Spain on December 2, 2014. On December 24, 2014, the United States was designated by the WHO as previously affected ( previously affected countries ) and the epidemic was declared over there. A 42-day period was then introduced: a country is now considered free of Ebola if 42 days have passed since the last case (died or tested twice negative) and all contacts have been followed up. On January 19, 2015, Mali was declared free of Ebola virus disease after this deadline . In the UK, the 42-day period expired on March 7, 2015 after the only patient was discharged as cured on January 23. The last country affected was Liberia: Here the epidemic was declared over on January 14, 2016, which prompted the WHO to officially declare the entire Ebola fever epidemic in West Africa to be over about two years after it broke out. Just one day later, a death in Sierra Leone was confirmed as a new Ebola case.
West Africa
The three main affected states have the following population figures:
- Guinea: 11,474,000 (July 2014 estimate)
- Liberia: 4,092,000 (July 2014 estimate)
- Sierra Leone: 5,744,000 (July 2014 estimate)
A total of over 21 million people live in these three countries.
Guinea

The Ministry of Health of Guinea informed on 23 March 2014, the WHO officially by an outbreak of Ebola fever . After on-site epidemiological research, a first case of infection was retrospectively identified in Guinea in December 2013. It was a two-year-old boy from Méliandou who died of complications from the disease on December 28th. Up to March 22nd, 49 cases of illness (including 29 deaths) were recorded in southeastern forest areas of Guinea. The diseases were limited to the prefectures of Guéckédou , Macenta and Nzérékoré within the Nzérékoré region and to the Kissidougou prefecture within the Faranah region , two of these prefectures border on Sierra Leone and Liberia, respectively. Further suspected cases and deaths from the capital Conakry were still being investigated at the time. Four medical workers were among the dead. On March 25, 2014, the Guinean Ministry of Health announced that the suspected cases in Conakry had been found virologically negative, but confirmed cases and deaths were also reported in Conakry shortly afterwards. At the Pasteur Institute in Lyon , the Ebola virus was detected directly in six of seven blood samples using PCR . The first partial sequences of the L gene indicate one of the subtypes of the virus species Zaire Ebola virus . This is the first documented occurrence of this virus in Guinea.
At the end of March 2014, the first cases from the Dabola and Dinguiraye prefectures within the Faranah region became known. In April 2014, the spatial distribution of the epidemic had hardly changed, the number of infected people had risen to 197. In mid-May 2014, the number of infected people was 248 and there have been no new cases in Kissidougou, Macenta, Dabola and Djingaraye for over a month, and no new cases from Conakry for 19 days. At the end of May, however, infections were reported from four previously unaffected areas: from the prefectures of Boffa and Boké in the Boké region of the same name in northwestern Guinea and from the prefectures of Télimélé and Dubréka in the Kindia region , which borders Sierra Leone. There were further transmissions in the capital and in the prefectures of Guéckédou and Macenta. The WHO stated that “ persistent community resistance” was partly responsible for this. In June 2014, the Kouroussa prefecture in the Kankan region was also affected; the total number of infected people was almost 400 in mid-June.
In mid-July (published on July 21, 2014) the number of infected people was 410, the epidemic was active in Conakry and the prefectures of Guéckédou, Boffa, Dubréka and also Fria (Boké region). Three more prefectures were added by the end of July (published on August 4, 2014): Pita in the Mamou region and Siguiri and Kouroussa in the Kankan region, the number of infected people was around 490. By mid-August (published on August 19, 2014 ), cases were also reported from the prefectures of Yomou and Nzérékoré in the Nzérékoré region, while the prefectures Guéckédou and Macenta (both also in the Nzérékoré region), Siguiri and Kouroussa (Kankan region), Pita (Mamou region), Dubréka (region Kindia) and the capital Conakry, the number of infected people had risen to around 530. Until the end of August, the epidemic was confined to these nine prefectures, with Guéckédou prefecture having the most cases. The number of people infected in Guinea rose to around 770.
By mid-September 2014, 12 prefectures in six regions in addition to the capital were affected, in the west of the country Conakry, Boffa (Boké region), Dubréka, Coyah and Forécariah (Kindia region), Pita and Dalaba (Mamou region); in the southeast of the country Guéckédou, Macenta, Nzérékoré and Yomou (Nzérékoré region), Kissidougou (Faranah region) and Kérouané (Kankan region). In mid-September the number of infected people was around 940. By the end of September, new cases of the disease had been registered in the prefecture of Kindia ( Kindia region) and in the Beyla and Lola (Nzérékoré region), both of which border the Ivory Coast . The number of infected people rose to around 1,200. In October, the situation worsened, with around 100 confirmed new cases being reported each week. Many new infections were reported from the prefectures of Guéckédou and Macenta as well as from the capital. In the middle of the month, the prefectures of Coyah (bordering Conakry), Nzérékoré and Kérouané were particularly affected. The epidemic was also active again in the northwestern prefecture of Boké, which borders Guinea-Bissau . The total number of infected people was around 1,500. At the end of October 2014, Conakry and the three prefectures in the southeast, Kérouané, Macenta and Nzérékoré, were most severely affected; the total number of infected people was given as almost 1,700.
In November 2014, the WHO reported that the overall incidence rate for Guinea can be described as stable. About 100 new infections were reported each week. The situation in the south-east of the country, in the border area with Liberia, was still critical. Many new infections continued to be reported from the prefectures of Nzérékoré, Macenta and Kérouané, as well as from Beyla (Nzérékoré region) and Siguiri (Kankan region) on the border with Mali. In Guéckédou, on the other hand, there was only one new infection within three weeks. In November, the case of an imam from the village of Kourémalé (directly on the Malian border) in Siguiri prefecture became known. His trip to Mali caused more people to be infected there . Thousands of mourners were present at his funeral in Kourémalé at the end of October, some of whom touched the body as part of the traditional funeral ceremony. As a result, several new infections and the resulting chains of infection were reported in Guinea from early to mid-November, which are being investigated by WHO epidemiologists. A total of 23 prefectures in six regions in addition to the capital were affected by the epidemic by mid-November. The total number of infected people was around 1970, of which 86% of the cases were laboratory-confirmed.
At the beginning of December 2014, numerous infections and some deaths were reported again. According to the World Health Organization WHO, around 17,800 infections have been registered in Guinea and Sierra Leone. The number of deaths has risen to more than 6,300.
In mid-2015 there were still individual new cases. Suspected Ebola cases have been confirmed in the west of the country and in the capital. On December 29, 2015, the country was finally declared Ebola-free. Years later, Guinea suffers from the personal, social and economic consequences, especially in the affected villages and towns in forest Guinea .
Liberia

Because of the immediate vicinity of the outbreak area in Guinea, the first suspected cases were investigated in Liberia in March 2014. In late March 2014, the first confirmed cases of Ebola were reported in Foya , Lofa County , one of the country's 15 administrative regions . As it became known shortly afterwards, an infected person traveled from there to the capital Monrovia in Montserrado County and to neighboring Margibi County . In Liberia, the epidemic spread rapidly. In April 2014, infected people were already reported from six administrative regions: Lofa County, Bong County , Nimba County (all three located on the border with Guinea), Montserrado County, Margibi County and Grand Cape Mount County . In mid-May 2014, the epidemiological development in Liberia appeared less worrying as no new cases were reported. Another case from Foya became known at the end of May. The deceased was brought to Sierra Leone and buried there in his home in the Kailahun district. New infections were registered again in June 2014, and there were around 30 cases of infection in the middle of the month.
In mid-July (published on July 21, 2014) the number of infected people was around 200, the epidemic was active in six administrative regions (counties), in Lofa, Montserrado, Margibi, Bong, Nimba and now in Bomi County . By the end of July (published August 4, 2014), three more regions had been added: Grand Cape Mount, Grand Bassa and River Cess County , the number of infected people had risen to around 470. By mid-August (published on August 19, 2014) around 830 cases of illness had been reported from these nine counties. By the end of August, cases had been reported from three other regions, Grand Gedeh , River Gee and Sinoe Counties , affecting 12 of 15 regions. Lofa County and the capital Monrovia were particularly hard hit. The number of infected people in Liberia rose to around 1,700.
At the beginning of September 2014, the number of cases in Liberia rose again significantly, geographically 12 of the 15 regions were affected, Defense Minister Brownie Samukai spoke of a "conflagration". A particularly large number of cases were still reported from Monrovia and Lofa County, which borders the Guéckédou and Macenta prefectures in Guinea, which also had many infected people. In mid-September, the number of infected people was around 2,700, with a large increase in the capital. Many new infections were also reported from Bong, Margibi, Grand Bassa and Nimba Counties by the end of September. Geographically, 13 of the 15 regions were affected at this time, the number of infected people rose to around 3800. In October 2014, the WHO noted in its reports that the number of cases reported by the Liberian health authorities were becoming less reliable and that a slower increase in new cases in the In contrast to reports from the helpers on site. At the beginning of October, around 200 new infections were reported per week, mainly from Monrovia, and in the middle of the month Bong and Margibi Counties were also particularly affected. The total number of infected people was almost 4,300. Liberia remained the hardest hit country. Around 450 new infections were reported per week, at which point the WHO reported the total of confirmed, probable and suspected cases, as the number of laboratory-confirmed cases was considered too low (“ under-reported ”). By the end of October 2014, each of the 15 administrative regions had reported cases of Ebola, with Montserrado County with the capital, Bong, Margibi and Nimba County, the latter bordering the Ivory Coast, being particularly hard hit at that time. In contrast, the number of new infections in Lofa County fell, which was interpreted as a result of the containment measures implemented. Since the state health authorities were unable to publish the number of cases for several days in October and the reported data were partially contradicting (see Determination of the number of cases ), the WHO was skeptical about the no longer increasing number of new infections. She wrote in the Situation Report : “ The capacity to capture a true picture of the situation in Liberia remains hamstrung by underreporting of cases. ”(Translated as“ The ability to capture a true picture of the situation in Liberia remains paralyzed by the number of unreported cases when determining the cases. ”) Up to October 31, 2014, the number of infected people was given as more than 6500, which can be seen in the graph as a clear slope. The number of laboratory-confirmed infections rose from almost 1000 to over 2500 cases in one week, this was explained in the Situation Report with a belated notification by the authorities.
In November 2014, the WHO reported that there were signs of a decline in new infections for Liberia as a whole. Nevertheless, the situation in Monrovia and the surrounding Montserrado County remains critical. It was retrospectively confirmed that the number of new infections per week declined from mid-September to mid-October. The cautious all-clear reported in the Liberian media in October 2014 was also included in international reporting. How reliable the data reported from Liberia are is currently still to be questioned critically. In October 2014, less than 40% of the reported infections were laboratory-confirmed. About 160 new infections per week were reported in November. There were still many new infections in Montserrado County with the capital, as well as in Margibi, Bong and River Cess Counties. In Lofa County, however, there was no new infection within three weeks. The success of the containment efforts in Lofa County has also been confirmed by the CDC and Doctors Without Borders. The total number of infected people was over 7000 in mid-November. After Liberia had been Ebola-free since May 9, 2015, a new illness with fatal consequences was documented on June 30, 2015. Since September 3, 2015, Liberia has been free from Ebola again. On November 19, 2015, however, a new infection was reported again. It was not until January 14, 2016 that Liberia - as the last country ever - was declared Ebola-free, meaning that the epidemic is now considered over worldwide.
Sierra Leone

Investigations for the Ebola virus were also carried out in Sierra Leone in March 2014 because of the immediate vicinity of the outbreak area in Guinea . Two people who died of Ebola virus disease in Guinea were buried in their homeland, Sierra Leone. The contact persons involved were monitored over a period of 21 days and did not develop any symptoms . By the beginning of May 2014, more than 100 samples from patients with hemorrhagic fever had been examined, Lassa fever was diagnosed in some cases and no Ebola virus was detected. However, on May 28, 2014, the first 16 cases (seven of which were laboratory-confirmed) were reported in Sierra Leone. The infections were initially limited to one of the 14 districts , they were reported from Kailahun . This district belongs to the Eastern Province ( Eastern Province ) and is located on the border with Liberia and Guinea (Guéckédou Prefecture).
The epidemic spread rapidly in Sierra Leone as well. At the end of May 2014, 50 infected people were reported from a total of five districts: from Kailahun and the neighboring Kenema (both in the Eastern province with border with Liberia), from Koinadugu in the Northern province ( northern province , borders on Guinea) and from Bo and Moyamba in the Province of Southern ( Southern Province ). Most of the cases reported were in the Kailahun district. In June 2014, additional infections were known from the capital Freetown in the Western Area ( western area ) and four districts, Bombali , Port Loko , Kambia (all Northern Province) and Kono (Eastern Province). The total number of infected people was around 100 in mid-June and the WHO reported that the identification and observation of the contact persons by the population had been prevented.
In mid-July (published on July 21, 2014) the number of infected people was around 440, the epidemic was mainly active in six districts, in Kailahun, Kenema, Kambia, Port Loko, Bo and Western with the capital Freetown. By the end of July (published on August 4, 2014), five more districts had been added: Tonkolili and Bombali (Northern Province), as well as Moyamba, Bonthe and Pujehun (Southern Province), the number of infected people was around 650 Districts (including the Western Area with the capital) reported cases of infection, by mid-August (published August 19, 2014) the number of infected people had risen to around 850. At the end of August 2014, Sierra Leone was completely affected by the Ebola virus epidemic, with the number of infected people reaching around 1200. In Kailahun and Kenema, it was particularly difficult to get feedback on those infected or dead. The number of cases in Freetown was gradually increasing. At that time, Welthungerhilfe was already anticipating around 150,000 starving people as a direct result of the crisis.
In September 2014, cases were reported from 13 of the 14 districts, only in Koinadugu District in the Northern Province no new cases were registered. In mid-September, the number of infected people was around 1700, and by the end of the month many new cases of infection had been reported from the capital Freetown and the neighboring districts of Port Loko and Moyamba as well as from the districts of Bo, Bombali and Tonkolili. At the end of September, the number of infected people had risen to around 2,400. The situation worsened in October, with around 300 confirmed new cases reported per week, and later 450 new infections per week. The epidemic was particularly active in the last-mentioned districts, and in the middle of the month the number of infected people had risen to around 3,400. At the end of October 2014, Sierra Leone was again completely affected by the Ebola fever epidemic, especially from Freetown and the neighboring Western Area Rural , many new infections became known, and the situation in the districts of Port Loko, Bombali, Tonkolili, Bo and Kenema remained tense. At the end of October 2014, the number of infected people totaled 5,300, including more than 1,200 who were referred to as suspected cases.
In November 2014, the situation in Sierra Leone remained worrying with more than 400 new infections per week. In the middle of the month there were more than 500 new infections per week. In addition to Freetown and the adjacent Western Area Rural , the epidemic was particularly active in the northwestern districts of Port Loko, Bombali and Tonkolili. Central Bo District (Southern Province) and Koinadugu District (Northern Province) were also affected. In contrast, there were significantly fewer new infections in the southeastern districts of Kenema and Kailahun; in Kenema in particular, this was attributed to the containment measures carried out. The total number of infected people was over 6,000 in mid-November, of which 83% of the cases were laboratory-confirmed. Given the high number of new infections per week, the WHO warned that the number of cases for Sierra Leone would soon exceed that of Liberia.
In mid-2015 there were still individual new cases. Ebola cases have been confirmed in the center and west of the country, including the capital. On November 7th, Sierra Leone was finally declared Ebola-free by the World Health Organization. On January 15, 2016, a death in Sierra Leone was confirmed as a new Ebola case.
Nigeria
On July 20, a 40-year-old Liberian traveled by plane via Lomé ( Togo ) to Lagos in Nigeria . Symptoms of an Ebola virus infection arose during the trip. In Lagos, he went to a private clinic where the infection was found. The man died on July 25th. At the beginning of August 2014, he was identified as the first case of the disease ( index patient ) in Nigeria, and a blood sample tested positive for the Ebola virus. This case is related to a further nine suspected cases of contact persons (especially medical staff) in Nigeria, including one possible death. Research by the WHO showed that an outbreak in Port Harcourt , Nigeria, was also linked to the index case. In total, the number of infected people rose to 20, of which 8 people died. 891 contacts were monitored over a period of 21 days and developed no symptoms of the disease. The WHO announced the end of the epidemic in Nigeria on October 20, as twice the maximum incubation period, i.e. 42 days, had passed without a new infection being registered.
Senegal
On August 29, the first confirmed case of Ebola was reported from Senegal . According to the Ministry of Health, it was a man who had entered from Guinea. The young man had lived with relatives on the outskirts of Dakar for a few days , although he was already showing symptoms; an infection with the Ebola virus was only recognized later. In September 2014, this remained the case in Senegal. All contact persons of the infected person were monitored over a period of 21 days and did not develop any symptoms of the disease. During this period, the WHO reported on the cases of illness and death from Nigeria and Senegal, indicating that these are countries with initial cases and with limited geographical transmission. The end of the outbreak was announced on October 17, 2014. The 74 contact persons were observed for a total of 42 days and were not infected, and no outbreak of Ebola fever was reported from other areas of the country. The young man recovered from the infection, the laboratory diagnostics showed a negative result for the Ebola virus and he returned to his home country.
Mali
On October 24, 2014, a two-year-old girl died of Ebola fever in the hospital in Kayes in western Mali . The toddler's father had died of the disease three weeks earlier in Guinea. Several of the child's relatives had also died shortly before, and Ebola fever was identified as the cause of death for some. The child was then brought to Mali by relatives. On a long journey with a public coach over 1000 km from Guinea to Mali it already showed symptoms. A total of 118 people who had contact with the toddler were monitored over a period of 21 days, none of whom showed symptoms of the disease.
On November 12, 2014, the death of three other people was announced in the capital Bamako , who are considered probable or confirmed cases of Ebola. They had no contact with the toddler. By November 30, the number of infected people rose to a total of eight. Seven people who were infected independently of the first case had been infected by an imam who had traveled from Guinea or were contact persons for these infected people. Five of them died. Since the Imam already showed symptoms in Guinea, he is listed as a Guinean case. He was admitted to the Pasteur Clinic in Bamako on October 25, 2014, where he died two days later. No samples were taken for laboratory diagnostics. Two people involved in his treatment (a nurse and a doctor) fell ill a short time later and were admitted to hospital on November 8, 2014. Ebola viruses have been detected in them. The nurse's fiancée also showed symptoms on November 19. Four other cases involve members of a family that the Imam visited before he was treated at the Pasteur Clinic. The death of the father of the family is considered a likely case of Ebola, as no samples were taken from him. The infection of the mother and a son with Ebola virus was confirmed in the laboratory. Another son was admitted to an Ebola treatment center in Bamako on November 24th. 433 contact persons were identified, none of whom are under observation after 21 days of observation. In the meantime, however, Mali is considered to be free from Ebola fever.
Ebola cases outside of Africa
United States
On September 29, 2014, a case of Ebola was first detected in the USA. Thomas Eric Duncan , admitted to an isolation ward at the Texas Health Presbyterian Hospital in Dallas , was infected in Liberia. The man had reported to the hospital three days earlier, but had only been given medication without having been tested for the Ebola virus. This was only done after the CDC was informed. According to the CDC, fellow travelers on the flight from Liberia to the USA were not at risk because the patient had not yet shown any symptoms of the disease at that time. About 50 people with whom the infected person had contact in the USA were placed under observation for the duration of the incubation period. In this group there are ten people who had direct physical contact, as well as members of the host family and paramedics. The patient died in hospital on October 8th.
On October 12, it was reported that a nurse at the Dallas hospital was infected while treating the first infected. After the nurse developed a fever on October 10, she was immediately isolated. A first test for Ebola virus was positive, the result was confirmed by the CDC laboratory. Similar to the case in Spain (see section Spain ), it was not clear how the infection occurred to the nurse, as she wore gloves, protective clothing and a mask when caring for the Ebola patient. The home of the infected and other places where contact may have been made were disinfected.
On October 15, 2014, the infection was announced to another nurse. The person had also looked after the first infected person in Dallas. The caregiver had traveled to Ohio on October 10 and flown back on a passenger plane from Cleveland , Ohio to Dallas on October 13 and reported a mild fever the next morning. According to reports from the US television channel CNN , she had already had a slightly elevated body temperature before the return flight and reported this to the US health authority CDC. Since her temperature of 37.5 ° C was below the mark of 38.0 ° C defined for fever (or fever of at least 38.5 ° C is defined for suspected Ebola fever) and she had shown no further symptoms, she was not advised against the flight. Due to the close proximity of the flight and the first symptoms, the CDC, in cooperation with the airline, decided to contact and question all 132 passengers on the return flight. Shortly thereafter, this was expanded to include around 150 passengers on the outbound flight to Cleveland. A total of 177 people in the US were observed over a period of 21 days, none of whom showed symptoms of the disease. Two tests for the pathogen were negative for the two infected nurses and they were discharged from the hospital.
On October 24, 2014, Ebola virus infection was discovered in New York City by a doctor who had worked with the aid organization Médecins Sans Frontières in Guinea. On November 11, 2014, the doctor was released from the hospital as cured after two negative tests.
Spain
On October 6, 2014, the infection became known to a Spanish nurse who had previously cared for a Spanish missionary , Manuel Garcia Viejo, who had fallen ill in Sierra Leone in Madrid . Therefore, she is the first person to be infected by human-to-human transmission outside of West Africa. It could not be conclusively clarified how the infection of the nurse occurred during the treatment of the patient in the Carlos III Clinic . Allegations have been made that cuts, poor training, non-safety equipment and closures of the infection department all played a role. Unintentional contact with the face with a contaminated protective glove was named as a possible cause of the infection. The nurse's dog was killed as a precaution. On October 21, 2014 it was announced that no more pathogens could be detected in the nurse's blood after two tests were negative. 87 contact persons were observed over a period of 21 days, including 15 people whose risk of infection was estimated to be so high that they were quarantined at the Carlos III Clinic . In addition, 145 hospital employees were still under observation. None of them developed any symptoms of the disease, so that the end of the disease transmission was announced on December 2, 2014 after no new infections occurred over a period of 42 days.
United Kingdom
On December 29, 2014, a patient at Gartnavel Hospital in Glasgow was diagnosed with Ebola. The patient had previously worked as a nurse in Sierra Leone and had returned to the United Kingdom the day before, where she first arrived in London and then flew on to Glasgow. Upon arrival in London, she had stated that she felt feverish, but her temperature was not increased on several measurements. In this context, later considerations arose as to whether the screening procedures at airports should be reconsidered.
Incidence of illness and death among medical staff
The number of infections and deaths is also high among the helpers and has been described as "unprecedented" by the WHO. As of December 30, 2015, 881 health care workers in Guinea, Liberia and Sierra Leone had developed Ebola and 513 died (only confirmed cases). The reason given was the poor conditions in the African epidemic areas, such as missing or inadequate protective equipment and the high workload of the helpers. Since October 2014, cases of infections from hospitals in Spain and the USA have also been reported outside of Africa.
For the return of sick foreign aid workers, specially converted aircraft are required for the transport. The United States has such capabilities (two Phoenix Air machines based in Georgia ). The German federal government placed a similar order with Lufthansa in October 2014 .
In Germany itself there are an estimated twelve ambulances suitable for ambulance transport. The costs for a patient cared for in Germany may amount to up to 2 million euros, this sum was at least stated for the patient treated in Hamburg.
Unconfirmed suspected cases
Due to the increased public attention, suspected cases were repeatedly reported and isolated from various countries around the world, without these being confirmed afterwards.
Epidemiology
transmission
The pathogen occurs in the body fluids of sick people, for example in blood , excrement , saliva and semen . Infected animals (including the regionally common “bush meat” ) are also a possible source of infection. The Ebola virus can be transmitted through direct body contact, contact with body fluids (blood, feces , vomit ) and through contaminated objects. It penetrates the body through mucous membranes and open wounds such as cuts and stab wounds. In principle, these routes of infection can be reliably switched off primarily by disinfecting objects and avoiding “bush meat”, and secondarily by isolating the sick and protective clothing for caring relatives and medical staff. However, the necessary requirements are not met in all areas.
So far, the infectivity (measure of the ability of the virus to infect) has not been clarified, neither for transmissions from animal to person nor from person to person.
Lethality and Pathogenicity
The risk of dying from a virus infection after illness is described by lethality (death after illness). Not everyone infected with the Ebola virus becomes ill. Those infected without symptoms are not recorded when determining the mortality. The risk of falling ill after the virus has been transmitted is described by the pathogenicity .
How many people infected by the Ebola virus actually fall ill, i.e. how pathogenic the virus is, has not been conclusively determined. In addition to reports of outbreaks with statistically low cases, which suggest an extremely high disease rate after infection, a serological examination was able to detect antibodies against the Zaire Ebola virus in 19.4% of the inhabitants of endemic forest areas in Gabon without an episode of illness after the end of the disease Anamnestically known infection .
The mortality rate for the Zaire Ebola virus, to which the virus variant of the 2014 Ebola fever epidemic is counted, is around 50–90%. An investigation of selected cases of the 2014 Ebola fever epidemic, in which the clinical course is documented, showed a mortality rate of 71% for the first nine months (as of September 14, 2014). Another study indicates a 74% mortality rate for patients treated in hospital for May to June 2014 (basis: 87 patients in Sierra Leone). The group of patients under the age of 21 had significantly better chances of survival with a death rate of 57%, the group with an age of more than 45 years had significantly worse chances of survival with a death rate of 94%.
To determine lethality through statistical counts (instead of following a number of individual cases), both the absolute number of people with Ebola and the number of those who died of Ebola must be taken into account. Under the given circumstances in West Africa and during an epidemic, these data cannot be determined adequately.
A lethality for the current epidemic can be calculated from the total reported incidence and death rates (see table). This is less for an incomplete event than for a closed event, due to the statistical shift that causes the time between illness and death. The quotas for the various countries, calculated on the basis of the cumulative number of cases, differ significantly from one another; they indicate strong biases due to inadequate data collection. The WHO draws attention to this problem. The World Health Organization stopped specifying such a quota in its publications from mid-September, the percentage being referred to as deaths / total cases , i.e. the number of deaths / total number of cases . Until the beginning of September, the rate was given as CFR ( case fatality rate ). At the end of November 2014, the WHO again published data on mortality for the three most severely affected countries. Only cases were taken into account in which records can be used to trace whether the infected person died or was cured. According to this, the mortality rate for patients treated in a hospital or an Ebola treatment center has been 60% since the beginning of the epidemic, for Guinea the mortality rate is 60%, for Liberia 60% and for Sierra Leone 60%. If the records of patients who were not hospitalized are also taken into account, the total mortality rate is 72%.
Determination of the number of cases
The suspected cases and deaths are recorded in local hospitals and emergency facilities of international aid organizations and passed on to the WHO via the national health authorities. The virological confirmation is provided by existing institutions such as the VHF Laboratory in Kenema (Sierra Leone), branch offices of the Pasteur Institute and increasingly by field laboratories or small laboratory areas within hospital wards, which are looked after by various international institutions. These facilities are also used to send samples to research laboratories worldwide for more detailed virological testing. In addition, the laboratory capacities in the affected countries were expanded in the course of the epidemic, but they were not sufficient. Test procedures are increasingly standardized by the CDC and the WHO. A PCR detection method for the virus variant in West Africa was approved by the American FDA on August 5th. These measures were taken in order to accelerate the virological diagnosis on site and to achieve comparable valid results, also against the background that the different lethality values suggest a possible underestimation of the number of illnesses and / or deaths and thus an ineffective recording of the outbreak .
The WHO deals with suspected cases differently depending on the country. While the suspected cases from countries with widespread outbreaks are included in the total number of cases, this does not happen in countries with few cases, such as the USA and Spain. In countries with a large epidemic outbreak, people with the symptoms of Ebola are registered as suspected cases without a virological examination (and thus confirmation) always being carried out. This is not the case in less affected countries, which is why the WHO has limited itself to confirmed cases. For the same reason, the WHO does not include any suspected cases from regions without a confirmed outbreak in its statistics, see section unconfirmed suspected cases .
At the end of October 2014, the WHO estimated that in Guinea, Liberia and Sierra Leone 28 laboratories were necessary to confirm the infection or the cause of death, but only a total of 12 laboratories are available in the three countries. From mid-September 2014, it was already pointed out for Liberia that due to insufficient laboratory capacities and the delayed comparison with data from hospitals, the number of confirmed cases made up only a small proportion of the actual number of cases. For Sierra Leone it was reported that confirmed deaths were only those cases where the patients died in a hospital or treatment center. In addition to a high number of cases that did not become known in health centers, the breakdown in reporting from the centers due to the overload of work is now playing an increasingly important role, especially in Liberia. The slowed rise in new cases since the beginning of October contradicts the oral reports by health workers of increased new cases and rather reflects the deteriorating conditions in the centers. Since the end of September, the number of laboratory-confirmed deaths reported from Liberia was above the reported number of laboratory-confirmed cases, which in mid-October meant that the WHO only published a total number of deaths and a total number of cases of illness in this country and no longer confirmed them separately , probable and suspicious cases. Since October the situation reports of the WHO contain a remark that the reported numbers are to be regarded as too low: “ It is clear, however, that EVD cases are under-reported from several key locations. “Internally, the WHO expects that only half of the actually existing cases of illness and death are included in their official statistics.
In general, the WHO reports all cases of illness since the outbreak began. In this form, the number of cases does not allow a statement to be made about the current sick leave, as they also include patients who have already been cured or who have died. The development of the number of acutely ill would be important for the control of the epidemic z. B. Capacity planning, but it is difficult to determine. However, the WHO's assessment of this can be guessed at from the bed capacity required (in brackets the proportion of the available capacity, as of November 2014):
- Liberia 1269 (73%)
- Sierra Leone 517 (35%)
- Guinea 245 (50%)
Epidemiological factors of spread
The West African Ebola virus epidemic in 2014 is not only unusual in terms of the number of cases observed, some factors have also had a negative impact on the course compared to the previous Ebola virus outbreaks in Central Africa. The Emergency Committee of WHO presented after consultation with the regional health authorities in their particular vulnerability points of the outbreak determined that were complemented by further publication.
- The health systems of the initially affected countries are not suited to respond appropriately to the epidemic with regard to their personnel, financial and medical equipment.
- The lack of treatment places and medical equipment in Liberia means that infected people are transported in taxis to a hospital or treatment facility, where they are usually turned away. The vehicles are then not disinfected and are therefore considered a particular hot spot for the further transmission of the virus.
- Since the disease first appeared in these countries, there is no experience in dealing with Ebola. In particular, there is a lack of knowledge in the population about the transmission routes and risks of the infection.
- In parts of the rural population, the existence of the disease or virus is therefore denied as its cause. People with Ebola are seen as victims of poisoning or witchcraft. In the course of the epidemic, the slogan “ Ebola is real ” was therefore spread on banners and T-shirts.
- The ignorance about the infection routes led to infected relatives being hidden at home. Rejection in society is also given as a reason for this behavior.
- In rural areas, funerals take place without notifying the relevant health service, and the cause of death is often not investigated.
- There is a high degree of spatial mobility among the population, which leads to infected people crossing borders several times.
- In the capital cities of Conakry (Guinea), Monrovia (Liberia) and Freetown (Sierra Leone) several chains of infection with multiple pathogen passages have been observed (which suggests an overall ineffective containment).
- A large number of medical personnel have been infected, indicating inadequate hygiene practices in many medical facilities.
- In the course of the epidemic, the need for medical supplies, including personal protective equipment, could no longer be met.
There are currently no indications for an explanation of the spread dynamics and the (as of September) sustained spread over at least nine months with at the same time intensively used diagnostic techniques on site about an increased infectiousness of the pathogen compared to other ZEBOV outbreak strains or an increased contagiousness index .
Reproduction number
The base reproduction number R 0 indicates how many non-immunized people are infected by an infected person on average. The first calculations of R 0 were published at the beginning of September 2014 by the University of Bern and were 1.51 for Guinea, 2.53 for Sierra Leone and 1.59 for Liberia. These values were confirmed three weeks later by a WHO study which found a base reproduction number of 1.71 for Guinea, 2.02 for Sierra Leone and 1.83 for Liberia for the first 9 months of the current outbreak. The net reproduction number R t (ger .: Net or effective reproductive number ) was estimated on the basis of the WHO figures during the period June to August 2014, 1-2. A research group at ETH Zurich calculated a reproduction number of 2.18 for the period May to June 2014 from the change in the genetic sequences of the virus in 70 Ebola virus patients from Sierra Leone. A base reproduction number of 2 is rather small compared to other infectious diseases. A net reproduction number greater than 1 means that the disease is spreading. To contain an epidemic, it needs to be brought to 1, to end it, below 1.
Epidemiological forecast
The CDC described the outbreak in June 2014 as the largest identified Ebola epidemic to date, both in terms of the number of diseases recorded and the number of deaths. On August 14, 2014, the WHO stated that there were indications in the affected countries that the actual extent of the outbreak was far greater than the number of deaths and illnesses indicated, and spoke of an unreported number in the recording of the number of infected people . Reasons for this are, among other things, the poor medical supply situation and the ignorance of the infection routes in the affected countries.
At the end of August 2014, the WHO presented countermeasures and predicted that the number of sick people in West Africa could rise to more than 20,000 and that up to 10,000 deaths could be expected. Several epidemiologists consider this WHO forecast to be significantly underestimated. At the end of September 2014, the CDC named a correction factor of 2.5 to estimate the actual number of cases in Liberia and Sierra Leone. If effective measures are not taken against the epidemic, the number of infected people in these two countries will rise to 550,000 by the end of January 2015, and even to 1,400,000 if the correction factor is taken into account.
On August 31, the science journal Science quoted the mathematical epidemiologist Christian Althaus from the University of Bern with the statement that up to 100,000 cases of infection could be expected in Liberia alone by December if the epidemic could continue to spread unchecked. In mid-September 2014, the New York Times quoted scientists including epidemiologist Bryan Lewis from the Technical University of Virginia, bioinformatician Alessandro Vespignani from Northwestern University, Jeffrey Shaman from Columbia University and Lone Simonsen from George Washington University that the epidemic could 12 last up to 18 months and by mid-October 2014 alone up to 20,000, if the situation worsens, also cause more than 50,000 cases of infection. In a later assessment, the WHO also pointed out in early September that the number of cases of infection is increasing exponentially in some affected states .
On October 14, 2014, Bruce Aylward, Deputy Director General of the WHO announced that the WHO was forecasting 5,000 to 10,000 new cases per week for the beginning of December 2014.
At the end of September 2014, the science journalist Laurie Garrett criticized the reduction in funding for the WHO by the member states and the lack of a special unit to combat disease. She warned of an escalation of the epidemic and called for a central administration of donations as well as military support for logistical tasks and the protection of the helpers on site. Garret criticized the suspension of passenger and freight traffic by almost all airlines to the countries affected by Ebola. As a result, personnel and relief supplies did not reach the areas, while exhausted aid workers who needed a break could not leave.
In mid-October 2014, an internally prepared WHO report on the approach was made public. The aim of the report is to learn from the course of the epidemic and the measures taken at the end of the epidemic. This contained harsh criticism of the previous approach, especially in the early days. At the same time, Médecins Sans Frontières (Doctors Without Borders) raised serious allegations that the main burden was still with them. MSF coordinator Christopher Stokes said the virus was still out of control. UN coordinator David Nabarro rejected the criticism.
Medical measures
vaccination
When the epidemic broke out, no Ebola vaccine was available. In view of the severity of the 2014 Ebola fever epidemic and the risk also for Western countries, the development of a vaccine was accelerated. In October 2014, a vaccine was expected to be available for April 2015.
Quarantine and therapy measures
One of the most important measures is to place the patient in quarantine to prevent other family members and other people from becoming infected. This are isolation wards needed, the staff has with personal protective equipment be equipped. The patient's family should also be placed in household quarantine, as the incubation period of up to 21 days means that it must be ruled out that other people have been infected.
The treatment of the patients themselves includes hydration and the administration of painkillers and antipyretic agents.
Experimental therapies
A doctor and a missionary, both US citizens, were flown to their homeland after they were infected with the Ebola virus and were the first to be treated with an experimental immune serum . The name of the unapproved drug from San Diego- based Mapp Biopharmaceutical is ZMapp . It has so far been successfully tested on a few monkeys and showed clear improvements within a few hours in the two Americans. Both were discharged from the hospital after about two weeks. An infected Spanish citizen who had previously been flown from Liberia died despite being treated with the experimental drug.
The remedy is based on the principle of passive vaccination . The body of an infected person does not produce its own antibodies , but receives an injection of an immune serum that contains high concentrations of antibodies against the pathogen . In this case, the antibodies required for this are obtained by immunizing mice by infecting the test animals with certain Ebola virus proteins . However, these antibodies cannot be used directly because they can trigger an undesired immune reaction, i.e. they can be recognized by the human immune system as a foreign protein. They are therefore genetically modified to match human antibodies. The genetic material of the antibodies is introduced into tobacco plants , which then produce the antibodies in their leaves as genetically modified organisms (GMOs). Human antibodies in sufficient quantity (at least for the passive immunization of the medical support staff) and at the same time in a noticeably more effective quality can also be used in the form of blood plasma from blood donations from convalescent recipients. Previous attempts on infected people have been largely successful, but the number of cases is still too low to be able to derive a recommendation as a preventive measure. On October 23, 2014 it was announced that the EU had provided € 2.9 million for a project on blood transfusion therapy by an international team of experts. Since a distinction has to be made between prevention for predominantly non-infected people (medical support staff) and therapy for symptomatically infected people, it is particularly noteworthy that the therapy was already based on an Ebola outbreak in 1995 in the Democratic Republic of the Congo (despite statistically too few case numbers) indicated that of the symptomatically infected, approximately seven out of eight patients who received the therapy had survived.
The administration of a drug that has not been approved affects ethical issues. As no clinical studies have been conducted to date , nothing is known about possible side effects of the drug in humans. In extreme cases, the patient can, for. B. die from anaphylactic shock . The question of the selection criteria, i.e. those of the numerous infected people, is just as difficult. Since ZMapp is still in the early stages of development, the immune serum is not available in sufficient quantities to effectively fight the epidemic. The company said it will increase production capacity as soon as possible and is seeking rapid approval by the United States Food and Drug Administration .
After a debate in a committee made up of medical ethicists , scientific experts and laypeople from the countries concerned, the WHO announced on August 12, 2014 that the committee regards the provision of hardly tested preparations as ethically justifiable. The reasons given were the large number of infected people and the high mortality rate. The African Union (AU) welcomed this decision. The AU Commissioner for Social Affairs emphasized the importance of educating patients about possible advantages and disadvantages. In view of numerous media reports on these agents, the WHO stressed on August 15, 2014 that the effectiveness of the experimental preparations has by no means been proven and that possible side effects endanger patient safety. Attention was also drawn to the insignificance of the quantity available.
Ellen Johnson Sirleaf , the President of Liberia, had already asked US President Barack Obama for a delivery from ZMapp. The drug is intended to treat doctors who have been infected themselves. According to the manufacturer Mapp Biopharmaceutical, all supplies were sent to West Africa and the drug was made available free of charge. The Nigerian government also asked for the experimental agent to be delivered. In Liberia, two doctors and a nurse were treated with ZMapp, and two of the patients' health improved significantly. One patient initially showed a slight improvement, but died a few days later. According to the manufacturer, the small supply of the experimental agent has already been used up.
The Canadian government offered to help the WHO in mid-August 2014 and wants to provide a vaccine. It is about 800 to 1000 doses of an experimental preparation called VSV-EBOV , a preparation from Vesicular stomatitis virus with Ebola antigens . It was developed in the Canadian National Microbiology Laboratory and has already been successfully tested on monkeys, but has not yet been used in humans. Tests on humans began in October 2014; in the trial phase, the drug will be administered to 40 healthy volunteers in the United States. The Canadian government also provided the WHO with 800 tubes containing up to 1,600 vaccine doses. If the trial phase is successful, the vaccine could be administered to doctors and medical personnel in the epidemic areas.
A viral vector ( cAd3-ZEBOV ) based on the chimpanzee adenovirus was developed as a vaccine by GlaxoSmithKline and will be investigated in a clinical phase I study from September 2014. The active ingredient TKM-Ebola may be used in the USA under compassionate use conditions. The effectiveness of the antivirals brincidofovir , JK-05 , FGI-106 and BCX4430 is also being investigated.
The Japanese government also offered the use of the drug favipiravir . The preparation is approved in Japan as an active ingredient against influenza , and clinical studies are being carried out with it in the USA. The active ingredient marketed under the designation T-705 prevents the replication of the influenza viruses ; animal experiments with mice also show an effect against the Ebola virus. The extent of replication is significantly reduced, with the result that the infection does not lead to death in any of the test animals. The effect can be achieved when using the agent up to the sixth day after infection.
The non-governmental organization Doctors Without Borders wants to conduct clinical studies of Ebola drugs together with research institutions from Great Britain, France and Belgium. They should take place independently of one another, in two cases it is about antiviral agents, in one case about blood plasma of cured patients. Results can be expected from February 2015 at the earliest.
Due to the worldwide presence of the Ebola epidemic in the media, rumors were increasingly spread on social media that certain products or processes were suitable as a cure or preventive agent . The WHO issued a warning on August 15, 2014 against the use of such products or processes. In Nigeria, at least two people died after drinking salt water rumored to protect against Ebola.
Further measures

Measures in the affected states
Liberia
Most of the border crossings in Liberia were closed on July 27, 2014. Shortly afterwards, a national emergency was declared in Liberia . In July 2014 it was reported that two African airlines no longer served the capital Monrovia. At the two airports in Liberia, people entering and leaving the country were examined for signs of Ebola. Liberia was hardest hit by the Ebola virus epidemic (as of November 2014). The WHO reported in Liberia in particular that significantly more patients than expected appeared in newly opened treatment centers within a very short time. The World Health Organization interpreted this as an unreported number when recording the number of infected people. Treatment centers have been set up in Monrovia (250 beds) and Foya (40 beds), among others.
President Sirleaf announced on August 20, 2014 that a night curfew would apply. Quarantine measures have also been tightened in order to contain the spread of the disease. In Liberia, the West Point district of the capital Monrovia has been quarantined. The quarantine measures even affected entire cities, such as Foya in Liberia. As of October 2014, entry and exit was only possible in Monrovia at Roberts International Airport and James Spriggs Payne Airport as well as at the border crossings Foya Crossing , Bo Waterside Crossing and Ganta Crossing . The body temperature of the travelers was screened at these points . In addition, freedom of assembly was restricted and the Senate election planned for mid-October 2014 was postponed. In November, Sirleaf announced that it would not extend the state of emergency, but that the night curfew should still apply.
Sierra Leone
Because of the relatively low chance of survival in rural areas compared to cities, some isolation facilities were set up in July 2014 in the border area of Sierra Leone, Guinea and Liberia. These are located in Koindu and Buedu in the Kailahun district , among others . From there, patients are to be brought to the Ebola treatment center in Kailahun . In addition, 800 local health workers were trained there. The treatment center in Kailahun has 104 beds, another is in Bo, the capacity of which will be increased from 35 to 64 beds (as of November 2014). The aid organization Médecins Sans Frontières ( Doctors Without Borders ) described the existing capacities as "completely inadequate".
A national emergency was also declared in Sierra Leone at the end of August. As early as July 2014 it was reported that two African airlines were no longer flying to the capital Freetown. President Ernest Bai Koroma ordered far-reaching measures in Sierra Leone. Among other things, the epidemic areas were quarantined, and people infected were to be found through house searches and brought to a treatment center. Public gatherings were only allowed to provide information about Ebola. The cities of Kenema and Kailahun were affected by the quarantine measures . In August 2014, criminal law in Sierra Leone was tightened, and hiding people suffering from Ebola was prosecuted as a criminal offense.
A curfew was imposed on September 19-21 . Only security guards and around 28,000 volunteers were allowed to move outside the home during this period in Sierra Leone. The task of the helpers was to reach each of the nearly six million residents to provide information about the disease, find infected people and bring them to a treatment center. This quarantine for an entire country has been criticized by the organization Médecins Sans Frontières (Doctors Without Borders). She feared that the population would become even more insecure and that people suffering from Ebola would be hidden. International help, trained doctors or disease experts, etc. were also called for. a. by the local organization Don Bosco Fambul to get the epidemic under control. In October 2014, around 7,000 schools were closed.
For travelers at Lungi International Airport in Freetown, there were tightened measures from October 2014. All preventive and control measures to contain the epidemic were increasingly carried out by police and military forces.
Guinea
The schools were closed from July 2014 to January 19, 2015. Guinea closed its borders with Sierra Leone and Liberia on August 9, 2014 to stop the spread of the epidemic. There were quarantine measures a. in Guéckédou . Guinea was less present in the media than Liberia and Sierra Leone. The epidemic areas in Guinea are located on the borders with these two countries, these are "forest regions" which were the most difficult to access. In October 2014, in the context of the travel warning that had already been imposed, the CDC did not provide any information on precise measures in Guinea that should be used to contain the epidemic. There are treatment centers in Conakry, Guéckédou (85 beds each) and Macenta (35 beds), among others.
Nigeria
Nigeria declared a state of emergency on August 8, 2014 because of the epidemic. Among other things, President Goodluck Jonathan ordered that school holidays be extended to prevent possible transmission of the virus in schools. In addition, all deaths due to illness should be reported to the authorities.
Mali
The first cases of illness in Mali in October and November 2014 could be traced back to sick people who had come from Guinea. Nevertheless, the border with the neighboring country was not closed. The WHO announced that it was attempting to "vigorously monitor possible contacts" to bring the outbreak in Mali under control, similar to what had been done in Nigeria and Senegal. There is an Ebola treatment center in the capital Bamako. Pasteur Clinic, a major private clinic in the country, was closed after infections broke out there.
International health emergency and relief efforts
On August 8, 2014, the World Health Organization declared after deliberations of the competent emergency committee for the epidemic health emergency of international scope ( Public Health Emergency of International Concern , PHEIC). The classification as a PHEIC is a measure of the International Health Regulations ( English International Health Regulations , IHR ) and thus an international law binding provision.
The states in which cases of Ebola virus disease occur are called upon, among other things, to declare a state of national emergency and to provide financial means to contain the epidemic and to mobilize health care workers . The states should activate their disaster control in order to implement all preventive and emergency measures under central management. This also includes educating the population about the infectious disease. Local forces (tribal elders, religious leaders, traditional healers, etc.) should be involved in this process in order to convince the population of the advantages of early treatment. In the affected areas, the supply of medical goods and personal protective equipment (especially protective suits ) must be ensured for all people who come into contact with infected people.
Neighboring states should urgently set up a monitoring system for frequent cases of unexplained fever and a qualified laboratory for pathogen detection. If Ebola fever is suspected, the appropriate emergency measures should be implemented within 24 hours in order to prevent further spread. All states are given the opportunity to restrict international travel, although this is not generally recommended in the announcement.
Aid from individual states
On August 4, 2014, the World Bank pledged emergency aid of up to 200 million US dollars (149 million euros) to the countries affected by the epidemic. This is intended to finance containment and prevention measures in the states. The WHO has previously pledged US $ 100 million in aid. At the end of September 2014, the World Bank increased financial support to a total of 400 million US dollars.
The US government pledged in September 2014 to send around 3,000 military personnel to the region, including engineers and logistics experts, as well as doctors and paramedics. They are to set up 17 new treatment centers in Liberia and train the medical staff on site. This was welcomed by the WHO and described as a measure that was necessary to get the epidemic under control. In October the number of pledged helpers was increased by the USA to 4,000 military personnel. 750 British soldiers are also expected to help set up treatment centers and train medical staff in Sierra Leone.
Further help was offered in September 2014 by the Chinese government, which is providing Sierra Leone with a mobile diagnostic laboratory and sending health experts to the country. By mid-October 2014, financial resources equivalent to 97 million euros had been made available. The Chinese government has also promised to build a treatment center in Liberia and to increase the number of medical staff on site to 700. The Cuban government also promised the WHO in September that it would send a team of 461 experts to West Africa.
After Liberia's President Johnson Sirleaf asked the German government for help in a letter in mid-September 2014, the government also pledged support. This involves funding of 5 million euros for the WHO and for projects by non-governmental organizations (NGOs) such as Doctors Without Borders or Welthungerhilfe . In mid-October, the budget committee of the Bundestag approved additional funds in the fight against the epidemic, a total of 120 million euros.
The European Union also announced aid. In addition, the EU Commissioner Kristalina Georgieva announced that the EU member states are making 78 million euros available for measures against the epidemic. Almost 150 million euros had already been made available beforehand. The International Monetary Fund (IMF) made available US $ 130 million (€ 102.5 million) to fight the epidemic at the end of September.
Evacuation of helpers and medical care in other countries
Several infected people who had previously helped contain the epidemic have been flown to other states to provide them with better medical care. The following cases are known, among others:
- The American doctor Kent Brantly, who was infected while helping out in Liberia, was treated with ZMapp at Emory University Hospital in Atlanta . He was discharged from hospital as cured in late August 2014.
- The US nurse Nancy Writebol, Brantly's assistant, was also infected on an Ebola ward in a clinic in Monrovia, Liberia. She was also treated with ZMapp in Atlanta and survived.
- A British nurse who was infected in Sierra Leone was treated in a London clinic. He had given medical care to a toddler in whom the Ebola virus had initially not been detected. He also recovered from the virus infection.
- In France , a nurse working in Liberia has been treated as an infected person since September 18. Experimental therapy was attempted with her. In early October it was announced that she had survived the illness.
- Another patient was flown to Hamburg from Sierra Leone at the end of August . The infected WHO employee was treated at the University Medical Center Hamburg-Eppendorf (UKE). According to the attending physician, no experimental therapy was attempted, but the usual therapy for Ebola fever, which focuses on measures to lower the fever and compensate for the loss of fluids and electrolytes . After five weeks of treatment, the Senegalese was released from the UKE as cured.
- Following a request from the WHO, a doctor from Uganda who was infected with Ebola and who worked for an Italian non-governmental organization (NGO) in Sierra Leone was transferred to Germany on October 3rd . The infected employee was treated in isolation ward 68 at the University Hospital in Frankfurt am Main . On November 5, 2014, the university clinic announced that he was doing better.
- The treatment of the third patient began in Germany on October 9th. The UN employee was flown from West Africa to Leipzig and was looked after at the St. Georg Clinic . The patient came from Sudan and was infected while working in Liberia. According to the clinic, experimental drugs were used in his therapy in addition to conventional measures. The hospital management in Leipzig announced the death of the patient on October 14, 2014.
- On November 20, a Cuban doctor who became infected while treating patients with Ebola in Sierra Leone was flown to Geneva for treatment , where he was treated at the local university hospital. It was the first Ebola case to be treated in Switzerland . Contrary to the custom of the WHO to have sick helpers treated close to their relatives in their home countries, it concluded an agreement with the Cuban government to provide the best possible care for infected doctors abroad. In Cuba, adequate treatment is impossible because there is a lack of medication and knowledge. Cuban nurses who volunteered for this mission also had to sign a corresponding declaration that excludes repatriation in the event of an infection with Ebola. On December 6th, the 43-year-old patient was discharged cured after 16 days of hospitalization. He was awarded the zmapp predecessor ZMab and the equally experimental flu drug favipiravir the Japanese company Fujifilm treated.
Aid organizations
The WHO dispatched around 400 employees to the affected areas to support the personnel on site, as well as 70 employees through the CDC. The organization Médecins Sans Frontières (MSF, Doctors Without Borders ) employed around 3,100 national and 267 international employees (as of November 2014). In the epidemic areas, MSF established six treatment centers to care for a total of around 600 patients, as well as two screening centers to examine and temporarily isolate patients suspected of having an infection (as of November 2014). According to Florian Westphal, Germany's managing director of the aid organization, thousands are necessary.
The Red Cross has sent 130 international aid workers to the infected area so far (as of September 2014). A treatment center for 60 patients has been set up in Sierra Leone.
Welthungerhilfe has been carrying out several aid projects in Sierra Leone since 2004 and in Liberia since 2003. In Sierra Leone she was involved in educational work and provided 3,000 households affected by the curfew (approx. 15,000 people) with urgently needed food. Welthungerhilfe has been working with local authorities and partner organizations in southeast Liberia since mid-August to distribute awareness-raising and hygiene materials.
WHO
The WHO director for the Africa region, Luis Sambo, visited the states of Liberia, Sierra Leone and Guinea, which were affected at the time, from July 21-25, 2014. Meetings were held with the presidents, health ministers and other government representatives, as well as with international and local non-governmental organizations and UN representatives. The WHO director assured that the epidemic could be contained through the known prevention and control measures, but also emphasized how serious the situation was. In order to initiate internationally binding regulations, the World Health Organization (WHO) declared the epidemic on August 8, 2014 to be a health emergency of international concern .
At the end of August 2014, the WHO presented a plan ( roadmap ) on how to stop the epidemic within the next six to nine months. This included international aid measures in order to be able to set up treatment centers in the epidemic areas and provide the necessary goods. The WHO estimated the cost of this at US $ 500 million. Since the situation was steadily deteriorating, especially in Liberia and Sierra Leone, the UN Secretary General Ban Ki-moon made a public appeal at the beginning of September, calling on the industrialized countries in particular to provide more aid. On September 22, 2014, the Emergency Committee for International Health Regulations ( IHR Emergency Committee ) decided that the measures in the context of the international health emergency would continue to apply. Standards have also been set for control measures, such as locating contacts, safe burials and mobilizing the population. The WHO implemented this together with MSF and other organizations as part of the UN mission.
BIG SEA
On September 18, the United Nations Security Council met for the first time in its history on the occasion of a crisis caused by illness. The UN Secretary General Ban Ki-moon described the Ebola fever epidemic in West Africa as a "global threat to peace and security". He announced that a UN mission would be carried out for an emergency response to the epidemic. The international mission is known as UNMEER , the abbreviation for United Nations Mission for Ebola Emergency Response . The mission's five objectives were defined: stopping the epidemic, treating the sick, ensuring basic services, maintaining stability and preventing further outbreaks. Ban Ki-moon emphasized that success in the fight against the epidemic would only be possible with the support of the international community. He demanded that the measures would have to be increased by a factor of 20 and that financial resources amounting to a billion US dollars would have to be made available over the next six months.
Of the originally estimated requirement of one billion US dollars, only 100,000 US dollars had been paid up by the Colombian government at the start. As of January 16, 2015, the demand to March 2015 was estimated at 1.5 billion US dollars, of which approximately 1.18 billion (77%) had been collected. For the period from April to September 2015, UNMEER estimated the need at another 1.5 billion US dollars.
At the end of September 2014, the mission's headquarters were set up in Accra ( Ghana ) and are headed by the UN Secretary-General's Special Representative, Anthony Banbury . On October 14, 2014, Banbury reported to the UN Security Council on the upcoming measures. UNMEER takes on the management of the emergency operation in the epidemic area and coordinates the cooperation of other UN organizations, aid organizations and government organizations. For example, UNICEF is leading the way in mobilizing the population.
A 90-day plan was put into effect on October 1, 2014, with the aim of gradually containing the epidemic. Within 60 days, 70% of the sick are to be isolated and given medical care and 70% of those who have died of Ebola are to be buried safely and dignified (so-called 70-70-60 goal). These target rates should be 100% within 90 days (so-called 100-100-90 target). Further goals and their implementation have been listed in the WHO situation reports since October . The establishment of Ebola Treatment Centers (ETC, Ebola Treatment Centers ) is of great importance. At the end of October, only 22% of the required 4707 ETC places were available. Also are Community Care Centers (CCC, Public Assistance Centers) are established, which are operated by a municipality. They are intended to serve as an alternative to a treatment center when sick people are turned away because of overcrowding. At the end of October, only 4% of the required 2685 CCC places were available. Further indicators to measure the effectiveness of measures against the Ebola virus epidemic are shown in the table below. The underlying data are determined by UNMEER, WHO, IRFC ( International Red Cross and Red Crescent Movement ) and other organizations.
| country | Target percentage, if applicable |
Status at the end of October 2014 actual value / setpoint (in percent) |
Status at the end of November 2014 actual value / setpoint (in percent) |
Status at the end of December 2014 actual value / setpoint (in percent) |
|---|---|---|---|---|
|
|
Number of beds in operational ETCs | 160/670 (24%) | 245/490 (50%) | 250/695 (36%) |
| Number of beds in operational CCCs | 0/328 (0%) | 0/328 (0%) | 1/62 | |
| Isolated cases of illness / beds per reported patient (70% as of December 1 and 100% as of January 1, 2015) |
99% (estimated) |
100% / 2.3 | no data / 1.9 | |
| Funeral teams that are trained and on duty (70% as of December 1st and 100% as of January 1st, 2015) |
34/60 (57%) * | 50/60 (83%) ** | 64/62 (103%) | |
|
|
Number of beds in operational ETCs | 613/2732 (22%) | 1269/1733 (73%) | 660/1989 (33%) |
| Number of beds in operational CCCs | 88/1100 (8%) | 27/1100 (2%) | 103/428 (24%) | |
| Isolated cases of illness / beds per reported patient (70% as of December 1 and 100% as of January 1, 2015) |
no data | 100% / 11.7 | no data / 13.9 | |
| Funeral teams that are trained and on duty (70% as of December 1st and 100% as of January 1st, 2015) |
55/220 (25%) * | 77/100 (77%) | 89/100 (89%) | |
|
|
Number of beds in operational ETCs | 356/1209 (29%) | 517/1460 (35%) | 896/1783 (50%) |
| Number of beds in operational CCCs | 36/1208 (3%) | 190/1208 (16%) | 291/1208 (24%) | |
| Isolated cases of illness / beds per reported patient (70% as of December 1 and 100% as of January 1, 2015) |
37% (estimated) |
100% / 1.5 | no data / 3.6 | |
| Funeral teams that are trained and on duty (70% as of December 1st and 100% as of January 1st, 2015) |
50/90 (56%) * | 94/114 (82%) | 101/114 (89%) | |
| * As of mid-October 2014; ** As of mid-November 2014 | ||||
As of December 1, 2014 (the 70-70-60 target), the WHO announced that the targets had been achieved in Liberia and Guinea, but only in some regions in Sierra Leone. In the Situation Reports , attention was drawn to the fact that the 100% supply of the infected is only a greatly simplified representation. The number of beds available for treatment is divided by the number of new infections (each for a three-week period). In areas where there is currently a large number of new infections, it is still not possible to isolate all sick people, while treatment centers are partly empty in areas in which the epidemic is no longer active. According to the WHO, there are no reliable or comparable data from the clinics, so the information is given in this way. In addition, Bruce Aylward, Deputy Director General of the WHO, warned that, even if these goals are achieved, transmission and thus new infections cannot be ruled out. It is still not ensured that all sick people are found and that contact persons are identified and monitored. In comparison with the epidemiological forecasts of September and October, however, the countermeasures were successful.
Charity drives
In November 2014, organized by Bob Geldof , there was a new edition of the song Do They Know It's Christmas? in the musician project Band Aid 30 , with the aim of collecting donations for the fight against the epidemic with the proceeds of the single. The British version has raised £ 1.2m so far . In addition, a German version was published on November 21, 2014, this project was organized by Campino ( Die Toten Hosen ).
Measures in or by Germany
In contrast to Great Britain, France or the USA, there are no health checks at German airports and seaports. Federal Health Minister Hermann Gröhe does not consider this to be sensible for countries without direct flight connections to the Ebola region. There are no direct flights from Germany to the three most affected countries. Bavaria, on the other hand, is increasing its protection at its two international airports in Nuremberg and Munich. There are daily feeder flights from Frankfurt am Main or Brussels, from where West Africa is served. The Infectious Disease Task Force is to ensure that suspicious people are isolated in the airport building. To this end, five mobile doctor's stations and a sick room are to be set up in the airport building in the near future.
In addition to France, Great Britain and Spain, an inter-ministerial crisis team has also been set up in Germany in the Federal Foreign Office since July 2014 . On October 8, 2014, Walter Johannes Lindner , until then Ambassador to Venezuela, was appointed as the Federal Government's Ebola Commissioner.
An airlift to Monrovia in Liberia was set up from Dakar in Senegal at the beginning of October 2014 . In this way, relief supplies such as protective clothing and disinfectant materials were transported by the Bundeswehr . In addition, the Bundeswehr has its own forces in Mali and Senegal.
After an appeal by Federal Defense Minister Ursula von der Leyen and Health Minister Hermann Gröhe at the end of September, around 5,000 volunteers, including 1,200 civilian helpers at the German Red Cross (DRK). However, the DRK stated that fewer than 100 of them would be released from work or would be suitable for a longer period of time. Even at the end of October there were still too few qualified helpers. The civil aid workers are to help expand a treatment center in Kenema (Sierra Leone) to a treatment capacity of 100 beds. In addition, the commissioning of an Ebola Treatment Center (ETC) in Monrovia with 100 beds is planned for the end of November 2014 . Here helpers of the DRK and members of the medical service of the Bundeswehr should work together. Of the 3,000 people who originally volunteered for the Bundeswehr, 85 volunteers were trained by November 18, 2014. A first ten-member team made up of members of the German Armed Forces and the DRK traveled to Liberia on November 7th, and more helpers followed on November 24th. The Federal Ministry of Defense announced that their deployment would take four to five weeks. When they return, they have to be quarantined for a week. This is followed by two more weeks of voluntary observation.
Since the Bundeswehr did not have a special aircraft for evacuating highly contagious patients, it was decided on October 22, 2014 to purchase such an emergency aircraft. Lufthansa received the order to provide such a machine . The Ebola rescue aircraft went into operation on November 27, 2014. Lufthansa had provided an Airbus A340-300 . The former long-haul jet was set up with an isolation ward with which extreme Ebola cases can be treated clinically in flight. It is named after the German physician and microbiologist Robert Koch . In addition to Lufthansa and the German federal government , the Robert Koch Institute was also responsible for the overall renovation of the interior , the renovation was carried out in Hamburg.
In addition, the Bundeswehr purchased 20 special transport systems with which patients can be transported lying down and isolated in an airplane. In October 2014, transport isolators were subjected to a technical examination at the Bundeswehr Central Hospital in Koblenz.
The Ramstein Air Force Base serves the US military as a logistics center for their flights, through which material and personnel are transported to Africa. The US Army Barracks Smith Barracks in Baumholder , Rhineland-Palatinate, is intended as a quarantine station for American soldiers returning . A “controlled observation” with medical examinations is to take place there for three weeks. The first 20 US soldiers are already waiting (as of November 2014) in Africa for their return to Germany. In total, the barracks will accommodate up to 200 of them. The state of Rhineland-Palatinate and the Federal Ministry of Defense have already approved these plans. The approval of the Foreign Office in Berlin is still pending.
Travel restrictions and other measures
Restrictions on travel or trade are not recommended by the World Health Organization and its Travel and Transport Task Force . The WHO regards air travel as a low risk for the transmission of Ebola fever: “ Because the risk of Ebola transmission on airplanes is so low, WHO does not consider air transport hubs at high risk for further spread of Ebola. ”
Africa
Zambia announced travel restrictions for people from the epidemic areas in August 2014. The citizens of Zambia have been banned from traveling to these countries.
On August 23, 2014, it became known that the neighboring Ivory Coast was closing its borders with Guinea and Liberia for fear of the epidemic spreading. According to the World Health Organization, no cases of Ebola had yet occurred in the country. Previously, after the situation eased prematurely, Senegal had closed its borders with Guinea and decided to take appropriate measures for aircraft and ships from Guinea, Sierra Leone and Liberia. Even South Africa imposed a travel ban on people coming from the countries concerned.
In contrast, Mali kept the border with Guinea open. Mauritania, on the other hand, closed the border with Mali. The first cases of illness in Mali in October and November 2014 could be traced back to sick people who had come from Guinea. Epidemiologists pointed out that if the border crossings to Guinea are open, the risk of further cases for Mali is correspondingly high.
Outside of Africa
On August 13, 2014, the German Foreign Office asked all German citizens to leave the West African countries of Guinea, Sierra Leone and Liberia and urgently advised against traveling to these countries. It was stressed that this did not apply to medical and humanitarian personnel helping to contain the epidemic. The Foreign Office drew attention to the fact that increased controls can be expected at the borders and airports of West African countries, also outside those affected by the epidemic. Travelers with medical problems, such as fever, would have to expect forced quarantine. A partial travel warning was issued for Mali in November 2014.
The travel warnings for US citizens were on the highest level (Engl. 31 July 2014 at Level 3 Travel Notice set) for Guinea, Liberia and Sierra Leone. The Centers for Disease Control and Prevention (CDC) called on citizens to refrain from all travel to these states that is not absolutely necessary. After the first case diagnosed in the USA, stricter control measures were introduced at five US airports in October 2014. Travelers from Guinea, Liberia or Sierra Leone arrive at one of these five airports. People entering the United States from these states will have their body temperature measured and screened for symptoms of illness. A questionnaire is also carried out and they receive a CARE ( Check and Report Ebola ) kit with information and measuring devices to monitor their body temperature over a period of 21 days. Monitoring is carried out in collaboration with local or state health authorities. On November 17, 2014, these measures were also extended to passengers from Mali. Representatives of the Republican Party demanded that all flights from the West African epidemic areas to the USA should be banned.
For Nigeria, the Level 2 (Engl. Was founded in August 2014 Level 2 Travel Notice ) arranged an alert level (Engl. Alert ) that travelers to prompt comply advanced protection measures. On October 7, 2014, the warning level for Nigeria was lowered ( Level 1 Travel Notice ) with the information that the epidemic in this country could be contained.
At the same time, surveys of passengers from the African epidemic areas were introduced in London at Gatwick and Heathrow airports and at the Eurostar terminal . Also in October 2014, the first simulation of an Ebola outbreak in Europe took place in Great Britain . The UK government wanted to check that the health system was prepared enough. Also France and the Czech Republic announced checks at airports.
On the occasion of the Hajj , the Islamic pilgrimage to Mecca in October 2014, the authorities in Saudi Arabia took precautions against the Ebola epidemic. Pilgrims from the states affected by the epidemic were not given visas to enter the country. Quarantine stations were also set up.
At the end of October 2014, Canada imposed an entry ban on people who had been in one of the Ebola-affected countries in the past three months. Australia had previously imposed an entry ban. Also at the end of October 2014, the government of North Korea decided on a three-week quarantine for all foreigners entering the country. Travelers from infected areas should be placed under medical observation in hotels in isolation from other foreigners as directed by the government. In March 2015, the quarantine requirement was restricted to those arriving from the epidemic areas of Africa, but no foreign athletes were admitted to the planned marathon in Pyongyang .
Financial aid
On August 4, 2014, the World Bank announced that it would provide the affected countries Guinea, Liberia and Sierra Leone with emergency aid of up to US $ 200 million (EUR 149 million). Financial aid has also been promised by the African Development Bank (US $ 60 million) and the WHO (US $ 100 million).
The misappropriation of at least five million euros in Ebola funds resulted in considerable financial damage. According to a financial audit report, almost two million of the Red Cross donations were evaded by employees of the International Red Cross and Red Crescent Movement in Sierra Leone with the help of bank employees. Due to excessive prices for aid supplies and excessive personnel costs, around two million euros were lost in Liberia . One million euros was billed too much for customs clearance in Guinea . Further investigations were not yet completed in 2017.
Effects of the Epidemic
Economic consequences
The economic consequences of the epidemic for the three mainly affected countries Sierra Leone, Liberia and Guinea are far-reaching. The free movement of goods and people in the countries is considerably restricted due to the quarantine measures, which leads to price increases and a loss of income. Numerous international companies and development organizations brought their employees to safety in the course of the epidemic, so that the associated projects stalled or came to a standstill. In addition, there are considerable additional burdens for the state administration and for the public health system. The President of the World Bank, Jim Yong Kim , spoke on September 17, 2014 of an economic "catastrophe" for the three countries.
A study published by the United Nations Development Program (UNDP) in November also points to the devastating economic consequences of the epidemic. This had a noticeable impact on the population in the three countries mainly affected. In the past six months, the average household income in Guinea fell by 13%, in Sierra Leone by 30% and in Liberia by 35%. This was caused by loss of earnings and increased prices for basic food .
According to Wolfgang Jamann, General Secretary of Welthungerhilfe on the situation in Sierra Leone in October 2014, investors are cutting back or postponing planned investments and foreign companies are withdrawing from the country. The region would become increasingly isolated from international markets and government measures to contain the disease would affect trade. Weekly cement sales in the construction industry fell 60% between January and October 2014. Bars, restaurants and many markets had to close, and hotel occupancy rates have fallen from over 60% to 13% since the outbreak of the crisis.
The economies of several West African countries are on the verge of collapse due to the effects of the Ebola epidemic.
Humanitarian crises in the affected states
In August 2014, Welthungerhilfe warned of a humanitarian crisis in the affected areas. As a result of the quarantine measures, trade came to a standstill in several areas. The prices for staple foods had risen significantly. Furthermore, the supply of food and fuel was limited as international deliveries by ship or plane were suspended. Welthungerhilfe announced on August 21, 2014 that it would supply the people in the quarantined areas with food and hygiene items. In October 2014, Welthungerhilfe again warned of the far-reaching consequences for the supply of food. The epidemic will "have a significant impact on the food situation in the affected countries in the coming months," said Bärbel Dieckmann , President of Welthungerhilfe. The aid organization Médecins Sans Frontières (Doctors Without Borders) described the situation in the areas as a “ humanitarian catastrophe ” in August 2014 , especially as medical facilities for general health care were closed. She criticized the in her view insufficient commitment of the international community.
In Liberia, which was particularly hard hit by the epidemic, Defense Minister Brownie Samukai warned in a speech to the United Nations in September 2014 about the effects on the country, whose national existence was threatened. The already weak medical infrastructure is on the verge of collapse, as many helpers have already contracted Ebola or died from it. Trade, transport and food production collapsed, which could lead to the collapse of the state. To make matters worse, the country was only served by two international airlines. At the meeting of the IMF and World Bank in October 2014, the presidents of Sierra Leone, Ernest Bai Koroma and Guinea, asked Alpha Condé for faster support. The situation in the West African countries is "fragile".
The ELWA-3 Ebola treatment center with 120 beds set up by the organization Doctors Without Borders in Liberia's capital Monrovia was already full after a short time. The Belgian doctor Pierre Trbovic (Doctors Without Borders) reported that sick people can no longer be admitted and have to be sent back to their families. According to estimates by the WHO, in October 2014 only 23% of the places required for the treatment of Ebola fever were actually available.
The quarantine of the West Point district of the Liberian capital Monrovia led to riots . The inadequate supply of daily necessities and poor medical care led to looting and panic among those trapped in this slum area , and the police used tear gas. After the Liberian government failed to keep its promise to pay risk premiums to health care workers from October 9, 2014, the medical staff went on strike. It was reported that salaries from the previous month had not yet been paid. The strike ended after a few days. UN Under-Secretary-General Hervé Ladsous warned in the UN Security Council in mid-October of a state crisis and the collapse of the health system. He said that people's trust in the institutions was falling. As a result of the severely impaired health system, many Liberians no longer had regular health care available, so that, for example, from the end of October 2014, malaria drugs were distributed by the aid organization Doctors Without Borders .
In Freetown, the capital of Sierra Leone, the treatment of the sick could no longer be guaranteed. The health system collapsed, the hospital wards were overcrowded, so that infected people had to be turned away. The bodies of those who died of Ebola, through which the virus can be transmitted, remained in houses or on the streets for hours or days. According to estimates by the WHO, only 29% of the places required for the treatment of Ebola fever were actually available in October 2014. Unrest and acts of violence against aid workers have been reported in Sierra Leone . For example, in October 2014 two helpers were killed by a group of armed residents in Koidu . 1.6 million school children are affected by the closed schools, many of them lose their school meals. Food prices rose dramatically, between March and August 2014 the price of fish rose by 40%, for cassava by more than 50% and for rice by 13%.
In September 2014 in Guinea there were reports of fatalities among doctors and helpers who wanted to inform about Ebola virus in the remote region of Womey , a sub-prefecture of Guinea .
Medical care in hospitals in Sierra Leone was poor in December 2014 and endangered the fight against malaria. At least three doctors have died from the virus.
In March 2015, massive increases in measles, malaria, other diseases and maternal mortality are expected in the affected countries of Guinea, Liberia and Sierra Leone, well above the original number of victims of the epidemic. The already weak health systems collapsed with the epidemic.
tourism
Some African countries introduced travel restrictions to combat Ebola. For example, West African Guinea closed its borders with Sierra Leone and Liberia in October 2014 to prevent more infected people from entering the country. Zambia and other countries also reacted in a similar way with travel restrictions.
While countries around the world such as Canada, Australia or Saudi Arabia imposed an entry ban on residents of the West African states concerned, the EU countries mostly reacted more moderately with increased controls and health checks upon entry. Some states even abandoned restrictions and increased controls altogether. Germany also refrained from such precautionary measures, as the spread of Ebola in Germany by a sick flight passenger was generally assessed by the authorities to be very low.
The impact on tourism outside the three affected countries was small: the number of tourists arriving in sub-Saharan Africa rose by 3% in 2014 compared to 2013, while the global increase was 4.4%.
See also
Web links
- Information on the Ebola virus epidemic in West Africa from the Robert Koch Institute (RKI)
- Official site of the anti-Ebola strategy in Sierra Leone (English)
- Framework Concept Ebola Fever. Preparations for measures in Germany. (PDF) Guidelines for health authorities and medical professionals, RKI, December 1, 2014
- WHO information page on epidemic warnings
- Information from the European Center for Disease Prevention and Control (ECDC) on the Ebola virus epidemic in West Africa
- Website of the Bernhard Nocht Institute as the responsible national reference center for tropical infectious agents
- Ebola diary on taz.de
- Ebola here - danger or scaremongering? , Video from October 16, 2014 on tagesschau.de
- Fighting Ebola: A Grand Challenge for Development English-language platform from USAID with a link to a search for solutions to the 2014 Ebola fever epidemic advertised on openIDEO
- Ebola in Sierra Leone and Liberia , reports, videos and fact sheets from Welthungerhilfe
- Disease: West Africa is fighting Ebola - video from December 9, 2014 by Quarks & Co in the ARD Mediathek
Individual evidence
- ↑ a b 2014 Ebola Outbreak in West Africa - Outbreak Distribution Map. Centers for Disease Control and Prevention (CDC), September 14, 2014, accessed September 21, 2014 .
- ↑ Centers for Disease Control and Prevention (CDC): Chronology of Ebola Hemorrhagic Fever Outbreaks . On: cdc.gov from June 24, 2014.
- ↑ a b Ebola Situation Report - March 16, 2016. World Health Organization (WHO), March 16, 2016, accessed on March 18, 2016 (English).
- ↑ a b c d e f g h WHO: Ebola Response Roadmap Situation Report. (PDF; 1.78 MB) WHO: Situation reports: Ebola response roadmap , October 3, 2014, accessed on October 5, 2014 (English).
- ↑ a b c d WHO Ebola Response Team: Ebola Virus Disease in West Africa - The First 9 Months of the Epidemic and Forward Projections In: New England Journal of Medicine. September 9, 2014, p. 140926130020005, ISSN 0028-4793 . doi: 10.1056 / NEJMoa1411100 .
- ↑ a b Epidemic: Nigeria declares a national emergency because of Ebola . On: Spiegel Online from August 9, 2014.
- ↑ a b c d e f g h i WHO: Statements of the International Health Regulations Emergency Committee on the determination of the PHEIC . dated August 8, 2014.
- ↑ Ebola virus disease update - West Africa. World Health Organization (WHO): Disease Outbreak News, August 8, 2014, accessed August 9, 2014 .
- ↑ a b Ebola epidemic in West Africa - Canada offers untested vaccine. (No longer available online.) Tagesschau , August 13, 2014, archived from the original on August 13, 2014 ; accessed on August 14, 2014 .
- ↑ a b UN announces mission to combat Ebola, declares outbreak 'threat to peace and security'. UN , September 18, 2014, accessed September 19, 2014 .
- ^ "WHO declares Liberia Ebola-free", Spiegel-Online from May 8, 2015 spiegel.de
- ↑ Another Ebola case in Liberia. Die Tageszeitung , June 30, 2015, accessed on June 30, 2015 .
- ↑ Mali declares Ebola defeated . On: Sueddeutsche Zeitung online from January 19, 2015, accessed on January 19, 2015.
- ↑ a b c Ebola epidemic is over . On: Sueddeutsche Zeitung online , January 14, 2016, accessed on January 14, 2016.
- ↑ Another Ebola case confirmed . In: FAZ.net , January 21, 2016, accessed on January 21, 2016.
- ↑ spiegel.de
- ↑ Situation Report Ebola Virus Disease 10 June 2016. (PDF) 10 June 2016, accessed on 26 September 2018 (English).
- ^ Franziska Badenschier: Ebola: For decades in West Africa. Spektrum.de , May 12, 2015, accessed on May 13, 2015 .
- ↑ a b S. Baize, D. Pannetier u. a .: Emergence of Zaire Ebola Virus Disease in Guinea. In: The New England Journal of Medicine . Volume 371, No. 15, October 9, 2014, pp. 1418–1425, doi: 10.1056 / NEJMoa1404505 full text (PDF).
- ↑ G. Dudas, A. Rambaut: Phylogenetic Analysis of Guinea 2014 EBOV Ebolavirus Outbreak. In: PLoS Currents Outbreaks. Volume 6, May 2, 2014, ISSN 2157-3999 . doi: 10.1371 / currents.outbreaks.84eefe5ce43ec9dc0bf0670f7b8b417d . PMID 24860690 . PMC 4024086 (free full text).
- ↑ S. Calvignac-Spencer, JM Schulze u. a .: Clock Rooting Further Demonstrates that Guinea 2014 EBOV is a Member of the Zaïre Lineage. In: PLoS Currents Outbreaks. Volume 6, June 16, 2014, ISSN 2157-3999 . doi: 10.1371 / currents.outbreaks.c0e035c86d721668a6ad7353f7f6fe86 . PMID 24987574 . PMC 4073806 (free full text).
- ↑ a b c d e f g h i j k WHO: Ebola Response Roadmap Situation Reports. World Health Organization (WHO), December 13, 2014, accessed January 19, 2015 .
- ↑ a b c d WHO: Ebola Response Roadmap Situation Report. (PDF; 1.25 MB) WHO: Situation reports: Ebola response roadmap , September 24, 2014, accessed on September 25, 2014 (English).
- ↑ a b c d e WHO: Ebola Response Roadmap Situation Report. (PDF; 1.32 MB) WHO: Situation reports: Ebola response roadmap , October 1, 2014, accessed on October 2, 2014 (English).
- ↑ a b Questions and Answers: Estimating the Future Number of Cases in the Ebola Epidemic - Liberia and Sierra Leone, 2014–2015. Centers for Disease Control and Prevention (CDC), September 23, 2014, accessed September 28, 2014 .
- ↑ a b WHO: Ebola Response Roadmap Situation Report. (PDF; 1.55 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , December 31, 2014, accessed on January 3, 2015 (English).
- ↑ a b c d The outbreak of Ebola virus disease in Senegal is over. World Health Organization (WHO), October 17, 2014, accessed October 17, 2014 .
- ↑ a b Nigeria is now free of Ebola virus transmission. World Health Organization (WHO), October 20, 2014, accessed October 20, 2014 .
- ↑ a b c d WHO congratulates Spain on ending Ebola transmission. World Health Organization (WHO), December 2, 2014, accessed December 7, 2014 .
- ^ WHO: Ebola Response Roadmap Situation Report. (PDF; 1.55 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , December 24, 2014, accessed on January 4, 2015 (English).
- ^ WHO: Ebola Response Roadmap Situation Report. (PDF; 1.55 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , January 21, 2015, accessed on January 24, 2015 (English).
- ^ WHO: Ebola Response Roadmap Situation Report. (PDF; 1.81 MB) World Health Organization (WHO): Ebola Situation reports , March 4, 2015, accessed on March 12, 2015 .
- ^ New Ebola case in Sierra Leone; WHO continues to stress risk of more flare-ups . WHO statement, January 15, 2016
- ↑ a b c d Ebola situation in Liberia: non-conventional interventions needed. World Health Organization (WHO), September 8, 2014, accessed September 8, 2014 .
- ↑ CIA: The World Factbook . accessed on December 2, 2014.
- ↑ a b Ebola virus disease in Guinea. (No longer available online.) World Health Organization (WHO) Africa, March 23, 2014, archived from the original on October 9, 2014 ; accessed on October 9, 2014 (English).
- ↑ Republique de Guinee - Ministère de la Santé, Conakry, March 25, 2014: Infos sur la fièvre hémorragique a virus Ebola en Guinée ( Memento of October 6, 2014 in the Internet Archive ) (PDF).
- ↑ Ebola virus disease in Guinea - update. World Health Organization (WHO): Disease Outbreak News, March 27, 2014, accessed October 9, 2014 .
- ^ A b Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, April 1, 2014, accessed October 9, 2014 .
- ^ A b Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, April 17, 2014, accessed October 9, 2014 .
- ^ A b Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, May 15, 2014, accessed October 9, 2014 .
- ^ A b Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, May 28, 2014, accessed October 9, 2014 .
- ↑ a b c Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, May 30, 2014, accessed October 9, 2014 .
- ^ A b Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, June 10, 2014, accessed October 9, 2014 .
- ↑ a b c d Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, June 18, 2014, accessed October 9, 2014 .
- ↑ a b c d e f g h i j k l Previous Updates: 2014 West Africa Outbreak. Centers for Disease Control and Prevention (CDC), October 8, 2014, accessed October 9, 2014 .
- ↑ a b c WHO: Ebola Response Roadmap Situation Report 1. (PDF; 1.0 MB) WHO: Situation reports: Ebola response roadmap , August 29, 2014, accessed on September 14, 2014 (English).
- ↑ a b c Ebola virus disease outbreak - west Africa. World Health Organization (WHO): Disease Outbreak News, September 4, 2014, accessed October 9, 2014 .
- ↑ a b c d WHO: Ebola Response Roadmap Situation Report 3. (PDF; 546 kB) WHO: Situation reports: Ebola response roadmap , September 12, 2014, accessed on September 13, 2014 (English).
- ↑ a b WHO: Ebola Response Roadmap Update. (PDF; 451 kB) World Health Organization (WHO): Situation reports: Ebola response roadmap , September 16, 2014, accessed on September 17, 2014 (English).
- ↑ a b c d WHO: Ebola Response Roadmap Situation Report. (PDF; 1.68 MB) WHO: Situation reports: Ebola response roadmap , September 18, 2014, accessed on September 19, 2014 (English).
- ↑ a b c d WHO: Ebola Response Roadmap Situation Report. (PDF; 1.5 MB) WHO: Situation reports: Ebola response roadmap , October 8, 2014, accessed on October 8, 2014 (English).
- ↑ a b c d e f g WHO: Ebola Response Roadmap Situation Report. (PDF; 1.49 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , October 15, 2014, accessed on October 15, 2014 .
- ↑ a b c d WHO: Ebola Response Roadmap Update. (PDF; 3.5 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , October 17, 2014, accessed on October 18, 2014 (English).
- ↑ a b c d e f g WHO: Ebola Response Roadmap Situation Report. (PDF; 1.11 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , October 29, 2014, accessed on October 29, 2014 .
- ↑ a b WHO: Ebola Response Roadmap Situation Report. (PDF; 640 kB) World Health Organization (WHO): Situation reports: Ebola response roadmap , October 31, 2014, accessed on November 1, 2014 (English).
- ↑ a b c d e f g h WHO: Ebola Response Roadmap Situation Report. (PDF; 1.39 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , November 5, 2014, accessed on November 5, 2014 (English).
- ↑ a b c d e f g h i j k l m n o WHO: Ebola Response Roadmap Situation Report. (PDF; 1.6 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , November 19, 2014, accessed on November 20, 2014 (English).
- ↑ a b c d WHO: Ebola Response Roadmap Situation Report. (PDF; 1.9 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , November 12, 2014, accessed on November 13, 2014 (English).
- ↑ a b c d e f g h Mali: Details of the additional cases of Ebola virus disease (updated on 21 November). World Health Organization (WHO), November 20, 2014, accessed November 23, 2014 .
- ↑ a b c d Mali confirms 2 new cases of Ebola virus disease. World Health Organization (WHO), November 25, 2014, accessed November 28, 2014 .
- ↑ UN - Ebola continues to spread rapidly in Sierra Leone . On: Reuters December 9, 2014, accessed December 14, 2014.
- ↑ a b Ebola is back in Liberia. (No longer available online.) Tagesschau.de , July 2, 2015, archived from the original on July 4, 2015 ; Retrieved July 3, 2015 .
- ↑ a b c d Information on Ebola virus disease in West Africa, the situation in Germany and in other countries . Robert Koch Institute, September 4, 2015, accessed on September 9, 2015.
- ↑ Fabian Urech: Suffering from Ebola. The disease haunts the country of origin. The virus lives on in the mind. Four years after the Ebola epidemic, the people in Guinea, where the disaster originated, are still suffering from the consequences. Would the country be prepared for the virus to return? NZZ Zurich December 8, 2017, pp. 49–51
- ↑ Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, April 2, 2014, accessed October 9, 2014 .
- ↑ Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, April 10, 2014, accessed October 9, 2014 .
- ↑ a b c Appeal to the UN about the Ebola epidemic - “Liberia's national existence is threatened”. (No longer available online.) Tagesschau , September 10, 2014, archived from the original on September 10, 2014 ; Retrieved September 17, 2014 .
- ↑ a b c d WHO: Ebola Response Roadmap Situation Report. (PDF; 1.3 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , October 22, 2014, accessed on October 22, 2014 .
- ↑ a b Ebola diary - episode 39: "Ebola is going back" - really? taz , October 29, 2014, accessed November 14, 2014 .
- ↑ CDC Releases New Reports on Ebola Cases in Liberia and the United States. Centers for Disease Control and Prevention (CDC), November 14, 2014, accessed December 2, 2014 .
- ↑ a b c d e f g h Africa: Overview of the work of Doctors Without Borders in the fight against Ebola. Doctors Without Borders , November 25, 2014, accessed December 2, 2014 .
- ↑ usatoday.com
- ↑ Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, May 6, 2014, accessed October 9, 2014 .
- ↑ Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, June 4, 2014, accessed October 9, 2014 .
- ↑ Video interview with Jochen Moninger from Welthungerhilfe . World hunger Help; on Wikimedia Commons (1: 55-1: 59)
- ↑ a b WHO: Ebola Response Roadmap Situation Report. (PDF; 1.58 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , November 26, 2014, accessed on November 28, 2014 (English).
- ^ New Ebola case in Sierra Leone; WHO continues to stress risk of more flare-ups . WHO statement, January 15, 2016
- ^ A b Ebola virus disease, West Africa - update. World Health Organization (WHO): Disease Outbreak News, July 27, 2014, accessed October 9, 2014 .
- ↑ Ebola virus disease update - West Africa. World Health Organization (WHO): Disease Outbreak News, August 6, 2014, accessed August 9, 2014 .
- ↑ Ebola situation in Port Harcourt, Nigeria. World Health Organization (WHO), September 3, 2014, accessed September 6, 2014 .
- ↑ a b Epidemic in West Africa Ebola reaches Senegal. (No longer available online.) Tagesschau.de, August 29, 2014, archived from the original on August 31, 2014 ; Retrieved August 29, 2014 .
- ↑ Mali case, Ebola imported from Guinea. World Health Organization (WHO), November 10, 2014, accessed November 11, 2014 .
- ↑ WHO: Ebola Response Roadmap Update. (PDF; 844 kB) World Health Organization (WHO): Situation reports: Ebola response roadmap , October 25, 2014, accessed on October 25, 2014 (English).
- ^ WHO: Ebola Response Roadmap Situation Report. (PDF; 1.55 MB) World Health Organization (WHO): Situation reports: Ebola response roadmap , December 17, 2014, accessed on December 22, 2014 (English).
- ^ First Ebola case diagnosed in the US. BBC News , September 30, 2014, accessed September 30, 2014 .
- ↑ Ebola Case in Dallas - The Fear of Contagion. (No longer available online.) Tagesschau , October 2, 2014, archived from the original on October 4, 2014 ; accessed on October 2, 2014 .
- ↑ a b c d e f g Cases of Ebola Diagnosed in the United States. Centers for Disease Control and Prevention (CDC), November 12, 2014, accessed November 14, 2014 .
- ↑ a b Hospital in Texas - Ebola patient in Dallas in mortal danger. (No longer available online.) Tagesschau , October 5, 2014, archived from the original on October 5, 2014 ; Retrieved October 5, 2014 .
- ↑ DW: Nurses in the US tested positive for Ebola. Deutsche Welle , October 12, 2014, accessed on October 12, 2014 .
- ↑ CDC Confirms Healthcare Worker Who Provided Care for First Patient Positive for Ebola. Centers for Disease Control and Prevention (CDC), October 12, 2014, accessed October 13, 2014 .
- ↑ Second Ebola Case in the USA - How Did That Happen? (No longer available online.) Tagesschau , October 13, 2014, archived from the original on October 15, 2014 ; accessed on October 14, 2014 .
- ↑ a b CDC and Frontier Airlines Announce Passenger Notification Underway. Centers for Disease Control and Prevention (CDC), October 15, 2014, accessed October 16, 2014 .
- ↑ a b c Ebola in the USA: Infected nurse had a slight fever on the plane . On: Spiegel Online of October 16, 2014, accessed on October 16, 2014.
- ↑ Flow diagram: Help for the doctor in Germany to clarify whether there is a justified suspicion of Ebola fever. (PDF; 248 kB) RKI: Ebola - Dealing with Ebola Fever Suspected Cases , October 9, 2014, accessed on October 17, 2014 .
- ^ Epidemic in West Africa: Nurse in Madrid clinic infected with Ebola . On: Spiegel Online of October 7, 2014, accessed on October 7, 2014.
- ↑ Madrid - First Ebola infection in Europe. In: Zeit Online . October 6, 2014, accessed October 6, 2014 .
- ↑ Ebola Diary - Part 22: Ebola reaches Europe. taz , October 8, 2014, accessed October 8, 2014 .
- ↑ C. Briseño: Ebola infection in Madrid: "The smallest mistake can be fatal" . On: Spiegel Online of October 8, 2014, accessed on October 12, 2014.
- ↑ Result of the first Ebola virus test - Spanish nurse is virus-free. (No longer available online.) Tagesschau , October 19, 2014, archived from the original on October 19, 2014 ; accessed on October 21, 2014 .
- ↑ Spain: Ebola patient's dog euthanized as a precaution . On: Spiegel Online from October 9, 2014, accessed on October 13, 2014.
- ↑ Ebola case confirmed in Glasgow hospital. BBC News, December 29, 2014, accessed December 29, 2014 .
- ↑ UK Ebola nurse Pauline Cafferkey 'in critical condition'. BBC News, January 4, 2015, accessed January 5, 2015 .
- ↑ Unprecedented number of healthcare workers infected with Ebola virus. World Health Organization (WHO), August 25, 2014, accessed August 29, 2014 .
- ^ WHO: Ebola Response Roadmap Situation Report. (PDF; 1.61 MB) World Health Organization (WHO): Ebola Situation reports , December 30, 2015, accessed on December 31, 2015 (English).
- ↑ a b N. Weber: Ebola: Helpers in danger . On: Spiegel Online from August 29, 2014, accessed on August 29, 2014.
- ↑ a b Fight against Ebola - Lufthansa should develop emergency aircraft . handelsblatt.com, October 19, 2014; accessed on October 28, 2014.
- ↑ a b Analysis: Too few ambulances for Ebola patients in Germany . On: Berliner Zeitung of October 31, 2014, accessed on November 2, 2014.
- ↑ a b Costs of millions: Treatment of Ebola patients from Hamburg more expensive than expected . On: Spiegel Online from October 19, 2014, accessed on November 2, 2014.
- ↑ Franziska Badenschier in Deutschlandfunk Forschung aktuell, April 27, 2015: Healed people transmit deadly virus through sex
- ↑ a b P. Becquart et al .: High prevalence of both humoral and cellular immunity to Zaire ebolavirus among rural populations in Gabon. PLoS One. 2010, Volume 5, No. 2, PMID 20161740 .
- ^ A virologist's tale of Africa's first encounter with Ebola. On: sciencemag.org of August 11, 2014.
- ↑ Ebola Virus Infection - Epidemiology. Medscape, October 13, 2014, accessed October 15, 2014 .
- ↑ Clinical Illness and Outcomes in Patients with Ebola in Sierra Leone . In: The New England Journal of Medicine , October 29, 2014, doi: 10.1056 / NEJMoa1411680
- ↑ WHO: Ebola Response Roadmap Situation Report 2. (PDF; 687 kB) WHO: Situation reports: Ebola response roadmap , September 5, 2014, accessed on September 14, 2014 (English).
- ↑ US Food and Drug Administration: 2014 Ebola Virus Emergency Use Authorization. On: fda.gov from June 8, 2014.
- ↑ AWARENESS TIMES Sierra Leone News & Information, September 29, 2014: Sierra Leone News: Over 1,000 of 2,000 Lab-Confirmed Ebola Cases are not Accounted For! ( Memento from October 6, 2014 in the Internet Archive )
- ↑ Africa - Fresh Graves Point to Undercount of Ebola Toll. The New York Times , September 22, 2014, accessed October 8, 2014 .
- ↑ How many Ebola cases are there really? On: sciencemag.org , October 20, 2014.
- ↑ a b c d e f g h i Why the Ebola outbreak was underestimated. World Health Organization (WHO), August 22, 2014, accessed August 24, 2014 .
- ^ Reaching out to communities at risk of Ebola in Liberia. World Health Organization (WHO), July 31, 2014, accessed October 17, 2014 .
- ^ Christian L. Althaus: Estimating the Reproduction Number of Ebola Virus (EBOV) During the 2014 Outbreak in West Africa . In: PLoS Currents . 2014. doi : 10.1371 / currents.outbreaks.91afb5e0f279e7f29e7056095255b288 .
- ↑ H. Nishiura, G. Chowell: Early Transmission Dynamics of Ebola Virus Disease (EVD), West Africa, March To August 2014 . In: Eurosurveillance . tape 19 , no. 36 , September 11, 2014, p. 20894 (English, online [accessed October 15, 2014]).
- ↑ ETH researchers calculate the true extent of the Ebola epidemic. Tages-Anzeiger, October 8, 2014, accessed October 15, 2014 .
- ^ History and Epidemiology of Global Smallpox Eradication ( Memento of July 15, 2007 in the Internet Archive ) (PDF) CDC and WHO. P. 17.
- ↑ WHO considers the extent of the Ebola epidemic to be underestimated. On: Reuters, August 15, 2014, accessed on August 21, 2014
- ↑ WHO: Extent of the Ebola epidemic in West Africa clearly underestimated. ( Memento of August 26, 2014 in the Internet Archive ) On: AFP of August 15, 2014, accessed August 21, 2014.
- ↑ Rapid spread in West Africa - WHO fears 20,000 Ebola cases. (No longer available online.) Tagesschau , August 28, 2014, archived from the original on August 30, 2014 ; Retrieved August 29, 2014 .
- ↑ Kai Kupferschmidt: Disease modelers project a Rapidly rising toll from Ebola. From: sciencemag.org August 31, 2014, accessed September 20, 2014.
- ↑ Dismal forecast: US researchers fear hundreds of thousands of new Ebola cases . On: Spiegel Online of September 13, 2014, accessed on September 20, 2014.
- ^ WHO Virtual Press Conference on Ebola response. (PDF) of October 14, 2014.
- ↑ An alarm call from Laurie Garrett: Ebola puts the whole planet in danger . In: FOCUS magazine. No. 38, 2014; On: focus.de , last accessed on September 26, 2014.
- ↑ WHO response to internal Ebola document leaked to media. WHO, October 18, 2014, accessed October 23, 2014 .
- ↑ Ebola crisis: UN envoy rejects criticism of agency's response. BBC, October 18, 2014, accessed October 23, 2014 .
- ↑ Leaked documents reveal behind-the-scenes Ebola vaccine issues. science magazine, October 23, 2014, accessed November 30, 2014 .
- ↑ Quarantine after Ebola case 21 days prison in the own home /. (No longer available online.) Welthungerhilfe , December 20, 2014, archived from the original on December 21, 2014 ; Retrieved December 25, 2014 .
- ^ How the experimental Ebola serum works . CNN, Aug 6, 2014
- ↑ a b drug against Ebola disease - hope for a healing serum. (No longer available online.) Tagesschau , August 8, 2014, archived from the original on August 8, 2014 ; accessed on August 13, 2014 .
- ↑ a b c d e After treatment with ZMapp - US Ebola patients apparently cured. (No longer available online.) Tagesschau , August 21, 2014, archived from the original on August 24, 2014 ; accessed on August 22, 2014 .
- ^ First death in Europe: priest died in Spain . On: derstandard.at of August 12, 2014, accessed on August 19, 2014.
- ↑ a b Ebola Therapy From an Obscure Biotech Firm Is Hurried Along. The New York Times , August 6, 2014, accessed August 13, 2014 .
- ^ WHO: Experimental therapies: growing interest in the use of whole blood or plasma from recovered Ebola patients (convalescent therapies) . September 26, 2014
- ↑ James Gallagher: Ebola blood-therapy team set up. In: BBC News . October 23, 2014, accessed October 26, 2014 .
- ↑ Ebola expert on untested drugs - "More harm than help". Tagesschau , August 12, 2014, accessed on August 22, 2014 .
- ↑ Ethical considerations on the use of unauthorized drugs against Ebola. World Health Organization (WHO), August 12, 2014, accessed on August 14, 2014 .
- ^ A b c Epidemic in West Africa - AU for unapproved Ebola drugs. (No longer available online.) Tagesschau , August 13, 2014, archived from the original on August 13, 2014 ; accessed on August 13, 2014 .
- ↑ a b WHO Ebola news. World Health Organization (WHO), August 15, 2014, accessed August 16, 2014 .
- ↑ The Fight Against the Disease - Ebola Serum for Liberia's Doctors. (No longer available online.) Tagesschau , August 12, 2014, archived from the original on August 12, 2014 ; accessed on August 13, 2014 .
- ↑ Individual reports on experimental therapies. World Health Organization (WHO), August 21, 2014, accessed August 22, 2014 .
- ↑ a b Ebola epidemic in West Africa - doctor dies after ZMapp treatment. (No longer available online.) Tagesschau , August 25, 2014, archived from the original on August 27, 2014 ; Retrieved August 25, 2014 .
- ^ Philipp Graf: The anti-Ebola offensive. In: transcript. Issue 9, 2014, pp. 18-19.
- ↑ Canada offers experimental Ebola vaccine VSV-EBOV to West Africa. CBC News, August 12, 2014, accessed September 23, 2014 .
- ↑ Canada's experimental Ebola vaccine: How does it work? CTV News, August 13, 2014, accessed September 23, 2014 .
- ↑ Ebola epidemic in West Africa - Canada supplies WHO possible vaccine. (No longer available online.) Tagesschau , October 21, 2014, archived from the original on October 21, 2014 ; accessed on October 21, 2014 .
- ↑ International partnership conducts first clinical studies for Ebola drugs. Doctors Without Borders , November 13, 2014, accessed November 20, 2014 .
- ↑ a b c d e f g Exit call for the countries Guinea, Liberia and Sierra Leone. Federal Foreign Office , November 25, 2014, accessed on December 2, 2014 .
- ↑ a b c Epidemic in Africa: Guinea closes borders with Ebola countries . On: Spiegel Online from August 9, 2014.
- ↑ a b c Ebola: Sierra Leone declares a state of emergency, Liberia closes all schools . On: Spiegel Online from July 31, 2014.
- ↑ a b c d Ebola epidemic in West Africa - Night curfew in Liberia. (No longer available online.) Tagesschau , August 20, 2014, archived from the original on August 22, 2014 ; accessed on August 22, 2014 .
- ↑ a b c d Ebola - UN demands 20 times as much Ebola aid as promised. In: Zeit Online . October 9, 2014, accessed October 12, 2014 .
- ↑ Fight against epidemic in West Africa - Liberia lifts Ebola emergency. (No longer available online.) Tagesschau , November 13, 2014, archived from the original on November 16, 2014 ; accessed on November 14, 2014 .
- ↑ Ebola in West Africa: epicenter shifts to Sierra Leone. Doctors Without Borders , July 24, 2014, accessed November 12, 2014 .
- ↑ a b c Fear of the spread of the Ebola virus: Ivory Coast isolates itself. (No longer available online.) Tagesschau.de, August 23, 2014, archived from the original on August 24, 2014 ; accessed on August 24, 2014 .
- ↑ a b c curfew in African country - quarantine for all of Sierra Leone. (No longer available online.) Tagesschau , September 18, 2014, archived from the original on September 19, 2014 ; Retrieved September 20, 2014 .
- ↑ Three-day curfew in Sierra Leone - Ebola workers attacked at funeral. (No longer available online.) Tagesschau , September 20, 2014, archived from the original on September 21, 2014 ; Retrieved September 20, 2014 .
- ↑ Ebola: "Need soldiers who shoot if necessary". Courier, September 17, 2014, accessed October 29, 2014 .
- ^ Help for children in Sierra Leone. ZDF today, October 18, 2014, accessed on October 29, 2014 .
- ↑ a b c Sierra Leone: Ebola destroys economic development. Welthungerhilfe, October 16, 2014, accessed on November 26, 2014 .
- ↑ Ebola in Sierra Leone: Warning - Level 3. Centers for Disease Control and Prevention (CDC), October 7, 2014, accessed on October 8, 2014 .
- ↑ sueddeutsche.de
- ↑ a b Ebola Diary - Part 17: When the scouts came to Womey. taz , October 1, 2014, accessed October 8, 2014 .
- ↑ a b Ebola in Guinea: Warning - Level 3. Centers for Disease Control and Prevention (CDC), October 7, 2014, accessed on October 8, 2014 (English).
- ↑ FAQ: What is Ebola? Tagesschau , August 8, 2014, accessed on August 12, 2014 .
- ↑ Epidemic in West Africa: World Bank gives $ 200 million to fight Ebola . On: Spiegel Online from August 5, 2014.
- ↑ a b c IMF approves financial aid - $ 130 million against Ebola. (No longer available online.) Tagesschau , September 27, 2014, archived from the original on September 28, 2014 ; accessed on September 28, 2014 .
- ↑ Fight against Ebola - With 3000 helpers against the virus. (No longer available online.) Tagesschau , September 16, 2014, archived from the original on September 16, 2014 ; Retrieved September 17, 2014 .
- ^ WHO welcomes the extensive Ebola support from the United States of America. WHO, September 16, 2014, accessed September 17, 2014 .
- ↑ WHO welcomes Chinese contribution of mobile laboratory and health experts for Ebola response in west Africa. WHO, September 16, 2014, accessed September 17, 2014 .
- ↑ a b Ebola epidemic is spreading rapidly . On: Die Welt vom September 18, 2014, accessed on September 19, 2014.
- ↑ a b c EU health ministers discuss Ebola - help for West Africa - protection for Europe. Tagesschau , October 16, 2014, accessed on October 19, 2014 .
- ↑ Katja Ridderbusch: Both US Ebola patients are doing better . On: Die Welt from August 9, 2014.
- ↑ Michael Remke: "I already felt death" . On: Die Welt from September 4, 2014.
- ↑ Epidemic: British Ebola infected person reaches London clinic . On: Spiegel Online from August 25, 2014, accessed on August 31, 2014.
- ↑ Ebola: blood serum leads the global race to find a cure . On: The Week of October 22, 2014, accessed November 8, 2014.
- ^ France's First Ebola Patient to Get Experimental Drug. In: The Wall Street Journal, September 19, 2014; accessed October 3, 2014.
- ↑ Hamburg UKE treats Ebola patients. ( Memento from August 28, 2014 in the Internet Archive ) On: ndr.de from August 27, 2014, accessed on August 31, 2014.
- ↑ Treatment at the University Clinic - Frankfurt accepts Ebola patients. ( Memento from October 6, 2014 in the Internet Archive ) On: hr.de October 3, 2014, accessed on October 3, 2014.
- ↑ Treatment in the university clinic - Ebola patient is doing better. ( Memento of November 8, 2014 in the Internet Archive ) On: hr.de of November 5, 2014, accessed on November 8, 2014.
- ↑ St. Georg Hospital - Ebola patient in Leipzig in critical condition. ( Memento from October 10, 2014 in the Internet Archive ) On: mdr.de from October 9, 2014, accessed on October 9, 2014.
- ↑ Ebola patient died in Leipzig. Saxon Newspaper, October 14, 2014.
- ^ An Ebola patient has arrived in Geneva . Handelszeitung , November 21, 2014.
- ^ Philippe Reichen: expulsion from the country because of Ebola . Tages-Anzeiger Online, November 22, 2014
- ↑ Jan D. Walter / Nádia Pontes: Cuban doctors in a double mission . Deutsche Welle , October 24, 2014
- ↑ Ebola patient recovered in Geneva . nzz.ch , December 6, 2014
- ↑ Tom Miles: Influenza drug saves Cuban Ebola patients . Welt Online , December 6, 2014
- ↑ Deaths in the Democratic Republic of the Congo ... Fifth country reports Ebola victims. (No longer available online.) Tagesschau.de, August 24, 2014, archived from the original on August 24, 2014 ; accessed on August 24, 2014 .
- ↑ Questions and answers on the Ebola outbreak in West Africa in 2014. Doctors Without Borders , November 25, 2014, accessed on December 2, 2014 .
- ^ A b Paul Munzinger: Bundeswehr - Ebola aid from the government is an empty promise. In: Zeit Online . October 3, 2014, pp. 1–2 , accessed October 12, 2014 .
- ↑ West Africa - Red Cross committed to the fight against the Ebola epidemic. (No longer available online.) German Red Cross , September 15, 2014, archived from the original on November 29, 2014 ; Retrieved November 20, 2014 .
- ↑ Welthungerhilfe, PM August 16, 2014: Ebola in West Africa. Welthungerhilfe supports Sierra Leone in the fight against Ebola
- ↑ WHO issues roadmap for scaled-up response to the Ebola outbreak. World Health Organization (WHO), August 28, 2014, accessed September 17, 2014 .
- ^ Statement on the 2nd meeting of the IHR Emergency Committee regarding the 2014 Ebola outbreak in West Africa. World Health Organization (WHO), September 22, 2014, accessed November 8, 2014 .
- ↑ Emergency operation - United Nations establish special unit against Ebola. Handelsblatt , September 19, 2014, accessed on September 19, 2014 .
- ↑ United Nations - States leave Ebola aid funds empty. In: Zeit Online . October 17, 2014, accessed October 26, 2014 .
- ↑ UN Mission for Ebola Emergency Response (UNMEER) External Situation Report. (PDF) UNMEER , January 16, 2015, accessed on January 19, 2015 (English).
- ↑ UN Mission for Ebola Emergency Response established in Accra. World Health Organization (WHO), September 30, 2014, accessed October 17, 2014 .
- ↑ UN Mission for Ebola Emergency Response (UNMEER), October 16, 2014: UNMEER External Situation Report ( Memento of October 24, 2014 in the Internet Archive ), PDF file 564 kB
- ↑ UN Mission for Ebola Emergency Response (UNMEER), October 24, 2014: Ebola outbreak in west Africa - Key messages ( Memento from December 17, 2014 in the Internet Archive ), PDF file 140 kB
- ↑ a b Ebola spread: Has the WHO achieved its 70-70-60 target? On: Spiegel Online from December 1, 2014, accessed December 7, 2014.
- ^ WHO's contribution to the Ebola response. World Health Organization (WHO), December 1, 2014, accessed December 7, 2014 .
- ↑ Aaron Clamann: “Band Aid 30” single is overshadowed by discussions. RP ONLINE , November 21, 2014, accessed November 23, 2014 .
- ↑ a b Philipp Oehmke: German Band Aid: How to sing about Ebola without sounding completely idiotic? On: Spiegel Online from November 19, 2014, accessed on November 23, 2014.
- ↑ German version of "Band Aid" - With music against Ebola. (No longer available online.) Tagesschau , November 21, 2014, archived from the original on November 24, 2014 ; accessed on November 23, 2014 .
- ↑ EU waives stronger controls because of Ebola . On: zeit.de of October 16, 2014, last accessed on October 28, 2014.
- ↑ More protection in Bavaria. Task force against Ebola . On: sueddeutsche.de of October 7, 2014, last accessed on October 28, 2014.
- ↑ New suspected case in France: Ebola patient receives "ZMapp" . On: n-tv.de of October 10, 2014, last accessed on October 28, 2014.
- ↑ Ebola - British set up crisis team . On: aerztezeitung.de from July 30, 2014, last accessed on October 28, 2014.
- ^ Deutsche Welle, October 10, 2014: Spain sets up Ebola crisis team
- ↑ Ebola epidemic in West Africa - Claudia Roth accuses the federal government of failure . On: tagesspiegel.de from September 18, 2014, last accessed on October 28, 2014.
- ↑ Foreign Office: The Federal Government's Special Commissioner for the Fight against the Ebola Epidemic . On: Auswaertiges-amt.de as of October 8, 2014, last accessed on October 28, 2014.
- ↑ Aid flights to West Africa - Ebola aid from the German armed forces starts. (No longer available online.) Tagesschau , September 25, 2014, archived from the original on September 28, 2014 ; accessed on September 28, 2014 .
- ^ Bundeswehr medical service: Ebola: Inquiry with tropical medicine . On: sanitaetsdienst-bundeswehr.de from August 20, 2014, last accessed on October 28, 2014.
- ↑ a b c Help against Ebola is slow - too few doctors, too few donations. (No longer available online.) Tagesschau , October 22, 2014, archived from the original on October 25, 2014 ; Retrieved November 8, 2014 .
- ↑ a b c German Ebola helpers in Liberia - After the deployment to the hotel for 21 days? (No longer available online.) Tagesschau , November 18, 2014, archived from the original on November 19, 2014 ; Retrieved December 7, 2014 .
- ↑ Alexandra Möckel, Bianca Jordan: Departure of first assistants to Monrovia - If not us, then who? On: sanitaetsdienst-bundeswehr.de of November 7, 2014, accessed on November 8, 2014.
- ↑ Converted Lufthansa Airbus - Ebola plane goes into operation . On: handelsblatt.com of November 26, 2014, accessed on November 26, 2014.
- ^ Matthias Frank: Checking the transport isolators . On: sanitaetsdienst-bundeswehr.de of October 16, 2014, accessed on November 8, 2014.
- ↑ Michael Weissenborn: Fighting Ebola - How the US Army saves lives . On: stuttgarter-nachrichten.de of November 23, 2014, accessed on November 24, 2014.
- ^ WHO: Statement from the Travel and Transport Task Force on Ebola virus disease outbreak in West Africa. On: who.int of November 7, 2014, accessed November 12, 2014.
- ^ WHO: Air travel is low-risk for Ebola transmission. World Health Organization (WHO), August 14, 2014, accessed August 16, 2014 .
- ↑ Epidemic in West Africa: Senegal closes borders with Guinea because of Ebola at sueddeutsche.de, August 22, 2014, accessed on August 24, 2014.
- ↑ Ebola Hysteria in the USA: Undignified Confusion . On: Spiegel Online from October 26, 2014.
- ^ As West Africa Ebola outbreak worsens, CDC issues Level 3 Travel Warning. Centers for Disease Control and Prevention (CDC), July 31, 2014, accessed December 2, 2014 .
- ↑ a b Enhanced Airport Entry Screening to Begin for Travelers to the United States from Mali. Centers for Disease Control and Prevention (CDC), November 16, 2014, accessed December 2, 2014 .
- ↑ Ebola in Liberia: Warning - Level 3. (No longer available online.) Centers for Disease Control and Prevention (CDC), November 16, 2014, archived from the original on August 9, 2014 ; accessed on December 2, 2014 .
- ↑ Ebola in Nigeria: Alert - Level 2. Centers for Disease Control and Prevention (CDC), August 13, 2014, accessed on August 14, 2014 (English).
- ↑ Ebola in Nigeria: Watch - Level 1. Centers for Disease Control and Prevention (CDC), October 7, 2014, accessed on October 8, 2014 .
- ↑ a b simulation - WHO reports more than 4,000 deaths from Ebola. In: Zeit Online . October 11, 2014, accessed October 12, 2014 .
- ↑ Millions of people during the Hajj - fear of Ebola during the pilgrimage. (No longer available online.) Tagesschau , October 2, 2014, archived from the original on October 3, 2014 ; Retrieved October 3, 2014 .
- ↑ a b Fear of the Ebola virus - Canada imposes a ban on entry. (No longer available online.) Tagesschau , November 1, 2014, archived from the original on November 2, 2014 ; Retrieved November 2, 2014 .
- ↑ Whoever enters is isolated . ( Memento from November 2, 2014 in the Internet Archive ) Tagesschau , October 30, 2014
- ↑ Tourists are allowed to return to North Korea . n-tv , March 3, 2015
- ↑ Epidemic in West Africa: World Bank gives $ 200 million to fight Ebola . On: spiegel.de from August 5, 2014 (accessed August 5, 2014).
- ↑ Embezzled over five million euros. Retrieved December 2, 2017 .
- ↑ Red Cross: Five million euros embezzled in Ebola aid. Retrieved December 2, 2017 .
- ↑ Cases of fraud during the Ebola epidemic. Retrieved December 2, 2017 .
- ^ Richard Hamilton: Ebola crisis: The economic impact. BBC News, August 20, 2014, accessed September 17, 2014 .
- ^ Ebola could wreck W Africa economies, warns World Bank. BBC News, September 17, 2014, accessed September 17, 2014 .
- ↑ Ebola Diary - Episode 42: The poorest die. taz , November 2, 2014, accessed November 14, 2014 .
- ^ The non-medical impacts of the ebola Crisis in Sierra Leone. Deutsche Welthungerhilfe e. V., October 7, 2014, accessed November 26, 2014 .
- ↑ a b WHO: Ebola endangers progress in the fight against malaria . On: dw.de of December 9, 2014, accessed on December 14, 2014.
- ↑ Ebola virus disease update - west Africa. World Health Organization (WHO), August 20, 2014, accessed August 22, 2014 .
- ↑ Welthungerhilfe Index - Hunger in the world is falling. Tagesschau , October 13, 2014, accessed on October 21, 2014 .
- ↑ a b Doctors Without Borders' new Ebola treatment centers already overcrowded. Doctors Without Borders , August 28, 2014, accessed August 30, 2014 .
- ↑ Meeting of the IMF and World Bank - Ebola countries call for help to the world. (No longer available online.) Tagesschau , October 9, 2014, archived from the original on October 11, 2014 ; accessed on October 12, 2014 .
- ↑ Ebola patients turned away due to overcrowding. Treatment centers have to turn away more and more patients . On: heilpraxisnet.de from September 13, 2014, accessed on September 18, 2014.
- ↑ Pierre Trbovic: Experience report: "I went behind the Ebola station to cry" . On: aerztezeitung.de from September 12, 2014, accessed on September 18, 2014.
- ↑ Ebola Diary - Episode 26: The anger behind the protective suits. taz , October 13, 2014, accessed October 14, 2014 .
- ↑ Ebola Diary - Part 28: On the way to the state crisis. taz , October 15, 2014, accessed October 21, 2014 .
- ↑ Ebolas consequential damages: measles, malaria, maternal mortality . On: Spektrum.de from March 12, 2015, accessed on March 13, 2015.
- ↑ Epidemic in Africa: Guinea closes borders with Ebola countries. Spiegel.de, October 15, 2014, accessed on July 2, 2015 .
- ↑ Ebola travel restrictions: Visa ban, quarantine, screenings. Sueddeutsche.de, November 3, 2014, accessed on August 3, 2020 .
- ↑ UNWTO: Annual Report 2014 ( Memento of December 28, 2015 in the Internet Archive ) Ebola Page 17 of the PDF file 10.8 MB